Abstract
Aim
To report the outcomes of endoscopic guided anterograde 3 mm balloon dacryoplasty with silicone intubation in patients with acquired partial nasolacrimal duct obstructions in adults.
Methods
Retrospective case series, included 21 eyes with partially obstructed nasolacrimal ducts of 12 patients. All the 21 ducts were initially probed and the probe confirmed with an endoscope in the inferior meatus. After confirming the presence of probe in the inferior meatus, a 3 mm balloon was used for dilating the distal and proximal portions of nasolacrimal duct, followed by stenting of ducts with Crawford tubes. Main outcome measures were anatomical patency of the passage and resolution of epiphora.
Results
Of the 12 patients, 9 had bilateral and 3 had unilateral acquired partial nasolacrimal duct obstructions. All the patients underwent bicanalicular stenting under endoscopic guidance which were retained for a period of 12 weeks. A minimum follow up of 6 months following stent removal was considered for final analysis. 15 of the 21 ducts (71%) were freely patent on irrigation but 13 of the 21 reported improvement of epiphora. Two nasolacrimal ducts showed similar partial regurgitation and partial patency on syringing as before with no improvement of symptoms. Four nasolacrimal ducts were completely obstructed with complete regurgitation of fluid on syringing with worsening of the epiphora. Two eyes persisted with symptoms of epiphora despite patent nasolacrimal duct with grade 2 dye retention on dye disappearance test.
Conclusions
3 mm balloon dacryoplasty is an alternative and safe way to manage partial nasolacrimal duct obstructions with an anatomical success in 71% and functional success in 62% of the patients. Further studies with a large sample size and longer follow-up are required to ascertain the long term benefits.
Keywords: Balloon dacyroplasty, Nasolacrimal duct obstruction, Partial, Epiphora, Adults
Introduction
Balloon dacryoplasty is a term used for a set of minimally invasive lacrimal procedures that utilizes specially designed balloons, targeted at different points in the lacrimal system for a wide range of indications. Balloons were first used by Becker and Berry in 1989.1 Around the same time Munk et al. reported balloon catheter dilatation for adults with epiphora using an angioplasty catheter under fluoroscopic guidance.2 There are ongoing efforts worldwide to look for an alternative to dacryocystorhinostomy (DCR) in the management of nasolacrimal duct obstructions (NLDO). Probing alone or silicone intubation alone was not found to have encouraging results in studies that did not differentiate between complete and partial NLDO.3, 4 However bicanalicular silicone intubation specifically for partial NLDO was found to have a success rate of 54%.5 Balloon dacyroplasty is also rapidly gaining ground as a minimally invasive alternative for the treatment of partial nasolacrimal duct obstructions.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 The purpose of the present study is to describe the efficacy and complications of 3 mm balloon catheters in managing acquired partial or incomplete NDLO in adults.
Methods
Retrospective case series included 21 eyes with partially obstructed nasolacrimal ducts of 12 patients. Partial obstruction of nasolacrimal ducts was diagnosed by two ways, one a gentle and slow intra-sac syringing, wherein there was a partial regurgitation of the fluid as well as drainage of fluid into the nose. Second, a dacryoendoscopy was performed to ascertain the partial obstruction in the nasolacrimal duct. Patients with canalicular stenosis or partial canalicular obstructions and post-traumatic obstructions were excluded. None of the patients underwent any interventions for epiphora in the past. Balloon dilatation was performed as per the standard way published in the literature.6 The nasolacrimal ducts were initially probed and the probe confirmed in the inferior meatus with an endoscope. Subsequently the entire procedure was carried out under nasal endoscopic guidance. After the assembly of the balloon catheter with the inflation device (Atrion Corporation, Allen, Texas, USA), the 3 mm lubricated balloon (Fig 1) was then passed through the superior punctum into the distal portions of the nasolacrimal ducts. This is ascertained by the markings on the catheter (Fig 1) or by visualizing around half of the length of catheter in the inferior meatus (Fig 2). The balloon is stabilized in this position and with the help of manometer device (Fig 3), inflated to 8 atmospheres for 90 s, deflated and reinflated to 8 atmospheres for 60 s (Fig 4). The balloon is then withdrawn into the proximal portion of the nasolacrimal duct (Fig 5). The position is ascertained by the markings on the catheter or by visualizing just the tip of the catheter in the inferior meatus (Fig 5). The same cycle of inflation, deflation and reinflation is repeated again for the proximal portion of the nasolacrimal duct. The catheter was then withdrawn and irrigation of the lacrimal system was performed to assess the patency. This was followed by stenting of nasolacrimal duct with Crawford bicanalicular intubation under nasal endoscopic guidance (Fig 6). A well dilated nasolacrimal duct opening is noticed at the end of the procedure (Fig 6). Post-operatively the patients received topical antibiotic–steroid eye drops in a tapering dose for 2 weeks. Data collected include demographic data, clinical presentation, laterality, status of lids and puncta, irrigation findings, probing interpretations, and duration of intubation. Anatomical success was defined as patency of the lacrimal passage on irrigation and functional success was defined as resolution of epiphora.
Figure 1.

Distal end of a 3 mm balloon catheter with the balloon and its markings.
Figure 2.
Endoscopic view of the inferior meatus showing the balloon catheter exiting from the nasolacrimal duct. Note the length of the catheter seen.
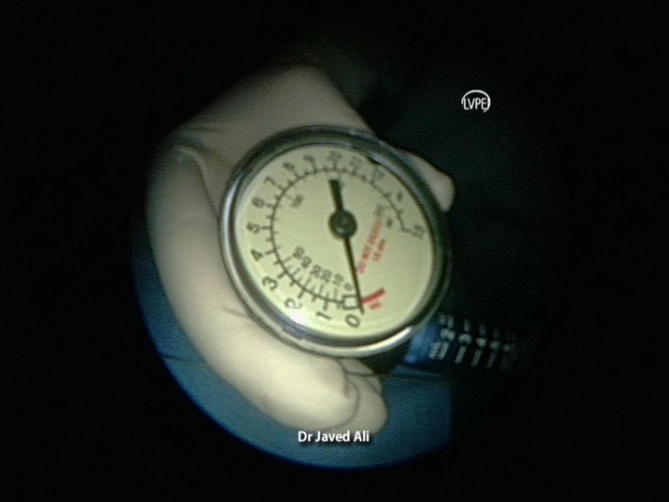
Figure 3.
Manometer mounted on the inflation device to show the pressure in atmospheres.
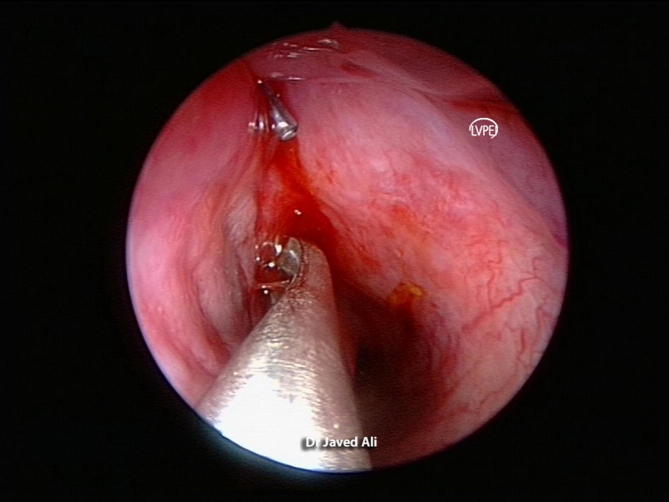
Figure 4.
Endoscopic view of the inferior meatus showing the balloon dilatation of the distal nasolacrimal duct. Note the inflated balloon and compare it with deflated stage in Fig. 2.
Figure 5.
Endoscopic view of the inferior meatus showing balloon dilatation of the proximal nasolacrimal duct. Note that only the tip of the catheter is visible at NLD. Compare this with the length of catheter seen in Figure 2, Figure 3.
Figure 6.
Endoscopic view of the dilated nasolacrimal duct opening. Note the silicone tube exiting the duct opening in inferior meatus.
Results
There were 4 male and 8 female patients. Mean age was 58.2 years (range 42–71 years). Of the 12 patients 9 had bilateral and 3 had unilateral partial nasolacrimal duct obstructions. All the patients underwent bicanalicular stenting under endoscopic guidance. All stents were retained for a period of 12 weeks. No significant complications were noticed. All patients reported occasional blood tinged nasal secretions in the first week following the procedure. Two patients reported infrequent irritation and discomfort due to stent. A minimum follow up of 6 months following stent removal was considered for final analysis. At the final follow up, 15 of the 21 ducts (71%) were freely patent on syringing and reported improvement of epiphora. Two nasolacrimal ducts (9.5%) showed similar partial regurgitation and partial patency on syringing as before with no improvement of symptoms. Four nasolacrimal ducts (19%) were completely obstructed with complete regurgitation of fluid on syringing and worsening of the epiphora. Two eyes persisted with symptoms of epiphora despite patent nasolacrimal duct with grade 2 dye retention on dye disappearance test. The anatomical success was 71% and the functional success rate was 62%.
Discussion
Dacryocystorhinostomy (DCR) has been the common modality of treatment of symptomatic partial NLDO in adults. External as well as endoscopic approaches for DCR has high success rates, but obviously are more invasive with blood loss, risks of general anesthesia if used and scarring in external DCR. The quest on this front has been to look into the feasibility of using minimally invasive alternatives. With the advent of balloons, several studies have looked at the efficacy of using 3-mm balloon catheters in such cases.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 The 3 mm balloon has an outer diameter of 3 mm and length of 15 mm, and targets at dilating the distal and proximal portions of nasolacrimal duct. The balloon dilatation likely interferes with the inflammation–stenosis–obstruction–stasis–infection cycle by restoring the anatomical patency.
A number of studies in the past have used the retrograde approach of balloon dilatation that requires additional radiographic control and multidisciplinary approach.2, 7, 8, 9, 10 In spite of these guidance tools, there can sometimes be a procedural failure because of the inability to catheterize the nasolacrimal duct. The success rates using retrograde approaches have been reported to vary between 25% to as high as 90%.2, 7, 8, 9, 10 The authors of the current study, like many other proponents of anterograde approach believe it to be much simpler with a short learning curve, can be performed by an ophthalmologist alone without encountering technical failures like inability to catheterize and is less expensive. At the same time we also stress on the use of nasal endoscopic guidance during the procedure since it ascertains an accurate dilatation of nasolacrimal ducts and also allows visualization of nasal cavity and inferior meatus for any pathology that may occlude the outlet.
Perry et al.11 used dacryocystography to assess the post-saccal stenosis and treated 15 partially obstructed nasolacrimal ducts in adults with balloon dilatation and intubation and at 6 months follow up reported anatomical success rates of 73%. They subjectively assess the epiphora using the Munk scale2 and reported the resolution of epiphora in 60% of patients.
Kuchar et al.12 used transcanalicular endoscopes to aid in the diagnosis of nasolacrimal duct obstructions and reported an overall subjective success of 73% at one year after balloon dilatation. The duration of epiphora in their study did not appear to influence the outcomes and most recurrences presented in the first six months following the procedure. It is interesting to note that all patients selected in this study were having complete nasolacrimal duct obstruction and 4 patients underwent laser canaliculoplasty for canalicular membranous obstructions. In contrast our study focused only on partial obstructions and excluded complete obstructions, post-traumatic obstructions as well as canalicular stenosis and obstructions. The authors of the current study concur with Luchtenberg et al.13 that these excluded cases do not do well with balloon dilatation.
In the largest study so far, Couch et al.14 studied 142 partially obstructed nasolacrimal ducts at a mean follow up of 7.5 months, reported an overall improvement in epiphora in 90% of their patients with the complete resolution of epiphora in 56%. Based on the substantial improvement of epiphora in their large series, they recommended it as a procedure of choice in patients with incomplete NLDO in the absence of secondary causes of epiphora.
The long term effects of balloon dacryoplasty were studied by Konuk et al.15 in 99 eyes of 94 patients with a mean follow up of 100 ± 38.4 months. The study subjects were a mixture of common canalicular stenosis, proximal and distal nasolacrimal duct obstructions. The overall long term success rates were not encouraging except for partial distal NLDO (73.3%), which made the authors recommend balloon dilatation as an alternative for this subset only.
The use of silicone intubation along with a balloon dacryoplasty is not clear. Kashkouli et al5 retrospectively compared balloon dilatation with intubation vs. intubation alone and reported no statistical difference between groups (61% vs. 54%) in the outcomes at a mean follow up of 14.60 months. However, it is important to note that this was not a randomized study. Bleyen et al.16 conducted a similar study but was a randomized control trial. They also did not find a significant difference between groups (52% vs. 57%).
Complications of balloon dacryoplasty reported in the literature include intra-operative pain, headaches, nasal bleed, blurred vision and iatrogenic false passages.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 The only major complication reported was a single case of orbital emphysema that was initiated with a forceful sneezing in a patient, but was managed successfully by a conservative approach.17 This brief list of complications does not make balloon dacryoplasty an unsafe procedure but helps the surgeon to counsel the patient in a better manner.
In conclusion, balloon dacryoplasty represents a minimally invasive technique which can be performed with satisfying results in adults with acquired partial nasolacrimal duct obstructions. The procedure appears to be safe, however, studies with larger sample size and longer follow up are required to conclusively prove or disprove its role in avoiding a dacryocystorhinostomy.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Becker B.B., Berry F.D. Balloon catheter dilatation in lacrimal surgery. Ophthalmic Surg. 1989;20:193–198. [PubMed] [Google Scholar]
- 2.Munk P.L., Lin D.T., Morris D.C. Epiphora: treatment by means of dacryoplasty with balloon dilatation of the nasolacrimal drainage apparatus. Radiology. 1990;177:687–690. doi: 10.1148/radiology.177.3.2243969. [DOI] [PubMed] [Google Scholar]
- 3.Bell T.A. An investigation into the efficacy of probing the nasolacrimal duct as a treatment for epiphora in adults. Trans Ophthalmol Soc UK. 1986;105:494–497. [PubMed] [Google Scholar]
- 4.Connell P.P., Fulcher T.P., Chacko E. Long term follow up of nasolacrimal duct intubation in adults. Br J Ophthalmol. 2006;90:435–436. doi: 10.1136/bjo.2005.084590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kashkouli M.B., Beigi B., Tarassoly K. Endoscopically assisted balloon dacryoplasty and silicone intubation versus silicone intubation alone in adults. Eur J Ophthalmol. 2006;16:514–519. doi: 10.1177/112067210601600402. [DOI] [PubMed] [Google Scholar]
- 6.Ali M.J., Naik M.N., Honavar S.G. Balloon dacryoplasty: ushering the new and routine era in minimally invasive lacrimal surgeries. Int Ophthalmol. 2013;33:203–210. doi: 10.1007/s10792-012-9652-z. [DOI] [PubMed] [Google Scholar]
- 7.Janssen A.G., Mansour K., Krabbe G.J. Dacyrocystoplasty: treatment of epiphora by means of balloon dilatation of the obstructed nasolacrimal duct system. Radiology. 1994;193:453–456. doi: 10.1148/radiology.193.2.7972762. [DOI] [PubMed] [Google Scholar]
- 8.Robinson R., Turner N., Brettle P. The treatment of epiphora with balloon dacryoplasty. Eye. 1993;7:687–690. doi: 10.1038/eye.1993.156. [DOI] [PubMed] [Google Scholar]
- 9.Song H.Y., Ahn H.S., Park C.K. Complete obstruction of the nasolacrimal system. Radiology. 1993;186:367–371. doi: 10.1148/radiology.186.2.8421736. [DOI] [PubMed] [Google Scholar]
- 10.Kumar E.N. Technical note: non-surgical treatment of epiphora by balloon dacyroplasty – the technique. Br J Radiol. 1995;68:1116–1118. doi: 10.1259/0007-1285-68-814-1116. [DOI] [PubMed] [Google Scholar]
- 11.Perry J.D., Maus M., Nowinski T.S., Penne R.B. Balloon catheter dilatation for treatment of adults with partial nasolacrimal duct obstruction: a preliminary report. Am J Ophthalmol. 1998;126:811–816. doi: 10.1016/s0002-9394(98)00278-5. [DOI] [PubMed] [Google Scholar]
- 12.Kuchar A., Steinkogler F.J. Antegrade balloon dilatation of nasolacrimal duct obstruction in adults. Br J Ophthalmol. 2001;85:200–204. doi: 10.1136/bjo.85.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luchtenberg M., Bartel J.H., Bink A. Clinical effectiveness of balloon dacyroplasty in circumscribed obstructions of the nasolacrimal duct. Ophthalmologica. 2007;221:434–438. doi: 10.1159/000107507. [DOI] [PubMed] [Google Scholar]
- 14.Couch S.M., White W.L. Endoscopically assisted balloon dacryoplasty treatment of incomplete nasolacrimal duct obstruction. Ophthalmology. 2004;111(3):585–589. doi: 10.1016/j.ophtha.2003.06.013. [DOI] [PubMed] [Google Scholar]
- 15.Konuk O., Ilgit E., Erdinc A. Long term results of balloon dacyroplasty: success rates according to the site and severity of the obstruction. Eye. 2008;22:1483–1487. doi: 10.1038/sj.eye.6702912. [DOI] [PubMed] [Google Scholar]
- 16.Bleyen I., Willem A., Bosch V.D. Silicone intubation with or without balloon dacryoplasty in acquired partial nasolacrimal duct obstruction. Am J Ophthalmol. 2007;144:776–780. doi: 10.1016/j.ajo.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 17.Ajit R., Inkster C., Tuck J. Orbital emphysema: an unusual complication of balloon dacryoplasty. Br J Radiol. 2004;77:1057–1058. doi: 10.1259/bjr/86898521. [DOI] [PubMed] [Google Scholar]