Abstract
AIM: To assess the current clinical evidence of the effectiveness of Xiangshaliujunzi Decoction (XSLJZD) for the treatment of diabetic gastroparesis (DGP).
METHODS: Randomized controlled trials (RCTs) were retrieved from seven major electronic databases including Medline, the Cochrane Library, Embase, Chinese Biomedical Literature Database (CBM), Chinese National Knowledge Infrastructure, Chinese Scientific Journal Database (VIP), and Wanfang Databases, using search dates from the beginning of the databases to May 2013. No language limitations were applied. We included RCTs that used XSLJZD or a modified XSLJZD compared with a control group for the treatment of DGP. The control groups included conventional treatment (Western medicinal treatment), placebo, and no treatment (blank), but not acupuncture. The main outcome index was clinical effectiveness, which was based on the gastric emptying test and variations in the gastrointestinal (GI) symptoms between the treatment and control groups after intervention. Data extraction, analysis, and quality assessment were conducted according to the Cochrane Handbook for Systematic Review of Interventions, Version 5.1.0.
RESULTS: Ten RCTs involving 867 patients (441 in the experimental groups, and 426 in the control groups) were identified, and the overall methodological quality was evaluated as generally low. In the treatment groups, all 10 trials used herbs alone as the treatment, whereas all control groups used prokinetic medicine. The period of intervention ranged from 2 to 8 wk. Three classes were used to evaluate treatment efficacy: significant effective, effective, and ineffective, and all trials used the clinical effective rate (based on the gastric emptying test and changes in GI symptoms) to evaluate efficacy. The data showed that the effects of XSLJZD for the treatment of DGP were superior to the control group (n = 867, RR =1.33, 95%CI: 1.24-1.42, Z = 8.11, P < 0.00001). Two trials recorded adverse events, and one trial reported follow-up.
CONCLUSION: XSLJZD could restore the gastric emptying rate and improve symptoms. However, the evidence remains weak due to the poor methodological quality of the included studies.
Keywords: Diabetic gastroparesis, Xiangshaliujunzi Decoction, Gastric emptying rate, Gastrointestinal symptoms, Systematic review
Core tip: This article is a systematic review of Xiangshaliujunzi Decoction (XSLJZD), which is used in traditional Chinese medicine to treat stomach discomfort and diabetic gastroparesis. This article aims to evaluate the efficacy of XSLJZD for the treatment of diabetic gastroparesis. The incidence of diabetes has increased significantly, and so it is necessary to take active steps to prevent and treat diabetic complications. The clinical manifestations of diabetic gastroparesis are extremely apparent. Traditional Chinese medicine, an alternative approach for improving the symptoms of patients, has specific advantages and so it its efficacy should be carefully assessed. In addition to the improvement of patient symptoms and clinical indications, improved quality of life is of interest of this article.
INTRODUCTION
Delayed gastric emptying affects a substantial proportion of patients with long-standing diabetes. Kassander used the term ‘‘gastroparesis diabeticorum’’ to describe abnormally increased gastric retention in these patients in 1958[1]. The American Gastroenterological Association and the American Nuclear Medicine Society define gastroparesis as a syndrome characterized by delayed gastric emptying in the absence of mechanical obstruction[1]. Patients often present with upper gastrointestinal symptoms such as early satiety, weight loss, abdominal bloating, abdominal discomfort, nausea, frequent vomiting, and impaired glycemic control. As such, quality of life is severely impacted[2]. Symptoms attributed to gastroparesis are reported by 5%-12% of patients with diabetes[3]. Several diabetic abnormalities could result in gastric motor dysfunction including autonomic neuropathy, enteric neuropathy involving excitatory and inhibitory nerves, abnormalities of the interstitial cells of Cajal, acute fluctuations in blood glucose, incretin-based medications, and psychosomatic factors[4]. The disorder can range from being mildly symptomatic to having severe symptoms leading to malnutrition, electrolyte imbalance, and impaired glycemic control[5].
Gastroparesis is increasingly being recognized as a significant health problem. Based on blood glucose control, the available treatment options of modern medicine include nutritional support, improvement of gastric emptying using prokinetics, control of symptoms, and the use of a gastric electric stimulator[6,7]. Medications for gastroparesis include metoclopramide, domperidone, cisapride, and erythromycin. However, these agents are of only limited efficacy, and many patients cannot tolerate them because of their side effects[8,9]. Surgical procedures, such as gastrectomy and antrectomy, are the last treatment options, but are controversial and need additional studies[10,11]. Providing nutritional support such as Jejunostomy tube feeding cannot cure gastroparesis[12]. Considering the high recurrence rate and the increasing incidence of diabetic gastroparesis (DGP)[13,14], finding drugs that show efficacy for the treatment of DGP are necessary.
Xiangshaliujunzi Decoction (XSLJZD) is, a traditional Chinese medicinal herbal containing eight commonly used herbs (Panax ginseng, Rhizoma atractylodis macrocephalae, Poria, Radix glycyrrhizae, Pericarpium citri reticulatae, Pinellia tuber, Fructus amomi, and Radix aucklandiae). It has long been used to treat gastrointestinal discomfort in clinical practice in China[15-19]. Its mechanism of action could be related to invigorating the spleen to resolve dampness, regulate the stomach, facilitate elimination and supplement to restore Qi based on the theory of Traditional Chinese Medicine (TCM)[20,21]. Recent studies revealed that XSLJZD could regulate gastrointestinal motility[22,23]. Biochemically, XSLJZD also increases the secretion of plasma motilin, lowers serum gastrin levels, and enhances smooth muscle contraction by increasing calcium levels[24-27].
Currently, we use XSLJZD as an alternative method for the treatment of DGP[28,29]. Several studies have suggested that XSLJZD is an effective treatment for DGP, but data are not yet definitive. This systematic review aims to assess the current clinical evidence for the efficacy of XSLJZD for the treatment of DGP by conducting literature reviews in databases for randomized controlled trials (RCTs).
MATERIALS AND METHODS
Databases and searches
A computer-based online search was conducted in the Medline, Cochrane Library, Embase, Chinese Biomedical Literature Database (CBM), Chinese National Knowledge Infrastructure, Chinese Scientific Journal Database (VIP), and Wanfang databases. The search terms used were (“diabetic gastroparesis” OR “gastrointestinal changes” OR “gastrointestinal disease”) AND (“herb” OR “Xiangshaliujunzi Decoction” OR “Xiangshaliujunzi” OR “Xiangshaliujunzi Tang”) AND (“randomized controlled trial” OR “controlled clinical trial” OR “random” OR “randomly” OR “randomized” OR “control”). We searched all articles that were published prior to May 2013.
Study selection
The RCTs included were restricted to those that compared XSLJZD as the treatment with a control group. We evaluated all forms of XSLJZD, such as XSLJZD and modified XSLJZD, whereas the control groups included conventional treatment (western medicinal treatment), placebo, and no treatment (blank), but not acupuncture. Studies that evaluated DGP patients were included regardless of gender, age, or nationality, but patients with other gastrointestinal diseases were excluded. The main outcome was clinical effectiveness, which was based on the gastric emptying test and variations in gastrointestinal (GI) symptoms. Studies used a 50% gastric emptying time. Any adverse events were also recorded. Duplicated publications reporting the same groups of patients were excluded.
Data extraction and quality assessment
Two authors carried out the literature searches (Tian JX, Li M), study selection (Tian JX, Liao JQ), and data extraction (Li M, Liao JQ) independently. The extracted data included the title of study, the authors, the year of publication, sample size, the gender and age of the participants, the names and components of the Chinese herbs, the details of the control interventions, the treatment process, outcomes, adverse effects, and details of the methods used. Discrepancies were resolved by consensus through discussion between the two authors and, if needed, by asking for additional information from a third party (Tong XL). The methodological quality of trials was assessed by two authors (Tian JX and Liu WK) independently based on the criteria from the Cochrane Handbook for Systematic Review of Interventions, Version 5.1.0[30]. Assessed parameters included random sequence generation (selection bias), allocation concealment (selection bias), the blinding of participants and personnel (performance bias), the blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. We judged each item on three levels (“Yes” for low bias, “No” for a high risk of bias, and “Unclear”). Then, we assessed the trials and categorized them into three levels: low risk of bias (all the items were categorized “Yes”), high risk of bias (at least one item ranked “No”), and unclear risk of bias (at least one item was “Unclear”).
Statistical analysis
RevMan 5.1 software was used for data analyses, which was offered by the Cochrane collaboration. Dichotomous data were expressed as relative risk (RR), and continuous outcomes as weighted mean difference (WMD), both with 95%CI. Heterogeneity was assessed using the I2 test with a significance level set at I2 over 50% or P < 0.1. If there was no heterogeneity (I2 < 50%) we selected the fixed effect model. Possible causes of heterogeneity (I2 > 50%) were explained using the random effects model. Publication bias was explored by funnel plot analysis if sufficient studies were found[30].
RESULTS
Description of studies
A total of 72 studies were initially identified from the electronic databases. The search results are summarized in Figure 1. After screening the titles and abstracts, 51 potentially relevant studies were found. However, most of these were excluded due to repetition, retrospective studies, animal studies, case reports, and literature reviews. Thirty-seven studies were excluded because of duplicated publications, three were excluded because they were animal studies, and the remaining 11 were non-controlled clinical trials including retrospective studies, case reports, and literature reviews. After a detailed evaluation of the full text, a further 11 studies were excluded. Three trials predominantly used Liujunzi decoction, which is similar to XSLJZD, two did not clarify the intervention used in the control group, three were excluded because they only reported the differences after treatment, and three trials were not in accordance with our inclusion criteria. Finally, 10 studies involving 867 patients were in accordance with our inclusion criteria without meeting the exclusion criteria. All studies were conducted in China and published in Chinese between 2003 and 2012. The bibliographic details of the included studies are shown in Table 1.
Figure 1.
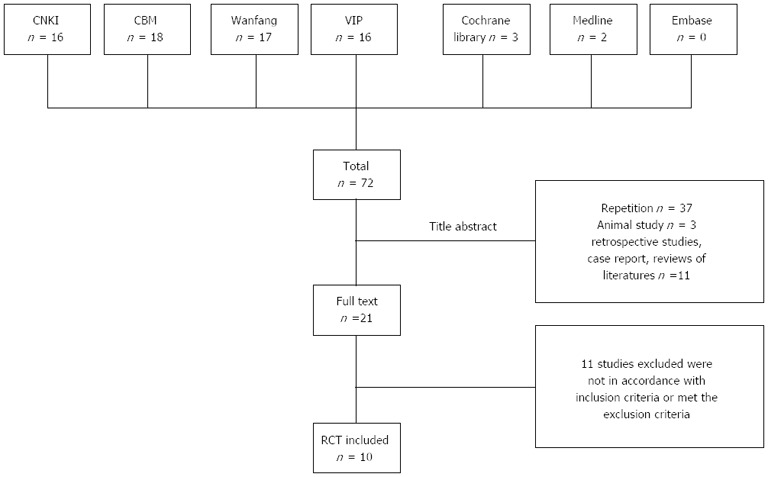
Flow chart of the trial selection process. CNKI: Chinese National Knowledge Infrastructure; CBM: China BioMedical Literature; VIP: VIP Database for Chinese Technical Periodicals; RCT: Randomized controlled trial.
Table 1.
Characteristics of included randomized controlled trials
| Trials | Sample size | Gender (E/C) | Experimental group | Control group | Period | Outcome measure | Balance report of baseline |
| Cai[31] | 54 (27/27) | (15M:12F)/(14M:13F) | Modified Xiangshaliujunzi Decoction, bid | Metoclopramide (10 mg, tid) | 4 W | Clinical effective rateGastric emptying testGI symptomsAdverse events | P > 0.05 |
| Feng[32] | 128 (64/64) | (30M:34F)/(34M:30F) | Modified Xiangshaliujunzi Decoction, bid | Cisapride (10 mg, tid), Metoclopramide (10 mg, bid) | 4 W | Clinical effective rateGI symptoms | P > 0.05 |
| Guo et al[33] | 62 (32/30) | (35M:27F) | Modified Xiangshaliujunzi Decoction, bid | Domperidone (10 mg, tid) | 8 W | Clinical effective rateGI symptoms | P > 0.05 |
| Lu[34] | 94 (48/46) | (28M:20F)/(24M:22F) | Modified Xiangshaliujunzi Decoction, bid | Domperidone (10 mg, tid) | 4 W | Clinical effective rateGI symptoms | P > 0.05 |
| Lu et al[35] | 142 (72/70) | (30M:42F)/(31M:39F) | Modified Xiangshaliujunzi Decoction, bid | Mosapride (5 mg, tid) | 4 W | Clinical effective rateGastric emptying testGI symptoms | P > 0.05 |
| Meng[36] | 62 (32/30) | (15M:17F)/(14M:16F) | Modified Xiangshaliujunzi Decoction, bid | Cisapride (10 mg, tid), Metoclopramide (10 mg, bid) | 4 W | Clinical effective rateGI symptoms | P > 0.05 |
| Wen[37] | 87 (44/43) | (25M:19F)/(23M:20F) | Modified Xiangshaliujunzi Decoction, bid | Cisapride (5 mg, tid) | 4 W | Clinical effective rateGastric emptying testGI symptomsAdverse events | No significant differences |
| Dai[38] | 70 (36/34) | (22M:14F)/(20M:14F) | Modified Xiangshaliujunzi Decoction, bid | Domperidone (10 mg, tid) | 3 W | Clinical effective rate Gastric emptying testGI symptoms | P > 0.05 |
| Ji[39] | 56 (30/26) | (14M:16F)/(12M:14F) | Modified Xiangshaliujunzi Decoction, bid | Domperidone (10 mg, tid) | 2 W | Clinical effective rateGI symptoms | No significant differences |
| Hou et al[40] | 112 (56/56) | (44M:12F)/(43M:13F) | Modified Xiangshaliujunzi Decoction, bid | Domperidone (10 mg, tid) | 8 W | Clinical effective rateGastric emptying testGI symptoms | P > 0.05 |
GI: Gastrointestinal; M: Male; F: Female.
Among the 10 studies, all participants came from the inpatient and/or outpatient Department of Gastroenterology or Endocrinology, and the experimental interventions were oral administration. The trials included 473 male and 394 female subjects with ages ranging from 30 to 85 years. The diagnostic criteria of the studies were as follows: seven trials[31-37] described the World Health Organization diabetes mellitus (DM) diagnostic criteria involving a certain duration of gastrointestinal discomfort such as postprandial fullness, nausea, vomiting, bloating, and delayed gastrointestinal emptying in the absence of other gastrointestinal diseases. Two trials[38,39] described DM that was diagnosed with a certain duration of gastrointestinal discomfort such as postprandial fullness, nausea, vomiting, bloating, and delayed gastrointestinal emptying in the absence of other gastrointestinal diseases. Finally, one trial[40] described matching the “Interpretation of TCM prevention Guide for diabetes”[41].
All 10 trials used herbals alone (modified XSLJZD) as the treatment group. In the control group, all studies used prokinetic medicine alone: one used Cisapride, one used Mosapride, and the others used Domperidone. The period of intervention ranged from 2 to 8 wk. Three classes were used to describe the treatment efficacy: significantly effective, effective, and ineffective. In addition, all trials used the clinical effective rate (including significant effective and effective) based on the gastric emptying test (50% emptying time) and variations in GI symptoms to evaluate efficacy, which was the main outcome index. Adverse events were also recorded.
Methodological quality of included trials
The quality assessments are summarized in Table 2. The sample size of the included trials varied from 50 to 150 patients. None of the 10 studies reported details for sample size calculation, and none were double-blinded placebo controlled studies. One study described adequate methods of randomization using random number tables[40], whereas the remaining nine simply reported “randomly allocating” participants as the method of randomization. No trials had clear a description of the method used for allocation concealment or the blinding procedures. All trials described the patient characteristics, and described similarities between comparison groups at baseline, but none reported the loss of any participants, which made it difficult to determine whether these studies had an attrition bias. Two trials reported adverse events, and one trial[34] reported follow-up. The methodological quality of the included studies was determined to be generally low according to the predefined quality assessment criteria, which indicated that further investigations might influence the confidence intervals of the meta-analysis, and the results would likely be reversed.
Table 2.
Quality assessment of included randomized controlled trials
| Trials | Randomization | Allocation concealment | Blinding of participants and personnel | Blinding of assessors | Incomplete outcome data | Selective reporting | Other sources of bias | Risk of bias |
| Cai[31] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Feng[32] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Guo et al[33] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Lu[34] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Lu et al[35] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Meng[36] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Wen[37] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Dai[38] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Ji[39] | Unclear | Unclear | High | Unclear | Yes | No | Unclear | High |
| Hou et al[40] | Table of random number | Unclear | High | Unclear | Yes | No | Unclear | Unclear |
Effect of the interventions
All the included studies compared the clinically effective rate between the treatment and control groups after intervention, which was based on the variations in the gastric emptying test and GI symptoms. Three classes were used to evaluate the effects of treatment: significant effective, effective, and ineffective. The total effective rate was the combination of the significant effective and effective rate, which was considered to be the main outcome index. The included trials exhibited homogeneity in the consistency of their results (χ2 = 12.99, P = 0.16, I2 = 31%). Thus, the fixed-effects model should be used for statistical analysis, and the treatment group scored significantly higher than the control group (n = 867, RR= 1.33, 95%CI: 1.24-1.42, Z = 8.11, P < 0.00001) (Figure 2).
Figure 2.
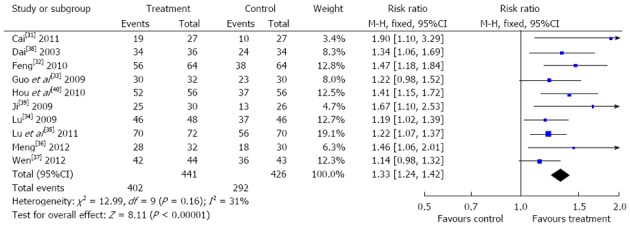
Effective rates of comparison between Xiangshaliujunzi Decoction and the control group.
Publication bias
Funnel plots based on the data of the effective rate are shown in Figure 3. The Figure was asymmetrical, which indicated that publication bias might influence the results of our analysis. Although we carried out comprehensive searches and tried to avoid bias, since all trials were published in Chinese we could not exclude potential publication bias.
Figure 3.
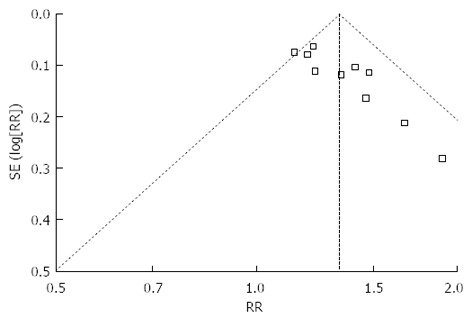
Funnel plot of publication bias.
Adverse events
Two trials[31,37] described safety reports: the control groups reported that one patient suffered from nausea, two with stomachache, one with headache, one with diarrhea, and four reported skin allergies. In treatment group there was only one report of an adverse effect, which was a patient with stomachache. All the side effects were cured spontaneously.
Follow-up
Only one trial[34] reported follow-up. Lu et al[34] reported that two patients reported recurrence 3 months after treatment, with a recurrence rate of 4.2%. In contrast, the recurrence rate in the control group was 28.3%, involving 13 patients. The difference between treatment group and control group was statistically significant (P < 0.01).
DISCUSSION
Disturbances in gastrointestinal motility with associated symptoms have long been recognized as a complication of diabetes mellitus, and typically develop after diabetes mellitus has been established for several years[1]. Once established, DGP tends to persist despite improvement of glycemic control[42], which reduces the quality of life for affected patients[3]. However, current management strategies are far from clinically satisfactory[10]. It was demonstrated that Chinese herbal medicines could not only promote gastric emptying, but also improve symptoms. Because XSLJZD is widely used to treat gastrointestinal discomfort in clinical practice[29,30], this study aimed to assess the current clinical evidence of the effectiveness of XSLJZD for the treatment of DGP.
We did not find many systematic reviews reporting the use of Chinese herbal medicines to treat DGP. This systematic review included 10 randomized trials and a total of 867 participants. The main findings of this study were that XSLJZD demonstrated potential effects on the promotion of gastric emptying (n = 867, RR = 1.33, 95%CI: 1.24-1.42, Z = 8.11, P < 0.00001) compared with the control group. However, the methodological quality of the trials was assessed to be generally low. Before reaching definitive conclusions, the following weaknesses must be considered.
None of the studies reported sample size calculations, and the efficacy could not be clarified on some outcome measurements due to the small number of studies. Thus, the reliability of the outcome might be questionable. All trials lacked a description of the methods used for randomization. Only one study mentioned the random form (Hou), whereas the others simply mentioned “randomly allocating” subjects with no additional information. Therefore, it is difficult to ascertain whether these studies were adequately randomized. In addition, no studies described allocation concealment, which may introduce some false “RCTs” in the review, which could mislead the results. We tried to contact the authors for further information about the trials, but we were unable to obtain any additional information. No studies described the method used for blinding, which could lead to performance and detection bias for subjective outcome measures if researchers were aware which patients were in the therapeutic intervention group.
DGP is a disease with complicated symptoms. The gastric emptying test is the gold standard for DGP diagnosis. However, patients that suffer from severe nausea and vomiting are unable to endure the test, which would leave any studies of DGP with a limited number of participants. We suggest that the scope of included patients should be expanded, specifically to include severe gastroparesis patients who could not undergo the gastric emptying test. Vomiting time and duration can be auxiliary indicators that could provide stronger evidence for wider clinical applications.
Gastrointestinal discomfort is the most important clinical characteristic, and improving the symptoms based on the gastric emptying are important for the evaluation of DGP. This is distinct from blood pressure, lipids, and blood sugar, which are expressed by specific numerical indices. This makes the determination of efficacy of gastrointestinal lesions complicated. The improvement of symptoms also needs to be standardized and quantified. The studies included in this review lacked a unified syndrome questionnaire to allow us to evaluate symptomatic variations in the syndrome. The Gastroparesis Cardinal Symptom Index is widely used to evaluate gastrointestinal lesions[43], but none of the included studies used this questionnaire. Thus, it is critical to standardize the evaluation of gastrointestinal lesions, which could help improve the consistency of future studies.
Only two studies[31,37] mentioned adverse effects including nausea, stomachache, headache, diarrhea, and skin allergies. Safety is a serious concern that should be recorded in detail. Thus, definitive conclusions about the safety of XSLJZD still cannot be drawn. No trials reported the loss of participants or used the intention to treat method, which made it difficult to determine whether these studies had attrition bias. Only one trial[34] reported follow up. Diabetic gastrointestinal disease can easily recur, and so long-term follow-up is required for accurate analysis. We tried to avoid language and location bias, but all the included studies were published in China, and so we cannot exclude potential publication bias.
In conclusion, we found that XSLJZD could improve the gastric emptying rate and improve diabetic gastrointestinal symptoms, and could therefore be considered as an alternative method for the treatment of DGP. However, there is no established efficacy determination system for assessing the use of TCM to treat DGP. The long-term efficacy and safety of XSLJZD for the treatment of DGP remains uncertain, because the methodological quality was generally low, and some possible bias existed. The results of our analysis should therefore be read with caution. Therefore, an efficacy determination system for using TCM to treat DGP should be established soon. The accumulation of clinical evidence of severe gastroparesis is increasingly necessary, and future studies should include improved randomization, safety reports, detailed follow-up, and blinded methods to improve their quality. Well-designed, large-scale, and high-quality randomized controlled clinical trials with scientific rigor are required to provide additional evidence.
COMMENTS
Background
Diabetic gastroparesis can cause stomach discomfort and significantly affect the patient’s quality of life. Traditional Chinese Medicine (TCM) has advantages for improving gastric emptying, particularly for the relief of symptoms. However, there are few systematic reviews of the use of TCM to improve diabetic gastroparesis. This study aimed to evaluate the efficacy of TCM Xiangshaliujunzi Decoction (XSLJZD) for the treatment of diabetic gastroparesis, and provide new options for the clinical diagnosis and treatment of diabetic gastroparesis (DGP).
Research frontiers
Research showed that XSLJZD could regulate gastrointestinal motility. Biochemically, XSLJZD also increases the secretion of plasma motilin, lowers serum gastrin levels, and enhances smooth muscle contraction by increasing calcium levels. This study aimed to evaluate XSLJZD for the treatment of gastric emptying disorders and relieving the symptoms of diabetic gastroparesis.
Innovations and breakthroughs
Few previous studies focused on systematic reviews of TCM for the treatment of diabetic gastroparesis. This study evaluated the effects of XSLJZD in diabetic gastroparesis. As the incidence of diabetes increases, the early prevention of diabetes-related complications is particularly important. The current modern medical treatments for diabetic gastroparesis are being explored and improved. This study explored the efficacy of XSLJZD for improving gastric emptying and stomach symptoms in patients with diabetic gastroparesis from the perspective of TCM. It should provide novel ideas and information for the diagnosis and treatment of diabetic gastroparesis.
Applications
Patients with diabetic gastroparesis symptoms are often plagued by stomach discomfort, severe nausea and vomiting, water and electrolyte imbalance, and the loss of nutrients, which can even be life-threatening. In this study, the authors assessed existing clinical studies, which suggest that TCM is a viable alternative treatment method that could improve the symptoms of diabetic gastroparesis. It may also improve the treatment of disease and improve the quality of life for patients.
Terminology
DGP is abnormal gastric retention caused by long-term diabetes. The mechanism of action of TCM in this model may be related to invigorating the spleen to resolve dampness, regulating the stomach, and promote gastric emptying and supplementation to restore Qi.
Peer review
This meta-analysis focuses on the Chinese herbal medicine XSLJZD and its clinical efficacy for the treatment of diabetic gastroparesis. This study evaluates the clinical efficacy of a traditional medicine, and the information obtained from this meta-analysis could enhance our understanding of XSLJZD for the treatment of diabetic gastroparesis.
Footnotes
Supported by National Natural Science Foundation of China, No. 81173259; and National Basic Research Program of China, 973 Program, No. 2010CB530600
P- Reviewers: Choi SM, Du P, Liu J S- Editor: Zhai HH L- Editor: A E- Editor: Wang CH
References
- 1.Parkman HP, Camilleri M, Farrugia G, McCallum RW, Bharucha AE, Mayer EA, Tack JF, Spiller R, Horowitz M, Vinik AI, et al. Gastroparesis and functional dyspepsia: excerpts from the AGA/ANMS meeting. Neurogastroenterol Motil. 2010;22:113–133. doi: 10.1111/j.1365-2982.2009.01434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thazhath SS, Jones KL, Horowitz M, Rayner CK. Diabetic gastroparesis: recent insights into pathophysiology and implications for management. Expert Rev Gastroenterol Hepatol. 2013;7:127–139. doi: 10.1586/egh.12.82. [DOI] [PubMed] [Google Scholar]
- 3.Bytzer P, Talley NJ, Leemon M, Young LJ, Jones MP, Horowitz M. Prevalence of gastrointestinal symptoms associated with diabetes mellitus: a population-based survey of 15,000 adults. Arch Intern Med. 2001;161:1989–1996. doi: 10.1001/archinte.161.16.1989. [DOI] [PubMed] [Google Scholar]
- 4.Camilleri M, Bharucha AE, Farrugia G. Epidemiology, mechanisms, and management of diabetic gastroparesis. Clin Gastroenterol Hepatol. 2011;9:5–12; quiz e7. doi: 10.1016/j.cgh.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khoo J, Rayner CK, Jones KL, Horowitz M. Pathophysiology and management of gastroparesis. Expert Rev Gastroenterol Hepatol. 2009;3:167–181. doi: 10.1586/egh.09.10. [DOI] [PubMed] [Google Scholar]
- 6.Abell TL, Bernstein RK, Cutts T, Farrugia G, Forster J, Hasler WL, McCallum RW, Olden KW, Parkman HP, Parrish CR, et al. Treatment of gastroparesis: a multidisciplinary clinical review. Neurogastroenterol Motil. 2006;18:263–283. doi: 10.1111/j.1365-2982.2006.00760.x. [DOI] [PubMed] [Google Scholar]
- 7.Aljarallah BM. Management of diabetic gastroparesis. Saudi J Gastroenterol. 2011;17:97–104. doi: 10.4103/1319-3767.77237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kashyap P, Farrugia G. Diabetic gastroparesis: what we have learned and had to unlearn in the past 5 years. Gut. 2010;59:1716–1726. doi: 10.1136/gut.2009.199703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pasricha PJ, Pehlivanov N, Sugumar A, Jankovic J. Drug Insight: from disturbed motility to disordered movement--a review of the clinical benefits and medicolegal risks of metoclopramide. Nat Clin Pract Gastroenterol Hepatol. 2006;3:138–148. doi: 10.1038/ncpgasthep0442. [DOI] [PubMed] [Google Scholar]
- 10.Arts J, Holvoet L, Caenepeel P, Bisschops R, Sifrim D, Verbeke K, Janssens J, Tack J. Clinical trial: a randomized-controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment Pharmacol Ther. 2007;26:1251–1258. doi: 10.1111/j.1365-2036.2007.03467.x. [DOI] [PubMed] [Google Scholar]
- 11.Friedenberg FK, Palit A, Parkman HP, Hanlon A, Nelson DB. Botulinum toxin A for the treatment of delayed gastric emptying. Am J Gastroenterol. 2008;103:416–423. doi: 10.1111/j.1572-0241.2007.01676.x. [DOI] [PubMed] [Google Scholar]
- 12.Malagelada JR, Distrutti E. Management of gastrointestinal motility disorders. A practical guide to drug selection and appropriate ancillary measures. Drugs. 1996;52:494–506. doi: 10.2165/00003495-199652040-00003. [DOI] [PubMed] [Google Scholar]
- 13.Punkkinen J, Färkkilä M, Mätzke S, Korppi-Tommola T, Sane T, Piirilä P, Koskenpato J. Upper abdominal symptoms in patients with Type 1 diabetes: unrelated to impairment in gastric emptying caused by autonomic neuropathy. Diabet Med. 2008;25:570–577. doi: 10.1111/j.1464-5491.2008.02428.x. [DOI] [PubMed] [Google Scholar]
- 14.Wang YR, Fisher RS, Parkman HP. Gastroparesis-related hospitalizations in the United States: trends, characteristics, and outcomes, 1995-2004. Am J Gastroenterol. 2008;103:313–322. doi: 10.1111/j.1572-0241.2007.01658.x. [DOI] [PubMed] [Google Scholar]
- 15.Bi JH, Yang TR. The experimental research of xiangshaliujunzi tang and its separated formulae on pepsin, SOD and MDA content of spleen deficiency gastric ulcer model rats. Nanjing Zhongyiyao Daxue Xuebao. 2010;26:280–282. [Google Scholar]
- 16.Wen YH, Liang S, Liang ZS, Zhang ZR, Zheng Q, Yang HL. The effect of Xiangshaliujunzi Decoction to acute gastric mucosal injury. Guangdong Yixue. 2007;28:30–32. [Google Scholar]
- 17.Wang J, Huang SP, Zhao XQ, Chen Y. Gastric hypersensitivity and the variation of Mucosa substance P, 5-HT in functional dyspepsia. Xinzhongyi. 2012;44:42–44. [Google Scholar]
- 18.Chen J, Li ZZ, Miao WH, Yang CG. Xiangshaliujunzi decoction treating 60 gastric cancer patients in Qi deficiency. Shaanxi Zhongyi Xueyuan Xuebao. 2006;27:1231–1232. [Google Scholar]
- 19.Gao Y. Moderated Xiangshaliujunzi decoction treating Helicobacter pylori-associated gastritis. Shizhen Guoyi Guoyao. 2011;22:1283–1284. [Google Scholar]
- 20.Pan ZL, Pan XG, Pan XD. The Clinical application of Xiangshaliujunzi Decoction in stomach illness. Zhongyi Zazhi. 2009;50:65. [Google Scholar]
- 21.Yi PY, Zhu FS. Traditional Chinese Medicine therapy and decoction application in chronic atrophic gastritis. Shijie Huaren Xiaohua Zazhi. 2011;19:3696–3699. [Google Scholar]
- 22.Zhang ZH. The Pharmacology and clinical application of Xiangshaliujunzi decoction. Liaoning Zhongyiyao Daxue Xuebao. 2013;15:245–247. [Google Scholar]
- 23.Kang LN, Lin XL. The Pharmacology and clinical application of Xiangshaliujunzi decoction in resent 10 years. Jiangxi Zhongyi Xueyuan Xuebao. 2010;41:67–69. [Google Scholar]
- 24.Zhang XP, Sun SJ. The effect of moderated Liujunzi decoction to plasma motilin in functional dyspepsia. Zhongyi Zazhi. 2002;43:517–519. [Google Scholar]
- 25.Liu K, Qi QH. Conduction disturbances of gastric motilin in spleen-qi deficiency syndrome. Zhongguo Zhongxiyi Jiehe Waike Zazhi. 2004;10:300–302. [Google Scholar]
- 26.Chen FJ, Qian JH. The impact of Integrative Medicine to gastric motilin in critically ill patients with gastrointestinal dysfunction. Zhongguo Zhongyi Jizheng. 2009;18:505–506. [Google Scholar]
- 27.Li J, Liu B, Li FY. The impact of Xiangshaliujunzi decoction to the animal model of spleen deficient gastric uler rat. Liaoning Zhongyiyao Daxue Xuebao. 2008;35:34–35. [Google Scholar]
- 28.Wang WP. Xiangshaliujunzi decoction treating Diabetic gastroparesis. Jiceng Yixue Luntan. 2004;8:144–145. [Google Scholar]
- 29.Ye JQ. Xiangshaliujunzi decoction combined with Banxiaxiexin decoction treating Diabetic gastroparesis. Neimenggu Zhongyiyao. 2012;(16):13. [Google Scholar]
- 30.Higgins JPT. Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1. 0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from: http://www. cochrane-handbook. org.
- 31.Cai D. Xiangshaliujunzi decoction treating Diabetic gastroparesis. (Master Thesis) Hubei University of Chinese Medicine, Wuhan, China. 2011. [Google Scholar]
- 32.Feng ML. Moderated Xiangshaliujunzi decoction treating 64 Diabetic gastroparesis patients. Zhongguo Zhongyiyao Xinxi Zazhi. 2010;2:59. [Google Scholar]
- 33.Guo QH, Zhai LL. Moderated Xiangshaliujunzi decoction treating 32 Diabetic gastroparesis patients. Yunnan Zhongyi Zhongyao Zazhi. 2009;30:31. [Google Scholar]
- 34.Lu YW. Moderated Xiangshaliujunzi decoction treating Diabetic gastroparesis. Liaoning Zhongyiyao Daxue Xuebao. 2009;11:136–137. [Google Scholar]
- 35.Lu YC, Yu XL. Xiangshaliujunzi decoction combined with Xuanfudaizhe decoction treating 72 Diabetic gastroparesis patients. Jiangsu Zhongyiyao. 2011;43:42–43. [Google Scholar]
- 36.Meng YF. Moderated Xiangshaliujunzi decoction treating 32 Diabetic gastroparesis patients. Zhongwai Jiankang Wenzhai. 2012;9:414. [Google Scholar]
- 37.Wen ZQ. Moderated Xiangshaliujunzi decoction treating 44 Diabetic gastroparesis patients. Zhongguo Linchuang Yanjiu. 2012;25:608–609. [Google Scholar]
- 38.Dai BH. Moderated Xiangshaliujunzi decoction treating 36 Diabetic gastroparesis patients. Hebei Zhongyi. 2003;25:809–810. [Google Scholar]
- 39.Ji ML. Moderated Xiangshaliujunzi decoction treating Diabetic gastroparesis. Shanxi Yiyao Zazhi. 2009;38:622. [Google Scholar]
- 40.Hou JZ, Zhang Q, Yan GH. Moderated Xiangshaliujunzi decoction treating 56 Diabetic gastroparesis patients. Xinzhongyi. 2010;42:17–19. [Google Scholar]
- 41.Tong XL. Interpretation of Traditional Chinese medicine prevention guide for diabetes. China: Chinese Medicine Press; 2009. pp. 166–167. [Google Scholar]
- 42.Jones KL, Russo A, Berry MK, Stevens JE, Wishart JM, Horowitz M. A longitudinal study of gastric emptying and upper gastrointestinal symptoms in patients with diabetes mellitus. Am J Med. 2002;113:449–455. doi: 10.1016/s0002-9343(02)01228-7. [DOI] [PubMed] [Google Scholar]
- 43.Revicki DA, Rentz AM, Dubois D, Kahrilas P, Stanghellini V, Talley NJ, Tack J. Development and validation of a patient-assessed gastroparesis symptom severity measure: the Gastroparesis Cardinal Symptom Index. Aliment Pharmacol Ther. 2003;18:141–150. doi: 10.1046/j.1365-2036.2003.01612.x. [DOI] [PubMed] [Google Scholar]


