Abstract
Aim
To study the prevalence, clinicopathological and radiological correlations of epithelial lacrimal gland tumors and compare these with similar published literature. The study was also designed to look at the natural history of benign mixed tumors (BMT) in regard to recurrence and malignant degeneration.
Methods
This was a retrospective study of all suspected epithelial tumors of the lacrimal gland surgically excised at King Khaled Eye Specialist Hospital (KKESH) for the period: 1983–2008. Exclusion criteria included structural lesions (dacryops) and inflammatory lesions. We included 26 cases of epithelial lacrimal gland tumors (from 24 patients). The histopathologic slides and the radiologic findings were reviewed. The corresponding demographic and clinical data were obtained by chart review using a data sheet.
Results
BMT accounted for 12/26 of the lesions while malignant lesions including adenoid cystic carcinoma (ACC) were more common (14/26). The mean age was 44.27 years (range 12–75). Commonest clinical presentation was proptosis. Median duration of symptoms in the BMT cases was 30 months and 7 months in the ACC group. The 12 BMT cases were primary in 9 and recurrent in 3 patients. The 11 ACC cases showed mostly cribriform pattern and low histopathologic grade. We had 2 cases of malignant mixed tumor (MMT) one of which arising in a recurrent tumor. One case of primary mucoepidermoid carcinoma with histopathologic grade 2 was noted. Radiologically, a well-defined appearance with bone remodeling was observed in BMT in contrast to invasive appearance with destruction in malignant lesions.
Conclusion
Our series information indicated a different distribution of benign and malignant epithelial lesions with a slightly higher rate of malignancy. BMT was the commonest benign tumor where recurrence was a squeal of incomplete surgical excision. ACC was the commonest malignant tumor with shorter duration of symptoms and radiologic evidence of invasiveness that correlated with the histopathologic features.
Keywords: Lacrimal gland, Tumor, Carcinoma, Adenoma, Adenocarcinoma
Introduction
Lacrimal gland tumors are considered one of the challenging types of tumor which are difficult to study because of their rare incidence as they represent almost only 10% of the space occupying orbital lesions.1 They are generally divided into 4 categories: inflammatory lesions, lymphomas, metastatic cancer, and primary epithelial tumors. The most common epithelial tumors are, in order of frequency, benign mixed tumor (BMT) or pleomorphic adenoma (PA), adenoid cystic carcinoma (ACC), and adenocarcinoma (ACA). Other rare variants of carcinoma are also seen, such as mucoepidermoid carcinoma. Some of the primary malignant epithelial tumors may arise from a preexisting BMT through a malignant transformation -the so called carcinoma ex pleomorphic adenoma (Ca ex PA), pleomorphic adenocarcinoma, or malignant mixed tumor (MMT) but most arise de novo. Because of rarity of these epithelial lacrimal gland tumors, most published articles describe single cases or small series, and only few large series have been reported in the English-language literature. The correlation of the histopathologic and radiologic features to the clinical presentation is important to diagnose different types of tumor and their behavior. Another important point is that lacrimal gland tumors have not been studied in detail before in our population. The aim of our study is to identify the distribution of different histologic types of primary epithelial lacrimal gland tumors in our population and to correlate the clinical, histopathologic and radiologic features of such tumors surgically treated at our tertiary referral center.
Methods
The clinical, histopathologic and radiologic data of all suspected epithelial tumors of the lacrimal gland surgically excised at King Khaled Eye Specialist Hospital (KKESH) for the period: 1983–2008 were included. A single pathologist reviewed the histopathologic slides. A single radiologist also reviewed the radiologic findings. The corresponding demographic information and clinical data were obtained by reviewing the charts of all the cases included. A specially designed Data Base Sheet was used to report all the previous information for each case. The data collected were then analyzed to calculate the prevalence of different types of epithelial lacrimal gland tumors. The correlation of the histopathologic and radiologic features to the clinical data was highlighted. Special attention was then directed toward any cases of recurrent pleomorphic adenoma to identify the pattern and occurrence of malignant change in comparison to other studies.
This study has been approved by the Human Ethics Committee-Institutional Review Board (HEC-IRB) of our institution.
Results
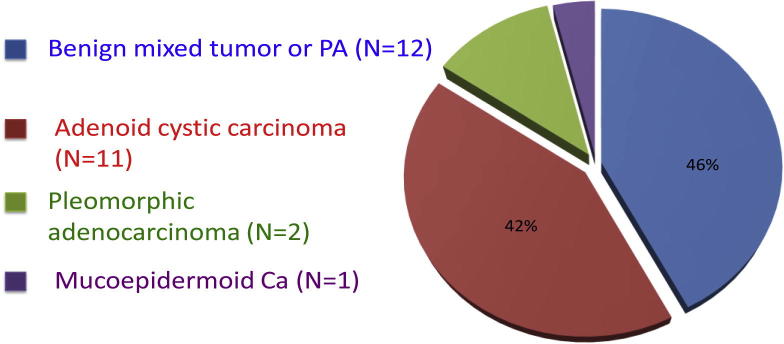
We have encountered a total of 28 excised lacrimal gland lesions at KKESH pathology department over a period of 26 years excluding structural (such as dacryops) and inflammatory conditions (such as Sjogren’s syndrome and non-specific dacryoadenitis). 3 lymphocytic lesions were identified through tissue diagnosis accounting for about 10% only for the lesions and these were not studied further. The rest were all true epithelial lacrimal gland tumors, which were the focus of our study. 26 epithelial tumors from 24 patients (since 2 patients had recurrent lesions over their period of follow-up at our institute) have been included. The benign category consisted all of BMT accounting for 12/26 of the lesions. The overall malignant lesions including ACC were more common accounting for more than half of the total lesions 14/26. The distribution of these cases is shown in Table 1 and Graph 1.
Table 1.
Frequency of epithelial lacrimal gland tumors.
| Histopathologic diagnosis | Number of cases | Percentage |
|---|---|---|
| BMT (pleomorphic adenoma) | 12 | 46 |
| Adenoid cystic carcinoma | 11 | 42 |
| Pleomorphic adenocarcinoma | 2 | 8 |
| Mucoepidermoid carcinoma | 1 | 4 |
| Total | 26 | 100% |
Graph 1.
Frequency of 26 epithelial lacrimal gland tumors.
The age ranged from 12 to 75 years with a mean of 44.27. The mean age did not differ much between the BMT and ACC groups. The lacrimal gland affected was on the right side in 14 cases and on the left side in 12. The male to female ratio was 15:11. The majority of the 24 patients were Saudis with a ratio of 16–8 non-Saudis.
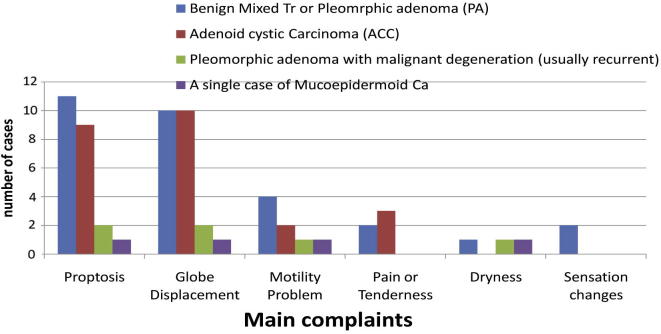
The duration of symptoms ranged from 1 to 180 months with an average of 38.19 months and median of 15 months. However when this was studied in benign and malignant groups separately, the median duration in the BMT group was 30 months, while it was shorter (7 months) in the ACC group. The median duration of symptoms in the Ca ex PA was 120 months. The commonest complaints were proptosis and globe displacement in 88% of the cases each. The distribution of the presenting symptoms according to the different types of tumor is demonstrated in Graph 2. Upon examination, the commonest finding was proptosis in 21/26 cases ranging from 1 to 10 mm on the affected side (median 4 mm) followed by a palpable visible mass in 19/26.
Graph 2.
The presenting symptoms in each type of epithelial lacrimal gland tumors.
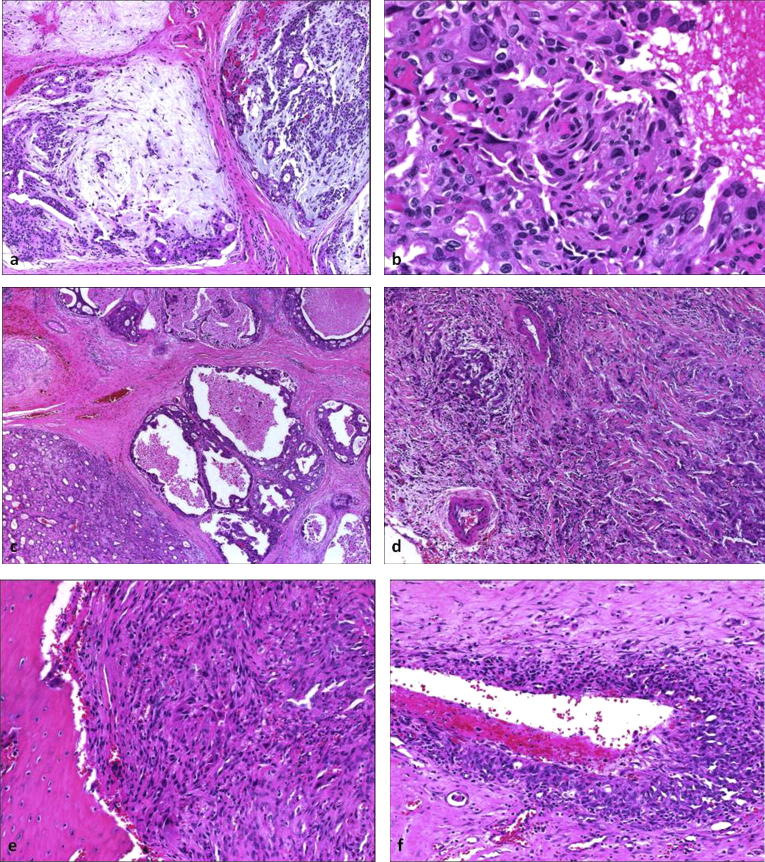
The gross pathologic examination showed intact pseudo-capsule in 10. 70% of benign lesions showed this feature. In contrast 89% (8/9) of the malignant tumors showed capsular infiltration. The only benign case with no intact capsule and an outer surface described, as “with bosselations” was a case of recurrent BMT. (Fig. 1a and b). The histopathologic findings of the BMT cases showed the presence of a pseudocapsule in all 12 cases (Fig. 1c), however the capsule was infiltrated by tumor extension in 5. The epithelial component was predominant (described as major or moderate component) in 5 cases only and consisted of tubular, cystic (ductal) or epithelial clusters in order of frequency (Fig. 1d). The stromal component was mostly myxomatous (6/12) followed by cartilagenous. (Fig. 1e and f). The least common type of stroma observed was osteoid and myoepithelial in 1 case each. The metaplasia of the epithelial component was mostly squamous and mainly observed in recurrent BMT.
Figure 1.
(a) Gross photo of a case of recurrent BMT with irregular outer surface, described as “with bosselations”; (b) The corresponding histopathologic appearance of the recurrent tumor with mixture of stromal and epithelial components. (Original magnification 100×. Hematoxylin and Eosin); (c) microscopic appearance of an intact capsule (red arrow) in a primary BMT. (Original magnification 100×. Hematoxylin and Eosin); (d) the epithelial component in another BMT forming several ducts (black arrows) within myxoid stroma. (Original magnification 100×. Hematoxylin and Eosin); (e) Microscopic appearance of the commonest classic myxoid stroma in BMT. (Original magnification 200×. Hematoxylin and Eosin); (f) chondroid-like stroma in a case of BMT. (Original magnification 200×. Hematoxylin and Eosin).
The 12 BMT cases were primary in 9 and recurrent in 3 patients. The period until recurrence is observed was: 3 years following the initial surgery in one case where the previous histopathologic examination showed capsular infiltration indicating incomplete excision at our institute, 9 years in one of the 2 remaining cases who had his initial primary surgery elsewhere but reported as incomplete excision as well and undetermined in the third case. Follow-up of 8/12 cases was available with a mean of 90 months and no evidence of further recurrence.
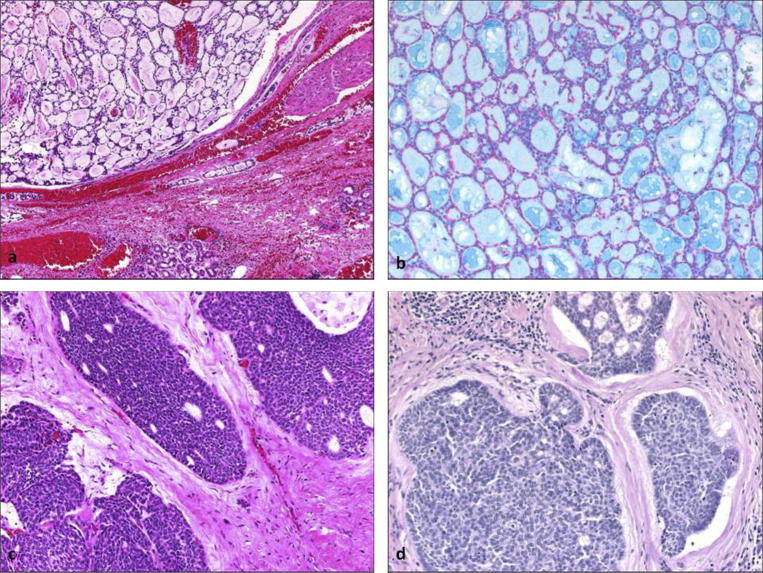
Of the 11 ACC cases, cribriform pattern was noted in 6, evident by characteristic Alcian Blue staining (Fig. 2a,b), solid pattern (often with palisading) in 4 lesions (Fig. 2c,d) and tubular in 1. The histologic grade was mostly G2 (7/11) and the rest were G3. In regard to tumor behavior, vascular invasion was documented in 5/11; orbital soft tissue and/or muscle invasion was also confirmed in 5/11. This was followed by perineural invasion in 1 case only. The TNM classification based on full systemic evaluation was mostly T2 in (6/11), T1 in (3/11). The last 2 cases were classified as T4 A and T4 B. Unfortunately more than half of our cases (6/11) were lost to follow-up. The mean follow up period of the remaining 5 cases was 82 months and they were well and alive. These cases were all classified as either T1 or T2.
Figure 2.
(a) A case of ACC with cribriform pattern. (Original magnification 100×. Hematoxylin and Eosin); (b) the same case with highlighted cribriform pattern stained with Alcian-Blue. (Original magnification 200×); (c) another ACC with solid pattern. (Original magnification 200×. Hematoxylin and Eosin); (d) a different ACC case of the solid type but showing evidence of palisading. (Original magnification 200×. Periodic acid Schiff).
We had 2 cases of MMT or pleomorphic adenocarcinoma. One of these cases was arising in a recurrent tumor (the so called carcinoma ex pleomorphic adenoma = Ca ex PA). This case had the malignant change in a second recurrence 14 years following the last excision at our institute (noted as incomplete excision). The histologic grade of the adenocarcinoma was high in this case. The other patient showed low grade malignant change (adenocarcinoma) arising in a primary tumor with no evidence of previous biopsy or excision. The malignant component was infiltrative in nature. Therefore was not considered carcinoma in situ. No follow-up was available for any of these 2 cases.
We had a single case of mucoepidermoid carcinoma of the lacrimal gland, which was arising “de novo” and was of low grade histopathologically.
Radiologic data were available for a total of 15 cases mainly in the form of computerized tomography (CT). The bone remodeling or excavation was described in 6 cases (4 benign and 2 malignant) while destruction was noted in 3 cases only – all malignant including the case of Ca ex PA. Other important features included encapsulation and evidence of invasion as presented in Graph 3. Calcification was an additional finding in 3 BMT cases. Invasion was further documented by radiologic examination in 3 cases of ACC.
Graph 3.
Variable radiologic findings among benign versus malignant lesions.
Discussion
Out of all the lacrimal gland lesions, epithelial tumors account for only 20–30% while inflammatory and lymphocytic lesions account for the remaining 70–80%.1, 2 Among the reported epithelial lesions, Shields et al. in 2004 concluded that approximately 55% are benign and 45% are malignant.2 Their conclusion was based on a comprehensive literature review on the subject. This prevalence however might not be applicable to various populations. Perez and his co-investigators reported the clinicopathologic features of 18 epithelial lacrimal gland tumors in a single institution in Brazil over a period of 36 years. 66.7% were ACC, 27.8% pleomorphic adenoma and 5.5% carcinoma ex pleomorphic adenoma.5 This indicates a different distribution of benign and malignant epithelial lesions with a higher rate of malignancy. On the other hand, studies in India demonstrated a distribution of benign and malignant tumors of the lacrimal gland similar to what was known in the old literature.3 The authors included all the surgically excised lacrimal gland lesions over a 10 year period. The distribution of benign and malignant lesions was 51% and 42%, respectively. Their benign lesions have included 1 lacrimal gland cyst. They had additional 3 cases of pseudotumor and 1 case of sarcoidosis listed as other tumors (7%). Their overall conclusion is that more than half of the lesions were benign epithelial in origin mostly being pleomorphic adenoma.6 Shields et al. also concluded that among benign lesions the most common were pleomorphic adenomas and dacryops, whereas among the malignant lesions ACC was the most common (66%), followed by carcinoma ex pleomorphic adenoma (18%), primary adenocarcinoma (9%) and mucoepidermoid carcinoma (3%).2
The distribution of our epithelial lacrimal gland tumors might indicate higher frequency of malignant lesions (14/26) similar to what has been found by Danyel.5 However, BMT was the commonest (46%) if ACC was compared to other tumors individually (42%). This was also reported in a larger series where BMT constituted 48% and ACC accounted for 32% out of all tumors.10 Also the commonest benign tumor was still BMT as shown in other series.1, 2, 3, 4, 5, 6, 7 Similarly ACC remained the commonest among the malignant lesions.6, 8 In regard to the histological classification of our 26 lesions, rare tumors (except for our single case of mucoepidermoid carcinoma) were not observed.10 It is worth mentioning that our technique in the pathological grading of all these epithelial tumors followed the recommendation by Rootman and White.11
Demographics in our series showed wide age range (12–75 years). The youngest patient had BMT. The mean age was similar in both benign and malignant tumor groups being 43.82 in the first and 43.35 in the second. On the other hand the mean age for the pleomorphic adenocarcinoma was older (47 years). Others have also observed a wide age range.6, 10 There was slight male predominance similar to what has been reported by Agarwal.6 Shields and their group have suggested that ACC is slightly more common in women but no overall general predilection for race or sex.2 This was also observed in our cases with F:M = 7:4 in the ACC group only.
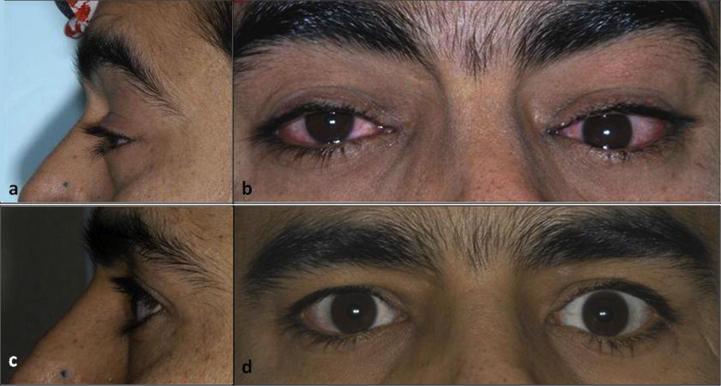
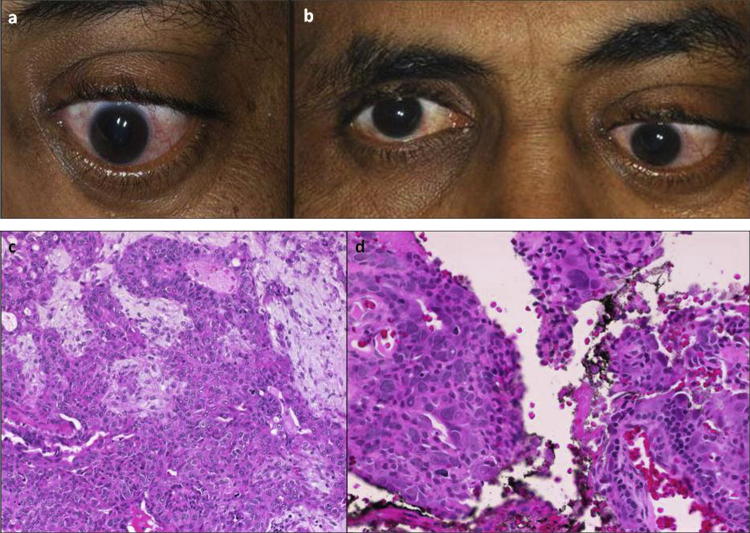
Clinically, Graph 2 reflects the distribution of symptoms among different categories according to diagnosis showed that pain or tenderness was more common in ACC compared to BMT possibly owing to their aggressive behavior.2, 5 The duration of symptoms had wide range however the median for BMT was 30 months and much shorter (less than a year) for ACC which was expected.4, 5 The median duration of symptoms for pleomorphic adenocarcinoma was 120 months. The eye on the affected side was found proptotic in almost all the cases (benign and malignant) by clinical examination (Fig. 3a and b). A palpable mass was another common finding however motility problems and diplopia in our series were not as common as expected even in the malignant category.2, 5
Figure 3.
(a and b) The preoperative clinical appearance of left eye proptosis in one of the cases in the benign group (BMT); (c and d) the postoperative clinical appearance of the same patient with completely resolved left eye proptosis.
BMT
Pleomorphic adenoma remains the most common benign epithelial tumor being extensively studied to allow reaching the correct diagnosis and minimizing the risk of local recurrence.5 The findings in our limited series clearly showed that incomplete excision (evidenced by capsular infiltration) was a major problem and a presumed cause for recurrence of BMT as seen in 3 recurrent cases of our BMT. This was noted especially in patients who had their primary surgery elsewhere. On the other hand, cases operated in our institute showed complete excision and resolved symptoms and signs. (Fig. 3c and d)
Our BMT had mostly predominance of the stromal component, which was myxomatous in most of the cases. Other stromal components described in literature such as cartilagenous or osteoid were also observed. Squamous metaplasia of the epithelial component was mainly observed in the recurrent cases.
The malignant degeneration that can occur with BMT is another unique and important feature mainly occurring in recurring tumors following inadequate excision. Therefore, careful surgical excision and good pathological examination of such specimens were mandatory to document capsular infiltration as in one of our cases.11 The findings in our limited series clearly showed that incomplete excision (probably by non experienced surgeons) in other institutions was a major problem for recurrence of PA as seen in 4 recurrent cases, 3 of which recurring as BMT. The range of time interval between primary tumor diagnosis and removal of the recurrent tumor was wide: 3 to 14 years with a median of 6.5 years.
Recurrent BMT/MMT
It has been known that the recurrence of BMT carries the risk of malignant degeneration5, 10, 12, 13 however out of the total 4 recurrent cases in our series, 1 only was found to be malignant occurring 14 years after the second recurrence. It is worth mentioning that the first recurrence of this tumor had shown focal areas of atypia (Fig. 4a,b) however not enough to warrant the diagnosis of an adenocarcinoma.10, 11 This malignant change (Fig. 4c and d) presented with a long history of 23 years (9 + 14) after the primary lesion since it was considered to be a second recurrence. Shield’s has reported such a transformation in a case even after longer period of 60 years.14 The other case of MMT was not recurrent (pleomorphic adenocarcinoma).
Figure 4.
(a) Histologic appearance of first recurrence of the BMT. (Original magnification 100×. Hematoxylin and Eosin); (b) the same BMT first recurrence showing focal atypia (Original magnification 400×. Hematoxylin and Eosin); (c) Ca ex PA malignant cystic areas of the second recurrence in the same patient. (Original magnification 40×. Hematoxylin and Eosin); (d) Ca ex PA showing capsular infiltration (Original magnification 100×. Hematoxylin and Eosin); (e) Ca ex PA showing bone invasion (Original magnification 100×. Hematoxylin and Eosin); (f) Ca x PA showing perivascular invasion (Original magnification 200×. Hematoxylin and Eosin).
In regard to the histological classification of these cases, Rootman and his co-authors stressed on differentiating circumscribed carcinoma within a pleomorphic adenoma “Carcinoma in situ” versus an invasive carcinoma originating from pleomorphic adenoma.7, 11 The sub classification of such cases included noninvasive, intracapsular or carcinoma “in situ”/minimally invasive and noninvasive depending on the extent of invasion from the capsule.1 Our recurrent case was classified as invasive, showing high histologic grade of adenocarcinoma and with evidence of perivascular and bone invasion (Fig. 4e and f).
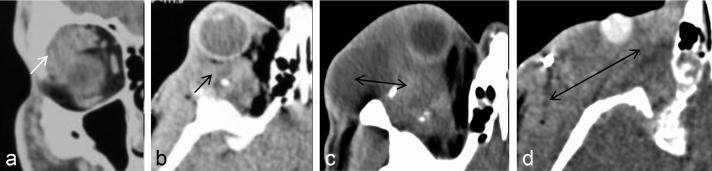
The radiologic features of repeated CT films over 1 year of follow up correlated with the clinical suspicious of malignant degeneration in this case. (Fig. 5a–d). The second case of pleomorphic adenocarcinoma was not recurrent, the patient presented with significant proptosis and globe displacement. Microscopic examination of the tumor showed low histologic grade of adenocarcinoma (Fig. 6a–d). Unfortunately no long follow up periods were available for any of these 2 cases.
Figure 5.
(a) Initial CT scan of the patient at the time of his first recurrence in 1989 which was 9 years following primary BMT excision elsewhere showed homogeneously enhancing mass lesion involving the right lacrimal gland with molded appearance and rounded border; (b) Follow-up sequential contrast enhancing Axial CT scans with second recurrence in 2002; (c and d) follow up CT in 2003, 14 years post an incomplete resection showing irregular soft tissue mass with heterogeneous enhancement combined with aggressiveness of the recurrent, malignant mixed tumor (double head arrow).
Figure 6.
(a and b) The clinical presentation in a case of primary pleomorphic adenocarcinoma with more profound left eye proptosis and globe displacement; (c) pleomorphic adenocarcinoma primary (microscopic appearance). (Original magnification 200×. Hematoxylin and Eosin); (d) the capsular infiltration in the same case (Original magnification 400×. Hematoxylin and Eosin).
ACC
Out of the malignant tumors, the commonest was ACC, which has a high frequency of recurrence.4, 6, 8 This tumor of the lacrimal gland shared with its salivary counterpart, some cardinal biologic features of indolence, persistance, metastasis and death.7 ACC might present an advanced tumor with bone invasion.5 Graph 2 representing the distribution of the symptoms among different categories according to diagnosis showed that pain or tenderness was more common in ACC compared to BMT possibly owing to their aggressive behavior.2, 7
In our cases, the cribriform pattern was the most common morphologically (6/11) followed by the solid or basaloid (often with palisading) in 4/11 which was different than what has been observed by others where the solid pattern was much less commonly encountered.7, 10
The chance of second recurrence in such a tumor was reported to be 46% with a mean interval of 9.7 months from excision.8 The limited follow up in our ACC cases (5 patients with mean period of 82 months) indicated favorable outcome, as they were all well and alive with no evidence of metastasis or recurrence. Our ACC cases however were all classified as either T1 or T2, which might have affected the prognosis in these patients.
Mucoepidermoid carcinoma
We have encountered a single case of this rare malignant epithelial tumor of the lacrimal gland. The grading of mucoepidermoid carcinomas is usually according to the degree of differentiation and relative number of mucin producing cells where lower grades have more mucin cells. The classification includes: grades 1–3 based on: cellularity, hyperchromatism and frequency of mitotic figures. The most important prognostic factor is the histologic grade. Our case was graded histopathologically as grade 2. (Fig. 7a–d). Our case did not seem to be arising from a preexisting PA in contrary to the cases studied by Rootman and White.7 The excision was complete in our case, with resolved postoperative symptoms (Figs. 7e–h) however, no long-term follow up was available for this patient.
Figure 7.
(a) Mucoepidermoid carcinoma appearance with low grade histopathologic features. (Original magnification 200×. Hematoxylin and Eosin); (b) the same tumor appearance with Periodic acid Schiff stain. (Original magnification 100×); (c) Mucicarmine positive tumor areas (Original magnification 100×); (d) mucin producing cell in the tumor (Original magnification 400×. Alcian Blue); (e and f) the preoperative appearance of the patient with mucoepidermoid carcinoma (right lacrimal gland); (g and h) the postoperative appearance of the same patient with resolved proptosis after complete removal of the tumor.
Radiology
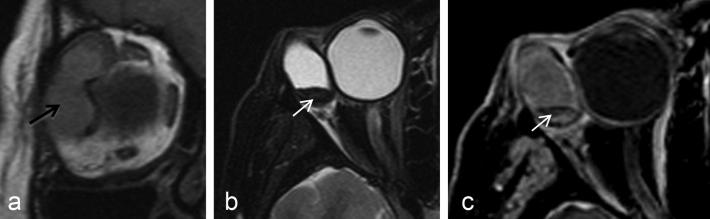
CT and MRI are utilized to differentiate between different types of lacrimal gland masses and to determine the extent of lesions involving the lacrimal fossa. Although many diseases that affect the lacrimal gland are specifically diagnosed by imaging, it is sometimes very difficult to differentiate each specific disease on the basis of image characteristics alone, however radiologic studies can still aid physicians in their differential diagnoses.9 Recently, addition of Diffusion weighted MRI sequence (DWI) and Apparent diffusion coefficient (ADC) measurement coupled with MRI technique had enabled effective characterization of pathological features of lacrimal gland lesions that might help in the early detection of malignant lesions.15 Owing to the relatively long history, benign lesions in our series showed bone remodeling or excavation in addition to a well-delineated mass.1, 6, 9 (Fig. 8) In contrast, ACC showed bone invasion and destruction.5
Figure 8.
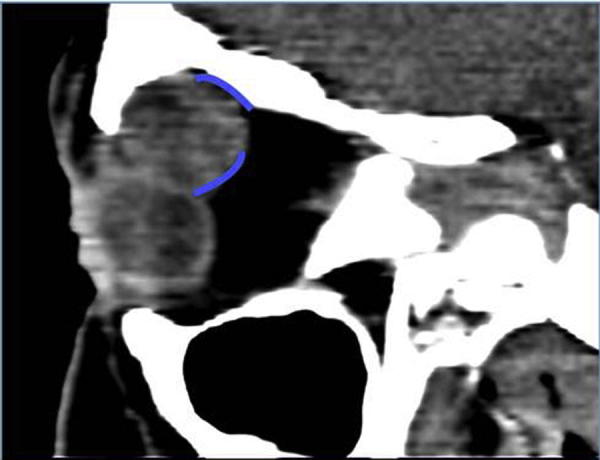
CT scan of a case of BMT showing well-defined mass in the area of the lacrimal gland (blue curved lines).
The mucoepidermoid carcinoma case was studied by Magnetic Resonance Imaging (MRI) and showed non-homogenous mass, cystic in nature with poor contrast enhancement with hemorrhagic changes (Fig. 9a–c) This case had an intact capsule by histopathologic examination with lymphoid follicles within the capsule and no evidence of invasion histologically and radiologically.
Figure 9.
MRI photos in the case with mucoepidermoid carcinoma: (A–C) coronal T1 WI, Axial T2 with fat suppression and post contrast axial T1 with fat suppression showed poorly enhancing bi-lobulated right lacrimal gland mass (black arrow) with hemorrhage (white arrow).
Our radiologic findings aided in the clinical diagnosis and had correlated well with the histopathologic characteristics in general in our series.
Conclusion
We have observed that we tend to have higher number of malignant epithelial lacrimal gland tumors with a ratio of 14:12. The commonest benign tumor was BMT or PA, while the commonest malignant tumor was ACC. We had an overall male predominance, however ACC in our series showed female predominance. The mean age and the clinical symptoms were similar in both benign and malignant groups. Recurrence of PA was a major problem which seemed to be related to incomplete surgical excision. Risk of malignant change in our recurrent cases was relatively low. None of our ACC cases with available follow up showed evidence of metastatic disease or recurrence. Radiology could aid in the diagnosis of cases and in differentiating between benign and malignant lesions.
These observations would encourage further detailed studies on the management and prognosis of these tumors. The information would also be considered as baseline diagnostic information for future studies on cytogenetic characteristics of epithelial lacrimal gland tumors in our population.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Bernardini F.P., Devoto M.H., Croxatto J.O. Epithelial tumors of the lacrimal gland: an update. Curr Opin Ophthalmol. 2008;19:409–413. doi: 10.1097/ICU.0b013e32830b13e1. [DOI] [PubMed] [Google Scholar]
- 2.Shields J.A., Shields C.L., Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 mongometry lecture, part 1. Ophthalmology. 2004;111:997–1008. doi: 10.1016/j.ophtha.2003.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Zimmerman L.E., Sanders T.E., Ackerman L.V. Epithelial tumors of the lacrimal gland: prognostic and therapeutic significance of histologic types. Int Ophthalmol Clin. 1962;2(2):337–367. [Google Scholar]
- 4.Sanders T.E., Ackerman L.V., Zimmerman L.E. Epithelial tumors of the lacrimal gland. A comparison of the pathologic and clinical behavior with those of the salivary gland. Am J Surg. 1962;104:657–665. doi: 10.1016/0002-9610(62)90414-2. [DOI] [PubMed] [Google Scholar]
- 5.Perez D.E.C., Pires F.R., Almeida O.P., Kowalski L.P. Epithelial lacrimal gland tumors: clinicopathological study of 18 cases. Otolaryngol Head Neck Surg. 2006;134:321–325. doi: 10.1016/j.otohns.2005.09.024. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal K.R., Verma M., Menon S., Kumar K., Biswas J., Subramaniam N. Profile of lacrimal gland lesions at a tertiary care centre. All India Ophthalmol Soc Proc. 2006:389–391. [Google Scholar]
- 7.Rootman J., White V.A., Alkatan H. 2nd ed. Lippincott Williams and Wilkins; Philadelphia: 2003. Tumors of the lacrimal gland; pp. 343–361. (Diseases of the orbit-a multidisciplinary approach). [Google Scholar]
- 8.Ramon L.F., Shannon L.S., Richard G.B. Malignant epithelial tumors of the lacrimal gland: a clinicopathologic study of 21 cases. Arch Ophthalmol. 1998;116:613–616. doi: 10.1001/archopht.116.5.613. [DOI] [PubMed] [Google Scholar]
- 9.Jung W.S., Ahn K.J., Park M.R. The radiological spectrum of orbital pathologies that involve the lacrimal gland and the lacrimal gland fossa. Korean J Radiol. 2007;8:336–342. doi: 10.3348/kjr.2007.8.4.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weis E., Rootman J., Joly J.T., Alkatan H.M. Epithelial lacrimal gland tumors. Pathologic classification and current understanding. Arch Ophthalmol. 2009;127(8):1016–1028. doi: 10.1001/archophthalmol.2009.209. [DOI] [PubMed] [Google Scholar]
- 11.Rootman J., White V.A. Changes in the 7th edition of the AJCC TNM classification and recommendations for pathologic analysis of lacrimal gland tumors. Arch Ophthalmol Lab Med. 2009;133:1268–1271. doi: 10.5858/133.8.1268. [DOI] [PubMed] [Google Scholar]
- 12.Riley F.C., Henderson J.W. Report of a case of malignant transformation in benign mixed tumor of the lacrimal gland. Am J Ophthalmol. 1970;70:767–770. doi: 10.1016/0002-9394(70)90499-x. [DOI] [PubMed] [Google Scholar]
- 13.Henderson J.W., Farrow G.M. Primary malignant mixed tumors of the lacrimal gland. Ophthalmology. 1980;87:466–475. doi: 10.1016/s0161-6420(80)35206-8. [DOI] [PubMed] [Google Scholar]
- 14.Shields J.A., Shields C.L. Malignant transformation of presumed pleomorphic adenoma of lacrimal gland after 60 years. Arch Ophthalmol. 1987;105:2403–2405. doi: 10.1001/archopht.1987.01060100105037. [DOI] [PubMed] [Google Scholar]
- 15.El-khamary S.M. Lacrimal gland lesions: can addition of diffusion-weighted MR imaging improve diagnostic accuracy in characterization? Egypt J Radiol Nucl Med. 2012;43(2):165–172. [Google Scholar]