Abstract
Objectives
We compare findings from 10 years of experience evaluating physicians referred for fitness-to-practice assessment to determine whether those referred for disruptive behavior are more or less likely to be declared fit for duty than those referred for mental health, substance abuse or sexual misconduct.
Method
Deidentified data from 381 physicians evaluated by the Vanderbilt Comprehensive Assessment Program (2001–2012) were analyzed and compared to general physician population data and also to previous reports of physician psychiatric diagnosis found by MEDLINE search.
Results
Compared to the physicians referred for disruptive behavior (37.5% of evaluations), each of the other groups was statistically significantly less likely to be assessed as fit for practice [substance use, %: odds ratio (OR)=0.22, 95% confidence interval (CI)=0.10–0.47, P<.001; mental health, %: OR=0.14, 95% CI=0.06–0.31, P<.001; sexual boundaries, %: OR=0.27, 95% CI=0.13–0.58, P=.001].
Conclusions
The number of referrals to evaluate physicians presenting with behavior alleged to be disruptive to clinical care increased following the 2008 Joint Commission guidelines that extended responsibility for professional conduct outside the profession itself to the institutions wherein physicians work. Better strategies to identify and manage disruptive physician behavior may allow those physicians to return to practice safely in the workplace.
Keywords: Professionalism, Medical ethics, Fitness for duty, Fitness to practice, Disruptive behavior, Physician health and wellness, Comprehensive psychiatric assessment, Psychiatric diagnosis
1. Introduction
“Professionalism is based on the principles of primacy of patient welfare, patient autonomy, and social justice. It involves the following professional responsibilities: competence, honesty, patient confidentiality, appropriate relations with patients, improving quality of care, improving access to care, just distribution of finite resources, commitment to scientific knowledge, maintaining trust by managing conflicts of interest, commitment to professional responsibilities.”
American Board of Internal Medicine Foundation, American College of Physicians, European Foundation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med 2002;136:243–246
Ethical guidance [1] for physician conduct [2] has evolved over millennia and reflects cultural mores. To our knowledge, this report is the first to describe findings and remedial recommendations for physician subjects referred for fitness-for-duty (FFD) evaluation following the 2005 American Psychiatric Association guidelines [3]. Interested readers are referred to other sources [4–9] describing the standards and practices for evaluation of physicians, but little data on the comprehensive FFD evaluation of physicians have been published. In this article, we describe the results of preliminary analysis of data accumulated conducting physician FFD evaluations using a standardized comprehensive assessment methodology at our center over 10 years. Comparison of these findings with the general physician population [10] might help to elucidate certain environmental, cultural, legal and economic characteristics that result in such FFD referrals and may serve to influence policymakers who strive to enhance the quality of healthcare in this country and beyond.
2. Design and methods
The Vanderbilt Comprehensive Assessment Program (V-CAP) has conducted FFD evaluations since 2001 for licensed clinicians who practice outside Vanderbilt's Health Affiliated Network. V-CAP is a multidisciplinary team of specialists in psychiatry, addiction, internal medicine, psychology, neuropsychology, sex therapy, social work and nursing. Psychiatric examination includes focused assessment of substance use along with other psychiatric disorders plus appropriately targeted psychological testing (Table 1).
Table 1.
Elements of the V-CAP FFD evaluation
| Detailed collateral information |
Assessment procedures |
Optional consults |
|---|---|---|
| Preevaluation | Psychiatry | Neuropsychological evaluationb |
| Referral reason | Internal medicine | |
| Pertinent records | Laboratory | Subspecialty |
| Hearing & vision | (e.g., neurology) | |
| With authorized releases | EKG, stress test | |
| Practice performance | Spirometry | Polygraph Examination |
| Workplace environment | ||
| Family & social life | Psychological testing | |
| MMPI-2, PAI, EQi | ||
| MoCA or MMSE | ||
| (Other specific tests)a | ||
| Self-report screening tools |
EKG, electrocardiogram; MMPI-2, Minnesota Multiphasic Personality Inventory [11]; PAI, Personality Assessment Inventory [12]; EQi, Emotional Quotient Inventory [13]; MoCA, Montreal Cognitive Assessment [14]; MMSE, Mini Mental Status Examination [15].
Additional specific testing of memory and cognitive function, e.g., Wechsler Adult Intelligence Scale [16].
Halstead–Reitan Neuropsychological Battery and other standardized tests of neuropsychology [17].
The reasons for referral, the questions being posed and the degree of confidentiality are all clarified before the evaluation is scheduled. Typically, 2 full days, at minimum, are required for the assessment team to elicit necessary information from the subject.
After obtaining consent, extensive collateral information is gathered systematically from relevant third-party informants that may include spouse, therapist, physicians, treatment program, colleagues, administrative staff and others in the doctor's work (clinical) environment.
A comprehensive report is generated describing the multiaxial diagnosis, based upon the Diagnostic and Statistical Manual of the American Psychiatric Association [18], in language that is clear and sufficiently free of mental health jargon to ensure comprehension by an average physician. FFD status is designated as (a) fit or (b) unfit for practice, and remedial recommendations are included when appropriate. Deidentified data are digitally recorded, with approval of the Vanderbilt University Medical Center Institutional Review Board, utilizing Research Electronic Data Capture.
2.1. Statistical analysis
Descriptive statistics were used to summarize the demographic, diagnosis and referral variables. Years of age were described using means and standard deviations. We attempted to assess for consistency of our findings by seeking possible differences in the characteristics of the physicians (arbitrarily 50% of total) referred for FFD evaluations during the early years (2001–2007) in comparison with more recent years (2008–2012). χ2 tests of independence were used for all of the nominal and ordinal data, and independent t test was used for years of age at referral. Associations of the reasons for referral with the presence of an Axis I and Axis II diagnosis made during the evaluation and the FFD recommendation were conducted using multiple logistic regression analysis. A P value of .05 was used for reaching a conclusion of statistical significance for all tests conducted.
3. Results
3.1. Characteristics of V-CAP FFD + referrals
Three hundred eighty-one physicians (M.D. or D.O.) had been referred for evaluation at V-CAP between 2001 and March 2012. The demographic characteristics (age, sex, marital status, location by state or province, and practice specialty) of the physician subjects are displayed in Table 2.
Table 2.
Demographic characteristics and primary specialties of physicians referred to V-CAP
| 2009 population estimatea | Total (N=381) | |
|---|---|---|
| Mean (S.D.) | ||
| Age (years) | 48.9 (9.5) | |
| % | N (%) | |
| Age interval | ||
| <35 years | 15.0 | 22 (5.8) |
| 35–44 years | 22.0 | 103 (27.0) |
| 45–54 years | 22.7 | 147 (38.6) |
| 55–64 years | 19.6 | 92 (24.1) |
| ≥65 years | 20.7 | 17 (4.5) |
| Male | 70.4 | 341 (89.5) |
| White | 71.0 | 318 (83.5) |
| Married | 259 (68.0) | |
| Trained in the USA | 74.1 | 307 (83.4) |
| Anesthesiology | 4.7 | 23 (6.0) |
| Emergency medicine | 3.7 | 10 (2.6) |
| Family medicine | 10.9 | 62 (16.3) |
| Internal medicine | 41.4 | 105 (27.6) |
| Pediatrics | 8.7 | 15 (3.9) |
| Psychiatry | 5.3 | 19 (5.0) |
| Obstetrics gynecology | 4.7 | 35 (9.2) |
| Radiology oncology | 6.9 | 23 (6.0) |
| Surgery | 13.7 | 78 (20.5) |
| Resident trainee | 9 (2.4) | |
| Other | 2 (0.5) |
Information published by the AMA.
When compared to general physician demographic characteristics published for 2009 by the American Medical Association (AMA) [10], the V-CAP referrals were more likely to be middle-aged (63% were 45–64 years old vs. 42% 2009 AMA, P<.001), to be male (90% vs. 70%, P<.001), to be white (84% vs. 71%, P<.001) and to have been trained in the United States (83% vs. 74%, P=.002).
In comparison with published distributions of specialties in the 2009 AMA tables, family medicine (16% vs. AMA 11%) and surgery (21% vs. AMA 14%) tended to be overrepresented in the V-CAP referrals, while internal medicine (28%) tended to be underrepresentative of the general US physician population in 2009 (41%) (P<.001) (Table 2).
3.2. Referral sources
Overall, the most common source of referral was the state Physician Health Programs (approximately 40%, Table 3). No statistically significant differences were observed among the physician specialties in terms of referral source (data not shown, P=0.949).
Table 3.
Sources and characteristics of physicians referred to V-CAP
| Total (N=381) | |
|---|---|
| N (%) | |
| Self-referral | 29 (7.6) |
| Hospital referred | 72 (18.9) |
| Practice referred | 31 (8.1) |
| State physician health | 153 (40.2) |
| State medical board | 36 (9.4) |
| Personal attorney | 35 (9.2) |
| Therapist referred | 4 (1.0) |
| Other | 21 (5.5) |
| Disruptive behavior | 143 (37.5) |
| Sexual boundary issues | 86 (22.6) |
| Substance use issues | 77 (20.2) |
| Mental health issues | 57 (4.7) |
| Other | 18 (4.7) |
| Medical board involvement | 108 (28.5) |
| History of licensure sanctions | 103 (27.9) |
| Suspension of privileges | 175 (51.0) |
| Monitoring agreement | 144 (38.8) |
3.3. Reasons for referral and professional sanctions
As shown in Table 3, complaints alleging disruption of clinical outcome, commonly including threats, intimidation or demeaning behavior towards other staff by physicians, were the single most commonly cited primary reason for referral (n= 143 of 381, 37.5%). Rates of referral for disruptive behavior were higher among the surgical specialties (47 of 78, 60% vs. 21%–36%) than among the others (Table 4). Family medicine had the highest rates of referral for sexual boundary issues (39% vs. 8% surgery, 23%–24% internal medicine and others), and family practitioners were more likely than other specialties to have current board involvement (52% vs. 14%–34%, P<.001) or license sanctioning (31% vs. 5%–20%, P<.001) when evaluation occurred.
Table 4.
Referral characteristics by specialty group
| Family medicine (n=62) | Internal medicine (n=105) | Surgery (n=78) | Other specialty (n=125) | P value | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||
| Reason for referral | .001 | ||||
| Substance use disorder | 12 (19.4) | 26 (24.8) | 12 (15.4) | 24 (19.2) | |
| Mental health | 11 (17.7) | 13 (12.4) | 9 (11.5) | 21 (16.8) | |
| Disruptive behavior | 13 (21.0) | 37 (35.2) | 47 (60.3) | 45 (36.0) | |
| Sexual boundaries | 24 (38.7) | 25 (23.8) | 6 (7.7) | 29 (23.2) | |
| Other | 2 (3.2) | 4 (3.8) | 4 (5.1) | 6 (4.8) | |
| Board involvement | 32 (51.6) | 35 (34.0) | 11 (14.1) | 28 (22.4) | <.001 |
| License sanctioned (previous) | 11 (18.3) | 11 (10.9) | 5 (6.6) | 11 (9.1) | .146 |
| License sanctioned (current) | 19 (31.1) | 21 (20.4) | 4 (5.3) | 16 (13.2) | <.001 |
| Privileges suspended (previous) | 7 (12.7) | 16 (17.6) | 10 (13.9) | 14 (12.4) | .738 |
| Privileges suspended (current) | 22 (40.0) | 34 (36.6) | 26 (35.6) | 41 (36.0) | .956 |
| In monitoring agreement (previous) | 10 (16.4) | 20 (19.6) | 9 (12.0) | 13 (10.6) | .235 |
| In monitoring agreement (current) | 16 (26.2) | 27 (26.7) | 19 (24.7) | 26 (21.1) | .772 |
3.4. Psychiatric diagnoses
Summaries of the diagnoses resulting from the evaluations are detailed in Table 5. The number of Axis I psychiatric disorders diagnosed for each subject was typically one or none (67%). The diagnosis made most frequently was substance use disorder (35.2%) followed by unipolar depression (19.4%). Approximately half of the referrals received an Axis II diagnosis, most commonly personality traits. The only substantial difference in rates of diagnoses among the specialties was a higher rate of bipolar spectrum illness among the group of family medicine specialties than among the other specialties (bipolar: 14 of 63, 22.6% vs. 10%–12% among all others, P=.012). Rates of sexual disorder diagnosis were higher among the family medicine (16 of 62, 26%) and internal medicine (19 of 109, 18%) physicians than they were among the surgical specialists (7 of 78, 9%) and other specialties (16 of 125, 13%) (P=.033) (data not shown).
Table 5.
Summaries of diagnoses of physicians referred to V- CAP
| Total (N=381) | |
|---|---|
| No. of Axis I diagnoses | N (%) |
| 0 | 116 (30.4) |
| 1 | 140 (36.7) |
| 2 | 78 (20.5) |
| 3 | 40 (10.5) |
| 4 | 7 (1.8) |
| Axis I diagnosesa | |
| Adjustment disorder | 41 (10.8) |
| Anxiety disorder | 24 (6.3) |
| Bipolar spectrum | 44 (11.5) |
| Cognitive disorder | 6 (1.6) |
| Dysthymia | 28 (7.3) |
| Mood disorder, not otherwise specified | 11 (2.9) |
| Posttraumatic stress disorder | 15 (3.9) |
| Psychotic disorder | 2 (0.5) |
| Sexual disorder | 64 (16.0) |
| Substance-induced mood | 4 (1.0) |
| Substance use disorder | 134 (35.2) |
| Unipolar depression | 74 (19.4) |
| Axis II diagnoses | |
| Personality disorder | 107 (28.1) |
| Personality trait | 176 (46.2) |
Other (13) Axis I psychiatric diagnoses not included in the table included organic (due to general medical condition) mood disorder (1), intermittent explosive disorder (4), attention-deficit disorder (1) and impulse control disorder (1).
The group of physicians who were referred for disruptive behavior problems had statistically significantly lower overall rates of primary psychiatric (Axis I) diagnosis than among the other referral groups (48% vs. 79%–96%, P<.001) and increased frequency of Axis II personality diagnoses (90% vs. 48%–66%, P<.001). Given the previously mentioned finding of higher rates of referral for disruptive behavior among the surgical specialists referred, it is not surprising that rates of Axis I diagnoses were statistically significantly lower in surgical specialties (39 of 78, 50%) than in the other specialty groups (family medicine: 45 of 62, 73%; internal medicine: 82 of 105, 78%; other specialties: 90 of 125, 72%; P<.001). Differences in rates of personality (Axis II) diagnoses among the various specialties were not statistically significant (P=.081) (data not shown).
3.5. Recommendations
Recommendations for various types of remediation were often made as a result of the evaluations and are summarized in Table 6. The therapeutic strategies recommended were intended to improve health and well-being or to enhance the professional conduct of most subjects, regardless of the FFD determination. The most commonly documented recommendations were for educational intervention (48.3%), psychotherapy (47.0%), monitoring (39.6%) and short-term (1–2 weeks) intensive treatment interventions (33.3%). Finally, approximately 70% (n=256 of 364) of the referrals were deemed fit to practice at the time of evaluation.
Table 6.
Summaries of recommendations for physicians referred to V-CAP
| Total(N=381) | |
|---|---|
| N (%) | |
| Residential treatment | 78 (20.5) |
| Medical follow-up | 71 (18.6) |
| Psychiatry follow-up | 37 (9.7) |
| Medication change | 57 (15.0) |
| Education | 184 (48.3) |
| Psychotherapy | 179 (47.0) |
| Intensives | 127 (33.3) |
| Monitoring | 151 (39.6) |
| Fit to practicea | 256 (70.3) |
Total n=364 with data.
3.6. Reason for referral and Axis I/II with fitness recommendation
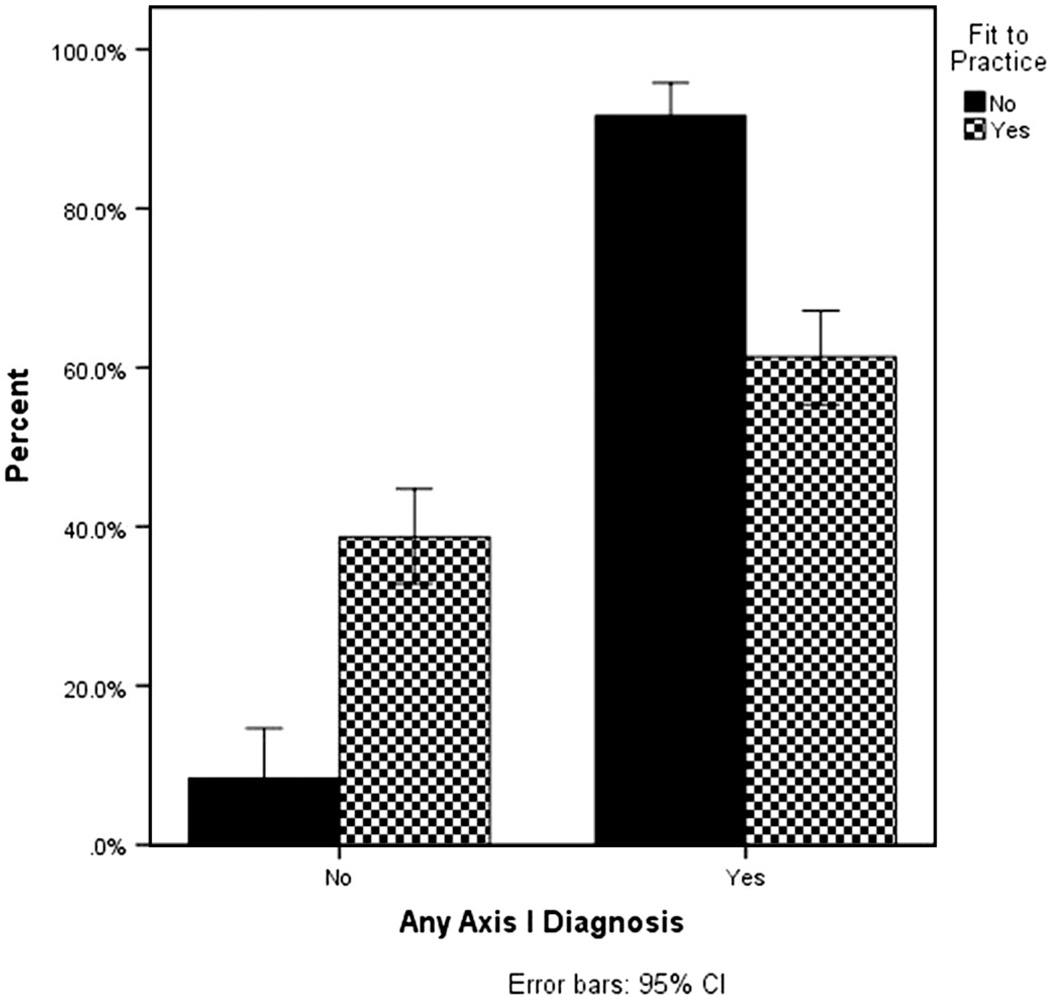
The association of an Axis I psychiatric diagnosis with the likelihood of a fit-to-practice recommendation is illustrated in Figure 1. A multiple logistic regression analysis that included reason for referral, Axis I diagnosis and Axis II diagnosis revealed that, after controlling for the associations of Axis I and Axis II diagnosis with a recommendation of fit to practice, the reason for referral was statistically significantly associated with a fit-to-practice recommendation (χ2(df=3)=28.74, P<.001). In comparison to the behaviorally disruptive physician referrals, each of the other three groups (substance use, mental health, sexual boundaries) was statistically significantly less likely to receive a fit recommendation [substance use: odds ratio (OR)=0.22, 95% confidence interval (CI)=0.10–0.47, P<.001; mental health: OR=0.14, 95% CI=0.06–0.31, P<.001; sexual boundaries: OR=0.27, 95% CI=0.13–0.58, P=.001]. Comparative analysis of the first half (2001–2007) and later half (2008–2012) of V-CAP evaluations revealed reasonable consistency between referral variables and findings (data not shown).
Fig. 1.
Association of Axis I diagnosis with fit-to-practice recommendation.
4. Discussion
The major finding of this analysis of results from FFD evaluations conducted over a 10-year period at our center is that physicians who were referred for alleged disruptive behavior (comprising 38% of all evaluations) had the lowest rate of Axis I psychiatric disorders (48%) and the highest proportion of abnormal personality (Axis II) diagnoses (90%), while being most likely (90%) to be deemed fit for duty as a result of the assessment. Physicians referred to our center were more likely to be middle-aged, white, male and US trained than would be predicted by AMA demographics.
Ford and Summer [19] (1997) described high rates of mixed and narcissistic personality (Axis II) diagnoses in physicians referred for assessment of behavior that had been disruptive to clinical care. They observed additionally that disruptive physicians rarely complied with recommended treatment [20]. Earlier reports describing physicians who required hospital admission [21–25] or rehabilitation treatment [26] provide few data for valid comparison with our findings, and not surprisingly, the incidence of psychotic illness appears lower in our sample of ambulatory physicians.
McGovern et al. [26] (2001) described 108 behavioral assessments of physicians, with a comparable age range but fewer female and “nonwhite” physicians than in our sample, and found higher rates of substance use disorders (58% vs. 38%). The lower rate of substance use diagnoses in our physician sample may be related to advances in addiction management [27–29]. Expertise in the recognition and management of substance use disorders in Physician Health Programs is now more widely available. Accordingly, referral for formal assessment of substance-use-disordered physicians may be necessary less often. Reduced rates of substance disorder diagnoses in our population may reflect a combination of improved recognition, diagnosis and treatment as well as decreasing stigmatization of addicted physicians.
Physician behavior that interferes with the optimal functioning of healthcare teams [30,31] can be detrimental to the culture of (clinical) safety [32]. Actions or speech by a physician that demeans, upsets or disrespects others decreases the ability of the clinical team to achieve its intended outcomes [33]. Such undermining behavior may be active (e.g., angrily throwing a scalpel), passive–aggressive (e.g., comments in patient records that are critical of other professionals) or passive (e.g., chronic lateness, failure to complete records or recurrent failure to respond to pager). Administrative guidelines from the Joint Commission [34,35] have now placed part of the responsibility for oversight of professional conduct onto the institutions in which physicians are employed or privileged to work [30]. Hospitals and practice groups increasingly identify and provide administrative management for physician behaviors that potentially diminish the quality of care. Continuation of privileges or employment may be threatened in order to increase physician compliance with various forms of corrective intervention.
Early recognition of disruptive behavior at the local level has been shown to result in prompt intervention and remediation [36]. Simple measures, such as giving formal peer feedback to the physician about the effects of problematic behaviors, with concurrently offered educational support, frequently allow the physician to understand and correct the dysfunctional behavior [37]. More specific approaches such as leadership training, professional coaching or practice management review may be employed to improve quality of care.
Remedial psychoeducational programs [38] that often offer continuing education credit are available [39] in several centers. These courses, many of which offer extended support and supervision, utilize transformational educational techniques [40] and 360° evaluation to assist the physician to recognize and modify the distressing behaviors that evoke complaints from patients or staff. A Vanderbilt Center for Patient and Professional Advocacy white paper [41] outlines administrative strategies for intervention if professionals may require referral for comprehensive evaluation.
The findings in this convenience sample are limited by unavoidable selection biases. The vast majority of referrals in our sample involved potential adjudication for licensure, privileges, insurance or potential exposure on the National Physician Data Bank [42]. Most of the physicians, except some referred by larger healthcare systems or the military, were personally responsible for the cost of assessment plus travel and accommodation. Finally, half of the referrals originated in our own state, Tennessee.
Referral for FFD evaluation tends to be requested when impairment is uncertain, when the cause is obscure or to clarify a basis for administrative action. Medical Boards, Physician Health Programs and executive committees of hospitals and practice groups routinely adjudicate the large majority of physician behavioral issues without requiring FFD for resolution. The number of referrals for FFD evaluation does not accurately reflect the incidence of problematic physician behaviors or the rate of impairment among medical practitioners. Referring healthcare systems differ in size and in the sophistication of administrative practices for dealing with problematic physician behaviors, and the decision to request FFD is subject to variability in severity and complexity. Finally, our findings clearly require replication and elaboration at other centers to which well-characterized physician samples have been referred for FFD evaluations.
5. Conclusion
This article describes results of data obtained during the evaluation of physicians referred for comprehensive fitness-for-duty assessment to the Vanderbilt Comprehensive Assessment Program. Our findings suggest that physicians referred for evaluation of alleged disruptive behavior were much more likely to be found fit for duty than those physicians referred for mental health issues, including substance abuse and sexual boundary issues. Behaviorally disruptive physicians significantly less frequently received primary Axis I psychiatric diagnoses and were more often diagnosed with Axis II personality abnormalities.
Maintaining a healthy physician workforce is vital for the healthcare of the nation and includes preventing impairment and reclaiming problematic physicians. Thorough, comprehensive, biopsychosocial evaluation of the doctors, their life and their workplace forms the current basis for informed opinion about safety to practice, upon which physicians, hospitals and medical boards frequently rely. For the potentially impaired practitioner, comprehensive FFD evaluation aims to provide accurate diagnosis and makes recommendations to improve health, enhance professionalism and facilitate return to safer, more effective practice.
Acknowledgments
The inspiration, guidance and support of Alexander Finlayson, M.B., Ch.B. (deceased), David T. Dodd, M.D. (deceased), Anderson Spickard Jr., M.D. and Pete Kopcsak, in establishing the Vanderbilt Comprehensive Assessment program is gratefully acknowledged. William H. Swiggart, MS, Stephan Heckers, MD, James W. Pichert PhD, James S. Walker, PhD, and Kimberly P. Brown, PhD provided editorial suggestions.
Footnotes
This study was approved (IRB #08060 and IRB #060459) by the Institutional Review Board, Vanderbilt University. The project (publication) described was supported by CTSA award no. UL1TR000445 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
References
- 1.American Board of Internal Medicine Foundation, American College of Physicians, European Foundation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med. 2002;136:243–246. doi: 10.7326/0003-4819-136-3-200202050-00012. [DOI] [PubMed] [Google Scholar]
- 2.AMA. [Accessed November 14, 2012];Code of medical ethics. Available at http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics.page. [Google Scholar]
- 3.Anfang SA, Faulkner LR, Fromson JA, Gendel MH. The American Psychiatric Association's resource document on guidelines for psychiatric FFD evaluations of physicians. J Am Acad Psychiatry Law. 2005;33:85–88. [PMID: 15809244] [PubMed] [Google Scholar]
- 4.Reynolds NT. A model comprehensive psychiatric fitness-for-duty evaluation. Occup Med. 2002;17:105–118. [PubMed] [Google Scholar]
- 5.Anfang SA, Wall BW. Psychiatric FFD evaluations. Psychiatr Clin North Am. 2006;29:675–693. doi: 10.1016/j.psc.2006.04.009. [PMID: 16904505] [DOI] [PubMed] [Google Scholar]
- 6.Meyer DJ. Psychiatry malpractice and administrative inquiries of alleged physician misconduct. Psychiatr Clin N Am. 2006;29:615–628. doi: 10.1016/j.psc.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Gendel M. Substance misuse and substance-related disorders in forensic psychiatry. Psychiatr Clin N Am. 2006;29:649–673. doi: 10.1016/j.psc.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Reid WH. Evaluating and treating disabled or impaired colleagues. J Psychiatric Pract. 2007;13:44–48. doi: 10.1097/00131746-200701000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Myer DJ, Price M. Forensic psychiatric assessments of behaviorally disruptive physicians. J Am Acad Psychiatry Law. 2006;34:72–81. [PubMed] [Google Scholar]
- 10.Division of Survey and Data Resources. American Medical Association; 2011. Physician characteristics and distribution in the US, 2011 edition; pp. 1–46. [Google Scholar]
- 11.Butcher JN, Dahlstrom WG, Graham JR, et al. The Minnesota Multiphasic Personality Inventory-2 (MMPI-2) manual for administration and scoring. Minneapolis, MN: University of Minneapolis Press; 1989. [Google Scholar]
- 12.Morey LC. Personality Assessment Inventory. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- 13.Bar-On R. Emotional Quotient Inventory (EQ-i): technical manual. Toronto, Canada: Multi-Health Systems; 1997. [Google Scholar]
- 14.Nasreddine Z. 2003 to 2011 — The Montreal Cognitive Assessment — MoCA©. [on December 29, 2011]; Accessed at http://www.mocatest.org/ [Google Scholar]
- 15.Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 16.Weschler D. Weschler Adult Intelligence Scale. New York: PsycholCorp; 1955. [Google Scholar]
- 17.Reitan RE, et al. Investigation of the validity of Halstead's measures of biological intelligence. Arch Neurol Psychiatry. 1955;73:28–35. doi: 10.1001/archneurpsyc.1955.02330070030005. [DOI] [PubMed] [Google Scholar]
- 18.Diagnostic and statistical manual of mental disorders, Fourth Edition, Text Revision (DSM-IV-TR) Arlington, VA: American Psychiatric Association; 2000. [Google Scholar]
- 19.Summer G, Ford C, Lightfoot W. The disruptive physician, I: the Alabama physicians' recovery network. Fed Bull. 1997;84:236–243. [Google Scholar]
- 20.Ford CV, Summer GL. The disruptive physician, II: the role of personality disorders. Fed Bull. 1998;85:20–29. [Google Scholar]
- 21.Duffy JC, Litin EM. Psychiatric morbidity of physicians. JAMA. 1964;189(13):989–992. doi: 10.1001/jama.1964.03070130009002. [DOI] [PubMed] [Google Scholar]
- 22.Small IF, Small JG, Assue CM, Moore DF. The fate of the mentally ill physician. Am J Psychiatry. 1969;125(10):1333–1342. doi: 10.1176/ajp.125.10.1333. [DOI] [PubMed] [Google Scholar]
- 23.Vincent MO, Robinson EA, Latt L. Physicians as patients: private psychiatric hospital experience. Can Med Ass J. 1969;100(9):403–412. [PMC free article] [PubMed] [Google Scholar]
- 24.Jones ER. A study of 100 physician psychiatric inpatients. Am J Psychiatry. 1977;134:1119–1123. doi: 10.1176/ajp.134.10.1119. [DOI] [PubMed] [Google Scholar]
- 25.Katsavdakis KA, Gabbard GO, Athley GI. Profiles of impaired health professionals. Bull Menninger Clin. 2004;68:60–72. doi: 10.1521/bumc.68.1.60.27732. [DOI] [PubMed] [Google Scholar]
- 26.McGovern MP, Angres DH, Leon S. for assessment at a behavioral health center. J Addictive Diseases. 2000;19:59–73. doi: 10.1300/J069v19n02_05. [DOI] [PubMed] [Google Scholar]
- 27.Baldisseri MR. Impaired healthcare professional. Crit Care Med. 2007;35(Suppl):S106–S116. doi: 10.1097/01.CCM.0000252918.87746.96. [DOI] [PubMed] [Google Scholar]
- 28.DuPont RL, McLellan AT, Carr G, Gendel M, Skipper GE. How are addicted physicians treated? A national survey of physician health programs. J Subst Abuse Treat. 2009;37:1–7. doi: 10.1016/j.jsat.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 29.McLellan AT, Skipper GS, Campbell M, DuPont RL. Five year outcomes in a cohort study of physicians treated for substance use disorders in the United States. BMJ. 2008;337:a2038. doi: 10.1136/bmj.a2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Piper LA. Addressing the phenomenon of disruptive physician behavior. Health Care Manag. 2003;22:335–339. doi: 10.1097/00126450-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Leape LL, Shore MF, Dienstag JL, et al. Perspective: A Culture of Respect, Part 1: The Nature and Causes of Disrespectful Behavior by Physicians. Academic Med. 2012;87:845–852. doi: 10.1097/ACM.0b013e318258338d. [DOI] [PubMed] [Google Scholar]
- 32.The Joint Commission. [Accessed May 7, 2011];Issue 40: behaviors that undermine a culture of safety. Available at http://www.jointcommission.org/assets/1/18/SEA_40.PDF. [Google Scholar]
- 33.Reason J. Human error. Boston: Cambridge University Press; 1990. [Google Scholar]
- 34.Stewart DM., Jr (Chair) American Medical Association Council on Ethical and Judicial Affairs. [Accessed July 19, 2013];AMA Code of Ethics Opinion 9.045 Behaviors that Undermine a Culture of Safety 2012. Available at http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion9045.page. [Google Scholar]
- 35.Rosenstein AH. The quality and economic impact of disruptive behaviors on clinical outcomes of patient care. Am J Med Quality. 2011;26:372–379. doi: 10.1177/1062860611400592. [DOI] [PubMed] [Google Scholar]
- 36.Hickson GB, Entman SS. Physicians' influence and the malpractice problem. Obstet Gynecol. 2010;115(4):682–686. doi: 10.1097/AOG.0b013e3181d732e9. [DOI] [PubMed] [Google Scholar]
- 37.Pichert JW, Hickson G, Moore I. [Accessed May 5, 2013];Using patient complaints to promote patient safety. Available at http://www.ncbi.nlm.nih.gov/books/NBK43703/ [PubMed]
- 38.McLaren K, Lord J, Murray S. Delivering effective and engaging continuing medical education on physicians' disruptive behavior. Academic Med. 2011;86:612–617. doi: 10.1097/ACM.0b013e318212e8ea. [DOI] [PubMed] [Google Scholar]
- 39.VUMC. [Accessed April 16, 2011];The Center for Professional Health. Available at http://www.mc.vanderbilt.edu/root/vumc.php?site=cph. [Google Scholar]
- 40.Samenow CP, Worley LLM, Neufeld R, Fishel T, Swiggart WH. Transformative learning in a professional development course aimed at addressing disruptive physician behavior: a composite case study. Acad Med. 2013;88:1–7. doi: 10.1097/ACM.0b013e31827b4cc9. [DOI] [PubMed] [Google Scholar]
- 41.Vanderbilt CPPA. [Accessed May 4, 2013];Referring a health care professional for assessment. Available at http://www.mc.vanderbilt.edu/centers/cppa/news/White_Paper_Referrals_March2013.pdf. [Google Scholar]
- 42.The National Practitioner Data Bank. Information. [Accessed July 19, 2013]; Available at http://www.npdb-hipdb.hrsa.gov.