Abstract
Families affected by HIV/AIDS in the developing world experience higher risks of psychosocial problems than non-affected families. Positive parenting behavior may buffer against the negative impact of child AIDS-orphanhood and caregiver AIDS-sickness on child wellbeing. Although there is substantial literature regarding the predictors of parenting behavior in Western populations, there is insufficient evidence on HIV/AIDS as a risk factor for poor parenting in low- and middle-income countries. This paper examines the relationship between HIV/AIDS and positive parenting by comparing HIV/AIDS-affected and non-affected caregiver-child dyads (n = 2,477) from a cross-sectional survey in KwaZulu-Natal, South Africa (27.7% AIDS-ill caregivers; 7.4% child AIDS-orphanhood). Multiple mediation analyses tested an ecological model with poverty, caregiver depression, perceived social support, and child behavior problems as potential mediators of the association of HIV/AIDS with positive parenting. Results indicate that familial HIV/AIDS’s association to reduced positive parenting was consistent with mediation by poverty, caregiver depression and child behavior problems. Parenting interventions that situate positive parenting within a wider ecological framework by improving child behavior problems and caregiver depression may buffer against risks for poor child mental and physical health outcomes in families affected by HIV/AIDS and poverty.
Keywords: Parenting; depression; social support; poverty; child behavior, HIV/AIDS; orphan; caregiver
Introduction
Families affected by HIV/AIDS in low- and middle-income countries face multiple psychosocial challenges (Richter et al., 2009). In comparison to non-affected children, children ages 10–17 who are orphaned by AIDS or living with AIDS-ill caregivers have increased risks of mental health problems, poor educational outcomes, stigma and isolation from peers, transactional sex, and child maltreatment (Cluver, 2011). Similarly, HIV-infected caregivers and caregivers of children orphaned by AIDS are at greater risk of having more physical and mental health problems than other caregivers (Kuo & Operario, 2011; Rochat, Bland, Coovadia, Stein, & Newell, 2011). Research has identified parenting as an important link between HIV/AIDS and negative child and caregiver outcomes (Richter, Beyrer, Kippax, & Heidari, 2010). In particular, positive parenting – generally conceptualized as involved, nurturing, and accepting behavior (Maccoby, 1992) – may be a potential buffer HIV/AIDS’s impact on poor child mental health.
In order to fully understand the relationship between positive parenting and HIV/AIDS, it is essential to situate familial HIV/AIDS within a larger ecological framework that includes the role of other social, parental, and child factors (Belsky, 1984). Parental physical illness and child orphanhood have been shown to negatively affect positive parenting by decreasing engagement, disrupting family routines, and increasing parental absence and neglect (Armistead, Klein, & Forehand, 1995). In South Africa, HIV/AIDS-affected families are associated with increased poverty (Gillies, Tolley, & Wolstenholme, 1996), parental depression (Kuo, Operario, & Cluver, 2012), lack of social support (Casale, 2012), and increased child behavior problems (Sipsma et al., 2013). Since these factors are also associated with reduced positive parenting, they may play a mediating role in the association between HIV/AIDS and positive parenting (Andersen, 1992; Gershoff, 2007; Lovejoy, Graczyk, O'Hare, & Neuman, 2000; Pardini, 2008).
However, there is limited evidence on the impact of HIV/AIDS on parent behavior in low- and middle-income countries – and even less on the mechanisms that by which HIV/AIDS affects parenting. Most research on HIV/AIDS and parenting has focused on HIV-positive mothers in the developed world. For instance, a 4-year longitudinal study in the United States found seropositive mothers of children ages 10–15 to have lower quality parent-child relationships and less positive parenting than HIV-negative mothers (Forehand et al., 2002). Another studied showed that HIV-positive mothers’ level of illness to negatively impact family routines and parental monitoring in families with adolescents (Murphy, Marelich, Herbeck, & Payne, 2009). Likewise, lower levels of social support were found in HIV-positive mothers in comparison to uninfected mothers of children ages 6–11 (Dorsey, Klein, & Forehand, 1999). Searches for developing world evidence found only one quantitative study examining parent behavior amongst elderly caregivers of AIDS-orphaned children. This cross-sectional survey in Kenya (n = 141) found high levels of aggressive parenting and parenting stress in grandmothers of children orphaned by AIDS aged 6–10 (Oburu & Palmerus, 2003). However, no comparison groups were available to assess whether parent behavior was specifically due to caring for an AIDS-orphaned child.
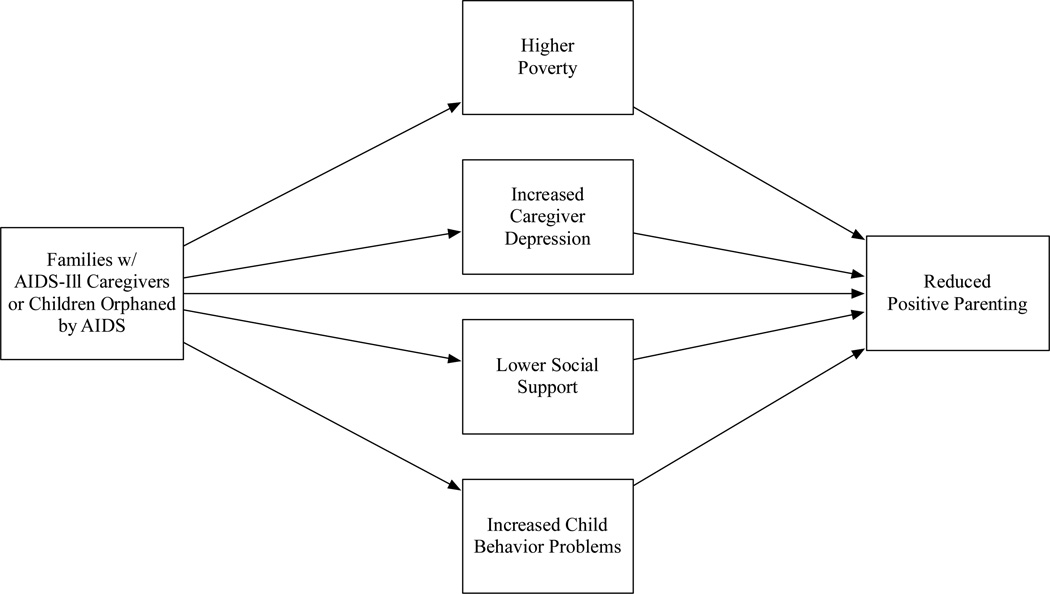
By comparing affected and non-affected families from a cross-sectional survey of caregiver-child dyads in South Africa (n = 2,477), this paper examines two key questions regarding the relationship between HIV/AIDS and positive parenting in low- and middle-income countries: 1) Are families with AIDS-ill caregivers or children orphaned by AIDS associated with reduced positive parenting in comparison to non-affected families? 2) Are these associations consistent with mediation by other risk factors related to positive parenting and HIV/AIDS (Figure 1)?
Figure 1.
Hypothesized multiple mediation model of familial HIV/AIDS's association with positive parenting.
Methods
Participants
Caregiver-child dyads (n = 2,477) were selected by means of stratified systematic random sampling in rural and peri-urban sites with over 30% HIV prevalence in the KwaZulu-Natal province of South Africa (Department of Health, 2011). Census enumerator and tribal authority areas were randomly selected with door-to-door household sampling (Stoker, 1987). This study recruited families with children ages 10–17 due to the high risk of adolescent HIV-infection as a result of transactional sex and other risk behavior including substance abuse, school dropout, and criminal activity (Dunkle et al., 2007). Inclusion criteria required both children and caregivers (adults over the age of 18 and identified as the child’s primary caregiver) to reside in the same household for at least 4 nights per week. In the event of multiple eligible children living in the same household, one child was randomly selected for the study.
Procedure
Ethical protocols were approved by the University of Oxford, the University of KwaZulu-Natal, and the KwaZulu-Natal Departments of Health and Education. Adult and child questionnaires were translated into isiZulu and back-translated into English to assure accuracy. Trained and supervised isiZulu research assistants conducted face-to-face interviews that lasted between 40–60 minutes per participant. Participation was voluntary with informed consent obtained from both children and caregivers. The study followed strict confidentiality procedures with the exception of a child reporting risk of significant harm, in which cases were referred to welfare and health services. No incentive or financial remuneration for participation was provided with the exception of a certificate of appreciation.
Measures
Positive Parenting
This study used child reports of the positive parenting subscale from the Alabama Parenting Questionnaire-Short Form (APQ-SF; 3-items) (Elgar, Waschbusch, Dadds, & Sigvaldason, 2007). Although no parenting scales have been psychometrically tested in South Africa, the APQ-SF has been widely used as a reliable measurement of parent behavior (Frick, 1991). Children reported on frequency of positive parenting over the past month (e.g. – “your caregiver says you have done something well”). Higher scores indicate more frequent positive parenting (α = .80).
AIDS-related Parental Death and Caregiver Illness
In South Africa, determining caregiver HIV-status and AIDS-related parental mortality is challenging due to low availability of clinical data, low testing rates, and unreliable self-reports of current HIV-status (Peltzer, Matseke, Mzolo, & Majaja, 2009). Therefore, this study used child and caregiver reports of the Verbal Autopsy Questionnaire (VA) to determine child AIDS-orphanhood and caregiver AIDS-illness (Lopman et al., 2006). The VA has been validated in South Africa with a 76% positive prediction rate, 89% sensitivity, and 93% specificity (Hosegood, Vanneste, & Timaeus, 2004; Kahn, Tollman, Garenne, & Gear, 2000). This study required the presence of 3 or more AIDS-related symptoms (e.g. – oral candidasis, respiratory tract infection, and persistent diarrhea) to define caregiver AIDS-illness and/or AIDS-related parental mortality (WHO, 1994).
Socio-demographic factors
Socio-demographic information – age and gender, household size, and whether the caregiver was the child’s biological parent – were measured using items from the South Africa National Census and South Africa Demographic and Health Survey (Statistics South Africa, 2001). These factors were controlled for as potential confounders in all data analyses.
Poverty
The Basic Necessities Scale (BNS; 8-items) assessed socioeconomic status by measuring access to socially perceived household necessities for children (Wright, 2008). This scale has been used previously in the South African Social Attitudes Survey (Pillay, Roberts, & Rule, 2006). It identifies basic household items that families are unable to afford – food, toiletries, clothes, and shoes, as well as school uniforms, equipment, and fees. Higher scores indicate higher levels of poverty (α = 0.84).
Caregiver depression
Caregiver depression was measured by the Centre for Epidemiological Studies Depression Scale (CES-D, 20-items) (Radloff, 1977). The CES-D has been used previously in multiple South African populations (Pretorius, 1991). Adults reported on the frequency of specific negative thoughts or feelings during the past week (e.g. – “I have no hope for the future”). Higher scores indicate higher depression (α = .95).
Caregiver perceived social support
Perceived social support was measured with adult reports of the Medical Outcome Study Social Support Survey (19-items; MOS-SSS) (Sherbourne & Stewart, 1991). Although not validated in South Africa, the MOS-SSS has been used extensively to assess social support in HIV-positive populations (Burgoyne, 2000). Adults reported on the frequency of support available (e.g. – “someone to confide in or talk to about yourself or your problems”). Higher scores indicate higher social support (α = .99).
Child behavior problems
This study assessed child behaviour problems using adult reports of the Strengths and Difficulties Questionnaire (SDQ; 20-items) (Goodman, 2001). The SDQ provides an overall assessment of internal and external child behavior problems and has prior use in South African populations (Goodman, Lamping, & Ploubidis, 2010; Goodman, Cluver, Tshandu, & Vondani, 2004). Adult caregivers reported on the quality of their child’s behavior over the last month (e.g. – “often loses temper”). Higher scores indicate more behavior problems (α = .71).
Analysis strategy
This study used child reports of positive parenting and caregiver reports for potential mediating factors to avoid method overlap in which poor parental mental health may negatively influence self-reports of parenting behavior (Gardner, 2000). Analyses were conducted using SPSS Statistics 18.0. Missing data was less than 1% and missing at random. For psychometric scales, the study used mean imputation (Schlomer, Bauman, & Card, 2010). The distribution of continuous predictor variables was normal, with the exception of caregiver depression (skew = 1.049) and household poverty (skew = 1.384). These were normalized using log transformations (Osborn, 2002).
Data analyses were conducted in two steps. First, a series of hierarchical multivariate regression analyses were used to assess associations among caregiver illness, child orphanhood, potential mediating factors, and positive parenting: a) caregiver illness (AIDS-illness and other illness) and potential mediators (poverty, caregiver depression, social support, and child behavior problems) predicting positive parenting; b) child orphanhood (AIDS-orphanhood and orphanhood by other causes) and potential mediators predicting positive parenting; c) caregiver illness variables predicting potential mediating variables; d) child orphanhood variables predicting potential mediating variables. Inclusion in subsequent multiple mediation analyses required significant relationships (p < .05) among HIV/AIDS-related, potential mediating, and positive parenting variables (Baron & Kenny, 1986).
Second, multiple mediation tests were conducted to further examine the associations between familial HIV/AIDS and positive parenting. This study used bootstrapping, a nonparametric resampling procedure to allow for simultaneous testing for indirect effects of multiple mediators, thus determining the extent to which each variable mediates a predictor in the presence of other potential mediators (2004). Based on 1,000 bootstrap samples, tests for significant mediation required bias corrected 95% confidence intervals to not overlap zero (Preacher & Hayes, 2008). All analyses controlled for age, gender, household size, and whether the caregiver was the child’s biological parent.
Results
Socio-demographic statistics for the population sample are summarized in Table 1. The sample of predominantly isiZulu-speaking dyads of African descent (n = 2,477) included 685 dyads with AIDS-ill caregivers (27.7%) and 184 dyads with children orphaned by AIDS (7.4%).
Table 1.
Characteristics of population sample (n = 2477 dyads).
| African (n, %) | 2473 (99.8) |
| isiZulu language (n, %) | 2375 (95.9) |
| Caregiver age (M, SD) | 44.23 (13.87) |
| Caregiver gender, female (n, %) | 2199 (88.8) |
| Child age (M, SD) | 13.57 (2.23) |
| Child gender, female (n, %) | 1334 (53.9) |
| Number of people in household (M, SD) | 6.0 (2.68) |
| Biological parent (n, %) | 1637 (66.1) |
| Caregiver non-AIDS-illness (n, %) | 568 (22.9) |
| Caregiver AIDS-illness (n, %) | 685 (27.7) |
| Child orphaned other causes (n, %) | 306 (12.4) |
| Child orphaned by AIDS (n, %) | 184 (7.4) |
Hierarchical regression analyses
Tables 2 and 3 summarize results for hierarchical regression analyses. Although effect sizes were small, families with AIDS-ill caregivers or with AIDS-orphaned children were significantly related to less positive parenting, higher poverty, higher depression, and more behaviour problems in comparison to non-affected families. There were no significant associations for families with non-AIDS-related caregiver illness or children orphaned by other causes. Higher poverty, higher caregiver depression, less social support, and more child behaviour problems were related to reduced positive parenting in both models. Since social support was not related to AIDS-illness or AIDS-orphanhood, it was not included in subsequent multiple mediation analyses. Both multivariate models accounted for 13% of the variance in positive parenting.
Table 2.
Summary for hierarchical multiple regressions examining associations among caregiver AIDS-illness, caregiver other illness, potential mediating factors, and positive parenting.
| Familial HIV/AIDS | Positive Parenting |
Household Poverty |
Caregiver Depression |
Social Support |
Behaviour Problems |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | |
| Step 1. Demographics | .01* | .00 | .01** | .02*** | .00 | |||||
| Child age | −.017 | −.009 | .008 | .050* | −.015 | |||||
| Child gender | −.033 | .027 | .008 | .019 | −.046* | |||||
| Caregiver age | .045* | −.017 | .080*** | −.013 | −.019 | |||||
| Caregiver gender | .001 | −.013 | −.048** | .061** | −.018 | |||||
| Biological parent | .058** | .012 | .013 | .016 | −.039 | |||||
| Household size | .008 | .042* | .011 | .130*** | −.027 | |||||
| Step 2. Caregiver Illness | .01*** | 03*** | .08*** | .00* | .02*** | |||||
| Other-illness | −.041 | −.083*** | −.014 | .059* | −.022 | |||||
| AIDS-illness | −.064** | .123*** | .284*** | −.014 | .136*** | |||||
| Step 3. Mediating Factors | .12*** | |||||||||
| Other-illness | .012 | |||||||||
| AIDS-illness | −.020 | |||||||||
| Household Poverty | −.137*** | |||||||||
| Caregiver Depression | −.049** | |||||||||
| Social Support | .260*** | |||||||||
| Behaviour Problems | −.072** | |||||||||
p < .05;
p < .01;
p < .001
Table 3.
Summary for hierarchical multiple regressions examining associations among orphanhood by AIDS, orphanhood by other causes, potential mediating factors, and positive parenting.
| Positive Parenting |
Household Poverty |
Caregiver Depression |
Social Support |
Behaviour Problems |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | |
| Step 1. Demographics | .01* | .00 | .01** | .02*** | .00 | |||||
| Step 2. Child Orphanhood | .00* | .01*** | .00* | .00 | .00* | |||||
| Other Causes | .005 | .068** | .038* | .016 | .024 | |||||
| AIDS-related | −.051* | .066** | .049* | −.030 | .045* | |||||
| Step 3. Mediating Factors | .12*** | |||||||||
| Other Causes | 015 | |||||||||
| AIDS-related | −.028 | |||||||||
| Household Poverty | −.139*** | |||||||||
| Caregiver Depression | −.055** | |||||||||
| Social Support | .259*** | |||||||||
| Behaviour Problems | −.073*** | |||||||||
Note: Controlling for child and caregiver gender, child and caregiver age, household size, and whether the caregiver was a biological parent.
p < .05;
p < .01;
p < .001
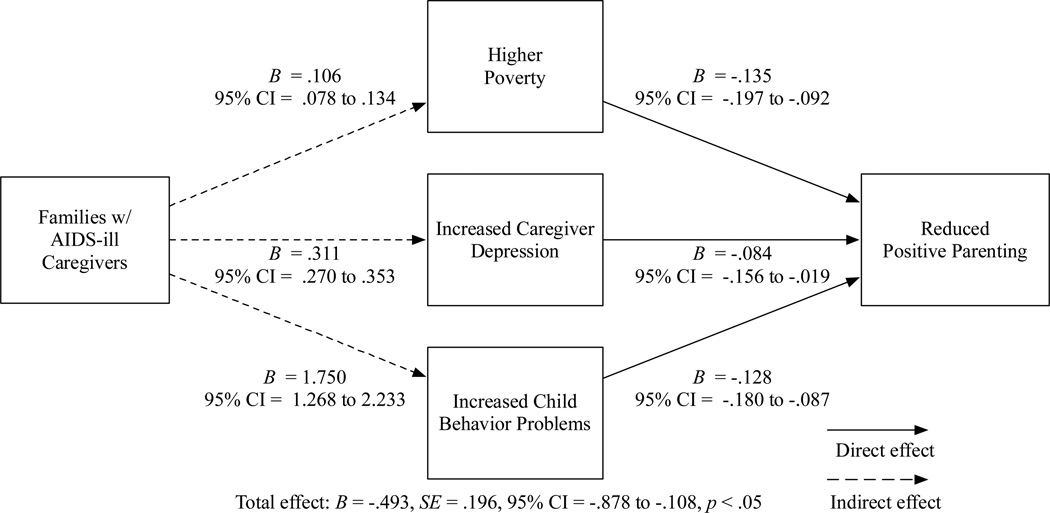
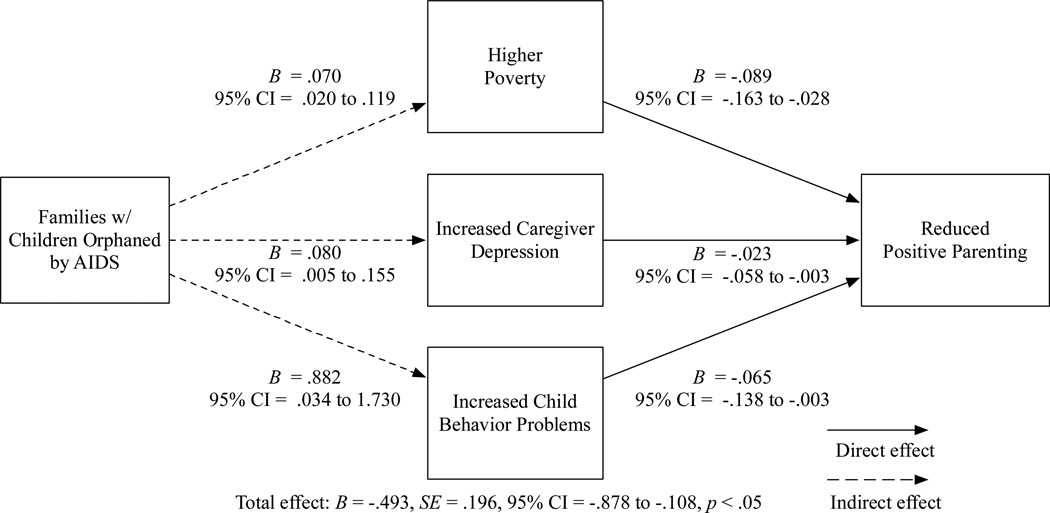
Multiple mediation analyses
Two separate multiple mediation models were used to determine the extent by which hypothesized ecological factors mediated the relationship between HIV/AIDS and positive parenting: Model 1) families with AIDS-ill caregivers compared to those with non-sick caregivers or caregivers with other illnesses; Model 2) families with child AIDS-orphanhood compared to those with non-orphaned children or children orphaned by other causes. Controlling for age, gender, household size, and biological parent status, both models included poverty, caregiver depression, and child behavior problems as potential mediators.
Model 1 (Figure 2) accounted for 7% of variance in positive parenting (R2 = .07, F(10,2458) = 19.08, p < .001). Caregiver AIDS-illness was fully mediated by poverty (B = −.135, 95% CI −.197 to −.092), caregiver depression (B = −.084, 95% CI −.156 to −.019), and child behavior problems (B = −.128, 95% CI −.180 to −.087).
Figure 2.
Final multiple mediation model predicting caregiver AIDS-illness's association with positive parenting, controlling for age, gender, household size, and whether the caregiver was the child's biological parent.
Model 2 (Figure 3) also accounted for 7% of variance in positive parenting (R2 = .07, F(10,2458) = 19.32, p < .001). Child AIDS-orphanhood was fully mediated by poverty (B = −.089, 95% CI −.163 to −.028), caregiver depression (B = −.023, 95% CI −.058 to −.003), and child behavior problems (B = −.065, 95% CI −.138 to −.003).
Figure 3.
Final multiple mediation model predicting child AIDS-orphanhood's association with positive parenting, controlling for age, gender, household size, and whether the caregiver was the child's biological parent.
Discussion
This study is the first large-scale survey to examine the effect of HIV/AIDS on parenting behavior in the developing world. Although effect sizes were small, families with AIDS-ill caregivers and those with children orphaned by AIDS were associated with less positive parenting in comparison with to non-affected families. On the other hand, families with non-AIDS related sick caregivers or children orphaned by other causes were not associated with positive parenting. This indicates that there may be a specific association between HIV/AIDS and caregivers’ ability to positively engage with their children. Recent research in South Africa found that children orphaned by AIDS and living with AIDS-ill caregivers are more vulnerable to abuse and maltreatment by their caregivers than non-affected children (Cluver, Orkin, Boyes, Gardner, & Meinck, 2011). Furthermore, AIDS-sickness is associated with less capacity to care, as is the case with many other chronic illnesses, thus affecting parental engagement and nurturance (Armistead et al., 1995).
Multiple mediation analyses provided a more in depth understanding of the ecological context of HIV/AIDS and parenting. The role of poverty is consistent with research showing low socioeconomic status linked to less maternal involvement and less positive parent-child interaction (Bradley & Corwyn, 2002). This is particularly relevant in HIV/AIDS affected families due to loss of work, sickness, and medical and funeral expenses (Collins & Leibbrandt, 2007). Furthermore, depression may limit caregivers’ capacity to engage positively with their AIDS-orphaned children due to increased stress and perceived stigma associated with HIV/AIDS (Kuo et al., 2012). Likewise, negative life events, such as parental illness or bereavement, are associated with increased maternal depression and reduced positive parent-child interaction (Webster-Stratton & Hammond, 1988).
The role of child behavior problems requires further discussion. Results are consistent with research in South Africa that has shown more child behavior problems in families with children orphaned by AIDS (Cluver, Gardner, & Operario, 2007) or AIDS-symptomatic mothers (Sipsma et al., 2013). Other research has linked child behavior problems to reduced parenting skills due to increased stress associated with HIV/AIDS (Murphy, Marelich, Armistead, Herbeck, & Payne, 2010). However, whether parenting mediates child behavior or vice versa is inconclusive. Although parenting has traditionally been considered an antecedent to developing child behavior problems (Reid & Patterson, 1989), recent longitudinal research in the United States demonstrates a bidirectional relationship (Pardini, 2008). Moreover, while parenting tends to affect child behavior in younger children, this relationship shifts during early adolescence in which child behavior influences parenting more than the reverse (Bradley & Corwyn, 2012). Future longitudinal or interventional research could valuably establish causal or reciprocal associations between child behavior and parenting in HIV/AIDS affected families.
This study had a number of limitations. First, no parenting scales have been psychometrically tested in South Africa. Therefore, it is important to interpret these findings with caution, as the APQ-SF may function differently in the current sample than with Western populations. Nonetheless, the reliability of the positive parenting subscale was consistent with applications of the APQ-SF in other settings (Robert, 2009). Moreover, causal inference of results must be treated with caution. Cross sectional surveys can only determine probable associations between predictive factors and parenting behavior and not the direction of those associations (Grimes, 2002). Finally, the final mediation models only accounted for 7% of the variance in positive parenting, indicating the presence of other untested factors.
Additional research is necessary to fully understand the relationship between HIV/AIDS and parent behavior. Since evidence in the United States suggests that HIV-infected children are likely to receive inadequate parenting (Potterton, Stewart, & Cooper, 2007), it is important to the impact of child HIV-status on parent behavior in developing countries. Furthermore, future research on HIV/AIDS and parenting should explore other potential mediators, moderators, and moderated mediators (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). In addition to social support as a moderator (Dorsey et al., 1999), these may include boys (Mboya, 1995), parenting stress (Abidin, 1992), parenting self-efficacy (Raikes & Thompson, 2005), parental substance abuse, marital dysfunction (Erel & Burman, 1995), intimate partner violence (Levendosky, Leahy, Bogat, Davidson, & von Eye, 2006), social capital (Lee, 2009), child anxiety or depression (McLeod, Wood, & Weisz, 2007), and prevailing cultural attitudes, (Barber, 2000). Finally, research is needed on the impact of HIV/AIDS on parenting in families with preadolescent children and infants, especially due to the potential negative impacts of mother-to-child transmission and child abuse.
These findings suggest that interventions targeted at strengthening child-caregiver relationships may require consideration of the broader social factors that influence parent behavior (Richter, 2013). Rotheram-Borus et al. have argued for the need to re-conceptualize HIV/AIDS from an individual disease to a family-level experience that impacts family functioning (2005). This perspective resonates family systems theory, in which the family unit is the primary context for understanding parenting (Cox, 1997). Family disruptions as severe as AIDS-related parental illness, parental absence and parental death can substantially impact parenting (Antle, Wells, Goldie, DeMatteo, & King, 2001). Results from this study support this theoretical framework by indicating that the impact of HIV/AIDS on parenting may not be direct, but rather due to increased financial insecurity, parental depression, and child behavior problems. Due to the cumulative risk factors facing families affected by HIV/AIDS, parenting interventions may benefit from additional attention to the impact of poverty, caregiver depression, and child behavior problems (Cohen, Hien, & Batchelder, 2008). For instance, parent management training may need to incorporate cognitive behavioral strategies in order to adequately address parental depression (Tomlinson, 2010). Moreover, in low-resource developing countries, parenting interventions for HIV/AIDS affected families may be more cost effective by targeting the most vulnerable – those in high deprivation areas. Finally, given the complex socioeconomic factors influencing families affected by HIV/AIDS, parenting interventions may be more effective if integrated within a wider network of support services that address financial insecurity and family mental health.
Acknowledgements
This Young Carers study was funded by the Health Economics and HIV and AIDS Research Division (HEARD) at the University of Kwazulu-Natal, the Economic and Social Research Council (UK), the National Research Foundation (SA), the National Department of Social Development (South Africa), the Claude Leon Foundation, and the John Fell Fund. Support to Caroline Kuo for analysis and writing was generously funded by the National Institute for Mental Health Award Number T32 NIMH 078788 (PI: Larry Brown), K01 MH096646-01A1 and L30 MH098313 (PI: Caroline Kuo). We would like to acknowledge the important contribution of our entire Young Carers KwaZulu-Natal research team and our local NGO partner in the rural site, Tholulwazi Uzivikele, to this research. We would also like to thank the children and their families who welcomed us into their homes.
REFERENCES
- Abidin RR. The Determinants of Parenting Behavior. Journal of Clinical Child Psychology. 1992;21(4):407–412. [Google Scholar]
- Andersen P, Telleen S. The relationship between social support and maternal behaviors and attitudes: a meta-analytic review. American Journal of Community Psychology. 1992;20(6) [PubMed] [Google Scholar]
- Antle BJ, Wells LM, Goldie RS, DeMatteo D, King SM. Challenges of parenting for families living with HIV/AIDS. Social Work. 2001;46(2):159–169. doi: 10.1093/sw/46.2.159. [DOI] [PubMed] [Google Scholar]
- Armistead L, Klein K, Forehand R. Parental Physical Illness and Child Functioning. Clinical Psychology Review. 1995;15(5):409–422. [Google Scholar]
- Barber B. Parent-Adolescent relations across cultures: the protective conditions of connection, regulation and psychological autonomy. Presentation to the World Health Organisation, Department of Child and Adolescent Health and Development; Geneva. 2000. [Google Scholar]
- Baron RM, Kenny DA. The Moderator Mediator Variable Distinction in Social Psychological-Research - Conceptual, Strategic, and Statistical Considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Belsky J. The Determinants of Parenting - a Process Model. Child Development. 1984;55(1):83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Bradley RH, Corwyn R. From Parent to Child to Parent…: Paths In and Out of Problem Behavior. Journal of Abnormal Child Psychology. 2012 doi: 10.1007/s10802-012-9692-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley RH, Corwyn RF. Socioeconomic status and child development. Annual Review of Psychology. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Burgoyne RW, Saunders DS. Perceived support in newly registered HIV/AIDS clinic outpatients. AIDS Care. 2000;12(5):643–650. doi: 10.1080/095401200750003815. [DOI] [PubMed] [Google Scholar]
- Casale M, Wild L. The relationship between social support and the health of HIV-positive caregivers of children: A review of the empirical literature. Vulnerable Children and Youth Studies, iFirst Article. 2012:1–23. [Google Scholar]
- Cluver L. Children of the AIDS pandemic. Nature. 2011;474:27–29. doi: 10.1038/474027a. [DOI] [PubMed] [Google Scholar]
- Cluver L, Gardner F, Operario D. Psychological distress amongst AIDS-orphaned children in urban South Africa. Journal of Child Psychology and Psychiatry. 2007;48(8):755–763. doi: 10.1111/j.1469-7610.2007.01757.x. [DOI] [PubMed] [Google Scholar]
- Cluver L, Orkin M, Boyes ME, Gardner F, Meinck F. Transactional sex amongst AIDS-orphaned and AIDS-affected adolescents predicted by abuse and extreme poverty. Journal of Acquired Immune Deficiency Syndromes. 2011 doi: 10.1097/QAI.0b013e31822f0d82. [DOI] [PubMed] [Google Scholar]
- Cohen LR, Hien DA, Batchelder S. The impact of cumulative maternal trauma and diagnosis on parenting behavior. Child Maltreatment. 2008;13(1):27–38. doi: 10.1177/1077559507310045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins D, Leibbrandt M. The financial impact of HIV/AIDS on poor households in South Africa. AIDS. 2007;21(Suppl 7):S75–S81. doi: 10.1097/01.aids.0000300538.28096.1c. [DOI] [PubMed] [Google Scholar]
- Cox MH, Paley B. Families as systems. Annual Review of Psychology. 1997;48:243–267. doi: 10.1146/annurev.psych.48.1.243. [DOI] [PubMed] [Google Scholar]
- Department of Health. 2010 National Antenatal Sentinel HIV & Syphilis Prevalence Survey. Pretoria: 2011. [Google Scholar]
- Dorsey S, Klein K, Forehand R. Parenting self-efficacy of HIV-infected mothers: The role of social support. Journal of Marriage and the Family. 1999;61(2):295–305. [Google Scholar]
- Dunkle K, Jewkes R, Nduna M, Jama N, Levin J, Sikweyiya Y, Koss M. Transactional sex with casual and main partners among young South African men in the rural Eastern Cape: prevalence, predictors, and associations with gender-based violence. Social Science and Medicine. 2007;65(6):1235–1248. doi: 10.1016/j.socscimed.2007.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar F, Waschbusch D, Dadds M, Sigvaldason N. Development and Validation of a Short Form of the Alabama Parenting Questionnaire. Journal of Child and Family Studies. 2007;16(2):243–259. [Google Scholar]
- Erel O, Burman B. Interrelatedness of Marital Relations and Parent-Child Relations - a Metaanalytic Review. Psychological Bulletin. 1995;118(1):108–132. doi: 10.1037/0033-2909.118.1.108. [DOI] [PubMed] [Google Scholar]
- Forehand R, Jones DJ, Kotchick BA, Armistead L, Morse E, Morse PS, Stock M. Noninfected children of HIV-infected mothers: A 4-year longitudinal study of child psychosocial adjustment and parenting. Behavior Therapy. 2002;33(4):579–600. [Google Scholar]
- Frick PJ. Alabama parenting questionnaire. University of Alabama: Author; 1991. [Google Scholar]
- Gardner F. Methodological issues in the use of observational methods for measuring parent child interaction. Clinical Child and Family Psychology Review. 2000;3:185–198. doi: 10.1023/a:1009503409699. [DOI] [PubMed] [Google Scholar]
- Gershoff ET, Aber L, Raver C, Lennon M. Income is Not Enough: Incorporating Material Hardship into Models of Income Associations with Parenting and Child Development. Child Development. 2007;78(1):70–95. doi: 10.1111/j.1467-8624.2007.00986.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies P, Tolley K, Wolstenholme J. Is AIDS a disease of poverty? AIDS Care. 1996;8(3):351–363. doi: 10.1080/09540129650125768. [DOI] [PubMed] [Google Scholar]
- Goodman A, Lamping DL, Ploubidis GB. When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the Strengths and Difficulties Questionnaire (SDQ): data from British parents, teachers and children. [Validation Studies] Journal of Abnormal Child Psychology. 2010;38(8):1179–1191. doi: 10.1007/s10802-010-9434-x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Goodman R, Cluver L, Tshandu V, Vondani P. Xhosa version of the Strengths and Difficulties Questionnaire (Child report and Parent report) London: Institute of Psychiatry; 2004. [Google Scholar]
- Grimes DA, Schulz KF. Descriptive studies: what they can and cannot do. The Lancet. 2002;359(9301):145–149. doi: 10.1016/S0140-6736(02)07373-7. [DOI] [PubMed] [Google Scholar]
- Hosegood V, Vanneste A, Timaeus I. Levels and causes of adult mortality in rural South Africa: the impact of AIDS. AIDS. 2004;5(18):663–671. doi: 10.1097/00002030-200403050-00011. [DOI] [PubMed] [Google Scholar]
- Kahn K, Tollman SM, Garenne M, Gear JSS. Validation and application of verbal autopsies in a rural area of South Africa. Tropical Medicine & International Health. 2000;5(11):824–831. doi: 10.1046/j.1365-3156.2000.00638.x. [DOI] [PubMed] [Google Scholar]
- Kuo C, Operario D. Health of adults caring for orphaned children in an HIV-endemic community in South Africa. AIDS Care. 2011:1–8. doi: 10.1080/09540121.2011.554527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo C, Operario D, Cluver L. Depression among carers of AIDS-orphaned and other-orphaned children in Umlazi Township, South Africa. Global Public Health. 2012;7(3):253–269. doi: 10.1080/17441692.2011.626436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y. Early motherhood and harsh parenting: The role of human, social, and cultural capital. Child Abuse & Neglect. 2009;33(9):625–637. doi: 10.1016/j.chiabu.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Levendosky AA, Leahy KL, Bogat GA, Davidson WS, von Eye A. Domestic violence, maternal parenting, maternal mental health, and infant externalizing behavior. Journal of Family Psychology. 2006;20(4):544–552. doi: 10.1037/0893-3200.20.4.544. [DOI] [PubMed] [Google Scholar]
- Lopman B, Barnabas R, Boerma T, Chawira J, Gaitskell K, Harrop T, Gregson S. Creating and Validating an Algorithm to Measure AIDS Mortality in the Adult Population using Verbal Autopsy. Public Library of Science Medicine. 2006;3(8):1273–1281. doi: 10.1371/journal.pmed.0030312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Maccoby EE. The Role of Parents in the Socialization of Children - an Historical Overview. Developmental Psychology. 1992;28(6):1006–1017. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [Comparative Study, Research Support, U.S. Government, P.H. S.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mboya MM. Variations in Parenting Practices - Gender-Related and Age-Related Differences in African Adolescents. Adolescence. 1995;30(120):955–962. [PubMed] [Google Scholar]
- McLeod BD, Wood JJ, Weisz JR. Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review. 2007;27(2):155–172. doi: 10.1016/j.cpr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Armistead L, Herbeck DM, Payne DL. Anxiety/stress among mothers living with HIV: effects on parenting skills and child outcomes. AIDS Care. 2010;22(12):1449–1458. doi: 10.1080/09540121.2010.487085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Herbeck DM, Payne DL. Family routines and parental monitoring as protective factors among early and middle adolescents affected by maternal HIV/AIDS. Child Development. 2009;80(6):1676–1691. doi: 10.1111/j.1467-8624.2009.01361.x. [Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oburu PO, Palmerus K. Parenting stress and self-reported discipline strategies of Kenyan caregiving grandmothers. International Journal of Behavioral Development. 2003;27(6):505–512. [Google Scholar]
- Osborn J. Notes on the use of data transformation. Practical Assessment, Research, and Evaluation. 2002;8(6) [Google Scholar]
- Pardini DA. Novel insights into longstanding theories of bidirectional parent-child influences: Introduction to the special section. Journal of Abnormal Child Psychology. 2008;36(5):627–631. doi: 10.1007/s10802-008-9231-y. [DOI] [PubMed] [Google Scholar]
- Peltzer K, Matseke G, Mzolo T, Majaja M. Determinants of knowledge of HIV status in South Africa: results from a population-based HIV survey. BMC Public Health. 2009;9(1):174. doi: 10.1186/1471-2458-9-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillay U, Roberts B, Rule S, editors. South African social attitudes: changing times, diverse voices. Cape Town: HSRC Press; 2006. [Google Scholar]
- Potterton J, Stewart A, Cooper P. Parenting stress of caregivers of young children who are HIV Positive. African Journal of Psychiatry. 2007;10(4):210–214. doi: 10.4314/ajpsy.v10i4.30257. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behaviour Research Methods. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Pretorius T. Cross-cultural application of the Centre for Epidemiological Studies Depression Scale: A study of Black South African students. Psychological Reports. 1991;69:1179–1185. doi: 10.2466/pr0.1991.69.3f.1179. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D Scale: a self-report symptom scale to detect depression in a community sample. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Raikes HA, Thompson RA. Efficacy and social support as predictors of parenting stress among families in poverty. Infant Mental Health Journal. 2005;26(3):177–190. doi: 10.1002/imhj.20044. [DOI] [PubMed] [Google Scholar]
- Reid JB, Patterson GR. The Development of Antisocial-Behavior Patterns in Childhood and Adolescence. European Journal of Personality. 1989;3(2):107–119. [Google Scholar]
- Richter L, Beyrer C, Kippax S, Heidari S. Visioning services for children affected by HIV and AIDS through a family lens. Journal of the International AIDS Society. 2010;13(Suppl 2):I1. doi: 10.1186/1758-2652-13-S2-I1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter L, Sherr L, Adato M, Belsey M, Chandan U, Desmond C, Wakhweya A. Strengthening families to support children affected by HIV and AIDS. AIDS Care. 2009;21:3–12. doi: 10.1080/09540120902923121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter LM, Naicker S. A Review of Published Literature on Supporting and Strengthening Child-Caregiver Relationships (Parenting) Arlington, VA: USAID's; 2013. AIDS Support and Technical Assistance Resources, AIDSTAR-One, Task Order 1. [Google Scholar]
- Robert CJ. Parenting Practices and Child Behavior in Mexico: A Validation Study of the Alabama Parenting Questionnaire. Minnesota, Minneapolis: 2009. (Doctor of Philosophy) [Google Scholar]
- Rochat T, Bland R, Coovadia H, Stein A, Newell M. Towards a family-centred approach to HIV treatment and care for HIV-exposed children, their mothers and their families in poorly resourced settings. Future Virology. 2011;6(6):687–696. doi: 10.2217/fvl.11.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus M, Flannery D, Rice E, Lester P. Families living with HIV. AIDS Care. 2005;17(8):978–987. doi: 10.1080/09540120500101690. [DOI] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. J Couns Psychol. 2010;57(1):1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Sherbourne C, Stewart A. The Medical Outcomes Survey (MOS) social support survey. Social Science and Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Sipsma H, Eloff I, Makin J, Finestone M, Ebersohn L, Visser MJ, Forsyth B. Behavior and psychological functioning of young children of HIV-positive mothers in South Africa. AIDS Care. 2013;25(6):721–725. doi: 10.1080/09540121.2013.779627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics South Africa. Census 2001: Household Questionnaire. Pretoria: Statistics SA; 2001. [Google Scholar]
- Stoker DJ. The 1985 sample census in the Transkei Republic. Southern African Journal of Demography/Suidelike Afrikaanse Tydskrif vir Demografie. 1987;1(1):26–31. [PubMed] [Google Scholar]
- Tomlinson M. Family-centred HIV interventions: lessons from the field of parental depression. Journal of the International AIDS Society. 2010;13(Suppl 2):S9. doi: 10.1186/1758-2652-13-S2-S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Maternal depression and its relationship to life stress, perceptions of child behavior problems, parenting behaviors, and child conduct problems. Journal of Abnormal Child Psychology. 1988;16(3):299–315. doi: 10.1007/BF00913802. [Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- WHO. WHO case definition of AIDS surveillance in adults and adolescents. Weekly Epidemiological Record. 1994;69:273–275. [PubMed] [Google Scholar]
- Wright G. Findings from the Indicators of Poverty and Social Exclusion Project: A Profile of Poverty using the Socially Perceived Necessities Approach. Pretoria: Department of Social Development, Republic of South Africa; 2008. Key Report 7. [Google Scholar]