Abstract
Background Malunions following distal radius fractures are common, with shortening, translation, and rotation occurring. The patients frequently lose forearm rotation, but there is no data to indicate whether this is due to mechanical misalignment between the radius and the ulna or to contracture of the soft tissues.
Material and Methods Seven fresh cadaveric specimens were used to determine the loss of forearm rotation with varying simulated distal radius fracture malalignment patterns. Uniplanar malunion patterns consisting of dorsal tilt, radioulnar translation, or radial shortening were simulated by creating an osteotomy at the distal end of the radius.
Description of Technique By orienting the distal fragment position using an external fixator and maintaining the position with wedges and a T-plate, varying degrees of malunion of the distal radius could be simulated. Rotation of the forearm was produced by fixing the elbow in a flexed position and applying a constant torque to the forearm using deadweights. Forearm rotation was measured with a protractor.
Results Dorsal tilt to 30° and radial translation to 10 mm led to no significant restriction in forearm pronation or supination ranges of motion. A 5-mm ulnar translation deformity resulted in a mean 23% loss of pronation range of motion. Radial shortening of 10 mm reduced forearm pronation by 47% and supination by 29%.
Conclusion Because a severe osseous misalignment was required to produce a significant loss in rotation, contracture of the soft tissues is most likely the cause of the loss of rotation in most cases.
Keywords: allograft, artilage, thumb arthritis, ligament, stability
As the most common fracture, distal radius fractures comprise ∼15% of all fractures that occur. The principles of treatment of this condition consists of reducing the fracture and maintaining position with cast immobilization, external and/or internal fixation.1 2 Several studies have shown that many of patients have experienced suboptimal results from treatment of their fracture.3 4 5 6 7 Unreduced fractures or those with unrecognized loss of reduction lead to malunion, eventual arthrosis, and a resultant decrease in function of the forearm, wrist, and digits and may require an osteotomy to realign the radiocarpal and radioulnar joints and regain function.4 5 8 In many cases, the degree of the deformity does not correlate with the severity of the function loss. Fig. 1 demonstrates a case of a patient with pain and a severe deformity but good range of motion of the wrist.
Fig. 1.
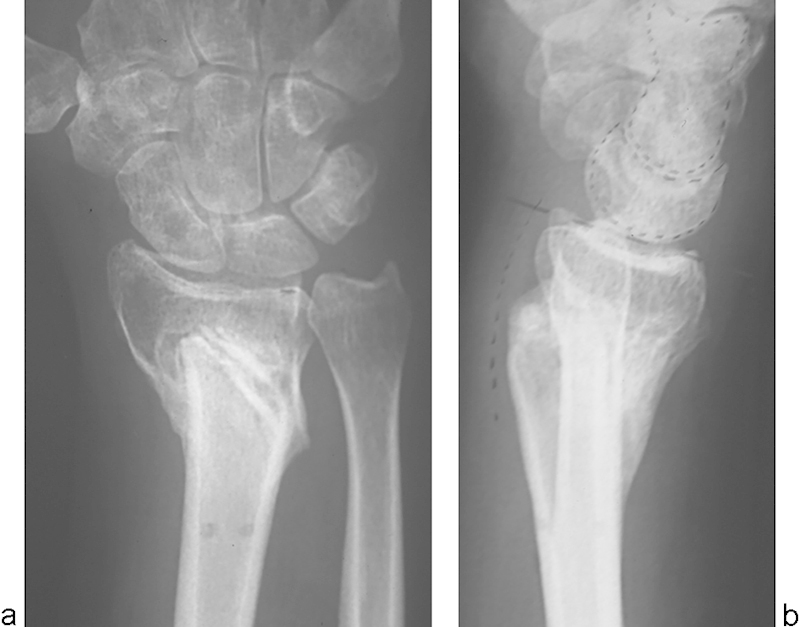
(a) An anteroposterior view demonstrates a distal radius malunion with significant loss of height and radial inclination. (b) This lateral radiograph demonstrated the reversal of the normal palmar inclination to a severely dorsally tilted malunion. (Reprinted from Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: A cadaveric study. J Hand Surg Am. 1997;22(2):258-262, with permission from Elsevier.)
As a result of a distal radius fracture, patients can experience considerable disability from loss of motion due to either changes in the alignment in the joint or contracture of the soft tissues following the injury and immobilization. Possible biomechanical explanations for the decreased wrist motion in the setting of a malunion include a decrease in the volume and contact pressures in the distal radioulnar joint (DRUJ).9 Another biomechanical study suggests that the radius malunion may cause altered carpal kinematics.6 These patients are often enrolled in therapy programs to regain their range of motion (ROM). On one hand, the fact that many patients do not regain full motion despite adherence to therapy regimens is possibly due to DRUJ malposition caused by distal radius malalignment rather than to soft tissue scarring. If joint malalignment is the etiology of motion loss, then continued therapy would be of no benefit to the patient. On the other hand, a clinical report of corrective osteotomy of radii malunions suggests that correcting the deformity does not restore functional motion.5 Therefore, a cadaveric model of the upper extremity was used to determine how varying degrees of fracture malalignment affect the limits of forearm rotation.
Materials and Methods
Specimen Preparation
Fresh cadaveric upper extremities were used with intact hand, wrist, and elbow joints and sectioned at midhumerus. The specimens were inspected visually and radiographically for degenerative or abnormal changes, and seven were selected for testing. On the day of testing, each specimen was thawed and a mounted onto a testing apparatus using a cross-locked rod placed into the medullary canal of the humerus.
To reproduce varying degrees of fracture displacement accurately, a highly adjustable wrist external fixator (Agee Wrist Jack, Hand Biomechanics Laboratory, Sacramento, CA, USA) was applied to the specimen, with pins placed proximally into the radial shaft and distally into the second metacarpal (Fig. 2). The fixator is designed to have separate adjustments of hand flexion/extension, radioulnar deviation, and shortening/ lengthening. Using a microsagittal saw, a transverse osteotomy was performed 15 mm proximal to the dorsal lip of the articular surface of the distal radius, at the level of Lister's tubercle. Shortening was controlled by the amount of bone resected at the osteotomy, measured using an electronic caliper (Xtra-value Cal, Beijing, China). By inserting brass wedges of appropriate angle into the osteotomy site, the degree of dorsal tilt was controlled (Fig. 3). Radial and ulnar shift were measured directly using a caliper (Fig. 4). Each simulated malunion position (tilt, shortening, or shift) was created one at a time, held by the external fixator. The distal component of the osteotomy was fixed in its malaligned position to the proximal radius with a 3.5 mm semitubular T-plate (Synthes Inc., Paoli, PA, USA) on the volar surface (Fig. 5).
Fig. 2.

Schematic diagram of an apparatus used to load and measure forearm rotation of upper extremity specimens. The humerus is fixed, but the forearm can rotate freely. The distal end is pinned to a pulley, through which a torque is applied by a deadweight. (Reprinted from Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: A cadaveric study. J Hand Surg Am 1997;22(2):258-262, with permission from Elsevier.)
Fig. 3.
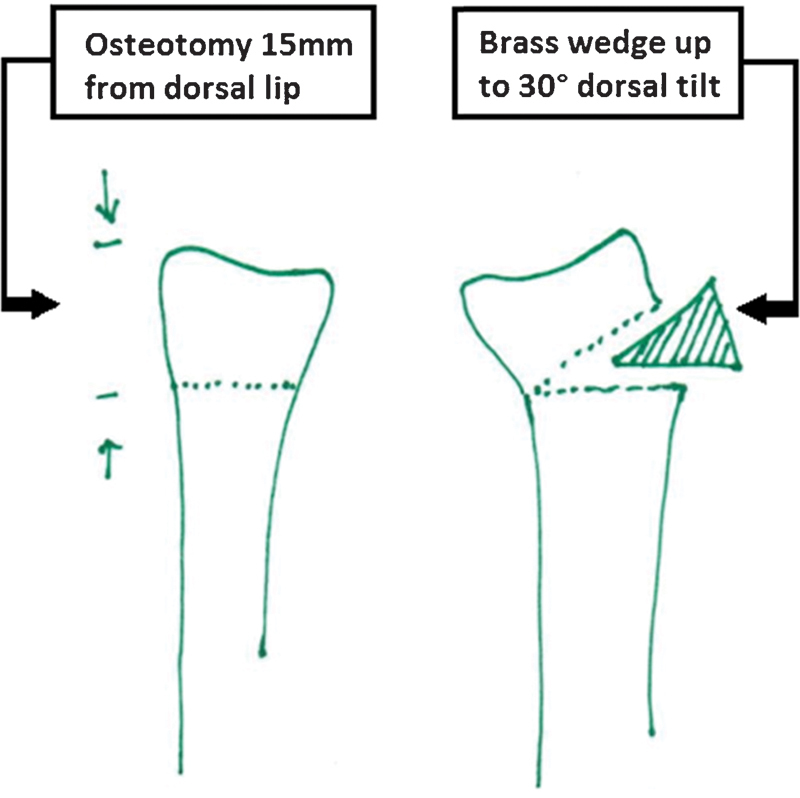
Dorsal tilts of 0°, 15°, and 30° were simulated using brass wedges inserted into the osteotomy. (Reprinted from Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: A cadaveric study. J Hand Surg Am 1997;22(2):258-262, with permission from Elsevier.)
Fig. 4.
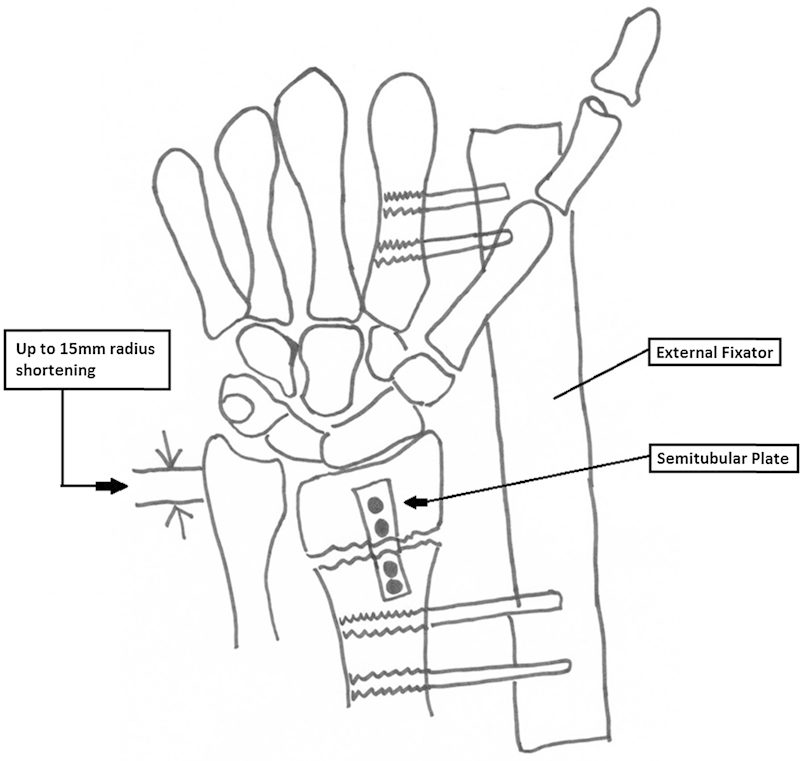
Up to 15 mm of radius shortening was simulated using the external fixation device. (Reprinted from Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: A cadaveric study. J Hand Surg Am 1997;22(2):258-262, with permission from Elsevier.)
Fig. 5.
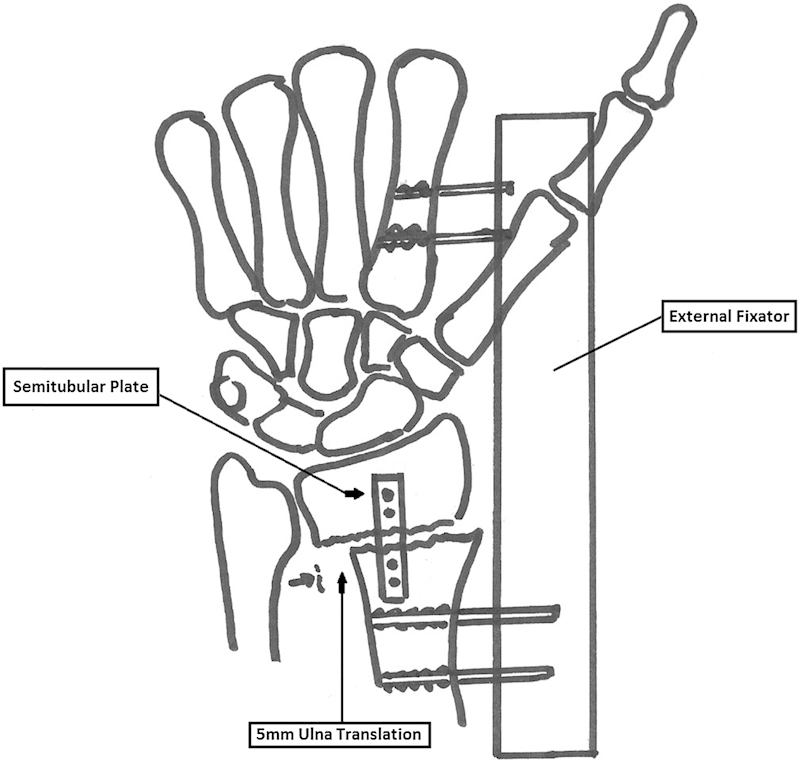
Radial (5 mm and 10 mm) and ulnar (5 mm) translations were simulated using translation with the external fixator. (Reprinted from Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: A cadaveric study. J Hand Surg Am 1997;22(2):258-262, with permission from Elsevier.)
Applying Loads to the Specimen
Using a frame to support the extremity, the arm was suspended hanging freely downward with the elbow in 90° flexion (Fig. 5) To control rotation, the hand was placed within a U-shaped bracket and coupled to it by a pin passed through the distal part of the extremity and the bracket, and the bracket was connected to a turntable. To standardize the torque applied for pronation and supination, the turntable had a cable wrapped around its perimeter; the cable was connected to the turntable on one end and to a 0.714-N deadweight on the other, allowing a 0.277-Nm torque to be applied to the extremity. Correspondingly, the center of rotation of the turntable was aligned with the ulna of the specimen. A protractor was used to measure forearm rotation (360° range, ± 0.5° accuracy) fixed to the turntable. The apparatus did not allow motions in directions other than axial rotation.
Experimental Procedure
Pronation and supination were assessed as total rotation of the intact forearm, as measured by applying a torque in one direction and then in the other and measuring angular motion in each direction. The midpoint of the total rotation was defined as the neutral pronation/supination position. Each of the measurements was repeated three times. After eliminating sources of friction in the loading apparatus, rotation was repeatable to within the accuracy of measurement of the protractor. With the specimen securely mounted, the fixator was then applied, the osetotomy was created, and the measurement was repeated with the cut component in anatomic position, to determine whether creation of the osteotomy and application of hardware affected forearm ROM. The distal radius fracture component was then located in each of the positions noted in Fig. 2, with measurements made of forearm rotation: radioulnar shift of 0 mm, 5 mm, 10 mm radial and 5 mm ulnar, and then returned to anatomic position; dorsal tilt of 0°, 15°, and 30° and then returned to anatomic position; and radial shortening of 0 mm, 5 mm, and 10 mm.
Data Analysis
Comparisons between forearm rotation intact and after osteotomy and between anatomic positioning and malpositioning of the distal radius component were made using an analysis of variance. Fisher's PLSD post-hoc comparison was used to compare the mean values of forearm rotation in anatomic position and each malaligned position of the distal end of the radius. Significance was set at P < 0.05.
Results
The average arc of anatomic forearm rotation for the seven specimens was 181° (range, 146–216°).
Mean anatomic pronation angle for the specimens before osteotomy was 89.9° (SD = 14.8°) and supination angle was 91.1° (SD = 16.4°). There was no significant change in forearm rotation with dorsal tilt of the distal radius of up to 30° (Fig. 6). There was no significant difference in rotation with translation of the distal radius up to 10 mm in the radial direction (Fig. 7). Ulnar translation of 5 mm led to a mean 23% loss of pronation (mean angle, 68.9°, SD = 9.6°, compared with 89.9°, SD = 14.6° intact, P < 0.01). Supination angle was unchanged.
Fig. 6.
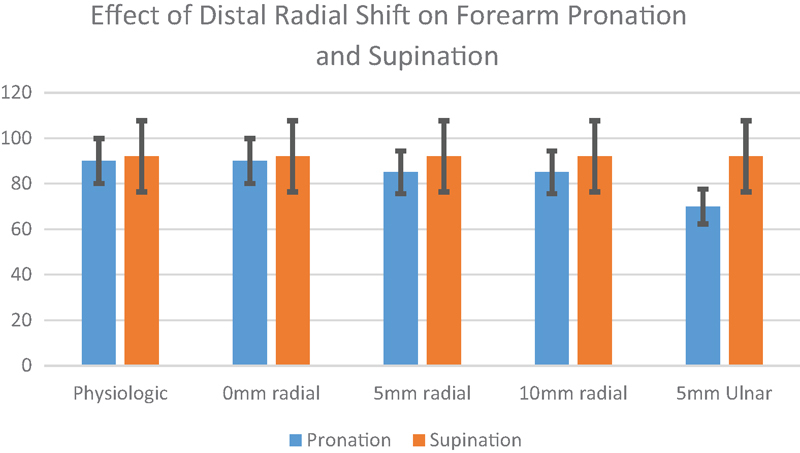
Effect of distal radius shift on forearm pronation and supination motions (n = 7: P < .01 compared with anatomic). (Reprinted from Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: A cadaveric study. J Hand Surg Am 1997;22(2):258-262, with permission from Elsevier.)
Fig. 7.
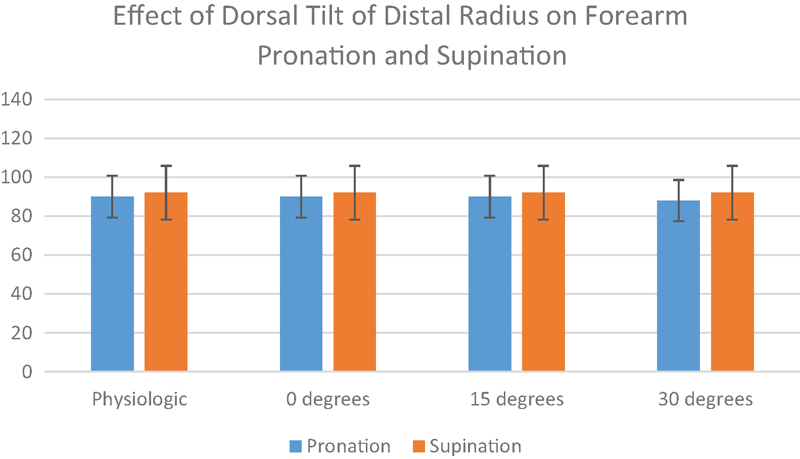
Effect of dorsal tilt of the distal radius on forearm pronation and supination motions (n = 7). (Reprinted from Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: A cadaveric study. J Hand Surg Am. 1997;22(2):258-262, with permission from Elsevier.)
Radial shortening of 5 mm or less had no effect on forearm rotation; however, shortening of 10 mm produced a mean of 47% loss of pronation (P < 0.0001) and 29% of supination ROM (P < 0.001) (Fig. 8). The average pronation angle was 46.4° (SD = 20.2°), and supination angle was 64.6° (SD = 11.3°). Radial shortening of 15 mm created ulnocarpal abutment, which effectively locked the DRUJ and prevented any forearm rotation.
Fig. 8.
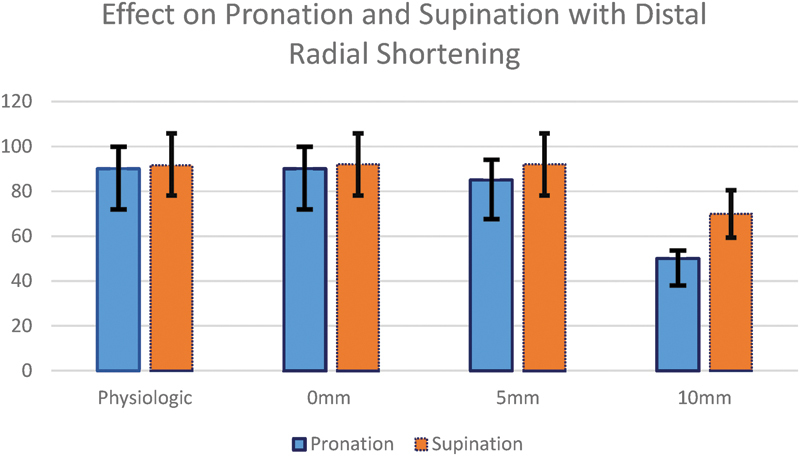
Effect of radial shortening at the distal end on forearm pronation and supination motions (n = 7: P < .01 compared with anatomic). (Reprinted from Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: A cadaveric study. J Hand Surg Am 1997;22(2):258-262, with permission from Elsevier.)
Discussion
Our results revealed that an acute loss of forearm rotation can be expected if a radius fracture at this level is allowed to heal in 5 mm or more of ulnar translation (which is an unusual clinical problem) or 10 mm or more of radial shortening, while deformities in the plane of dorsal tilt of up to 30° and radial translation of up to 10 mm have no effect on forearm rotation. Using the American Medical Association guidelines for functional impairment, our data would translate to an impairment rating of 3% for the effect of ulnar translation deformity on pronation and a combined additive rating of 10% for radial shortening of 10 mm. These numbers are only for illustrative purposes and obviously neglect the additional impairment resulting from any loss in radial and ulnar deviation or wrist flexion and extension motions, which were not measured in this study. It should also be pointed out that many of these deformities occur in combination (e.g., dorsal tilt and shortening with comminution). Our study was designed to study each deformity separately to determine its individual effect.
There has been an interest in the rotational effects of diaphyseal forearm deformities after fracture. Matthews et al10 investigated the effect of residual angulation from simulated fractures of both bones of the forearm. They found that residual angulation of less than 10° in midshaft forearm fractures does not limit forearm rotation but that angulation greater than 20° at this level contributed to a significant loss of forearm rotation. Tarr et al7 studied angular and rotatory deformities of the distal and middle diaphyseal forearm. They found a loss in pronation–supination rotation of 13%, with a 10° simulated malunion in the distal forearm and a 16% loss in rotation with the same malunion in the midforearm. Supination losses were much less affected in forearms with deformities at the distal third level, while the losses were considered drastic for middle-third deformities. They concluded that the fact that anatomic restoration of radial alignment, which is often obtained after fixation, does not always result in complete restoration of motion suggests that the residual impairment is due to soft tissue scarring. Our study would tend to agree with these conclusions by indirect deduction, since we found very few changes in motion due to distal radius malalignment in a radial direction in our specimens, which had bony deformities but unchanged soft tissues.
Footnotes
Conflict of Interest None
References
- 1.Cole J M Obletz B E Comminuted fractures of the distal end of the radius treated by skeletal transfixion in plaster cast. An end-result study of thirty-three cases J Bone Joint Surg Am 1966485931–945. [Case Reports] [PubMed] [Google Scholar]
- 2.Peltier L F Fractures of the distal end of the radius. An historical account Clin Orthop Relat Res 198418718–22. [Biography Historical Article] [PubMed] [Google Scholar]
- 3.Cooney W P III, Dobyns J H, Linscheid R L. Complications of Colles' fractures. J Bone Joint Surg Am. 1980;62(4):613–619. [PubMed] [Google Scholar]
- 4.Fernandez D L. Correction of post-traumatic wrist deformity in adults by osteotomy, bone-grafting, and internal fixation. J Bone Joint Surg Am. 1982;64(8):1164–1178. [PubMed] [Google Scholar]
- 5.Flinkkilä T, Raatikainen T, Kaarela O, Hämäläinen M. Corrective osteotomy for malunion of the distal radius. Arch Orthop Trauma Surg. 2000;120(1-2):23–26. doi: 10.1007/pl00021237. [DOI] [PubMed] [Google Scholar]
- 6.Park M J, Cooney W P III, Hahn M E, Looi K P, An K N. The effects of dorsally angulated distal radius fractures on carpal kinematics. J Hand Surg Am. 2002;27(2):223–232. doi: 10.1053/jhsu.2002.32083. [DOI] [PubMed] [Google Scholar]
- 7.Tarr R R, Garfinkel A I, Sarmiento A. The effects of angular and rotational deformities of both bones of the forearm. An in vitro study. J Bone Joint Surg Am. 1984;66(1):65–70. [PubMed] [Google Scholar]
- 8.Jupiter J B, Ruder J, Roth D A. Computer-generated bone models in the planning of osteotomy of multidirectional distal radius malunions. J Hand Surg Am. 1992;17(3):406–415. doi: 10.1016/0363-5023(92)90340-u. [DOI] [PubMed] [Google Scholar]
- 9.Crisco J J, Moore D C, Marai G E. et al. Effects of distal radius malunion on distal radioulnar joint mechanics—an in vivo study. J Orthop Res. 2007;25(4):547–555. doi: 10.1002/jor.20322. [DOI] [PubMed] [Google Scholar]
- 10.Matthews L S, Kaufer H, Garver D F, Sonstegard D A. The effect on supination-pronation of angular malalignment of fractures of both bones of the forearm. J Bone Joint Surg Am. 1982;64(1):14–17. [PubMed] [Google Scholar]


