Abstract
Do differences in rates of use among managed care and Fee-for-Service Medicare beneficiaries reflect selection bias or successful care management by insurers? I demonstrate a new method to estimate the treatment effect of insurance status on health care utilization. Using clinical information and risk-adjustment techniques on data on acute admission that are unrelated to recent medical care, I create a proxy measure of unobserved health status. I find that positive selection accounts for between one-quarter and one-third of the risk-adjusted differences in rates of hospitalization for ambulatory care sensitive conditions and elective procedures among Medicare managed care and Fee-for-Service enrollees in 7 years of Healthcare Cost and Utilization Project State Inpatient Databases from Arizona, Florida, New Jersey and New York matched to Medicare enrollment data. Beyond selection effects, I find that managed care plans reduce rates of potentially preventable hospitalizations by 12.5 per 1,000 enrollees (compared to mean of 46 per 1,000) and reduce annual rates of elective admissions by 4 per 1,000 enrollees (mean 18.6 per 1,000).
1 Introduction
A long-standing question in health economics asks whether managed care and insurance design can reduce health care utilization without affecting quality of care. There is a lack of consensus in the literature, and evaluations of the effects of managed care on quality of care and unnecessary utilization have been limited by the challenge of differentiating quality of care from patient selection. Proponents of managed care have long argued that competition between plans can improve efficiency in the Medicare program and consequently reduce government spending. Although enrollment in and spending on MMC plans has increased dramatically over the past several years with over a quarter of all Medicare beneficiaries now enrolled in a Medicare managed care (MMC) plan, little is known about the care that they receive (Kaiser Family Foundation, 2011).
The MMC program, currently known as Medicare Advantage, was first introduced as a way to provide Medicare beneficiaries with additional benefits while reducing Medicare spending on their care. MMC plans contract with the government to provide both basic Medicare coverage and supplemental benefits to Medicare beneficiaries who choose managed care over traditional Fee-for-Service (FFS) Medicare. Plans were expected to compete on price and quality, generating savings that plans would use to offer additional benefits or reduced cost-sharing to enrollees (White House, 2003). However, critics contend that MMC plans merely attract the healthiest Medicare beneficiaries, and therefore spend less on average than FFS because their enrollees have lower utilization (Berenson, 2004; MedPAC, 2006).
Despite encouraging findings in other populations, previous research indicates problems in MMC on a variety of dimensions, including beneficiary dissatisfaction with care and receipt of appropriate services in the inpatient, outpatient and rehabilitative settings (Retchin et al., 1997; Experton et al., 2000; Guadagnoli et al., 2000; Landon et al., 2004). Although other studies find that MMC plans outperform FFS on some measures of preventive service use and do reduce out-of-pocket spending for enrollees (Gold et al., 2004; Landon et al., 2004; Morales et al., 2004; Rizzo, 2005), most of this research relies on older administrative data released prior to changes to the MMC program and MMC plan reporting requirements. After 1997, MMC plans were largely exempted from reporting data about the amount and quality of care provided to enrollees.
Most studies of managed care quality have been unable to address the adverse selection problem that arises because sicker people are less likely to enroll in managed care. This makes it difficult to determine whether managed care improves health or simply attracts the healthy. Those studies that used econometric approaches to correct for this bias have focused on a limited number of self-report and mortality outcomes (Mello et al., 2002; Rizzo, 2005; Balsa et al., 2007; Huesch, 2010; Dowd et al., 2011). This study uses administrative data covering the universe of hospitalizations in Arizona, Florida, New Jersey and New York from 1999 through 2005, states where nearly a quarter of MMC enrollees lived during the study period. The study compares rates of hospitalizations for MMC and FFS enrollees for conditions reflecting both quality and access to care.
Two types of hospitalizations are compared for MMC and FFS enrolles. The first type, Ambulatory Care Sensitive (ACS) admissions, are hospitalizations for conditions that could be prevented through timely and effective outpatient services such as vaccination and antibiotic use. Lower rates of ACS admissions conditional on patient characteristics are evidence of higher quality outpatient care.1 The second type, Referral-sensitive (RS) admissions are hospitalizations for elective heart and joint replacement surgery, which are indicators of access to costly elective procedures. Because these types of admissions require a specialist’s referral, lower rates of RS admissions can indicate problems accessing specialty care.
Differences in rates of ACS and RS admissions are driven by underlying differences in the health and health behavior of MMC and FFS enrollees (selection) and the differential care provided to enrollees. I develop a measure of typically unobserved underlying health status and health behavior to isolate the contribution of quality versus selection. This measure is based on the ratio of observed to expected (OE ratio) marker hospitalizations; admissions for acute medical events such as hip fractures that occur regardless of quality of care or amount of recent health care consumption (Billings, 2003). Marker hospitalizations previously have been used in the health economics literature because they are not influenced by insurance type or health care access (Backus et al., 2002; Aizer, 2003; Card et al., 2009). I show that marker hospitalizations do, however, correlate with other measures of patient health and health behaviors that may influence both choice of MMC and subsequent health care utilization. These properties enable me to use the marker OE ratio as a proxy for the omitted health status information.
This paper contributes to the literature by providing new evidence about the quality of care provided by MMC plans and by proposing a methodology for differentiating quality and selection effects in situations when health insurance choice is non-random. A similar approach may be used to evaluate insurance options offered through Affordable Care Act implementation. Fixed effect regressions controlling for enrollee demographic characteristics, county and year fixed effects highlight marked differences in rates of hospitalization between MMC and FFS enrollees. MMC enrollees average 17.3 fewer ACS admissions per 1,000 enrollees per year (overall mean 46) and 6.3 fewer RS admissions (overall mean 18.6).
Estimates using the marker hospitalization OE ratio to control for enrollee health status indicate that positive selection into MMC accounted for 23 to 35 percent of the observed differences in risk-adjusted rates of ACS and RS admissions during the study period. MMC plans reduced annual rates of ACS admissions by 12.5 hospitalizations per 1,000 enrollees relative to FFS, with reductions driven by conditions that can be managed with rapid provision of antibiotics or other low-cost interventions. MMC plans also reduced annual rates of RS admissions by 4.1 admissions per 1,000 enrollees per year.
2 Managed Care and Health Care Utilization
2.1 Medicare Managed Care
Managed care plans have provided services to some Medicare beneficiaries since the 1980s. This paper focuses on the program from 1999 through 2005, when it was known first as Medicare+Choice and later as Medicare Advantage. Beneficiaries who choose to enroll in MMC accept restrictions on provider networks and utilization in return for additional benefits not covered by FFS Medicare. Supplementary benefits offered during the study period included lower out-of-pocket spending on cost-sharing and premiums as well as and benefits for services not covered under FFS Medicare including some preventive services, dental care, gym memberships and prescription drug coverage.2 During the years of analysis, MMC enrollment was concentrated in Health Maintenance Organizations (HMOs), a form of managed care typified by restrictions on access to specialists and use of gatekeeper primary care physicians who would manage care of enrollees. Participation in MMC was and continues to be voluntary for health plans and Medicare beneficiaries.
Capitated monthly payments to plans were set at the county level and adjusted for enrollee age, sex, Medicaid eligibility and institutional status. Between 2001 and 2003, Medicare phased in more complete risk adjustments, ultimately basing 30 percent of the payment on demographic and utilization characteristics.3
Incomplete risk adjustment during the study period provided incentive for plans to attempt to enroll healthier-than-average Medicare beneficiaries in the hope of reducing the proportion of high-cost enrollees. Medicare beneficiaries have heterogeneous and widely varying health spending patterns (CBO, 2005). In 2001, for example, 5 percent of Medicare enrollees accounted for 43 percent of FFS spending, while the 50 percent of beneficiaries with lowest utilization accounted for only 4 percent of program expenditures. Plans may have found it more profitable to discourage the highest-cost beneficiaries from enrolling than to find ways of reducing the cost of their care. Another complicating factor during the study period was that MMC enrollees could disenroll from plans monthly, which put plans at risk of losing members before realizing cost returns on long-term investments in members’ health.
2.2 Conceptual Framework
Hospital care, which accounts for more than 40% of FFS spending, is a natural starting point for MMC cost-saving efforts. Capitated payments create financial incentives for plans to reduce hospital admission rates. Studies ranging from the RAND Health Insurance Experiment to recent work in Medicare report reductions in hospital care under managed care (Newhouse, 1993; Landon et al., 2013) Managed care plans can achieve this through several channels.
Improve or maintain enrollee health. Managed care plans can directly influence demand for outpatient medical services believed to reduce hospitalization by encouraging members to receive vaccinations and preventive services by reducing the financial or time costs (Landon et al., 1998). Plans may facilitate use of high-quality care by contracting only with high-quality physicians and providers who give better care. (Landon et al., 1998).
Reduce Utilization. Plans can influence the services a patient uses by altering physician behavior through financial incentives, treatment guidelines and utilization review, including denial of payments for services deemed unnecessary or inappropriate (Landon et al, 1998). These strategies may improve quality of care by reducing overprovision of profitable elective procedures and excessive diagnostic testing, or they may reduce quality of care by denying treatment to patients who would benefit from service receipt.
Positive Selection/Benefit Package Design. Managed care plans can limit spending on hospitalizations by attracting relatively healthy beneficiaries who will require fewer expensive services (including hospital stays), a practice known as ‘cream-skimming’ or positive selection. This approach does not focus on quality of care provided to beneficiaries, but on designing benefit packages that will predominantly appeal to enrollees with low expected utilization. For example, higher cost-sharing for treatments of chronic illnesses may discourage high-utilization beneficiaries from enrolling.
2.3 Empirical Evidence
A large body of work has considered the effects of commercial health maintenance organizations on health care spending, access to preventive services, quality and satisfaction with care received. Most of the commercially insured population is currently enrolled in some form of managed care, creating interest in evaluating the effects of managed care on health outcomes (Glied, 2000). In a series of literature reviews synthesizing two decades of research on managed care, Miller and Luft (1994; 1997; 2002) consistently find mixed evidence of the effects of managed care on many dimensions of health and utilization. Managed care plans generally outperform comparison groups on measures of preventive service use, but look worse on other quality measures.
Studies of Medicare managed care comprise a relatively small area of the managed care literature, but are more likely to find negative effects of HMOs on quality than the commercial HMO literature (Miller and Luft, 2002). Several recent papers have evaluated survey data collected by the Centers for Medicare and Medicaid Services (CMS) to monitor quality in MMC and FFS. Nationally, MMC enrollees average lower satisfaction with overall care received and with physician and specialty services than are FFS beneficiaries (Landon et al., 2004; Rizzo, 2005).
Additionally, for-profit Medicare managed care plans (which enroll the majority of MMC ben-eficiaries) have lower quality scores than non-profit plans on measures including breast cancer screening, diabetic eye examination, beta-blocker medication after heart attack, and follow-up after hospitalization for mental illness (Schneider et al., 2005). Huesch (2010) found that MMC patients in Florida undergoing cardiac stenting were treated by physicians with worse average patient outcomes than physicians used by FFS patients.
MMC plans typically outperform FFS on measures of preventive care. MMC beneficiaries are more likely to receive pneumonia and influenza vaccinations and advice to quit smoking than those in FFS (Landon et al., 2004). Some studies suggest that MMC enrollment mitigates racial and socioeconomic disparities in rates of preventive service use and access to care (Morales et al., 2004; Balsa et al., 2007).
Mello et al. (2003) analyzed survey data and reviewed 18 studies on the health status of MMC enrollees through 1996, find evidence of positive selection on many but not all measures of health status and sociodemographic characteristics used to proxy for health status. A small number of studies that analyze recent survey data find that those leaving MMC are likely to be worse health than those who remain in MMC and that MMC enrollees report better levels of health than FFS beneficiaries (Mobley et al., 2007; Shimada et al., 2009).
3 Data
I use hospital discharge data the State Inpatient Databases (SID; Arizona, Florida, and New York), Healthcare Cost and Utilization Project (HCUP), created by the Agency for Healthcare Research and Quality from 1999 through 2005 and New Jersey SID data from 2003 – 2005.4 SID data contain the universe of discharge abstracts for all in-state hospitalizations including diagnostic and procedure codes and payer information. The four states included in this project are chosen because they report whether the payer for each Medicare hospitalization is FFS or MMC and provide geographic identifiers at the county or zip code level. During the study period, nearly 25 percent of all MMC enrollees resided in one of these states. The HCUP data have been used in other studies to examine the care of MMC and FFS patients residing in these states (Zhan et al., 2004; Basu and Mobley, 2007; Nicholas, 2011).5
International Classification of Disease (ICD-9) diagnostic and procedure codes are used to identify three different types of hospitalizations among Medicare beneficiaries detailed in Table 2 and described below.
Table 2.
Rates of Hospitalization Per 1,000 Medicare Beneficiaries by Type of Admission
| Overall | MMC | FFS | |
|---|---|---|---|
| Ambulatory Care Sensitive (all) | 45.98 (22.35) | 30.04 (16.63) | 61.91 (14.65) |
| Acute ACS | 17.62 (9.26) | 10.77 (6.14) | 24.47 (6.32) |
| Dehydration | 3.28 (1.96) | 1.95 (1.33) | 4.61 (1.53) |
| Pneumonia | 10.42 (5.55) | 6.47 (3.75) | 14.36 (4.06) |
| Ruptured Appendix | 0.23 (0.17) | 0.18 (0.20) | 0.28 (0.11) |
| Urinary Tract Infection | 3.93 (2.34) | 2.36 (1.66) | 5.49 (1.82) |
| Chronic ACS | 28.36 (13.67) | 19.27 (10.97) | 37.44 (9.40) |
| Angina | 1.10 (1.03) | 0.79 (0.84) | 1.40 (1.12) |
| Asthma | 1.42 (1.08) | 0.95 (0.84) | 1.89 (1.10) |
| Chronic Obstructive Pulmonary Disease | 7.57 (2.86) | 5.63 (2.34) | 8.21 (2.72) |
| Congestive Heart Disease | 17.76 (5.63) | 12.51 (4.9) | 19.5 (4.7) |
| Diabetes Short-term | 0.30 (0.23) | 0.22 (0.24) | 0.38 (0.20) |
| Diabetes Long-term | 2.29 (1.46) | 1.59 (1.29) | 2.99 (1.27) |
| Diabetes Uncontrolled | 0.32 (0.33) | 0.21 (0.28) | 0.42 (0.34) |
| Diabetes Amputation | 0.76 (0.49) | 0.53 (0.47) | 0.99 (0.39) |
| Hypertension | 0.84 (0.62) | 0.64 (0.61) | 1.05 (0.55) |
| Referral-Sensitive (all) | 18.59 (8.78) | 14.41 (7.68) | 22.77 (7.76) |
| Angioplasty | 6.50 (3.96) | 5.09 (3.47) | 7.90 (3.93) |
| Coronary Artery Bypass | 3.14 (1.90) | 2.75 (2.08) | 3.53 (1.60) |
| Elective Joint Replacement | 7.05 (3.72) | 5.20 (3.31) | 8.90 (3.14) |
| Pacemaker Insertion | 1.91 (1.41) | 1.37 (1.31) | 2.45 (1.29) |
| Marker (all) | 8.73 (4.60) | 5.28 (3.00) | 12.18 (3.10) |
| Appendicitis | 0.32 (0.22) | 0.22 (0.22) | 0.43 (0.16) |
| Gastrointestinal Obstruction | 2.97 (1.58) | 1.87 (1.14) | 4.08 (1.11) |
| Hip Fracture | 5.43 (3.04) | 3.18 (1.94) | 7.67 (2.16) |
|
| |||
| MMC*County*Year Observations 22 | 822 | 411 | 411 |
HCUP SID and Medicare data, AZ, FL, NJ, NY 1999–2005.
Standard deviations in parentheses.
Insurance type, county, year cells weighted by enrollment.
Ambulatory Care Sensitive (ACS) Admissions are potentially avoidable hospitalizations for conditions that can be managed or prevented through effective primary care, such as complications of diabetes or high blood pressure. ACS admissions often signify lack of access to primary care or receipt of low-quality services (Billings et al., 1996). Lower rates of ACS admissions per 1,000 enrollees indicate higher quality of care. I examine rates of ACS hospitalizations for acute and chronic conditions separately since they represent different dimensions of outpatient care. Acute admissions are potentially preventable through timely outpatient intervention or vaccination, while admissions for chronic conditions may be prevented with ongoing monitoring and patient compliance.
Referral-Sensitive Admissions include elective surgical procedures, such as total hip replacement. These are high-cost procedures that can improve patient well-being and generally require a referring physician, indicating that the patient received necessary outpatient services prior to the admission (Billings, 2003; Billings et al., 1993). From an efficiency standpoint, it is unclear whether higher or lower rates of these admissions are desirable as they should be performed in accordance with patient preferences. Accordingly differences in rates are uninterpretable as signals of quality, though very high (low) rates may indicate overprovision (barriers to access).
Marker Admissions are inpatient hospitalizations for acute conditions such as hip fractures which are unlikely to be affected by recent primary care. There are clear practice guidelines and agreements across providers that patients with one of these conditions should be hospitalized (Billings, 2003). Marker hospitalizations are non-deferrable admissions that occur with similar frequency on weekdays and weekends (Card et al., 2009). These admissions provide information about enrollees’ underlying health status.
SID data provide a unique resource for analyzing health care utilization among MMC en-rollees absent plan encounter data. Since inpatient data only contain information about patients hospitalized in a given year, patient-level data are aggregated to provide counts of each type of hospitalization, Hicy for patients with insurance type i in county c in year y. I include all hospital-izations among patients age 65 and older with MMC or FFS as the primary payer. These counts are merged with total enrollment counts and average demographic characteristics (age, race, sex, Medicaid dual eligibility and End Stage Renal Disease status) for MMC and FFS enrollees taken from the 100 percent Medicare Beneficiary Annual Summary File (BASF) aggregated in the same fashion.6 The dependent variables of interest are rates of hospitalization by admission type per 1,000 Medicare beneficiaries.
MMC is arranged at the county level. CMS sets payment rates for each county, and insurers decide which counties to enter and what products to offer in each county. There are 1,071 county-years of data in the merged dataset, including many small counties and counties with no MMC availability. The analysis sample is limited to counties with at least 1,500 MMC enrollees and 5,000 Medicare beneficiaries. These restrictions ensure that the cells are large enough to generate reliable hospitalization rates. Estimates of the magnitude of selection into MMC will be biased toward no selection if the FFS sample includes beneficiaries who are unable to opt into an MMC plan as well as those who actively choose to remain in FFS. The final sample includes 822 insurance type-county-year cells from 84 counties. 81% of Medicare beneficiaries in the included state years and 98% of MMC enrollment live in these counties.
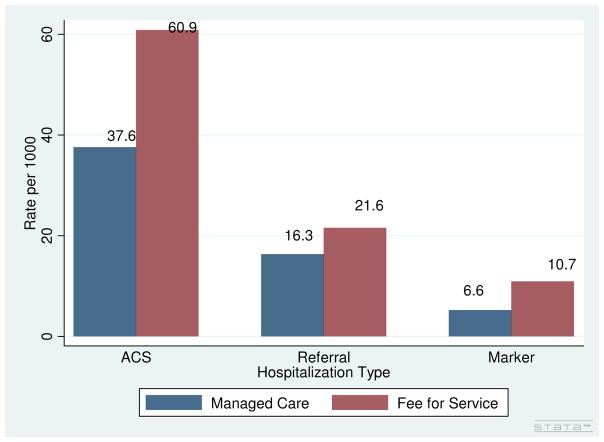
MMC and FFS enrollees are demographically similar (Table 1). The two groups do not differ on age or gender, but MMC enrollees are more likely to be Black (11 % vs. 9%) and less likely to be dually eligible for Medicaid, a rough measure of socioeconomic status (8% vs. 14%). However, MMC enrollees average lower rates of all types of hospitalization during the study period (Figure 1, Table 2). MMC enrollees experience fewer ambulatory care sensitive (37.6 vs. 60.9 per 1,000 enrollees), referral-sensitive (16.3 vs. 21.6), and marker (6.6 vs. 10.7) admissions. The large differences in hospitalization rates across the two demographically similar enrollee populations is consistent with either positive selection into MMC (patients differing on unobserved health characteristics), the influence of managed care on utilization patterns, or both.
Table 1.
Summary Statistics: Medicare Enrollment Demographics
| Overall | Managed Care | Fee-for-Service | |
|---|---|---|---|
| Black | 0.07 (0.08) | 0.08 (0.09) | 0.07 (0.06) |
| Hispanic | 0.02 (0.04) | 0.02 (0.04) | 0.02 (0.04) |
| Other Race | 0.02 (0.02) | 0.02 (0.02) | 0.03 (0.02) |
| Female | 0.57 (0.03) | 0.57 (0.03) | 0.57 (0.03) |
| Medicaid | 0.09 (0.07) | 0.06 (0.04) | 0.12 (0.08) |
| Age | 74.8 (1.8) | 74.6 (1.3) | 75.0 (2.2) |
| End Stage Renal Disease | 0.004 (0.003) | 0.003 (0.001) | 0.006 (0.003) |
|
| |||
| MMC*County*Year Observations | 822 | 411 | 411 |
Medicare Beneficiary Annual Summary File data at the county-insurance status-year level of aggregation for Medicare beneficiaries aged 65 and up in AZ, FL, NJ, NY 1999–2005. Sample limited to 84 counties with at least 1,500 MMC and 5,000 FFS beneficiaries. Standard deviations in parentheses.
Figure 1.
Rates of Hospitalization per 1,000 Enrollees: Medicare Managed Care vs. Fee-for-Service, AZ, FL, NJ, NY, 1999 – 2005
4 Empirical Approach
If Medicare beneficiaries were randomly assigned to MMC or FFS, the treatment effect of managed care on rates of hospitalization Hicy could be estimated as
| (1) |
where X is a vector of exogenous, observable (to payers and researchers) beneficiary characteristics used for risk adjustment, C is a vector of county fixed effects that captures time-invariant health and practice pattern characteristics of the beneficiary’s county of residence, Y is a vector of year fixed effects, and ζicy is a mean zero error term.
In practice, Medicare beneficiaries voluntarily enroll in managed care plans available in their county of residence, with private information about their health status and preferences for health care utilization that are unobservable to analysts. Estimates of the γ term in Equation (1) will be biased if health is related to the choice of coverage type and hospital usage. The literature on MMC selection suggests a positive correlation between health status MMC enrollment, so isolating the true effect of managed care on utilization requires a measure of beneficiary health status Zicy in Equation (1). I assume that Zicy is a continuous measure of health status and preferences covering the spectrum of expected utilization from low (healthy, prefer maintenance care only) to high users (complex health conditions, frequent specialist care).
| (2) |
Under a standard omitted variables bias framework, γ represents the sum of the true MMC effect and the health status effect scaled by the partial correlation between Zicy and MMCicy, α + β* ρMMC,Z. Under positive selection into MMC, omission of a health status measure will overstate the effect of MMC in reducing rates of hospitalization.
I use marker hospitalizations to create a proxy for Zicy (Wooldridge, 2002). As there is uniform clinical agreement in the medical community about the need for admission (Billings, 2003; Dart-mouth Atlas, 2006), the SID data include the universe of patients experiencing a marker condition regardless of the patient’s insurance status. These conditions (and resulting hospital admissions) occur independent of the quality or amount of recent health care consumption, and are thus un-correlated with differential quality of care by insurance type. However, marker hospitalizations do correlate with health status and behavioral measures that may affect the decision to enroll in managed care, and therefore can be used to proxy for selection.
4.1 Clinical Properties of Marker Hospitalizations
4.1.1 Hip Fractures
Hip fractures are common in older adults with low bone density (Karlsson et al., 2005; Jackson et al., 2006). While exercise and weight-bearing exercise can mildly increase bone mass density among older adults, most accumulation occurs early in life and is complete by adulthood (Karlsson et al., 2005). Despite common beliefs that calcium and vitamin D can protect against hip fracture risk, large, randomized clinical trials typically find no evidence to support this claim (Finkelstein, 2006). During the study period, physicians rarely diagnosed osteoporosis, the loss of bone mass density that increased fracture risk, so patient information about risk is also unlikely to be related to health care utilization.
4.1.2 Intestinal Obstruction
Intestinal obstruction occurs when the bowels are partially or fully blocked, which can be induced by mechanical causes such as abdominal twisting, or by ileus, where the bowel function is impeded without anatomic problem (Medline, 2007). Obstructions generally cannot be prevented through medical care, though risk is believed to be exacerbated by patients consuming low-fiber diets (Bogardus, 2006). Consequently, these types of hospitalizations can provide information about patient health behavior (diet) and underlying propensity to need hospital care. I exclude all obstructions with a secondary diagnosis of cancer, because cancer can increase the likelihood of developing certain types of intestinal obstructions.
4.1.3 Appendicitis
Appendicitis, an inflammation of the vermiform appendix, is believed to be caused by trapped food, worms, or fecal matter resulting in inflammation. This acute condition can happen at any time, and no peer-reviewed studies have found a way to prevent onset, suggesting that it is unrelated to preventive health care utilization or behavior (Braveman et al., 1994). Incidence of appendicitis is highest in children, so beneficiaries would also have private information about whether their risk for appendectomy is zero (previously removed), or non-zero.
4.2 Econometric Rationale for Marker Hospitalizations
Marker hospitalizations are useful indicators of patient selection because they correlate with two typically unobserved determinants of managed care enrollment; underlying health status and health behaviors. Table (3) demonstrates the correlation between experiencing a hip fracture in a given year and several chronic conditions measured in the BASF.7 Hip fracture is positively and significantly correlated with numerous chronic conditions including arthritis, heart disease and chronic obstructive pulmonary disease. Calculations are based 10% random sample of 2004 the Medicare Beneficiary Annual Summary File.
Patient preferences for preventive service use may also both influence selection into managed care and subsequent hospital utilization (Rizzo, 2005). Health and Retirement Study survey data from 1996 to 2008 are used to demonstrate the relationship between hip fractures and health behaviors in the previous period. Since injuries in the current period may impede patients’ ability to receive routine primary care, I consider the association between smoking and preventive service use in the previous wave and whether the respondent has a hip fracture during the current wave. Linear probability models are estimated to control for age, since some services are less appropriate for older patients. Table (4) shows a negative relationship between the probability of hip fracture and preventive health behaviors; hip fractures are more likely among smokers and less likely among flu shot recipients and women who have mammographies and breast exams.
Table 4.
Age-Adjusted Relationship Between Hip Fracture and Lagged Health Behaviors
| Smoking | Flu Shot | Cholesterol Screening | Mammogram | Breast Exam | Pap Smear | Prostate Exam | |
|---|---|---|---|---|---|---|---|
| Hip Fracture | .04** | −0.03† | −0.01 | −0.03† | −0.03† | −0.02 | −0.02 |
| 0.01 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.03 | |
|
| |||||||
| N | 66,109 | 66,109 | 66,109 | 38,088 | 38,088 | 38,088 | 28,021 |
Statistically significant at
p < 0.10,
p < 0.05,
p < 0.01.
Health and Retirement Study data, 1996 – 2008. Linear probability model regression coefficients control for age. Association between reporting a hip fracture and health behaviors in the previous 2-year period.
4.3 Estimation Strategy
Two assumptions are necessary for an observable characteristic, Q, to be used as a proxy variable to mitigate omitted variable bias (Wooldridge, 2002). A valid proxy variable should be redundant or ignorable in a regression after controlling for the omitted variable, so that if we had the omitted Zicy, E[Hicy,|Xicy, Zicy, Qicy] = E[Hicy |Xicy, Zicy]. Additionally, there should be no significant relationship between Zicy and the other explanatory variables after partialling out the relationship between Zicy and Qicy. I use the ratio of observed to expected (OE ratio) marker hospitalizations for each insurance type, county, year cell as a proxy variable Qicy with these properties.
OE ratios are commonly used in health outcomes research as a measure of hospital or health system performance for outcomes such as heart attack mortality, where adverse outcomes reflect both patient characteristics and the type of care received (Staiger et al., 2009). The ratio is the number of observed events scaled by the number that would be expected given observable patient characteristics. A marker OE ratio less than 1 would indicate a lower rate of admission than would be predicted using enrollee demographics. Clinical evidence suggests that OE ratios for marker admissions should be 1 absent selection bias.
The proxy variable Qicy is defined as , where Micy is the rate of marker hospitalizations per 1,000 enrollees in each insurance type*county*year cell. Predicted rates of marker hospitalization are calculated using least squares to estimate Equation (3). I do not control for MMC status in this equation as managed care status only provides information about marker hospitalizations through the correlation with unobserved health status Zicy.
| (3) |
The marker OE ratio measures the extent to which unobserved health characteristics of each group yield more or fewer hospitalizations than expected relative to persistent differences across counties and time. Since this measure reflects dimensions of health status related to marker hospitalizations, it satisfies assumption 1, that there would be no relationship between rates of other types of admissions Hicy and the proxy Qicy in a regression that controlled for Zicy, the full measure of health status.
The second assumption implies that there would be no relationship between unobserved health status and managed care status (or any of the other control variables) after controlling for the marker OE ratio in a regression of the Zicy on Qicy and the other covariates in Equation (1). The clinical and econometric evidence presented above support this assumption. Marker hospitalizations are not influenced by medical care, and thus can’t be driven by managed care status. Furthermore, marker hospitalizations contain information about health behaviors and health states that would correlate with managed care status under positive (or adverse) selection.
The marker hospitalization correction is implemented by using least squares regression to estimate Equation (3) and then Equation (4), which includes the OE ratios from Equation (3) as the proxy variable Qicy.
| (4) |
I weight insurance-county-year cells by enrollment and adjust the robust standard errors in Equation (4) to account for the inclusion of the generated regressor Qicy using a pairs-clustered bootstrap. This approach ensures that the bootstrap resampling includes both the MMC and FFS observation for the given county-year selected. The entire system of equations is bootstrapped 1,000 times to obtain clustered standard errors.
This empirical approach is most closely related to Basu and Mobley (2007), who compare the risk of having an ACS admission relative to a marker admission for MMC and FFS enrollees. However, their approach implicitly assumes that the relationship between all types of ACS and marker hospitalizations is constant. In contrast, this paper presents a flexible approach that allows the influence of the selection term to vary across types of admissions, providing additional information about the mechanisms through which managed care plans influence quality of care. Furthermore, the OE ratios themselves can be used in further analyses, for example to understand the extent to which selection is greater in markets with high or low managed care penetration.
5 Results
Consistent with the unadjusted rates shown in Figure 1, MMC enrollees average lower rates of all types of hospital admissions studied conditional on enrollee demographics and geographic patterns of care (Table 5). Inclusion of control variables reduces the magnitude of the unadjusted difference in rates of hospitalization across MMC and FFS enrollees, though significant differences remain. MMC enrollment is associated fewer risk-adjusted ACS hospitalizations for acute (7.7 fewer per 1,000 enrollees) and chronic conditions (9.6 fewer per 1,000 enrollees) annually, and 6.3 per 1,000 fewer RS admissions annually after adjusting for differences in demographics and regional practice patterns. Increases in the proportion of the enrollee population that is Black increases rates of hospitalizations; other demographic variables are largely statistically insignificant.
Table 5.
Annual Hospitalization Rates per 1,000 Enrollees: Medicare Managed Care versus Fee-for-Service Medicare
| Marker | Ambulatory Care Sensitive | Acute ACS | Chronic ACS | Referral Sensitive | |||||
|---|---|---|---|---|---|---|---|---|---|
| MMC | −2.23* (1.10) | −17.29** (4.56) | −12.54** (4.07) | −7.74** (1.81) | −5.93** (1.60) | −9.56** (2.89) | −6.61* (2.64) | −6.28** (2.30) | −4.06† (2.11) |
| OE Ratio | 13.99† (7.72) | 5.32† (2.91) | 8.67† (4.82) | 6.54* (3.27) | |||||
| Marker Corrected | n/a | No | Yes | No | Yes | No | Yes | No | Yes |
|
| |||||||||
| MMC* County* Yr | 822 | 822 | 822 | 822 | 822 | 822 | 822 | 822 | 822 |
Cluster robust standard errors in parentheses
p < 0.10,
p < 0.05,
p < 0.01
Models control for county and year fixed effects, % Black, Hispanic, other race, female, Medicaid-eligible, ESRD, 75 – 84 and 84 and above enrollees. MMC coefficient is difference in rates of hospitalization per 1,000 MMC vs. FFS enrollees.
Marker corrected models control for the observed:expected ratio of marker hospitalizations, which proxies for unobserved health status (mean MMC OE = 0.91, mean FFS = 1.01, with values < 1 indicating better than expected health. better than 822 insurance type-county-year cells from 84 counties weighted by enrollment.
AZ, FL, NJ, NY State Inpatient Databases, Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality and Medicare data, 1999–2005.
Controls for patient demographics and time-invariant unobserved county characteristics attenuate but do not eliminate the difference in marker hospitalizations, MMC patients average 2.2 fewer marker hospitalizations per 1,000 enrollees in the risk-adjusted models. Since amount or quality of recent medical care is not a determinant of these hospitalizations, the significant MMC coefficient likely reflects bias resulting from the absence of a health status measure. Table 6 presents expected and observed rates of marker hospitalization amongst MMC and FFS enrollees. MMC enrollees are expected to have lower rates of hospitalization than FFS enrollees (5.9 vs. 10.8 per 1,000) given demographic and geographic characteristics. However, observed rates of marker admissions for MMC enrollees (5.2 per 1,000 enrollees; are 12% lower than predicted by observable characteristics.
Table 6.
Expected and Observed Rates of Marker Hospitalizations
| Marker Rate | MMC | FFS |
|---|---|---|
| Observed | 5.2** (3.0) | 10.9 (2.4) |
| Expected | 5.9** (2.1) | 10.8 (2.0) |
| OE Ratio | 0.91** (0.64) | 1.01 (0.17) |
Standard deviations in parentheses
statistically different at 1% from Fee-for-Service
HCUP SID and Medicare data, AZ, FL, NJ, NY 1999–2005
Table 5 reports the MMC effect for ACS and RS hospitalizations in regressions that do and do not control for Qicy, the marker OE ratio. Controlling for enrollee health status reduces the magnitude of the difference in rates of ACS and RS admissions. The difference in overall rates of ACS admissions between MMC and FFS declines by 26%, from −17.29 to −12.54 per 1,000. Qicy is significant in the ACS regressions at the 10% significance level. Since Qicy is a proxy for Zicy, the proxy coefficient remain biased, this is a limitation of the proxy variable approach. However, the positive direction of these coefficients indicates that rates of ambulatory care sensitive hospitalizations are higher amongst enrollees with worse health (higher marker OE ratios). Ignoring the bias for illustrative purposes, the overall ACS λ coefficient 13.99 indicates that moving from the mean MMC OE ratio (0.91) to the mean FFS ratio (1.01) would increase rates of hospitalization by 1.4 per 1,000 enrollees (13.99*(1.01–0.91)).
The reduction in the MMC effect after controlling for selection is more pronounced for chronic ACS conditions (α = −9.6 in the fixed effect regressions and −6.6 in the marker corrected; selection accounting for 31% of the risk-adjusted difference) than the acute ACS conditions (α = −7.7 in the fixed effect regressions and −5.9 in the marker corrected; 23% explained by selection). Reducing ACS admissions related to chronic conditions may require more comprehensive disease management programs or long-term investments in beneficiary health, which are themselves costly to plans. The 31% decline in the magnitude of the MMC effect after controlling for enrollee health status suggests that MMC plans may use benefit package design to attract enrollees who have few chronic conditions and will therefore experience lower rates of chronic ACS admissions regardless of quality of care provided. The acute ACS results are consistent with MMC plans focusing quality activities on conditions where short-term, inexpensive interventions can reduce hospitalization risk.
The magnitude of the RS difference is reduced by 35% (from 6.28 to 4.02 per 1,000 enrollees) with the inclusion of the health status measure, a managed care effect that is statistically significant only at 10%. The OE ratio is a significant determinant of hospitalization rates at the 5% significance level and indicates that moving from the mean MMC ratio to mean FFS would increase rates of RS admissions by 3.5% (0.65 admissions per 1,000). MMC plan network and benefit package design may play an important role in attracting managed care enrollees who anticipate undergoing elective surgery. Plans may choose to contract with relatively few specialty surgeons or offer high cost-sharing for rehabilitative care to deter patients anticipating costly surgical procedures from enrolling. MMC review mechanisms may reduce unnecessary procedure use, with the higher rates in FFS reflecting overutilization, though this explanation is less consistent with the observed selection effect.
To better understand the mechanisms through which managed care plans reduce rates of hospitalization, I reestimate Equation (4) separately for each type of ACS and RS admission. Reductions in acute ACS hospitalizations for MMC enrollees are driven by dehydration, pneumonia, and urinary tract infection (UTI) (Table 7). Pneumonia and UTI are conditions where short-term, inexpensive investments in vaccination or antibiotics can prevent hospitalization. Hospitalizations for dehydration can be prevented by managing underlying health conditions. Relative to FFS, managed care plans are likely to provide greater access to these types of interventions in the outpatient setting. There is no difference in ACS admissions related to ruptured appendix, a type of admission that results from delayed receipt of hospital care.
Table 7.
Marker-Corrected Regressions of Ambulatory Care Sensitive Hospitalization Rates on Medicare Managed Care Status
| Acute | Dehydration | Pneumonia | Ruptured Appendix | Urinary Tract Infection | ||
|---|---|---|---|---|---|---|
| MMC | −0.94** (0.32) | −3.30** (1.10) | −0.01 (0.03) | −1.68** (0.42) | ||
| OE Ratio | 1.06† (0.58) | 3.09† (1.73) | 0.07† (0.04) | 1.18† (0.61) | ||
|
| ||||||
| Chronic | Asthma | COPD | CHF | Diabetes L-T | Diabetes Uncontrol | Hypertension |
|
| ||||||
| MMC | −0.75** (0.23) | −1. 48 (0.89) | −2.79† (1.30) | −0.83** (0.26) | −0.13* (0.07) | −0.53** (0.14) |
| OE Ratio | 0.26† (0.16) | 2.08† (1.22) | 4.67† (2.54) | 0.63† (0.40) | 0.05 (0.06) | 0.27† (0.15) |
Notes and full models follow Table 5
Insignificant results for angina, short-term diabetes and amputation not reported
Improved access to prescription drugs may also account for the reductions in hospitalizations for chronic ACS admissions (Table 7), where MMC gains are observed in asthma, long-term diabetes complications and hypertension. There were no differences in rates of hospitalization between MMC and FFS for many chronic ACS admissions after controlling for selection into MMC. The managed care coefficient is insignificant for COPD (α = −1.48, s.e. = 0.89), the second-largest cause of chronic ACS admissions, and significant only at 10% for congestive heart failure (α = −2.79, s.e. = 1.30), the largest driver of chronic ACS admissions.
Positive selection into MMC accounts for differences in rates of elective angioplasty and coronary artery bypass graft (CABG) surgery across MMC and FFS enrollees (Table 8). However, differences in managed care quality or practice patterns, explain lower rates of joint replacement and pacemaker insertion. Lower rates of procedure use among MMC enrollees may reflect barriers to access within plans or managed care plans’ effective reduction of unnecessary service use.
Table 8.
Marker-Corrected Regressions of Referral-Sensitive Hospitalization Rates on Medicare Managed Care Status
| Angioplasty | CABG | Joint Replacement | Pacemaker Insertion | |
|---|---|---|---|---|
| MMC | −1.34 (0.92) | 0.63 (0.41) | −2.49** (0.96) | −0.87** (0.30) |
| OE Ratio | 2.44* (1.19) | 1.37* (0.65) | 2.17† (1.21) | 0.56† (0.30) |
Notes and full models follow Table 5
Results were robust to alternative functional forms for the OE ratio. The magnitude and significance of the MMC coefficient was unchanged in regressions including the OE ratio and its square, and the quadratic term was statistically insignificant. I report the linear specification to limit the number of generated regressors. In other applications of this methodology, users might find that alternative functional forms better match their data. Although I consider different types of hospitalizations, my results are consistent in magnitude with recent national estimates from Landon et al. (2012) suggesting that service utilization is 20 – 30% lower in MMC than FFS.
6 Discussion
As managed care plans deliver benefits to a growing share of Medicare beneficiaries, it is important to monitor the quality of care plans deliver. This task is complicated by non-random selection into Medicare managed care plans. MMC enrollees are believed to be unobservably healthier than those who remain in Fee-for-Service Medicare, so simple comparisons of utilization rates may overstate effects of managed care. I use a proxy variable methodology to capture unobserved health status using the observed-to-expected ratio of marker hospitalizations for enrollee populations defined at the county*insurance type level. I find that both positive selection and managed care plan effects contribute to lower rates of hospitalization for MMC enrollees in four states observed from 1999 –2005. Selection effects account for 26% of the difference in risk-adjusted rates of ambulatory care sensitive admissions and 35% for referral-sensitive admissions among MMC and FFS patients. Beyond selection, MMC plans reduce rates of ACS admission by an additional 5.9 per 1,000 beneficiaries (12% of the unadjusted mean) and RS admission by 4.02 per 1,000 (21.6% of the mean rate).
The relative reduction in hospitalizations for Medicare managed care enrollees is driven primarily by admissions where inexpensive, short-term interventions and routine provision of maintenance medications can reduce risk of hospitalization. During the study period, MMC enrollees’ ability to disenroll at any time limits plans’ capacity to realize savings from long-term investments in health. The current 1-year lock-in period likely helps to make these investments more attractive to plans (Newhouse et al., 2012). Focusing on the provision of short-term and maintenance interventions may help MMCs reduce the cost of care significantly by reducing preventable hospitalizations. For example, urinary tract infections detected early on can be treated with a course of antibiotics priced between $35 and $70, compared to the $17,741 in hospital charges averaged by UTI admissions in the sample. Policy changes in FFS to encourage access to these types of treatments, including Part D benefits, which were largely unavailable during the study period, may help to narrow differences in rates of potentially preventable hospital admissions across the two groups. Greater efforts to improve access to low-cost treatment in FFS Medicare could further address this gap.
This paper demonstrates a new way of controlling for non-random selection into health insurance. The OE ratio proxy method is especially appropriate for settings where large amounts of administrative data are available to construct reliable rates of hospitalization. Thus, this technique would make it difficult to assess managed care performance in counties with low levels of enrollment, or individual plan performance within a small geographic market- for example comparing the performance of several MMC plans within a given county. With more extensive data, this approach could be extended to generate average measures of managed care firm-specific qualify. This strategy could be extended nationally by requiring MMC plans to report marker hospitalization information along with the other admissions types currently collected by the annual Medicare Advantage HEDIS (Healthcare Effectiveness and Data Information Set) reporting.
Additional research may be needed to identify appropriate marker hospitalizations that occur with sufficient frequency in younger populations to use a similar strategy to study other types of insurance expansions or delivery system changes that the Affordable Care Act will bring. Using both administrative and survey data, I demonstrate that the marker hospitalizations used are correlated with measures of disease and health behaviors. If this were not the case, this methodology would not correct for the multiple dimensions across which positive selection may occur. Admission types used for younger populations should share the characteristics of not being influenced by recent health care utilization, but correlated with health and health behaviors.
This study is limited by data availability. MMC hospitalizations are only identifiable in four states, none of which report the highest levels of enrollee satisfaction with MMC in national surveys (Landon et al., 2004). None of the states are in the Pacific Northwest, where Kaiser Permanente, an integrated delivery system, dominates MMC enrollment. Although quality across plans and across states is likely to be heterogeneous, available data only facilitates analysis of the average MMC treatment effect. Results suggest that, on average, beneficiaries will have better preventative care in MMC, but potentially reduced access to some elective procedures. Findings may not generalize to the specific plan or county-level choices faced by individual beneficiaries.
Reliance on administrative inpatient data limits my focus to a few dimensions of quality and limits the potential for subgroup analyses due to discrepancies between the HCUP and Medicare claims data. Although information about the quality of care provided to vulnerable populations is critical for informing patient choice and policy evaluation, making these comparisons with currently available data would contain significant measurement error, and even if correctly measured, rates of hospitalizations for subpopulations are unlikely to be reliably measured in many counties. Some beneficiary characteristics in the Medicare data are measured with error, particularly Hispanic ethnicity and dual Medicare-Medicaid eligibility status, denominator information from Medicare would not necessarily correspond to numerators calculated from SID observations (Res-DAC, 2009).
This precludes sensitivity analyzes excluding dual eligibles, who are more likely to be enrolled in FFS (12% of the FFS sample) but have additional Medicaid benefits including prescription drug coverage and limited cost-sharing. To the extent that these additional benefits make FFS more like MMC for dual eligibles, they bias the MMC effect towards 0. At the same time, dual eligibles in MMC (6% of the MMC sample) have even more generous coverage than standard MMC benefits, which could accentuate the MMC effect. Improvements in more recent Medicare data products and HMO information-only encounter reporting can help to mitigate these analytic challenges. Researchers linking HCUP data to population based datasets may face similar limitations.
In summary, I find that positive selection into Medicare managed care explains between 23 and 35 percent of the difference in rates of potentially preventable and elective hospitalizations among MMC and Fee-for-Service beneficiaries. Plans also independently reduce rates of both potentially preventable and elective hospitalizations. These quality effects come at a cost, however, payments to managed care plans exceed average FFS spending during the study period and through the present. Policymakers should assess whether these payments and other efforts to bolster the MMC program should be sustained.
Table 3.
Correlation Between Hip Fracture in Current Year and Chronic Conditions among Fee-for-Service Medicare Beneficiaries
| Alzheimers/Dementia | 0.09 |
| Arthritis | 0.05 |
| Cataracts | 0.03 |
| Chronic Obstructive Pulmonary Disease | 0.05 |
| Congestive Heart Failure | 0.06 |
| Diabetes | 0.01 |
| Ever Heart Attack | 0.02 |
| Osteoporosis | 0.07 |
| Stroke | 0.05 |
|
| |
| N | 3,713,286 |
All correlations statistically significant at p < 0.01.
Source: 10% sample of Fee-for-Service enrollees, Medicare BASF 2004.
Acknowledgments
I am grateful to the Agency for Healthcare Research and Policy (Grant R36HS016836), the John A. Hartford Foundation, and the National Institute on Aging (grant K01AG041763). Findings do not represent official views of the funders.
Footnotes
Considerable research has been done to validate these hospitalizations as quality indicators (UCSF-Stanford, 2001; Billings, 2003). These indicators have been widely used to assess quality of care in FFS Medicare and for the under-65 population.
Prior to the introduction of the drug benefit, there was little FFS coverage for outpatient prescription drugs. Following the recent introduction of the Medicare prescription drug benefit, beneficiaries enrolled in MMC plans have had access to drug benefits with lower monthly premiums and less cost sharing on average than the stand-alone drug benefits available to those in FFS Medicare (Carino, 2006). Plans can also rebate all or part of enrollees’ Part B premiums.
New and more comprehensive measures of risk adjustment are currently used. There is lack of consensus as to whether favorable selection into MMC has increased (Brown et al., 2011) or decreased (McWilliams et al., 2012) in response to the new policies.
Separate indicators for MMC enrollees were not reported in New Jersey prior to 2003.
MMC patients are flagged using the state-specific flag for MMC; Medicare Risk in Arizona, Medicare HMO or PPO in Florida, and Medicare HMO in New Jersey and New York.
HCUP data are de-identified, so hospitalizations cannot be matched to specific enrollees in the BASF file.
Since chronic conditions are identified in the BASF data using a claims-based algorithm, these indicators cannot be reliably calculated for MMC enrollees. Hip fractures are the only marker condition included in the BASF, precluding a more comprehensive analysis. In this analysis, I treat all beneficiaries who have ever met the claims criteria for diagnosis (including current and previous year), as having a comorbid condition. Hip fractures occur during the study year only.
References
- 1.Aizer Anna. Low Take-Up in Medicaid: Does Outreach Matter and for Whom? American Economic Review. 2003;93(2):238–241. [Google Scholar]
- 2.Backus L, Moron M, Bachetti P, Baker LC, Bindman AB. Effect of managed care on preventable hospitalization rates in California. Medical Care. 2002;40(4):315–324. doi: 10.1097/00005650-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Balsa AI, Cao Z. Does managed health care reduce health care disparities between minorities and Whites? Journal of Health Economics. 2007;26(1):101–121. doi: 10.1016/j.jhealeco.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Basu J, Mobley LR. Do HMOs Reduce Preventable Hospitalizations for Medicare Beneficiaries? Medical Care Research and Review. 2007;64(5):544–567. doi: 10.1177/1077558707301955. [DOI] [PubMed] [Google Scholar]
- 5.Berenson RA. Medicare disadvantaged and the search for the elusive ’level playing field’. Health Affairs. 2004 doi: 10.1377/hlthaff.w4.572. Web Exclusive W4–572 – W4–585. [DOI] [PubMed] [Google Scholar]
- 6.Billings J, Zeitel L, Lukomnik J. Impact of socioeconomic status on hospital use in New York City. Health Affairs. 1993;12(1):162–73. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 7.Billings J, Anderson G, Newman L. Recent findings on preventable hospitalizations. Health Affairs. 1996;15(3):239–49. doi: 10.1377/hlthaff.15.3.239. [DOI] [PubMed] [Google Scholar]
- 8.Billings J. Tools for Monitoring the Health Care Safety Net. Rockville, MD: Agency for Health care Research and Quality; 2003. Using administrative data to monitor access, identify disparities, and assess performance of the safety net. [Google Scholar]
- 9.Bogardus ST. What do we know about diverticular disease? A brief overview. Journal of Clinical Gastroenterology. 2006;40(S3):S108S111. doi: 10.1097/01.mcg.0000212603.28595.5c. [DOI] [PubMed] [Google Scholar]
- 10.Braveman P, V, Schaaf M, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. The New England Journal of Medicine. 1994;331(7):444–449. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- 11.Brown J, Duggan M, Kuziemko I, Woolston W. Evidence from the Medicare Advantage program. Cambridge (MA): National Bureau of Economic Research; 2011. How does risk selection respond to risk adjustment? NBER Working Paper No. 16977. [DOI] [PubMed] [Google Scholar]
- 12.Card, Dobkin DC, Maestas N. Does Medicare Save Lives? The Quarterly Journal of Economics. 2009;124:597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carino T. The potential impact of the new prescription drug benefit on Medicare beneficiaries. Presentation at the AcademyHealth Annual Research Meeting; 27 June 2006.2006. [Google Scholar]
- 14.Cutler DM, McClellan M, Newhouse JP. How does managed care do it? RAND Journal of Economics. 2000;31(3):526–548. [PubMed] [Google Scholar]
- 15.Dartmouth Atlas Project. The care of patients with severe chronic illness: An online report on the Medicare program. 2006 [PubMed] [Google Scholar]
- 16.Dowd B, Maciejewski ML, O’Connor H, Riley G, Geng Y. Health plan enrollment and mortality in the Medicare program. Health Economics. 2011;20(6):645–659. doi: 10.1002/hec.1623. [DOI] [PubMed] [Google Scholar]
- 17.Experton B, Ozminkowski R, Pearlman DN, Li Z, Thompson S. How does managed care manage the frail elderly? The case of hospital readmissions in fee-for-service versus HMO systems. American Journal of Preventive Medicine. 1999;16(3):163–172. doi: 10.1016/s0749-3797(98)00098-1. [DOI] [PubMed] [Google Scholar]
- 18.Finkelstein J. Calcium plus Vitamin D for Postmenopausal Women - Bone Appetit? The New England Journal of Medicine. 2006;354:750–752. doi: 10.1056/NEJMe068007. [DOI] [PubMed] [Google Scholar]
- 19.Glied S. Handbook of Health Economics. Amsterdam: Elesvier; 2000. Managed care. [Google Scholar]
- 20.Gronholz M. Prevention, Diagnosis, and Management of Osteoporosis-Related Fracture: A Multifactoral Osteopathic Approach. The Journal of the American Osteopathic Association. 2008;108:575–585. [PubMed] [Google Scholar]
- 21.Guadagnoli E, Landrum MB, Peterson EA, Gahart MT, Ryan TJ, McNeil BJ. Appropriateness of coronary angiography after myocardial infarction among Medi-care beneficiaries - managed care versus fee for service. New England Journal of Medicine. 2000;343(30):1460–1466. doi: 10.1056/NEJM200011163432006. [DOI] [PubMed] [Google Scholar]
- 22.Huesch MD. Managing Care? Medicare Managed Care and Patient Use of Car-diologists. Health Services Research. 2010;45(2):329–354. doi: 10.1111/j.1475-6773.2009.01070.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackson R, LaCroiz A, Gass M, Wallace R, Robbins J, Lewis C, Bassford T, Beresford S, Black H, Blanchette P, Bonds D, Brunner R, Brzyski R, Caan B, Cauley J, Chle-bowski R, Cummings S, Granek I, Hays J, Heiss G, Hendrix S, Howard B, Hsia J, Hubbell A, Johnson K, Judd H, Kotchen J, Kuller L, Langer R, Lasser N, Limacher M, Ludlam S, Manson J, Margolis K, McGowan J, Ockene J, O’Sullivan M, Phillips L, Prentice R, Sarto G, Stefanick M, Van Horn L, Wactawski-Wende J, Whitlock E, Anderson G, Assaf A, Barad D. Calcium plus Vitamin D Supplementation and the Risks of Fractures. The New England Journal of Medicine. 2006;354:669–683. doi: 10.1056/NEJMoa055218. [DOI] [PubMed] [Google Scholar]
- 24.Kaiser Family Foundation. Medicare spending and financing fact sheet – April 2005. Washington, DC: KFF; 2005. [Google Scholar]
- 25.Kaiser Family Foundation. Medicare Advantage fact sheet – November 2011. Wash-ington, DC: KFF; 2011. [Google Scholar]
- 26.Karlsson MK, Gerdhem P, Ahlborg HG. The prevention of osteoporotic bone fractures. Journal of Bone and Joint Surgery, British Volume. 2005;87-B(10):1320–1327. doi: 10.1302/0301-620X.87B10.16578. [DOI] [PubMed] [Google Scholar]
- 27.Kruzikas DT, Jiang HJ, Remus D. HCUP Fact Book No 5. Rockville, MD: Agency for Health care Research and Quality; 2000. Preventable hospitalizations: Window into primary and preventive care. [Google Scholar]
- 28.Landon BE, I, Wilson B, Cleary P. A conceptual model of the effects of health care organizations on the quality of medical care. Journal of the American Medical Association. 1998;279(17):1377–1382. doi: 10.1001/jama.279.17.1377. [DOI] [PubMed] [Google Scholar]
- 29.Landon BE, Zaslavsky AM, Bernard SL, Cioffi MJ, Cleary PD. Comparison of performance of traditional Medicare versus Medicare managed care. Journal of the American Medical Association. 2004;291(14):1744–1752. doi: 10.1001/jama.291.14.1744. [DOI] [PubMed] [Google Scholar]
- 30.Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, Newhouse JP, Ayanian JZ. Analysis Of Medicare Advantage HMOsCompared With Traditional Medicare Shows Lower Use Of Many Services During 200309. Health Affairs. 2012;31(12):2609–2617. doi: 10.1377/hlthaff.2012.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McWilliams JM, Hsu J, Newhouse JP. New Risk-Adjustment System Was Associated With Reduced Favorable Selection In Medicare Advantage. Health Affairs. 2012;31(12):2630–2640. doi: 10.1377/hlthaff.2011.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Medline Plus Encyclopedia. Intestinal Obstruction. 2007. [Google Scholar]
- 33.Mello MM, Stearns SC, Norton EC, Ricketts TC. Understanding biased selection in Medicare HMOs. Health Services Research. 2003;38(3):961–992. doi: 10.1111/1475-6773.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller RH, Luft HS. HMO plan performance update: An analysis of the literature. Health Affairs. 2002;21(4):63–86. doi: 10.1377/hlthaff.21.4.63. [DOI] [PubMed] [Google Scholar]
- 35.Miller RH, Luft HS. Does managed care lead to better or worse quality of care? Health Affairs. 1997;16(5):7–25. doi: 10.1377/hlthaff.16.5.7. [DOI] [PubMed] [Google Scholar]
- 36.Mobley LR, McCormack L, Wang J, Squire C, Kenyon A, Lynch JT, Heller A. Voluntary disenrollment from Medicare Advantage plans: Valuable signals of market performance. American Journal of Managed Care. 2007;13(12):677–684. [PubMed] [Google Scholar]
- 37.Morales LS, Rogowski J, Freedman VA, Wickstrom SL, Adams JL, Escarce JJ. Use of preventive services by men enrolled in Medicare+Choice plans. Ameri-can Journal of Public Health. 2004;94(5):796–802. doi: 10.2105/ajph.94.5.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Newhouse JP. Free for All? Lessons from the RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- 39.Newhouse JP, Price M, Huang J, McWilliams JM, Hsu J. Steps To Reduce Favorable Risk Selection In Medicare Advantage Largely Succeeded, Boding Well For Health Insurance Exchanges. Health Affairs. 2012;31(12):2618–2628. doi: 10.1377/hlthaff.2012.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nicholas LH. Modeling the Impact of Medicare Advantage Payment Cuts on Ambulatory Care Sensitive and Elective Hospitalizations. Health Services Research. 2011;46(5):1417–1435. doi: 10.1111/j.1475-6773.2011.01275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Research Data Assistance Center . Phone communication. 2009 Apr [Google Scholar]
- 42.Rizzo JA. Are HMOs bad for health maintenance? Health Economics. 2005;14(11):11171131. doi: 10.1002/hec.993. [DOI] [PubMed] [Google Scholar]
- 43.Schneider EC, Zaslavsky AM, Epstein AM. Quality of care in for-profit and not-for-profit health plans enrolling Medicare beneficiaries. Journal of the American Medical Association. 2005;118(12):1392–1400. doi: 10.1016/j.amjmed.2005.05.032. [DOI] [PubMed] [Google Scholar]
- 44.Shimada SL, Zaslavsky AM, Zaborski LB, O’Malley JA, Heller A, Cleary PD. Market and Beneficiary Characteristics Associated With Enrollment in Medicare Managed Care Plans and Fee-for-Service. Medical Care. 2009;47(5):517–523. doi: 10.1097/MLR.0b013e318195f86e. [DOI] [PubMed] [Google Scholar]
- 45.Staiger D, Baser O, Fan Z, Dimick JB. Empirically Derived Composite Measures of Surgical Performance. Medical Care. 2009;47(2):226–233. doi: 10.1097/MLR.0b013e3181847574. [DOI] [PubMed] [Google Scholar]
- 46.UCSF-Stanford Evidence-based Practice Center. Refinement of the HCUP quality indicators. Rockville, MD: Agency for Health care Research and Quality; 2001. [PubMed] [Google Scholar]
- 47.Weineck RA, Billings J, editors. AHRQ Publication No 03–0027. Rockville, MD: AHRQ; 2003. Tools for monitoring the health care safety net. [Google Scholar]
- 48.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge: The MIT Press; 2002. [Google Scholar]
- 49.Zaslavsky AM, Zaborski LB, Cleary PD. Plan, geographical, and temporal variation of consumer assessments of ambulatory health care. Health Services Research. 2004;39(5):1467–1486. doi: 10.1111/j.1475-6773.2004.00299.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhan C, Miller MR, Wong H, Meyer GS. The effects of HMO penetration on preventable hospitalizations. Health Services Research. 2004;39(2):345–361. doi: 10.1111/j.1475-6773.2004.00231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]