Abstract
Introduction
Health care reimbursement is increasingly based on quality. Little is known about how clinic-level patient characteristics affect quality performance, particularly in community health centers (CHCs).
Methods
Using electronic health record data for 4,019 diabetic patients from 23 CHC primary care clinics in the OCHIN practice-based research network, we calculated correlations between a clinic’s patient panel characteristics and delivery rates of diabetes preventive services in 2007. Using regression models, we estimated the proportion of clinic variability in clinics’ preventive services rates associated with the variability in the clinics’ patient panel characteristics. We also explored whether clinics’ performance rates were affected by how patient panel denominators were defined.
Results
Clinic rates of glycosylated hemoglobin testing, influenza immunizations, and lipid screening were positively associated with the percentage of patients with continuous health insurance coverage, and negatively associated with the percentage uninsured. Microalbumin screening rates were positively associated with the percentage of racial minorities in a clinic’s panel. Associations remained consistent with different panel denominators.
Conclusions
Clinic variability in delivery rates of preventive services correlates with differences in clinics’ patient panel characteristics, particularly the percentage of patients with continuous insurance coverage. Quality scores that do not account for these differences could create disincentives to diabetes care for vulnerable patients.
INTRODUCTION
Health care service reimbursements to providers are increasingly based on value1-5; for example, “pay-for-performance” is a payment mechanism proposed to incentivize the consistent delivery of high quality services.6,7 The premise underlying most such programs is to reward health care providers for delivering high quality care, and to provide regular feedback on adherence to performance standards.8,9
The metrics currently used to measure care quality rarely account for patient panel characteristics that might impact clinics’ quality performance.10-12 This is concerning, because a growing literature shows an association between the characteristics of clinics’ and providers’ patient panels and the quality of care provided to these panels.11,13-20 Much of the focus of this literature has been on the relationship between care quality and patients’ co-morbidity and disease severity characteristics, rather than their socio-demographic factors (i.e., race/ethnicity, income, insurance coverage status), despite the known relationship between such characteristics and care quality at the individual patient level.21,22 Further, little is known about which clinic-level patient panel characteristics are most strongly associated with variation in clinics’ rates of delivery of primary care services - information that may be especially pertinent for community health centers (CHCs) and others providing care to underserved populations (e.g., the uninsured and racial/ethnic minorities). While CHCs generally provide health care comparable in quality to that provided by private practices23-26, care quality and patient demographics may vary between individual CHCs.27,28
Practice-based Research Networks (PBRNs), composed of multiple clinics, provide a unique opportunity to further our understanding of which patient panel characteristics are most associated with a clinic’s performance profile. This is especially true if the clinics within the network PBRN share a common electronic health record (EHR). Linked EHR data also makes it possible to examine the extent to which a clinic’s quality measurements are affected when only patients seen primarily at that clinic are included in its ‘panel’ denominator, versus when all patients seen at the clinic are in the denominator. This question will become increasingly important as methods for measuring quality shift from manual chart reviews to the assessment of EHR data, which will make it possible to see which patients are being seen at multiple primary care clinics versus those utilizing only one clinic.
We hypothesized that, within our study CHCs, performance variation would be correlated with differences in characteristics of the clinics’ patient populations, and that a significant proportion of the clinic-level variability in rates of delivery of preventive services could be explained by the clinic level summaries of their patient panels’ socio-demographic characteristics. To test this hypothesis, we examined variability in rates of delivery of diabetes preventive services among the CHC primary care clinics that are members of the OCHIN PBRN, and share a linked EHR. We assessed the degree to which certain clinic-level patient panel characteristics (e.g. the percent of patients’ income and insurance coverage status categories) were correlated with clinic performance. Our objectives were to: 1) describe differences in clinic patient panels and rates of delivery of recommended diabetes care among 23 CHC primary care clinics in the OCHIN network, and 2) assess associations between clinic-level patient characteristics and variability in clinic rates of providing recommended diabetes preventive care services. Last, we sought to 3) assess the impact of using different methods to quantify the patient panel denominators by adjusting panel denominators to assign a patient to only one clinic (the clinic which the patient visited most often), or to all clinics utilized by that patient.
METHODS
Data Sources—EHR and Medicaid Insurance Enrollment Data
In 2001, a group of safety net organizations in Oregon collectively purchased the Epic EHR system and created the Oregon Community Health Information Network (OCHIN). This network provides health information technology (HIT) support to member CHCs, including a centrally hosted and maintained EHR. (This network has grown beyond Oregon and is now referred to as “OCHIN” with members from 13 states). OCHIN’s shared EHR and fully integrated electronic health information exchange allows each patient to have a single medical record shared across every clinic in the network.29 As most of the OCHIN PBRN’s member clinics are federally-qualified health centers (FQHCs), they are required to collect comprehensive information on patient demographics and insurance coverage, in addition to the clinical information commonly found information in EHRs, such as patient medical history and receipt of services and procedures.
FQHCs care for many of the nation’s most vulnerable populations, including uninsured patients. In this study, the OCHIN clinics’ shared EHR facilitated examination of quality metrics at the patient, clinic, and population levels.29 As most of the study CHCs were in Oregon, we also linked patient-level data on Medicaid insurance enrollment in Oregon, to supplement the EHR records on patients’ Medicaid coverage in 2007.
Study Population
The study population included adults (at least 19 years of age as of December 31, 2004) with diabetes mellitus who were seen at a CHC primary care clinic that had implemented OCHIN’s EHR by 2005. Within this population, we required patients to have at least two visits associated with an ICD-9 code for diabetes mellitus (type 1 or 2) in 2004-2005, and at least one primary care visit at a given clinic in both 2006 and 2007, to be considered part of a clinic’s ‘continuity panel.’ In the 48 CHC clinics with OCHIN EHR data available for the study period, 4,188 patients met these requirements. To enable clinic-level evaluations and avoid unstable estimates of preventive services rates, we further limited the analyses to primary care clinics with at least 50 diabetic patients meeting our continuity criteria (n=23 clinics in two states and 4,019 patients). We found that 417 of these 4,019 patients (11% of the population) met the continuity criteria for two clinics, and an additional eight patients met the criteria for three clinics. Thus, we used two approaches to defining clinic patient panels: (1) “restricted” panels limited each patient to a single clinic’s panel, and (2) “full” panels allowed the 425 patients who had multiple visits at two or more clinics to be included in the panel denominator for all clinics for which they met continuity criteria.
Clinic Patient Panel Characteristics
We described clinic panels according to several socio-demographic characteristics of their patients, including patient age, race, primary language, mean percent of federal poverty level (% FPL) in 2007, percent of patients with continuous insurance coverage in 2007, and percent of patients with no insurance coverage in 2007. As most clinics in the OCHIN PBRN are within FQHCs, information on patients’ income as a percentage of the FPL is reported at each visit. If more than one income level was reported for a patient in 2007, we used this information to estimate the mean % FPL for 2007 based by a weighted average of each patient’s reported % FPL, accounting for the amount of time between the reported FPLs. Percent of time patient had insurance coverage in 2007 was determined by start and stop dates of insurance coverage, as recorded in the EHR and supplemented by Oregon’s Medicaid insurance enrollment data for Oregon patients with public coverage in 2007.
Clinic Rate of Delivery of Diabetes Preventive Care Services
We assessed four evidence-based diabetes preventive care services: lipid (LDL-low density lipoprotein) screening, influenza vaccination, nephropathy screening (urine microalbumin), and glycosylated hemoglobin (HbA1c) monitoring. It is generally recommended that patients with diabetes mellitus receive each of these services at least annually.30 We used OCHIN EHR data to identify procedure codes that confirmed delivery of each service at least once in 2007.
Statistical Analyses
We described differences in clinic-level patient panels, and in rates of delivery of the four diabetes preventive services to clinics’ patient panels. We then calculated Spearman rank correlations to examine the strength of associations between clinic-level patient panel characteristics and percentage of patients provided the recommended services at each clinic. Linear regressions of quality metrics, modeled as continuous variables, were used to determine the proportions of variability in clinic performance metrics that were associated with variability in the patient panel socio-demographic characteristics. The increase in the proportion of variability accounted for by the models was determined by the change in the model r2 in stepwise additions of patient characteristics to the model. The order of addition of patient characteristics was determined using a maximum r2 criteria. Because rates of service delivery must fall between 0 and 100%, quality metrics were logit transformed prior to linear regression analysis. a
To explore whether clinic performance was affected by how the patient denominator was defined, we compared the association between patient characteristics and service delivery in both “full” clinic panels (including patients in the panel denominators of multiple clinics, if they met continuity criteria at each of those clinics) and in “restricted” clinic panels (limiting patients to the panel of the clinic which they attended most often; if attending two clinics equally often, we assigned them to the one they attended most recently).
This study was approved by the Institutional Review Board at our academic health center.
RESULTS
Clinic and Clinic Patient Panel Characteristics
There were 19 CHC primary care clinics geographically spread throughout the state of Oregon in both urban and rural settings, and four clinics in California. All but three of the study clinics were FQHCs. Among the 4,019 patients who met the study inclusion criteria, the mean number of diabetic patients per clinic in 2007 was 188 (range 59 - 379) for the full panels, and 173 (range 30 - 378) for the restricted panels (limiting the patients to one clinic resulted in less than 50 patients per clinic in some of the restricted panels). The clinics’ patient panel characteristics varied considerably (Table 1). For example, percent of clinic patients whose primary language was Spanish ranged from 0% to 87.4% in both the full panels (median 28.3%) and restricted patient panels (median 27.6%). Percent of clinic patients who were continuously uninsured in 2007 ranged from 1% to over 50% (full panel range: 1–57%, median 30.0%); restricted panel range: 2–56%, median 30.0%). Percent of clinic patients who were continuously insured ranged from 34% to 99% in the full panels (34%- 98% in the restricted panels).
Table 1.
Variability in patient panel characteristics
| Patients (n=4,019) | Clinic Panel Summary (n=23 clinics) | ||||
|---|---|---|---|---|---|
| Full Panels* | Restricted Panels† | ||||
| Patient Characteristics | Mean (SD) | Median (Range) | Mean (SD) | Median (Range) | |
| Patient Age | 55.8 (12.9) | 53.7 (2.9) | 53.9 (48.3 - 59.0) | 53.8 (3.1) | 53.7 (48.1 – 60.1) |
| Percent Minority‡ | 11.1% | 22.0 (19.8) | 16.0 (2.0 – 76.0) | 21.9 (19.6) | 16.0 (2.0 – 76.0) |
| Percent English-speaking | 58.8% | 60.6 (22.9) | 58.9 (12.6 – 100) | 61.7 (22.2) | 58.8 (12.6 – 100) |
| Percent Spanish-speaking | 32.1% | 33.2 (23.1) | 28.3 (0 – 87.4) | 32.0 (22.2) | 27.6 (0 – 87.4) |
| Percent with No Insurance | 28.6% | 28.6 (19.0) | 30.0 (1.0 – 57.0) | 28.5 (18.3) | 30.0 (2.0 – 56.0) |
| Percent with Continuous Insurance | 66.2% | 66.4 (21.1) | 63.0 (34.0 – 99.0) | 66.3 (20.6) | 64.0 (34.0 – 98.0) |
| Percent with Income <50% of FPL | 29.4% | 36.9 (19.7) | 31.0 (10.0 – 87.0) | 29.6 (13.7) | 31.0 (6.0 – 66.3) |
NOTE. FPL: Federal poverty level
This includes all diabetic patients meeting inclusion criteria of at least 1 visit in 2006 and 2007; 425 patients included in multiple clinic panels.
Each patient assigned to only one clinic denominator.
Any patient with a race other than “White.” This includes Black, Asian, Native American, Pacific Islander, Non-Caucasian, and “Other race.”
Variability in Patient Panels
Rates of delivery of diabetic preventive services also varied by clinic (Figure 1). In the full patient panels, the median rates of delivery of specific services were 68% for LDL (M = 57.3, SD = 29.7), 46% for influenza vaccination (M = 42.8, SD = 15.6), 23% for microalbumin (M = 33.6, SD = 23.6), and 83% for HbA1c screening (M = 74.5, SD = 23.6). The width of the inter-quartile range of rates of delivery of preventive services varied by service, with a fairly narrow range for delivery of influenza vaccination and HbA1c, and a much wider range for delivery of LDL and nephropathy screening. Little difference was seen in the evaluation of clinics’ performance by restricted versus full panels.
Figure 1. Variability in clinic-level percent of patients provided diabetes preventive services, full versus restricted patient panels.
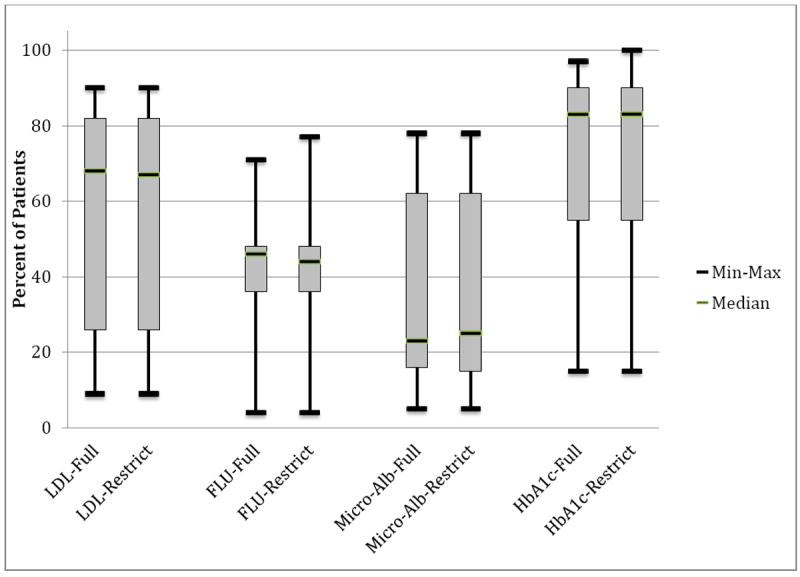
LDL: Low-density lipoprotein cholesterol screening; FLU: influenza vaccination; Micro-Alb: urine microalbumin screening; HbA1c: hemoglobin A1c monitoring
Clinic Patient Panel Characteristics and Rates of Diabetes Preventive Services
Table 2 displays the Spearman rank correlations between clinic patient panel characteristics and rates of diabetes preventive services. In both the full and restricted patient panel models, several panel characteristics correlated significantly with performance rates. Mean age of clinic patients was positively correlated with percent of patients provided influenza vaccinations and HbA1c testing, and percent of patients with no insurance in 2007 was negatively correlated with rates of HbA1c testing, LDL screening, and influenza vaccination. Conversely, clinic delivery of these three services was positively correlated with percent of clinic patients who were continuously insured in 2007. Percent of clinic patients with income <50% FPL was positively correlated with rates of influenza vaccination. Primary language of clinic patients was not correlated with delivery rates of any of the services. Rates of microalbumin screening were positively correlated with percent of minority (non-white) patients (which could be due to higher prevalence of diabetic nephropathy among non-Caucasians)31,32 and were not correlated with other clinic-level patient characteristics measured. The patterns of correlations were similar in the restricted model; only the correlation between rates of HbA1c testing and average patient age lost significance in the restricted models.
Table 2.
Correlations between clinic-level percent of patients provided diabetes preventive services and clinic-level patient panel characteristics
| Correlation of Clinic-Level Patient Panel Characteristic with Delivery of Diabetic Preventive Services | ||||||||
|---|---|---|---|---|---|---|---|---|
| Full Patient Panel† (Spearman Rank Correlation Coefficients) | Restricted Patient Panel‡ (Spearman Rank Correlation Coefficients) | |||||||
| Clinic Patient Panel Characteristic | LDL | FLU | Micro-Alb | HbA1c | LDL | FLU | Micro-Alb | HbA1c |
| Mean Age | 0.40 | 0.48* | 0.14 | 0.42* | 0.38 | 0.48* | 0.21 | 0.37 |
| Percent Minority§ | 0.22 | 0.15 | 0.73* | 0.21 | 0.22 | 0.22 | 0.68* | 0.24 |
| Percent English speaking | 0.11 | -0.15 | 0.05 | 0.08 | 0.19 | -0.16 | 0.05 | 0.11 |
| Percent Spanish speaking | -0.11 | 0.07 | -0.37 | 0.03 | -0.16 | 0.04 | -0.31 | 0.02 |
| Percent with No Insurance | -0.45* | -0.61* | -0.03 | -0.54* | -0.44* | -0.52* | -0.11 | -0.48* |
| Percent with Continuous Insurance | 0.46* | 0.60* | 0.04 | 0.55* | 0.45* | 0.53* | 0.08 | 0.48* |
| Percent with Income <50% of FPL | -0.01 | 0.45* | -0.17 | 0.13 | -0.03 | 0.41* | -0.11 | 0.10 |
NOTE. LDL: Low-density lipoprotein cholesterol screening; FLU: influenza vaccination; Micro-Alb: urine microalbumin screening; HbA1c: hemoglobin A1c monitoring; FDL: Federal Poverty Level.
p<0.05
This includes all diabetic patients meeting inclusion criteria of at least 1 visit in 2006 and 2007; 425 patients included in multiple clinic panels.
Each patient assigned to only one clinic denominator.
Any patient with a race other than “White.” This includes Black, Asian, Native American, Pacific Islander, Non-Caucasian, and “Other race.”
The proportions of clinic variability in delivery of diabetic services associated with variation in clinic patient panel characteristics are shown in Table 3 and illustrated in Figure 2. Of the patient panel characteristics included in this analysis, the percentage of clinic patients with continuous insurance coverage accounted for the largest proportion of clinic variance in LDL screening, HbA1c assessment, and flu immunization rates: it accounted for over 25% of the clinic variance in both LDL screening and HbA1c assessment rates in the full patient panels, and for 18% of the variance in rates of flu immunizations. Although percent of patients with no insurance coverage and mean patient age also accounted for a significant proportion of clinic variance in service rates, both were highly correlated with percent of patients with full insurance coverage (r=0.82 for mean age and -0.99 for patients with no insurance coverage in the full panels). Neither variable significantly increased the model fit if included in a regression with the percent of patients with full insurance coverage.
Table 3.
Proportion of variability in clinic-level percent of patients provided diabetes preventive services accounted for by clinic-level patient panel characteristics
| Proportion of variability accounted for by clinic-level patient panel characteristics (unadjusted) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model r2 | Full Patient Panel† | Restricted Patient Panel‡ | ||||||
| Clinic Patient Panel Characteristic | LDL | FLU | Micro-Alb | HbA1c | LDL | FLU | Micro-Alb | HbA1c |
| Mean Age | 0.21* | 0.12 | 0.01 | 0.20* | 0.22* | 0.16 | 0.02 | 0.30* |
| Percent Minority§ | 0.12 | 0.06 | 0.55* | 0.08 | 0.12 | 0.06 | 0.51* | 0.02 |
| Percent English speaking | 0.02 | 0.10 | 0.01 | 0.01 | 0.04 | 0.06 | 0.01 | 0.02 |
| Percent Spanish speaking | 0.03 | 0.03 | 0.08 | <0.01 | 0.06 | 0.01 | 0.08 | 0.01 |
| Percent with No Insurance | 0.25* | 0.18* | <0.01 | 0.29* | 0.25* | 0.18* | <0.01 | 0.25* |
| Percent with Continuous Insurance | 0.26* | 0.18* | <0.01 | 0.31* | 0.25* | 0.18* | <0.01 | 0.28* |
| Percent with Income <50% of FPL | 0.04 | 0.15 | 0.02 | 0.06 | 0.03 | 0.15 | 0.01 | 0.08 |
| Change in proportion of variability accounted for by clinic-level diabetes patient panel characteristics (after controlling for % patients continuously insured)3 | ||||||||
| Change in model r2∥ | LDL | FLU | Micro-Alb | HbA1c | LDL | FLU | Micro-Alb | HbA1c |
| Mean Age | 0.01 | <0.01 | 0.02 | <0.01 | 0.02 | 0.02 | 0.03 | 0.05 |
| Percent Minority§ | 0.13* | 0.07 | 0.55* | 0.10 | 0.12 | 0.06 | 0.48* | 0.02 |
| Percent English speaking | 0.01 | 0.07 | 0.01 | <0.01 | 0.01 | 0.11 | 0.01 | <0.01 |
| Percent Spanish speaking | 0.01 | 0.08 | 0.09 | 0.01 | 0.01 | 0.07 | 0.05 | 0.02 |
| Percent with Average Income <50% of FPL | 0.02 | 0.03 | 0.03 | 0.02 | 0.02 | 0.02 | <0.01 | 0.03 |
NOTE. LDL: Low-density lipoprotein cholesterol screening; FLU: influenza vaccination; Micro-Alb: urine microalbumin screening; HbA1c: hemoglobin A1c monitoring; FDL: Federal Poverty Level. Values were estimated using regression models of the logit transformation of % Panel receiving service on the panel characteristic.
p<0.05
This includes all diabetic patients meeting inclusion criteria of at least 1 visit in 2006 and 2007; 425 patients were included in multiple clinic panels.
Each patient assigned to only one clinic denominator.
Any patient with a race other than “White.” This includes Black, Asian, Native American, Pacific Islander, Non-Caucasian, and “Other race.”
The difference between the r2 of a model containing the listed patient characteristic and the % of patients with continuous insurance and the r2 of a model containing only the % of patients with continuous coverage. Changes in r2 were not reported for % patients with no insurance because of the high correlation of the measure with % continuously insured.
Figure 2. Proportion of variability in clinic-level percent of patients provided diabetes preventive services accounted for by clinic-level patient panel characteristics.
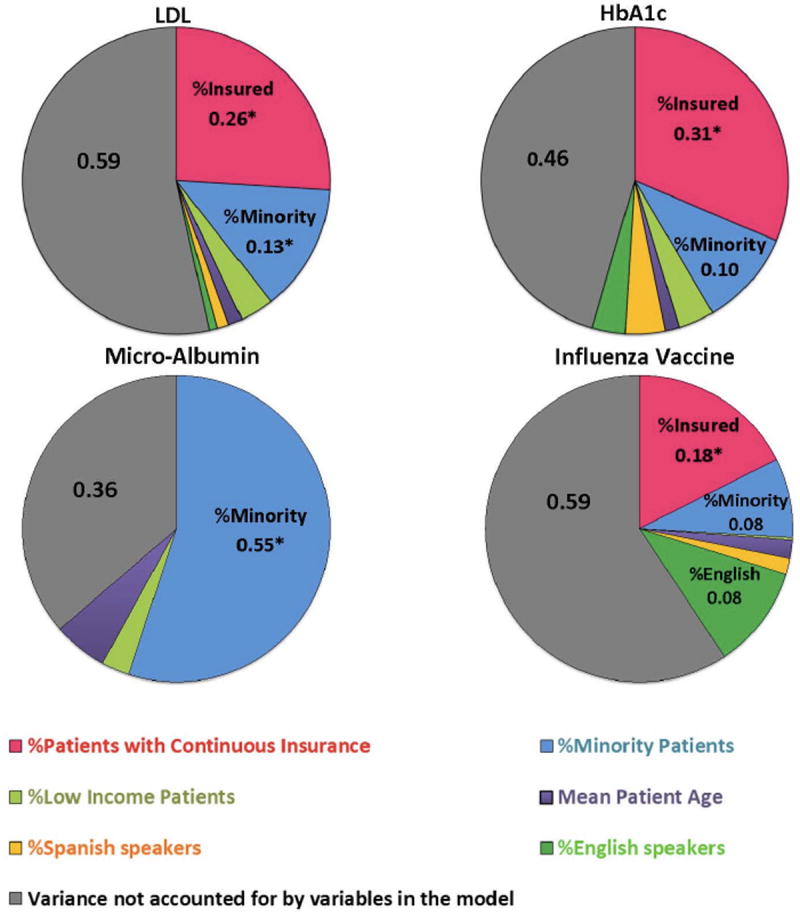
Note. The percent variability associated with Clinic Patient Panel characteristics was determined from the change in r2 when the variable was added to a model already containing the variables with stronger association with delivery of the service. The variable order was determined through stepwise selection based on the variable addition resulting in the maximum change in r2. The proportion of clinic variability in delivery of a service that is not explained by a model including all patient characteristics in this study is shown in gray.
*p<0.05.
Neither percent of the clinic patient panel who were English- or Spanish-speaking, nor percent with an average income level <50% FPL, accounted for a significant proportion of variability in clinic delivery of diabetic services. Minority status did not account for a significant portion of the variability in the rates of LDL screening, HbA1c assessments, or flu immunization, but it accounted for 55% of the variability in microalbumin assessment rates. The positive association between the percent of racial minorities and rates of LDL and microalbumin assessments were the only associations with significant semi-partial correlations when we also adjusted for the percent of patients with continuous insurance coverage.
To view the associations described in Table 3 in a different modality, Figure 3 shows the observed clinic rates of LDL and HbA1c tests superimposed on the rates predicted from the linear regression of clinic rates of the preventive service on the percent of continuously insured patients in the clinic’s patient panel. As shown, a clustering of clinics falls within the 95% confidence interval predicted by the percentage of patients in their panels with full insurance coverage. Many other clinics fall close to these predicted preventive service rates; there are few outliers.
Figure 3. Observed rates of diabetes preventive services by clinic, as compared to rates predicted by the percentage of each clinic’s patient panel with full insurance coverage.
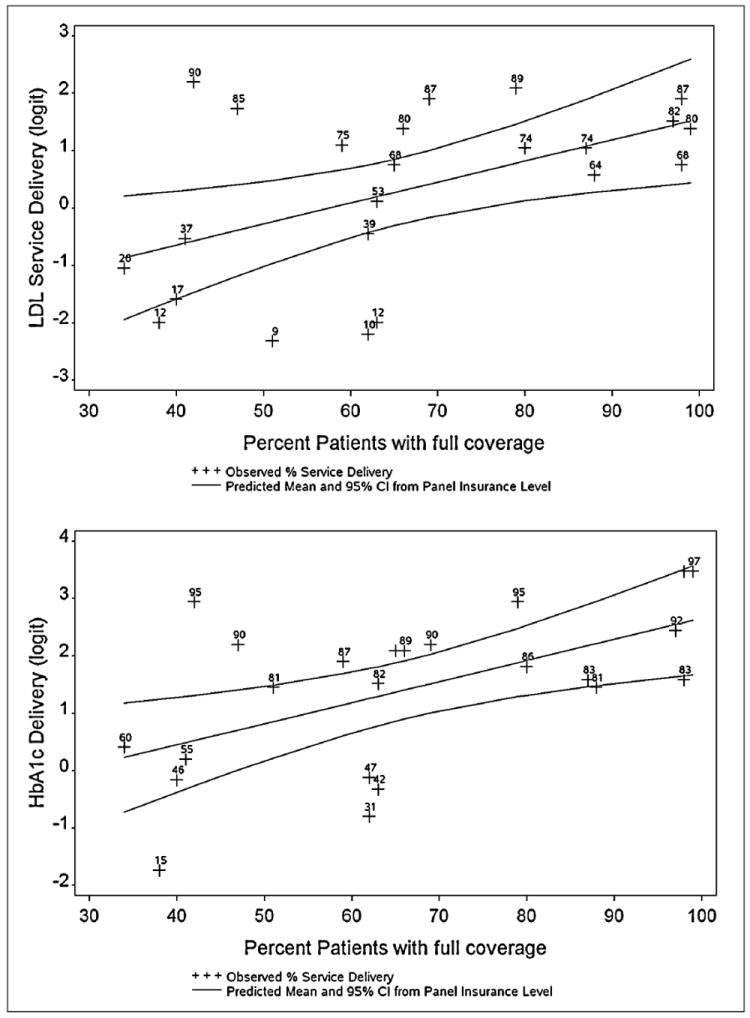
Note. Predicted values and 95% confidence intervals were estimated from regression models of delivery of preventive service rates on the percent of patient panel with full insurance coverage. The model used logit transformed rates to keep the predicted rates bounded between 0 and 100%. Graphed values are the logit transformed values (y axis) of observed values labeled with the actual rates (%) to facilitate interpretation.
DISCUSSION
Variability in clinics’ rates of delivery of diabetes preventive services across the 23 study clinics was highly correlated with certain clinic-level patient panel characteristics. The strongest association was between rates of insurance coverage (or lack of coverage) in a clinic’s patient panel, and the clinic’s rates of delivering recommended care; the higher the percentage of a clinic’s patient panel continuously insured, the higher the clinic’s performance. This confirms and expands upon previous findings of an association between insurance coverage and rates of diabetes care at the individual patient level, by demonstrating this association at the clinic level.21,33,34
One possible explanation for this finding may be that even if services are ordered or recommended by clinicians, uninsured patients are more likely to forego or delay the service due to cost.35,36 If this is true, a clinic’s quality score may be less reflective of how consistently services were recommended, and more reflective of how likely it is that their patients can afford to access the recommended services. While our PBRN clinicians have reported this phenomenon anecdotally on several occasions, confirming this qualitatively was beyond the scope of this paper. Another possible explanation may be that clinicians were less likely to order recommended tests that would cost uninsured patients money out-of-pocket, compared to recommending care for insured patients. Previous studies have shown that clinicians do consider a patient’s insurance status when recommending care.37
Notably, we found few differences in clinic performance rates when a patient was assigned to only one clinic (restricted panel) compared to when a patient was included in more than one clinic’s denominator (full panel). This finding is relevant to discussions about how to define a clinic’s patient panel denominator for quality assessments and payment based on population health indicators. For example, a recent study reported on the complexity of defining clinic patient panels to enable them to generate quality reports based on an accurate denominator within a medical home setting.38
Implications for Practice and Policy
Our findings caution against the common practice of comparing clinics’ care quality performances without accounting for differences in their patient panel characteristics. The significant correlation between care quality and clinic patients’ insurance coverage suggests that insurance disparities may, at least in part, explain clinic quality differences, especially those measured using some of the current quality metrics. These findings further suggest that CHCs and other safety net providers may be constrained in their ability to improve performance quality until meaningful insurance coverage expansions are achieved and sustained in the United States. At the very least, it will be important that patients stay continuously covered.34,39,40 There is movement in this direction at the policy level as many states expand insurance coverage options and support through the implementation of the Affordable Care Act; however, it is too soon to know whether these efforts will translate into meaningful reform.
Our results also indicate the potential for unintended consequences of policies that incentivize clinics to improve quality without accounting for vulnerabilities in their patient panels. Many primary care practices already limit the number of uninsured patients on their panels due to financial constraints; unadjusted quality measurement policies could lead to further limitations of this kind, thus exacerbating the access problems already faced by vulnerable populations. As cautioned by others, clinic payment models that incentivize quality improvements must not dissuade providers from caring for vulnerable patients, or penalize clinics if services were not offered or performed due to lack of insurance or a patient’s inability to pay.41,42 As demonstrated in Figure 3, several of the study clinics’ performance assessments would be markedly improved by adequately adjusting for their patient panel characteristics. Although this is a simple model based on a single characteristic and a small number of clinics, adjusting for the clinic’s patient panel insurance coverage level shifted the quality ranking of four of the clinics to a higher quartile. This illustrates the potential impact of unadjusted quality indicators on the assessment of clinic performance.
Future Research Needs
Research is needed to further investigate the observed variability in clinics’ performance measures to better understand its underlying causes. Nevertheless, these results indicate the need for caution when comparing quality across diverse clinic sites without accounting for differences in patient panel characteristics. If reimbursement levels are based on such unadjusted metrics, it may damage an already fragile safety net and reduce vulnerable populations’ access to health care. There is an urgent need to develop and validate an evidence-based formula enabling “vulnerability adjustment” of clinic quality scores. As shown in Figure 2, continuous insurance coverage accounted for 18 to 31% of the variance in delivery rates for three of the four diabetes preventive services assessed; full adjustment likely would need to account for factors that influence patient care beyond insurance coverage and the other factors assessed here.
Another phenomenon that deserves further study is that of patients utilizing services in multiple clinics. Over 10% of the patients in our study made repeat visits to more than one clinic during the study period. Although our two methods of assigning patients to clinic panels (restricted vs. full) did not affect the clinics’ quality measures, further investigation would inform the development of prospective payment mechanisms and quality metrics based on accurately defined clinic populations. For example, if a patient goes to multiple clinics, which clinic should get a prospective global payment for care of that patient? Should multiple clinics be able to claim a patient on their panels? How can the primary clinic capture information on patient services provided at other sites, to more accurately report and not duplicate services?
PBRNs are ideally suited to address these research and practice-based needs, as they can generate information about the provision of services across clinics. Further, research involving multiple practices with diverse patient populations could be conducted in a network of PBRNs, such as those recently funded by the Agency for Research and Quality through the P30 Research Center in Primary Care Practice Based Research and Learning mechanism. This research will provide an unprecedented opportunity to assess the factors associated with service delivery in primary care settings across the United States.
Limitations
We used the most common codes for identifying diabetes preventive services, and may have missed some services; however, our analyses from other studies in this population suggest a low rate of missed services.43 We also might have missed services received outside of the OCHIN member clinics; however, our inclusion criteria ensured a minimum level of continuity of care at these clinics. Patients were identified as having diabetes if they had at least two visits associated with a diabetes diagnostic code, to avoid incorrectly identifying patients as diabetic based on a single visit. This likely resulted in missing some patients who had only one visit associated with a diabetes diagnosis during the study period. Thus, our results provide conservative estimates of study clinics’ diabetic population and delivery of preventive care.
Similarly, we had insurance continuity data available for all patients in the EHR, supplemented by Medicaid enrollment data for most patients, which may have resulted in conservative estimates of insurance coverage for some of the patients. In addition, we included only 23 primary care CHCs, limiting the generalizability of the observed association. The primary insurance sources for the patients at these clinics are Medicare and Medicaid; insurance coverage may have a different association in patient populations with higher coverage by private insurance carriers. We assessed only those patient factors available in the EHR data; these do not represent all factors that contribute to a patient’s health, and/or to a clinic’s ability to deliver high quality care. We recommend the development of policies that move towards the systematic collection of a more comprehensive set of patient factors in EHRs, including additional characteristics related to social determinants of health. Finally, we were unable to assess whether clinic variation in rates of diabetes care services was a result of clinic providers not offering the services, or because of patients’ refusal.
Conclusion
Significant variability in quality rates may be associated with differences in clinics’ patient panels. Quality measures need to acknowledge these differences and put mechanisms in place to account for them or risk creating disincentives for clinics to care for vulnerable patients.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the OCHIN practice-based research network health centers.
Funding: This study was supported by grant no. R01HL107647 from the National Heart, Lung, and Blood Institute.
Footnotes
Logit transformations (the log of proportion of patients with delivered services/(1- proportion patients with delivered services), the link function used in logistic regressions) were utilized to keep the predicted values from the regressions bounded between 0 and 1 and to improve the fit of the model residuals to a normal distribution.
Conflict of Interest: None.
The published version of this article can be accessed on the Journal of the American Board of Family Medicine website at: http://jabfm.org/content/26/6/669.full
Contributor Information
Steffani Bailey, Email: bailstef@ohsu.edu, Oregon Health & Science University, Department of Family Medicine, 3181 SW Sam Jackson Park Rd., Mailcode: FM, Portland, OR 97239.
Jean P. O’Malley, Email: omalleyj@ohsu.edu, Oregon Health & Science University, Department of Public Health and Preventive Medicine, 3181 SW Sam Jackson Park Rd., Mailcode: FM, Portland, OR 97239.
Rachel Gold, Email: rachel.gold@kpchr.org, Kaiser Permanente Northwest Center for Health Research, 3800 N. Interstate Ave., Portland, OR 97227.
John Heintzman, Email: heintzma@ohsu.edu, Oregon Health & Science University, Department of Family Medicine, 3181 SW Sam Jackson Park Rd., Mailcode: FM, Portland, OR 97239.
Sonja Likumahuwa, Email: likumahu@ohsu.edu, Oregon Health & Science University, Department of Family Medicine, 3181 SW Sam Jackson Park Rd., Mailcode: FM, Portland, OR 97239.
Jennifer E. DeVoe, Oregon Health & Science University, Department of Family Medicine, 3181 SW Sam Jackson Park Rd., Mailcode: FM, Portland, OR 97239, Ph: 503-494-8936.
References
- 1.VanLare JM, Conway PH. Value-based purchasing--national programs to move from volume to value. N Engl J Med. 2012 Jul 26;367(4):292–295. doi: 10.1056/NEJMp1204939. [DOI] [PubMed] [Google Scholar]
- 2.Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998 Sep 16;280(11):1000–1005. doi: 10.1001/jama.280.11.1000. [DOI] [PubMed] [Google Scholar]
- 3.McGlynn EA, Asch SM, Adams J, et al. The Quality of Health Care Delivered to Adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 4.Porter ME. What is value in health care? N Engl J Med. 2010 Dec 23;363(26):2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 5.Galvin RS, McGlynn EA. Using performance measurement to drive improvement: a road map for change. Medical care. 2003 Jan;41(1 Suppl):I48–60. doi: 10.1097/00005650-200301001-00006. [DOI] [PubMed] [Google Scholar]
- 6.Epstein AM, Lee TH, Hamel MB. Paying physicians for high-quality care. N Engl J Med. 2004 Jan 22;350(4):406–410. doi: 10.1056/NEJMsb035374. [DOI] [PubMed] [Google Scholar]
- 7.Committee on Quality of Health Care in America IoM. Crossing the Quality Chasm: A New Health System for the 21st Century. 2001 [Google Scholar]
- 8.Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S. Does pay-for-performance improve the quality of health care? Ann Intern Med. 2006 Aug 15;145(4):265–272. doi: 10.7326/0003-4819-145-4-200608150-00006. [DOI] [PubMed] [Google Scholar]
- 9.Lindenauer PK, Remus D, Roman S, et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007 Feb 1;356(5):486–496. doi: 10.1056/NEJMsa064964. [DOI] [PubMed] [Google Scholar]
- 10.Franks P, Fiscella K. Effect of patient socioeconomic status on physician profiles for prevention, disease management, and diagnostic testing costs. Medical care. 2002 Aug;40(8):717–724. doi: 10.1097/00005650-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Chien AT, Eastman D, Li Z, Rosenthal MB. Impact of a pay for performance program to improve diabetes care in the safety net. Prev Med. 2012 Nov;55(Suppl):S80–85. doi: 10.1016/j.ypmed.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Reschovsky JD, O’Malley AS. Do primary care physicians treating minority patients report problems delivering high-quality care? Health Aff (Millwood) 2008 May-Jun;27(3):w222–231. doi: 10.1377/hlthaff.27.3.w222. [DOI] [PubMed] [Google Scholar]
- 13.Shani M, Nakar S, Lustman A, Baievsky T, Rosenberg R, Vinker S. Patient characteristics correlated with quality indicator outcomes in diabetes care. Br J Gen Pract. 2010;60(578):655–659. doi: 10.3399/bjgp10X515368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salanitro AH, Safford MM, Houston TK, et al. Patient complexity and diabetes quality of care in rural settings. J Natl Med Assoc. 2011;103(3):234–240. doi: 10.1016/s0027-9684(15)30297-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Safford MM, Brimacombe M, Zhang Q, et al. Patient complexity in quality comparisons for glycemic control: An observational study. Implement Sci. 2009;4(2):2. doi: 10.1186/1748-5908-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenfield S, Kaplan SH, Kahn R, Ninomiya J, Griffith JL. Profiling care provided by different groups of physicians: effects of patient case-mix (bias) and physician-level clustering on quality assessment results. Ann Intern Med. 2002;136(2):111–121. doi: 10.7326/0003-4819-136-2-200201150-00008. Summary for patients in Ann Intern Med. 2002 Jan 15;136(2):I42; [DOI] [PubMed] [Google Scholar]
- 17.Carrier ER, Schneider E, Pham HH, Bach PB. Association between quality of care and the sociodemographic composition of physicians’ patient panels: a repeat cross-sectional analysis. J Gen Intern Med. 2011 Sep;26(9):987–994. doi: 10.1007/s11606-011-1740-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alberti H, Boudriga N, Nabli M. “Damm sokkor”: factors associated with the quality of care of patients with diabetes: a study in primary care in Tunisia. Diabetes Care. 2007 Aug;30(8):2013–2018. doi: 10.2337/dc07-0520. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Q, Safford M, Ottenweller J, et al. Performance status of health care facilities changes with risk adjustment of HbA1c. Diabetes Care. 2000 Jul;23(7):919–927. doi: 10.2337/diacare.23.7.919. [DOI] [PubMed] [Google Scholar]
- 20.Hong CS, Atlas SJ, Chang Y, et al. Relationship between patient panel characteristics and primary care physician clinical performance rankings. JAMA. 2010 Sep 8;304(10):1107–1113. doi: 10.1001/jama.2010.1287. [DOI] [PubMed] [Google Scholar]
- 21.Zhang JX, Huang ES, Drum ML, et al. Insurance status and quality of diabetes care in community health centers. American journal of public health. 2009 Apr;99(4):742–747. doi: 10.2105/AJPH.2007.125534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kulesher RR. Health Reform’s Impact on Federally Qualified Community Health Centers: The Unintended Consequence of Increased Medicaid Enrollment on the Primary Care Medical Home. Health Care Manag. 2013;32(2):99–106. doi: 10.1097/HCM.0b013e31828ef5d5. [DOI] [PubMed] [Google Scholar]
- 23.Cook NL, Hicks LS, O’Malley AJ, Keegan T, Guadagnoli E, Landon BE. Access To Specialty Care And Medical Services In Community Health Centers. Health Aff (Millwood) 2007;26(5) doi: 10.1377/hlthaff.26.5.1459. [DOI] [PubMed] [Google Scholar]
- 24.Hicks LS, O’Malley AJ, Lieu TA, et al. The quality of chronic disease care in U.S. community health centers. Health Aff (Millwood) 2006;25(6):1712–1723. doi: 10.1377/hlthaff.25.6.1712. [DOI] [PubMed] [Google Scholar]
- 25.Goldman LE, Chu PW, Tran H, Romano MJ, Stafford RS. Federally qualified health centers and private practice performance on ambulatory care measures. Am J Prev Med. 2012;43(2):142–149. doi: 10.1016/j.amepre.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shi L, Lebrun LA, Hung L-M, Zhu J, Tsai J. US Primary Care Delivery After the Health Center Growth Initiative: Comparison of Health Centers, Hospital Outpatient Departments, and Physicians’ Offices. J Ambulatory Care Manage. 2012;35(1):60–74. doi: 10.1097/JAC.0b013e31823abf07. [DOI] [PubMed] [Google Scholar]
- 27.Ulmer C, Lewis-Idema D, Von Worley A, et al. Assessing primary care content: four conditions common in community health center practice. J Ambulatory Care Manage. 2000 Jan;23(1):23–38. doi: 10.1097/00004479-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Long SK, Stockley K. The Impacts of State Health Reform Initiatives on Adults in New York and Massachusetts. Health services research. 2011;46(1p2):365–387. doi: 10.1111/j.1475-6773.2010.01211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Devoe JE, Gold R, Spofford M, et al. Developing a network of community health centers with a common electronic health record: description of the Safety Net West Practice-based Research Network (SNW-PBRN) Journal of the American Board of Family Medicine : JABFM. 2011;24(5):597–604. doi: 10.3122/jabfm.2011.05.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Diabetes Assocation. Standards of medical care in diabetes-2012. Diabetes Care. 352012:S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kenealy T, Elley CR, Collins JF, Moyes SA, Metcalf PA, Drury PL. Increased prevalence of albuminuria among non-European peoples with type 2 diabetes. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2012 May;27(5):1840–1846. doi: 10.1093/ndt/gfr540. [DOI] [PubMed] [Google Scholar]
- 32.Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 2005 Jan;28(1):164–176. doi: 10.2337/diacare.28.1.164. [DOI] [PubMed] [Google Scholar]
- 33.Gold R, DeVoe J, Shah A, Chauvie S. Insurance continuity and receipt of diabetes preventive care in a network of federally qualified health centers. Medical care. 2009;47(4):431–439. doi: 10.1097/mlr.0b013e318190ccac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gold R, DeVoe JE, McIntire PJ, Puro JE, Chauvie SL, Shah AR. Receipt of diabetes preventive care among safety net patients associated with differing levels of insurance coverage. Journal of the American Board of Family Medicine : JABFM. 2012;25(1):42–49. doi: 10.3122/jabfm.2012.01.110142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Voorhees K, Fernald DH, Emsermann C, et al. Underinsurance in primary care: a report from the State Networks of Colorado Ambulatory Practices and Partners (SNOCAP) Journal of the American Board of Family Medicine : JABFM. 2008 Jul-Aug;21(4):309–316. doi: 10.3122/jabfm.2008.04.080001. [DOI] [PubMed] [Google Scholar]
- 36.Ng JH, Kaftarian SJ, Tilson WM, et al. Self-reported delays in receipt of health care among women with diabetes and cardiovascular conditions. Womens Health Issues. 2010;20(5):316–322. doi: 10.1016/j.whi.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 37.Meyers DS, Mishori R, McCann J, Delgado J, O’Malley AS, Fryer E. Primary care physicians’ perceptions of the effect of insurance status on clinical decision making. Annals of family medicine. 2006 Sep-Oct;4(5):399–402. doi: 10.1370/afm.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marx R, Drennan MJ, Johnson EC, Solnit SA, Hirozawa AM, Katz MH. Creating a medical home in the San Francisco department of public health: establishing patient panels. Journal of public health management and practice : JPHMP. 2009 Jul-Aug;15(4):337–344. doi: 10.1097/PHH.0b013e31819d81a3. [DOI] [PubMed] [Google Scholar]
- 39.Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health services research. 2000 Apr;35(1 Pt 2):187–206. [PMC free article] [PubMed] [Google Scholar]
- 40.Gulley SP, Rasch EK, Chan L. Ongoing coverage for ongoing care: access, utilization, and out-of-pocket spending among uninsured working-aged adults with chronic health care needs. American journal of public health. 2011 Feb;101(2):368–375. doi: 10.2105/AJPH.2010.191569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Friedberg MW, Safran DG, Coltin K, Dresser M, Schneider EC. Paying for performance in primary care: potential impact on practices and disparities. Health Affairs. 2010 May;29(5):926–932. doi: 10.1377/hlthaff.2009.0985. [DOI] [PubMed] [Google Scholar]
- 42.Casalino LP, Elster A, Eisenberg A, Lewis E, Montgomery J, Ramos D. Will pay-for-performance and quality reporting affect health care disparities? Health Affairs. 2007 May-Jun;26(3):w405–414. doi: 10.1377/hlthaff.26.3.w405. Erratum appears in Health Aff (Millwood). 2007 Nov-Dec;26(6):1794 Note: Eisenberg, Andy [added]; Lewis, Evelyn [added]; Montgomery, John [added]; Ramos, Diana [added] [DOI] [PubMed] [Google Scholar]
- 43.Devoe JE, Gold R, McIntire P, Puro J, Chauvie S, Gallia CA. Electronic health records vs Medicaid claims: completeness of diabetes preventive care data in community health centers. Annals of family medicine. 2011 Jul-Aug;9(4):351–358. doi: 10.1370/afm.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


