Abstract
Because the distal radioulnar joint (DRUJ) is an inherently unstable joint, the diagnosis and treatment of DRUJ instability is often difficult in a clinical hand surgery practice. Several soft tissue stabilizers are recognized, of which the deep limbs of the radioulnar ligament are primary stabilizers. This article discusses the predictors of DRUJ instability in distal radius fractures based on our clinical and biomechanical analyses.
Keywords: radioulnar, joint, instability, predictor
The primary stabilizers of the distal radioulnar joint (DRUJ) include the superficial and deep radioulnar ligaments of the triangular fibrocartilage complex (TFCC).1 2 Secondary stabilizers include the ulnocarpal ligaments, extensor carpi ulnaris (ECU) sheath, pronator quadratus muscle, and interosseous membrane. Loss of integrity in one or more of these stabilizers may cause instability of the DRUJ, resulting in ulnar-sided wrist pain, weakness, and restricted range of forearm rotation. Instability of the DRUJ is frequently associated with distal radius fractures, and previous authors have reported the radiographic indicators of DRUJ instability.3 4 5 6 7 Owing to the attachment site of the deep radioulnar ligaments, a fracture of the base of the ulnar styloid or of the dorsoulnar corner of the distal radius may contribute to DRUJ instability.
Previous investigators hypothesized that the severity of fracture pattern and magnitude of fracture displacement are important predictors for DRUJ instability associated with distal radius fractures.3 4 5 6 This article discusses the predictors of DRUJ instability in distal radius fractures and focuses on radial translation (DRUJ gap) as a predictor, based on our clinical data as well as preliminary biomechanical analysis.
Materials and Methods
Clinical Study
From 2004 to 2012, we conducted a prospective study for evaluating DRUJ instability associated with unstable distal radius fractures. Open reduction with internal fixation (ORIF) was performed on 346 patients with unstable distal radius fractures. We defined unstable fractures requiring surgery as fractures with one or more of the following: dorsal tilt angle greater than 20° (or volar tilt angle greater than 20° in volarly displaced fractures), radial shortening of more than 5 mm, and intra-articular gap (measured in accordance with the technique described by Fujitani et al3) or step-off of at least 2 mm. Patients with concomitant carpal and/or forearm fractures, open fractures, and associated tendon or nerve injuries were included in the study. We excluded skeletally immature patients, patients with severe mental disorders, patients with bilateral fractures, and patients with prior ipsilateral wrist injuries. Our institutional review board approved this study, and we obtained informed consent from each patient.
All 346 patients underwent open reduction and internal fixation using volar locking plates and screws or intramedullary nailing under general or brachial plexus block anesthesia. Since 2008, we have treated 43 patients with extra-articular fractures and without intra-articular involvement using intramedullary nailing. Following fixation of the distal radius fracture, the surgeon manually examined the radioulnar ligament using the DRUJ ballottement test. The examiner tried to force the distal ulna in both the dorsal and volar directions relative to the radiocarpal unit with the forearm in neutral rotation. The criteria for assessing DRUJ instability were not only the amplitude of the translation, but also the quality of the end point. We defined DRUJ instability as a condition in which there were no solid end points in either the volar or the dorsal direction. We examined the contralateral wrist as well to exclude patients with general joint laxity. The injured wrist, which was judged to have ligamentous DRUJ instability and was unstable relative to the opposite side, was explored by arthroscopy followed by open surgery. When we judged that there was a complete tear of the foveal attachment, we performed an open capsulotomy to confirm the tear and performed a foveal repair using bone anchors (Fig. 1).
Fig. 1.
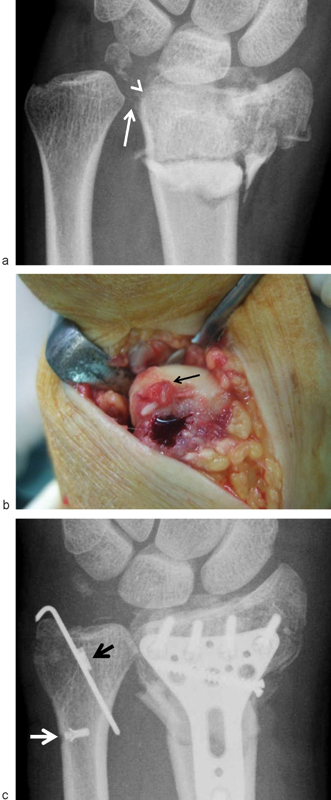
(a) Anteroposterior prereduction radiograph of a fractured wrist with a complete deep radioulnar ligament tear. White arrow indicates DRUJ widening between the distal radius and the ulnar head. Note the significant radial translation of the distal radial fragment. Arrow head points to the ulnar corner of the sigmoid notch of the radius. (b) Arthrotomy confirmed there was a complete radioulnar ligament tear at the fovea of the ulnar head (black arrow). We reattached the ligament using a suture anchor. (c) Postoperative X-ray indicating no DRUJ widening between the radius and the ulna. Two suture anchors fix the radioulnar deep ligament foveal avulsion (black arrow) and ulnar styloid fragment (white arrow).
A long-arm cast was applied for 3 weeks after surgery in patients who had a repair of the radioulnar ligament; the remaining patients, who did not have complete ligament tears, were given a short-arm splint for 2 weeks. All the patients were observed during the outpatient clinic for a minimum of 6 months after surgery. At each follow-up visit, patients were asked about ulnar wrist symptoms such as a painful click or a subjective sense of instability. The DRUJ ballottement test was performed again to evaluate chronic instability. When we found clinical evidence of symptomatic DRUJ instability in the postoperative period that had failed to respond to conservative treatment, we took the patient back to the operating room and explored the DRUJ to repair the deep radioulnar ligament.
Radiographic Predictor of DRUJ Instability
Potential radiographic predictors of DRUJ instability included three fracture characteristics: severity of the fracture pattern, an ulnar styloid fracture, and the magnitude of fracture displacement. We assessed the severity of the fracture pattern according to the AO classification. We used five radiographic parameters to assess the magnitude of fracture displacement: ulnar variance, radial inclination, radial translation in a posteroanterior (PA) radiograph, volar tilt, and sagittal translation on a lateral radiograph.
Statistical Analysis
We tested the univariate associations between the outcome variable and the potential predictor. A chi-square test was used for categorical variables, and a Student t-test was used for continuous variables. The outcome variable was the presence or absence of DRUJ instability due to a complete deep radioulnar ligament tear. We included predictor variables with significant differences in the univariate analyses and the patient characteristic variables in the final logistic regression analysis models to control their effects on possible independent predictors. We performed a multivariate logistic regression analysis using the log odds ratio of the presence of DRUJ instability as a dependent outcome variable. Values of P less than 0.05 were considered statistically significant. We derived adjusted odds ratios, computed 95% confidence intervals, and considered factors to be significant when the 95% confidence interval around the odds ratio did not include 1.
Biomechanical Study
Experimental Setup
We used three fresh upper extremity cadaveric specimens during a preliminary biomechanical study. The humerus and ulna were fixed to the testing apparatus with the elbow at 90° flexion. The radius, carpus, and metacarpal bone were fixed with the wrist in neutral position by Kirschner wires (K-wires), and the radiocarpal unit was allowed to rotate freely around the ulna. Weights were attached to the prime wrist movers to simulate a physiological load according to Kobayashi et al: extensor carpi radialis brevis (ECRB) and longus (ECRL), 2.5 kg; ECU, 1.6 kg; flexor carpi ulnaris (FCU), 2.2 kg; flexor carpi radialis (FCR), 1.6 kg; abductor pollicis longus (APL), 1 kg.8 A three-dimensional electromagnetic tracking device (3SPACE FASTRAK; Polhemus, Colchester, VT, USA) was used. One of two sensors was placed on the ulna, and the other was placed on the radius (Fig. 2). A screw was inserted into the radial styloid and was connected to a suture to apply loading in a radial direction.
Fig. 2.
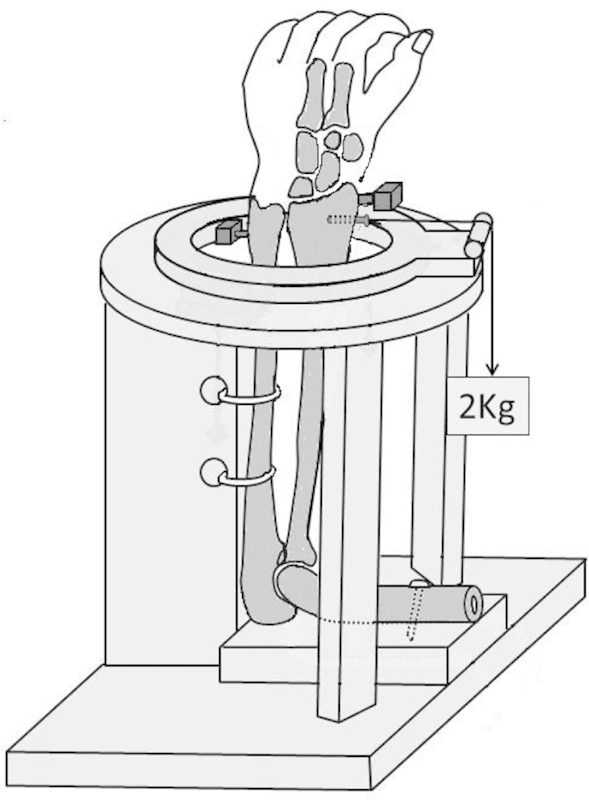
Experimental setup of upper extremity specimens shows fixation of the humerus and the ulna. The radius is held in the forearm neutral rotation, and 2 kg of radially directed force is applied to the distal radius fragment.
DRUJ Dissociation Testing and Data Acquisition
The radius was passively translated in a radial direction relative to the ulna using a load of 2 kgf in a radial direction with the forearm in neutral rotation. DRUJ instability was simulated by sectioning the following components of the TFCC: the deep radioulnar ligaments, the TFCC disk proper, the floor of the ECU sheath, the ulnocarpal ligaments, and the DRUJ capsule. In both the intact and TFCC-sectioned wrists, the DRUJ gap distances were measured during passive testing. The data were acquired by measuring changes in the location of the radius relative to the ulna during the passive testing, as monitored by the electromagnetic tracking device.
Results
Clinical Study
We found 22 patients with a complete radioulnar ligament tear. Of these patients, 19 patients were diagnosed as having DRUJ instability during the initial distal radius fracture surgery via manual stress testing, and three patients were diagnosed with DRUJ instability in the postoperative period because of persistent wrist pain and subluxation of the DRUJ. All of the 22 patients with DRUJ instability were found during open surgery to have a complete tear of the deep radioulnar ligament from the foveal attachment.
The deep radioulnar ligament tears were reattached to the fovea. The 19 patients who had a repair at the time of fracture fixation showed a stable and painless DRUJ during the follow-up period. Three patients showed DRUJ stability during the fracture fixation and were found to have ligament tears during the postoperative follow-up. One was a 39-year-old man and the others were 55-year-old and 24-year-old women. The DRUJ gap distance of these patients was 4, 3, and 1 mm, respectively. At 4, 6, and 12 months after the initial surgery, we performed open surgical repair of torn ligaments at the fovea of the ulnar head followed by immobilization in a long-arm cast for 3 weeks. The wrist pain and DRUJ instability subsided after the surgery.
In the current 346 prospective cohort, 22 patients had gross DRUJ instability with complete deep radioulnar ligament tears (Table 1). The remaining 324 patients had no gross DRUJ instability throughout the entire observation period. In univariate analyses, only the radial and sagittal translation were significant predictors of DRUJ instability. The radial translation (DRUJ gap distance) of the 22 patients with complete tears averaged 5.0 mm (range: 0–12), whereas those of the 324 patients without tears averaged 1.6 mm (range: 0–6.4). Multivariate logistic regression analysis using the initial cohort of 163 patients revealed that the radial translation ratio was a significant independent risk factor (adjusted odds ratio, 1.5; 95% confidence interval, 1.2–1.9; P < 0.001). Multivariate logistic regression analysis revealed that the sagittal translation ratio was not a significant independent risk factor (adjusted odds ratio, 1.0; 95% confidence interval, 0.2–1.0; P < 0.220).
Table 1. Comparison of patient and fracture characteristics.
| Controls (n = 324) | Cases (n = 22) | P Value | |
|---|---|---|---|
| Age (y) | 64 ± 19 | 60 ± 18 | .16 |
| Sex | .89 | ||
| Female | 201 (62%) | 14 (64%) | |
| Male | 123 (38%) | 8 (36%) | |
| AO classification | A3: 81 C1: 33 | A3: 3 C2: 9 | .12 |
| C2: 97 C3: 66 | C3: 10 | ||
| Ulnar styloid fracture | 211 (65%) | 18 (82%) | .11 |
Controls: patients without complete radioulnar ligament tear
Cases: patients with complete radioulnar ligament tear
Biomechanical Study
In the intact wrists, changes in the DRUJ gap distances during passive mobility testing averaged 1.9 ± 1.3 mm in neutral forearm rotation. In the TFCC-sectioned wrists, average change in the DRUJ gap distance increased to 4.6 ± 1.4mm.
Discussion
In the current analysis, a radiographic finding of widening of DRUJ gap distance on a posteroanterior view was the most important predictor to identify DRUJ instability accompanying an unstable distal radius fracture. The deep radioulnar ligament is a primary stabilizer of the DRUJ and provides a transverse link between the distal radius and the ulna. Therefore, it is reasonable to conclude that radioulnar dissociation likely occurs when there is DRUJ instability following fracture displacement and a complete deep radioulnar ligament tear. Based on a multivariate analysis, the only significant independent risk factor was an increase in the DRUJ gap distance by 1 mm, which increased the risk of radioulnar ligament tear by a factor of 5 in a patient of average wrist width.
Our preliminary biomechanical investigation, which measured changes in radial translation of the distal radius relative to the ulna, revealed that changes in the DRUJ gap distances during passive mobility testing in the intact wrists averaged 1.9 mm and those in the TFCC-sectioned wrists averaged 4.6 mm. It was intriguing that these biomechanical data are similar to our clinical data (Table 2), which indicated that radial translation (DRUJ gap distance) of the 22 patients with complete tears averaged 5.0 mm, whereas those of the 324 patients without tears averaged 1.6 mm. DRUJ widening in the fractured wrists was observed in patients with complete deep radioulnar ligament tears, even if no external force was applied. We acknowledge, however, that the biomechanical model does not approximate the clinical situation, since there was no simulated distal radius fracture and none of the wrist motors cause a 2-kg radial translation force. Previous investigators hypothesized that the severity of fracture pattern and magnitude of displacement in the other specific radiographic parameters are important predictors for DRUJ instability associated with distal radius fractures.3 4 5 6 7 A cadaveric study found that up to 5 mm of radial shortening occurs after radial osteotomy alone, but shortening by more than 10 mm did not occur unless both the interosseous membrane and the radioulnar ligament were transected.9 Radial shortening of more than 5 mm can stretch the dorsal and palmar radioulnar ligaments and result in ligament tears. Omori et al10 investigated three-dimensional changes in the length of the radioulnar ligament in patients with malunited distal radius fractures using computed tomography (CT). They found that, in a malunited radius, the superficial and deep dorsal limbs of the radioulnar ligament were significantly elongated compared with the contralateral side. This length change correlated with radiographic radial shortening and subluxation of the DRUJ. They suggested that overstretching and disruption of the dorsal radioulnar ligament in malunited distal radius fractures with severely increased radial shortening produces laxity in the DRUJ. In a retrospective study5 that reviewed 221 patients who underwent surgical treatment for unstable distal radius fractures, 10 patients were found to have DRUJ instability by intraoperative manual testing. Based on a univariate analysis, two factors increased the risk of DRUJ instability in distal radius fractures: an open wound at the wrist (relative risk: 4.5) and a positive ulnar variance of 6 mm or more on a prereduction radiograph (relative risk: 1.7). Saito et al11 conducted a biomechanical study examining the effects of dorsal angulation deformity and radioulnar ligament tears on DRUJ stability. The DRUJ stiffness in dorsal translation decreased significantly with dorsal tilts of 10° and 20° in pronation. Subsequent transection of the superficial and deep radioulnar ligaments resulted in a significant decrease of the DRUJ stiffness in in all forearm positions. The authors concluded that the dorsal angulation of the radius should be corrected to less than 10° of dorsal tilt to avoid DRUJ instability.
Table 2. DRUJ widening in radioulnar ligament tears (sectioning).
| DRUJ gap distance (mm) | ||
|---|---|---|
| Intact | Complete tear | |
| Clinical data (n = 346) | 1.6 ± 1.2 (n = 324) | 5.0 ± 3.2 (n = 22) |
| Biomechanical data (n = 3) | 1.9 ± 1.3 | 4.6 ± 1.4 |
Nakanishi et al12 analyzed fracture patterns and displacement in the DRUJ using three-dimensional CT scans of intra-articular distal radius fractures. Of the 72 fractures analyzed, 8% had dorsal comminution and displacement of the DRUJ, which may increase the risk for DRUJ instability.
Ulnar styloid fractures occur in isolation, but are often associated with distal radius fractures. Because the radioulnar ligament attaches to the base of the ulnar styloid, this type of fracture may be a predisposing factor for DRUJ instability. May et al7 reported that an associated ulnar styloid fracture occurred in 143 of 166 patients (86%) with distal radius fractures. Fractures at the base of the ulnar styloid and major displacement of an ulnar styloid fracture were both found to increase the risk of DRUJ instability. Bombaci et al6 conducted a prospective study of postreduction magnetic resonance imaging (MRI) data for 60 consecutive patients with distal radius fractures to determine the radiographic predictors of a TFCC injury. The fracture pattern, according to the Frykman classification, was found to be a significant predictor, and fracture types 6 and 8, in which fracture lines both extend into the sigmoid notch of the radius and involve the ulnar styloid, more frequently had an associated TFCC lesion than the other types of fractures.
Because the DRUJ is inherently unstable, the diagnosis and treatment of DRUJ instability is often difficult in clinical hand surgery practice. Although there is no robust evidence on whether associated soft tissue injury affects clinical outcomes for treating wrist fractures, knowledge of the predictors of DRUJ instability is important.
Footnotes
Conflict of Interest None
References
- 1.Palmer A K, Werner F W. The triangular fibrocartilage complex of the wrist—anatomy and function. J Hand Surg Am. 1981;6:153–162. doi: 10.1016/s0363-5023(81)80170-0. [DOI] [PubMed] [Google Scholar]
- 2.Nakamura T, Takayama S, Horiuchi Y, Yabe Y. Origins and insertions of the triangular fibrocartilage complex: a histological study. J Hand Surg [Br] 2001;26(5):446–454. doi: 10.1054/jhsb.2001.0562. [DOI] [PubMed] [Google Scholar]
- 3.Fujitani R, Omokawa S, Akahane M, Iida A, Ono H, Tanaka Y. Predictors of distal radioulnar joint instability in distal radius fractures. J Hand Surg Am. 2011;36(12):1919–1925. doi: 10.1016/j.jhsa.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Richards R S, Bennett J D, Roth J H, Milne K Jr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am. 1997;22(5):772–776. doi: 10.1016/S0363-5023(97)80068-8. [DOI] [PubMed] [Google Scholar]
- 5.Kwon B C, Seo B K, Im H J, Baek G H. Clinical and radiographic factors associated with distal radioulnar joint instability in distal radius fractures. Clin Orthop Relat Res. 2012;470(11):3171–3179. doi: 10.1007/s11999-012-2406-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bombaci H, Polat A, Deniz G, Akinci O. The value of plain X-rays in predicting TFCC injury after distal radial fractures. J Hand Surg Eur Vol. 2008;33:322–326. doi: 10.1177/1753193408090106. [DOI] [PubMed] [Google Scholar]
- 7.May M M, Lawton J N, Blazar P E. Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg Am. 2002;27(6):965–971. doi: 10.1053/jhsu.2002.36525. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi M, Garcia-Elias M, Nagy L. et al. Axial loading induces rotation of the proximal carpal row bones around unique screw-displacement axes. J Biomech. 1997;30(11-12):1165–1167. doi: 10.1016/s0021-9290(97)00080-8. [DOI] [PubMed] [Google Scholar]
- 9.Moore T M, Lester D K, Sarmiento A. The stabilizing effect of soft-tissue constraints in artificial Galeazzi fractures. Clin Orthop Relat Res. 1985;194(194):189–194. [PubMed] [Google Scholar]
- 10.Omori S, Moritomo H, Murase T. et al. Changes in length of the radioulnar ligament and distal oblique bundle after Colles' fracture. J Plast Surg Hand Surg. 2013;47:409–414. doi: 10.3109/2000656X.2013.775139. [DOI] [PubMed] [Google Scholar]
- 11.Saito T, Nakamura T, Nagura T, Nishiwaki M, Sato K, Toyama Y. The effects of dorsally angulated distal radius fractures on distal radioulnar joint stability: a biomechanical study. J Hand Surg Eur Vol. 2013;38:739–745. doi: 10.1177/1753193412473036. [DOI] [PubMed] [Google Scholar]
- 12.Nakanishi Y, Omokawa S, Shimizu T, Nakano K, Kira T, Tanaka Y. Intra-articular distal radius fractures involving the distal radioulnar joint (DRUJ): three dimensional computed tomography-based classification. J Orthop Sci. 2013;18(5):788–792. doi: 10.1007/s00776-013-0407-0. [DOI] [PubMed] [Google Scholar]


