Abstract
♦ Introduction: Rural residence is associated with increased peritoneal dialysis (PD) utilization. The influence of travel distance on rates of home dialysis utilization has not been examined in the United States. The purpose of this study was to determine whether travel distances to the closest home and in-center hemodialysis (IHD) facilities are a barrier to home dialysis.
♦ Methods: This was a retrospective cohort study of patients aged ≥ 18 years initiating dialysis between 2005 and 2011. Unadjusted PD and home hemodialysis (HHD) rates were compared by travel distances to both the closest home dialysis and closest IHD facilities. Adjusted PD and HHD utilization rates were examined using multivariable logistic regression models.
♦ Results: There were 98,608 patients in the adjusted analyses. 55.5% of the dialysis facilities offered home dialysis. IHD, PD and HHD patients traveled median distances of 5.4, 3.5 and 6.6 miles respectively to their initial dialysis facilities. Unadjusted analyses showed an increase in PD rates and decrease in HHD rates with increased travel distances. Adjusted odds of PD and HHD were 1.6 and 1.2 respectively for a ten mile increase in distance to the closest home dialysis facility, while for distances to the closest IHD facility the odds ratios for both PD and HHD were 0.7 (all p < 0.01).
♦ Conclusions: In metropolitan areas, PD and HHD generally increased with increased travel distance to the closest home dialysis facility and decreased with greater distance to an IHD facility. Examination of travel distances to PD and HHD facilities separately may provide further insight on specific barriers to these modalities which can serve as targets for future studies examining expansion of home dialysis utilization.
Keywords: Peritoneal dialysis, home hemodialysis, travel distances, predictors of home dialysis, United States
Home dialysis modalities are generally more cost effective than conventional in-center three times per week hemodialysis (IHD) (1-3) with equivalent outcomes (4-9). Despite its cost effectiveness, home dialysis remains underutilized in the United States compared to other developed countries (10). Potential barriers to home dialysis include physician familiarity with home modalities, limited access to home modality education and predialysis care, patient insurance and sociodemographics (11-16). Travel distances and times may also influence modality selection. Proximity of a satellite IHD unit was cited by patients in the province of Ontario as a reason for not selecting peritoneal dialysis (PD) (17). There was a trend towards a decrease in PD rates in geographic areas where satellite hemodialysis units were built in the province of Ontario, Canada (18). Patients may opt to follow their nephrologist to a dialysis facility and insurance coverage may influence patient choice of dialysis facility (19). In zip codes with higher proportions of African American residents, fewer facilities provided home dialysis therapies (12).
The degree to which travel distances pose a barrier to home dialysis in the United States has not been examined. The purposes of this study were to determine the influence of distance to the closest home dialysis unit and distance to the closest IHD on PD and home hemodialysis (HHD) utilization rates in the United States.
Materials and Methods
Study Design and Patients
This was a retrospective cohort study of end-stage renal disease (ESRD) patients aged ≥ 18 years who initiated dialysis from June 2005 to July 2011 in the United States. Patients were excluded if their initial dialysis modality was not recorded or their census tract of residence was not available or did not match a census tract from the American Community Survey (ACS) data from 2005 - 2009. Patients receiving a pre-emptive renal transplant were also excluded.
Data Sources
Patient-level data including initial dialysis modality, modality at six months, demographics and comorbidities were obtained from five out of the eighteen ESRD networks in the United States. These data were derived from the 2,728 forms which are completed by all dialysis programs and is the same database from which data are supplied by the ESRD networks to the United States Renal Data System (USRDS). End-stage renal disease networks 4, 9, 10, 15 and 17 supplied data for our study per a data use agreement, and patient residential information was used to provide more specific information on travel distances for our study than would be available from the USRDS database.
Area-level data at the level of census tract were obtained from the ACS 2005 - 2009. The United States Census Bureau uses the following hierarchical classification to categorize geographical areas: nation, regions, divisions, states, counties, census tracts, block groups and census blocks in descending order of size (20). Census tracts are subdivisions of counties and generally have a population of 1,200 to 8,000 with an average population of 4,000 people (21). Census tracts were chosen as the area unit of measurement as they were found to be the most sensitive geographic units to explain socioeconomic gradients in health and yielded the most consistent results compared to either census block groups or zip codes (22). Census tract-level data were obtained from the ACS and linked to the patient data using the census tract of residence at initiation of dialysis.
Exposure Variables and Outcomes
The two exposure variables were distance measures - i) travel distance by road from each patient’s residence to the closest home dialysis facility and ii) travel distance by road from each patient’s residence address to the closest IHD facility. Actual patient and facility addresses were used for these distance calculations and were done using the ArcGIS mapping software program (ArcGIS 9 ArcView 9.3.1 and the Network Analyst Pack, ESRI, Redlands, California, USA). This program mapped the closest travel distances to the nearest home dialysis and IHD facilities by road from each patient’s home. The proportions of ESRD patients initiating dialysis with i) PD and ii) HHD were the primary outcomes of this study.
Statistical Analyses
Baseline patient and area-level characteristics were compared between patients who attended dialysis facilities with home dialysis programs and patients who attended dialysis facilities without home dialysis options. ANOVA, Kruskal-Wallis and Cochrane-Armitage trend tests were used to compare continuous normal, non-normal and ordinal categorical variables respectively. Peritoneal dialysis and HHD utilization rates at dialysis initiation were analyzed by the two exposure variables. For the descriptive and unadjusted analyses, the distances were divided into six categories instead of the standard quartile distribution to allow for examination of the effects of the extremes of distance on PD and HHD utilization. The divisions were as follows: < 10th percentile, 10th to 25th percentile, 25th percentile to median, median to 75th percentile, 75th to 90th percentile and > 90th percentile. The proportions of facilities offering home therapies as well as median distances traveled for each modality were also reported.
Primary Analyses
The unadjusted rates of PD and HHD use are reported for all patients, and for comparison, also reported amongst only patients attending dialysis facilities where home dialysis was offered. The adjusted and supplementary analyses were limited to the sample of patients who attended facilities where home dialysis was available. This was done because most of the patients receiving home dialysis went to facilities which offered it. It follows that to receive a home dialysis therapy, one must travel to a facility where it is offered. Also there were a small minority of home dialysis patients who were traveling to facilities that did not offer home dialysis, which may have represented patients in remote rural regions. Given the significant baseline differences, including these patients would have caused the travel distances to be skewed by this small number of patients.
Peritoneal dialysis and HHD initiation rates were examined in adjusted multivariable logistic regression models. Generalized estimating equations were used to account for clustering of patients at the census tract level. In the regression models, distances to the initial dialysis facility and distances to the closest home dialysis and IHD facilities were divided by ten so that the effects per a 10-mile rather than a one-mile increase in distance on PD and HD rates could be evaluated as the former may be too small to be meaningful. Patient- and area-level covariates were included in the adjusted analyses. Patient-level variables included in the multivariate models were: age, sex, race, ethnicity, employment status, insurance status, medical comorbidities (atherosclerotic heart disease, congestive heart failure, stroke, peripheral vascular disease, other cardiac disease, diabetes, hypertension, COPD, cancer, smoking, drug and alcohol dependence, presence of amputation), needing assistance with activities of daily living, difficulty with ambulation, distances to the initial and distances to the closest home facility and closest in-center dialysis facility from each patient’s residential address. Area-level variables included at the census tract level were: population above age of 18 years, racial composition, percentages of the census tract with renter-occupied units, high school degree, bachelor degree, not speaking English well, and working in professional and managerial positions as well as percentage of residents in the census tract with income below the poverty level. These factors have been shown in previous studies to influence access to and availability of various aspects of renal care (12). To estimate the urban/rural status of a census tract, we used the metropolitan, micropolitan and rural categories from the US census bureau. These categories are based on zip codes since this measure is not available at the census tract level. The mean travel time for census tract residents from home to work was included to provide a measure of rurality of census tracts in the study.
Supplementary Analyses
Multivariate logistic regression models were run using patients’ modality at six months after dialysis initiation rather than at the start of dialysis. An analysis of census tract-level characteristics associated with presence or absence of a home dialysis facility was also done. Census tracts with fewer than 11 patients were suppressed for confidentiality purposes. All analyses utilized a type I error probability of 0.05 and were conducted using SAS version 9.2 (Cary, NC, USA).
Results
Patients
There were initially 180,899 patients in the dataset. Missing dialysis modality and census tract information accounted for 92 and 3,201 patients being excluded respectively resulting in a sample size of 177,606 patients.
Descriptive Results
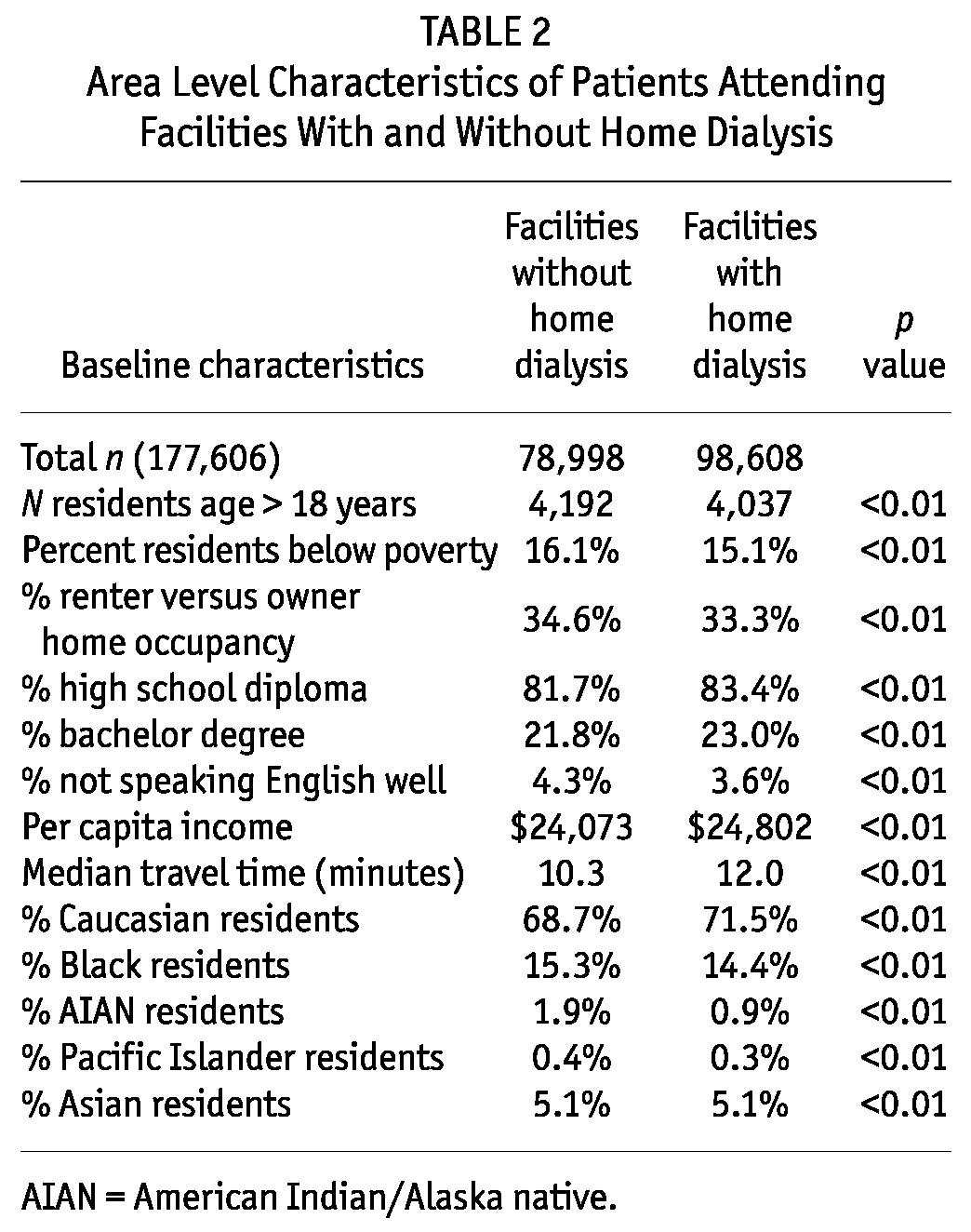
Baseline patient and census tract-level characteristics are shown for patients attending dialysis facilities with and without home dialysis programs in Tables 1 and 2 respectively. The baseline patient characteristics in our study were similar to the national incident cohort of dialysis patients from the USRDS in 2010. Incident patients nationally had a mean age of 62.8 years, 44.8% had diabetes mellitus, 65.9% were White, 27.9% were Black and 14.5% were Hispanic ethnicity (23). The median distances traveled by IHD, PD and HHD patients to their initial dialysis facilities were: 5.7, 12.6 and 17.8 miles respectively. Most patients travel farther then their closest dialysis facility regardless of dialysis modality. Median patient travel distance to their initial dialysis facility was 6.1 miles whereas the median distances that each patient lived from the nearest IHD and home dialysis facilities were 2.7 miles and 4.0 miles respectively. Only 55.5% of dialysis facilities in the study offered home dialysis therapies. By way of comparison, among the patients attending dialysis facilities with home dialysis programs (98,608 patients), the median distances traveled by IHD, PD and HHD patients were 5.4, 3.5 and 6.6 miles respectively.
TABLE 1.
Patient Baseline Characteristics in Facilities With and Without Home Dialysis
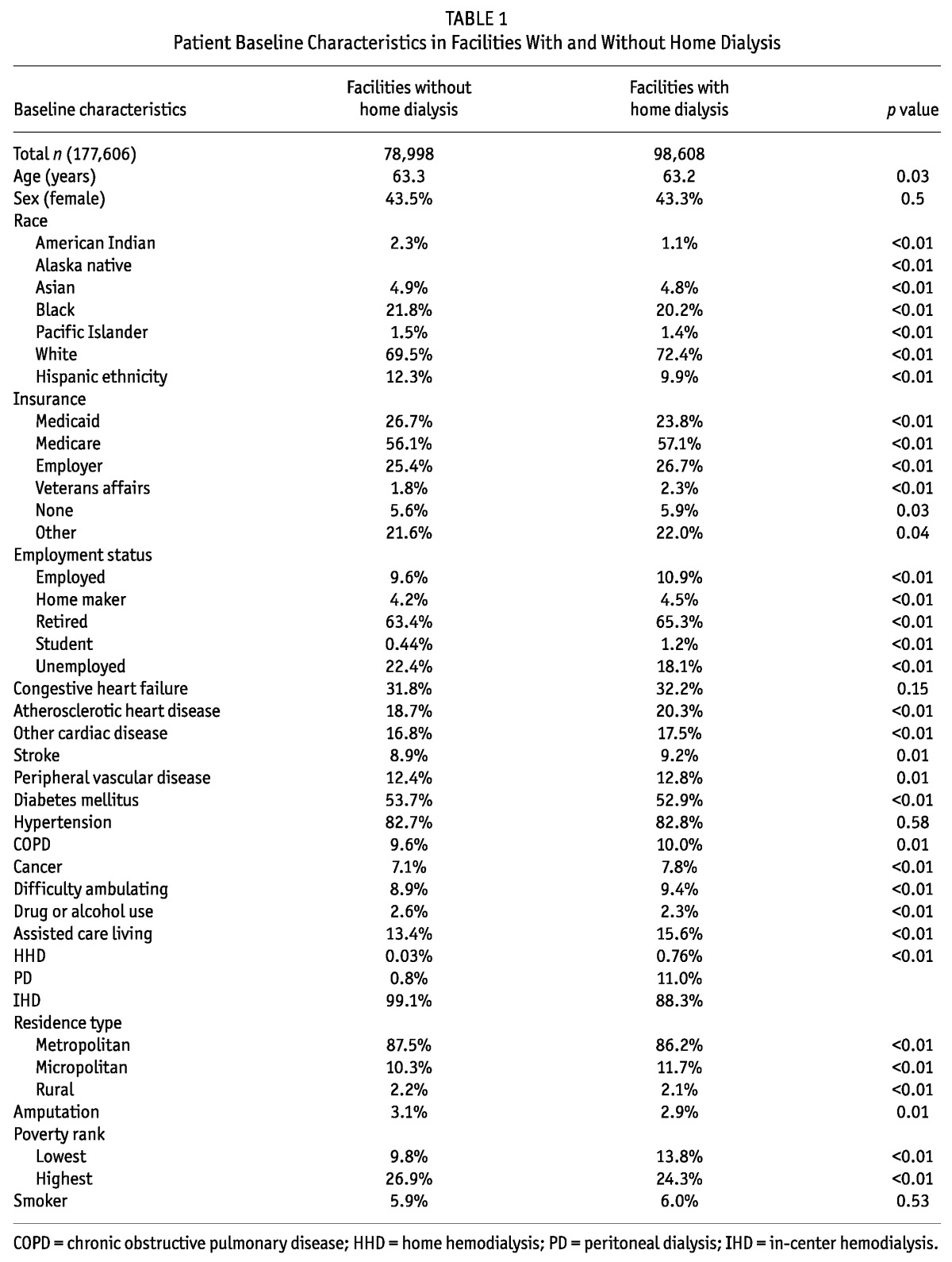
TABLE 2.
Area Level Characteristics of Patients Attending Facilities With and Without Home Dialysis
Primary Results
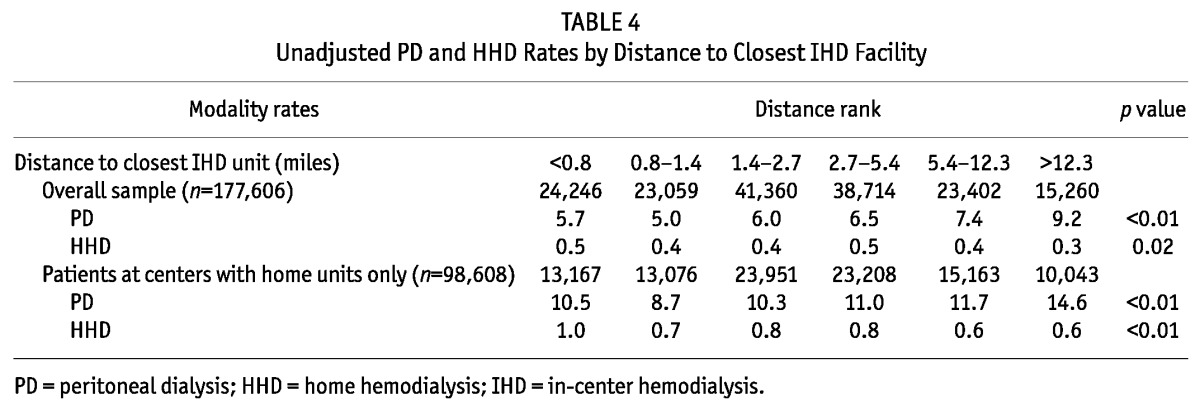
As the distance to closest home dialysis facility increased, the proportion of patients initiating PD increased from 5 - 8.4% while HHD utilization decreased from 0.6 - 0.3%. When examining these rates with only the cohort of patients who attended facilities with home dialysis options, the utilization of PD increased from 7.0 - 22.4% and there was no clinically significant change in HHD from 0.8 - 0.9% (Table 3). Peritoneal dialysis rates increased in both cohorts of patients as the distance to an IHD facility increased. As distance to an IHD facility increased, the HHD rates decreased in both cohorts of patients (Table 4).
TABLE 3.
Unadjusted PD and HHD Rates by Distance to Closest Home Dialysis Facility
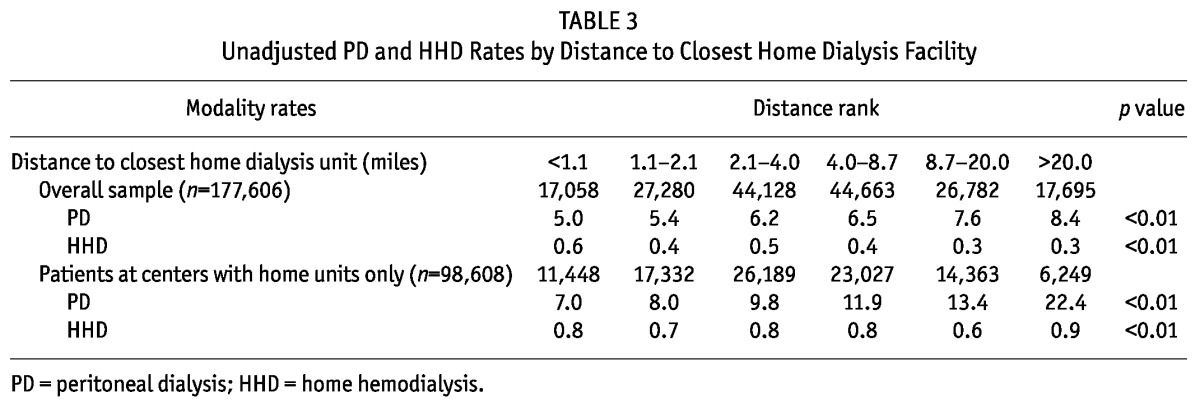
TABLE 4.
Unadjusted PD and HHD Rates by Distance to Closest IHD Facility
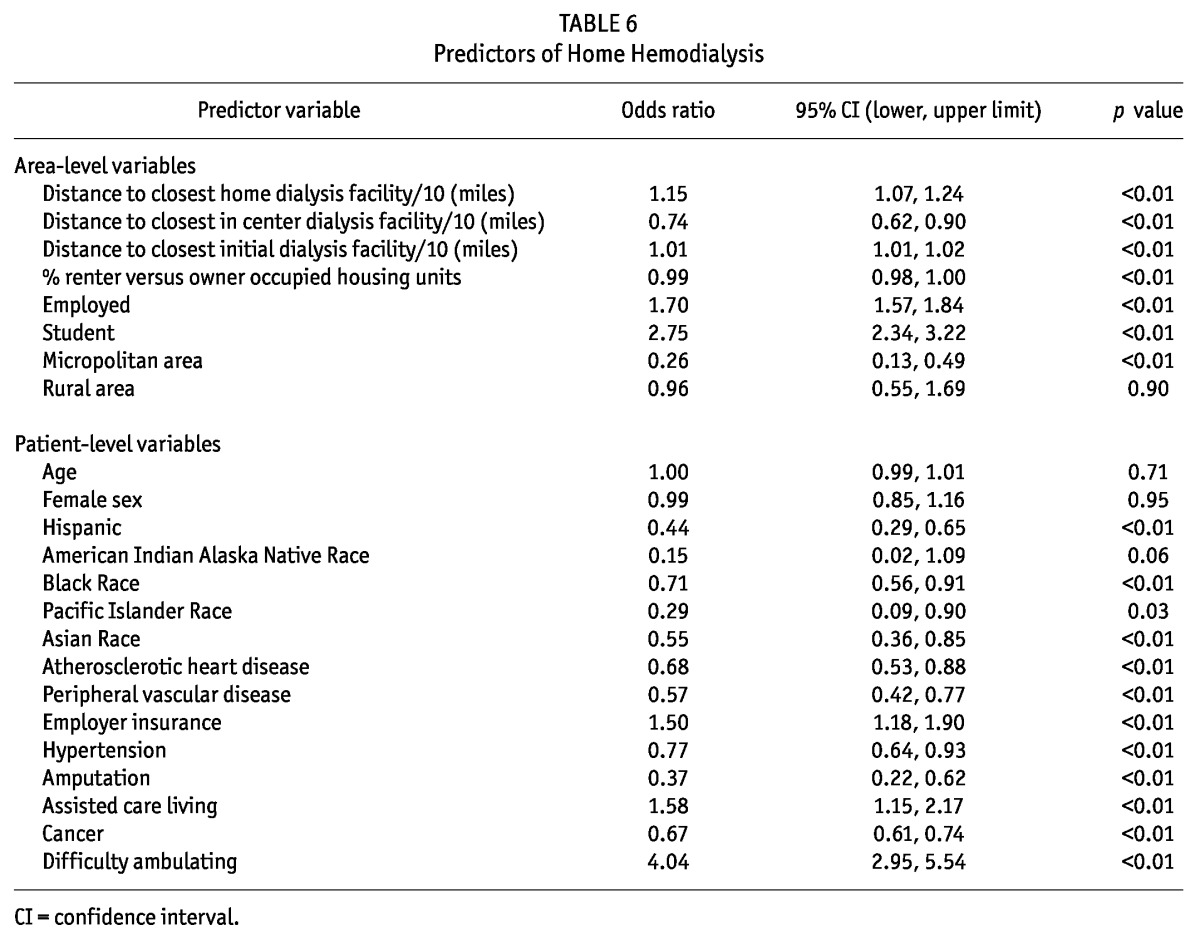
In the adjusted analyses, a 10-mile increase in distance to the closest home dialysis facility was significantly associated with increased PD utilization rates (odds ratio (OR) = 1.6, p < 0.01) while an increase in 10 miles to the closet IHD facility was associated with a significant decrease in PD utilization (OR = 0.7, p < 0.01). The interaction term between these two distances was statistically significant (OR = 0.98, p < 0.01). This may account for the fact that in the unadjusted results, increased distance to closest IHD unit is associated with higher PD rates whereas the adjusted results show a decrease in PD. This difference, however, may simply be the result of adjusting for multiple covariates as the OR of the interaction term is very close to 1.0. A 10-mile increase in distance to the closest home dialysis facility was associated with a significant increase in HHD utilization (OR = 1.14, p < 0.01) while increased distance to the closest IHD facility was associated with a decrease in HHD rates (OR = 0.7, p < 0.01). The interaction of the two distance terms was not significant in the HHD model (OR = 1.01, p = 0.19). The odds ratios, 95% confidence intervals and p values for the adjusted PD and HHD models are shown in Tables 5 and 6 respectively. Significant predictors of PD and HHD utilization are shown in Tables 5 and 6 respectively.
TABLE 5.
Predictors of Peritoneal Dialysis
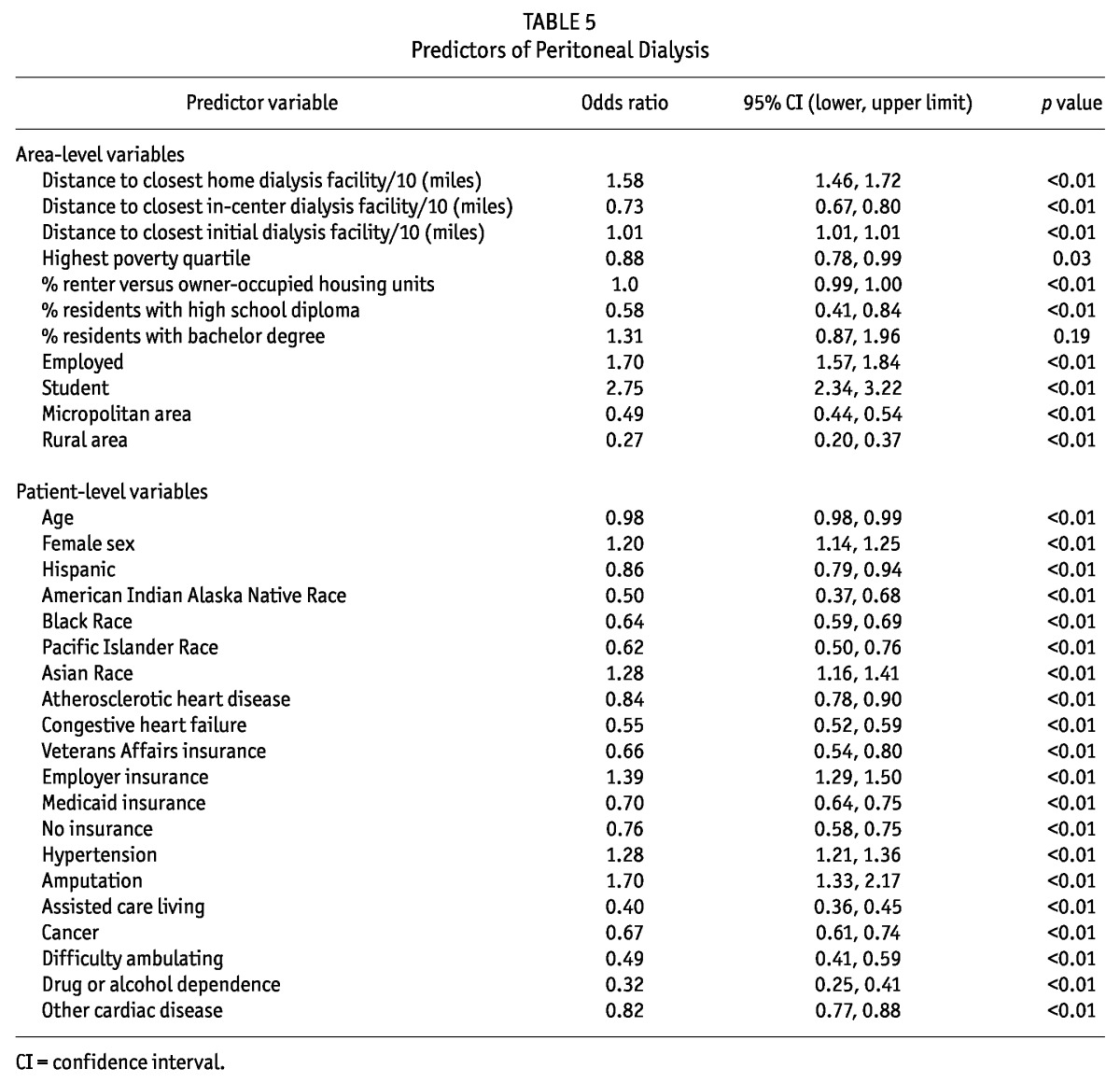
TABLE 6.
Predictors of Home Hemodialysis
Supplementary Analyses
The adjusted models were run using patient modality at six months rather than the initial modality and the results were very similar. The OR for PD rates by closest home and IHD facilities were 1.69 and 0.69 respectively and for HHD use by the closest home and IHD facilities were 1.16 and 0.78 respectively (all p < 0.01).
Area-level factors at the census tract level that were associated with significantly higher odds of having a dialysis facility that offered home therapies were: higher percentages census tract residents with high school degree or working in a professional or managerial position, having a higher percentage of residents in the census tract traveling more than 60 minutes to work and living in a micropolitan versus a metropolitan area (all p < 0.05).
Discussion
Peritoneal dialysis and HHD rates were affected in different ways by distances to the closest home dialysis and IHD facilities. In metropolitan areas, PD and HHD rates increased with increased distance to a home dialysis facility and they decreased with increased distance to an IHD facility. Approximately 85% of patients in the study reside in metropolitan areas so the results are largely shaped by this group. Micropolitan and rural residence were both associated with decreased PD and HHD. Only 55% of dialysis facilities offered home dialysis programs which meant that patients attending the remaining 45% of facilities may need to travel farther to reach a home dialysis facility. This is supported by the fact that the median travel times for the overall sample were higher for PD and HHD compared to the cohort only attending facilities with home dialysis programs. Regardless of modality, patients travel farther for dialysis than their closest facility which may be due to insurance or patient preference.
O’Hare et al. found that rural residence was associated with increased PD utilization in a large sample of incident ESRD patients in the United States, although facilities in rural areas were less likely to offer PD or HHD training than urban facilities (24). Our study found that patients in rural or micropolitan areas were less likely to be on PD. However, our study accounted for travel distance from the closest home and IHD facility, which was not available in their study. Although we did not have available training programs in our study, we were able to differentiate which facilities offered home dialysis programs and hence the travel distance to the closest home dialysis program. If a facility has a home program then that facility would train patients for home dialysis. O’Hare et al. found that HHD rates increased with increased rurality (24), while in our study we found that adjusted HHD rates were not affected by rural residence. Accounting for distances to closest IHD and home dialysis units may explain the differences in findings regarding rural residence and PD and HHD rates between the studies.
Poorer outcomes in PD patients in more rural areas may be an explanation for the lower rates of PD seen in our study in these areas. Mehrotra et al. examined transfer from PD to IHD in samples of patients treated with PD for any period between 2004 and 2009 in the United States. Remote rural residence was associated with an OR of 1.33 (95% confidence interval 1.05, 1.69) for transfer to IHD (25). A recent study by Pipkin et al. examined predictors of HHD among HHD patients in both Canada and the United States. Among the HHD patients from the United States, 53% were male, 55% were Caucasian, 44% had diabetes, and 39% had greater than a high school education (26). In comparison, our study showed that being employed or having employer insurance and being a student were positive predictors of HHD. Interestingly, patients in assisted care living or with difficulty ambulating were more likely to receive HHD. This may be because some assisted care facilities have on-site home dialysis facilities. However, in this study we were not able to determine the reason for the association. In contrast, there was a lower OR for PD with assisted care living and difficulty ambulating. Patients of Black, Asian, Pacific Islander, Alaska Native or American Indian race or Hispanic ethnicity were less likely than Caucasian patients to use HHD. Asian patients conversely were more likely to be on PD. This study highlights the need to more specifically explore some of the differences in barriers to PD and HHD in more detail.
This study had several limitations. This is an observational study so causation cannot be determined. The dataset did not have information that would allow us to separately assess which centers offered HHD versus PD. We were only able to identify whether centers offered a home modality (either PD or HHD) or not, and therefore did not have the ability to calculate the difference in distances traveled specifically for HHD versus PD. Area level income and education variables were used as a proxy for patient level data. Other influential factors on dialysis modality selection such as patient health literacy and knowledge of dialysis options were not available in our dataset. Patients’ addresses at time of dialysis initiation were utilized which meant that we were unable to account for patients moving after dialysis initiation.
In conclusion, greater travel distances to home dialysis facilities were associated with increased PD rates and, to a lesser extent, HHD rates. Increased travel distance to IHD units was associated with lower PD and HHD rates. The relationships between dialysis modality and travel distance are complex and other factors in addition to travel distance are likely important in dialysis modality selection and initiation. This study highlighted some differences in predictors of PD and HHD in a large incident ESRD cohort. Future studies examining specific travel distances to HHD and PD facilities separately and exploring barriers to accessing each of these modalities specifically may be helpful in increasing home dialysis use in the United States.
Disclosures
The results in this study have not been published in manuscript form previously. Some of the results have been published in abstract form by the ERA-EDTA as this study was presented in abstract form at the 2012 ERA meeting in poster format in Paris, France.
The analysis upon which this publication is based was performed under Contract Number ESRD Network 9, contract number HHSM-500-2010-NW009C entitled End Stage Renal Disease Networks Organization for the States of California, Arizona, New Mexico, Colorado, Utah, Pennsylvania, Delaware, Hawaii, Illinois, Kentucky, Ohio and Indiana, sponsored by the Centers for Medicare & Medicaid Services, Department of Health and Human Services. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The authors assume full responsibility for the accuracy and completeness of the ideas presented. This article is a direct result of the Health Care Quality Improvement Program initiated by the Centers for Medicare & Medicaid Services, which has encouraged identification of quality improvement projects derived from analysis of patterns of care, and therefore required no special funding on the part of this contractor.
Acknowledgments
The authors thank Dr. Steven Preston for his comments on the study, ESRD networks 4, 9, 10, 15 and 17 for providing the data, travel distance and time calculations, Rick Coffin for the travel time and distance calculations, Ann Holstein at Case Western Reserve University for her help with compiling the American Community Survey data and Dr. J. Sudano for his comments on area level measures. An abstract from this work was presented in poster format at the European Renal Association (ERA) meeting in May 2012, Paris, France. Dr. Prakash received a travel grant from the ERA to attend this meeting. Supported in part by NIH grants MD002265 and TR000439.
References
- 1. Berger A, Edelsberg J, Inglese GW, Bhattacharyya SK, Oster G. Cost comparison of peritoneal dialysis versus hemodialysis in end-stage renal disease. Am J Manag Care August 2009; 15(8):509–18 [PubMed] [Google Scholar]
- 2. Goeree R, Manalich J, Grootendorst P, Beecroft ML, Churchill DN. Cost analysis of dialysis treatments for end-stage renal disease (ESRD). Clin Invest Med December 1995; 18(6):455–64 [PubMed] [Google Scholar]
- 3. Lee H, Manns B, Taub K, Ghali WA, Dean S, Johnson D, et al. Cost analysis of ongoing care of patients with end-stage renal disease: the impact of dialysis modality and dialysis access. Am J Kidney Dis September 2002; 40(3):611–22 [DOI] [PubMed] [Google Scholar]
- 4. Collins AJ, Hao W, Xia H, Ebben JP, Everson SE, Constantini EG, et al. Mortality risks of peritoneal dialysis and hemodialysis. Am J Kidney Dis December 1999; 34(6):1065–74 [DOI] [PubMed] [Google Scholar]
- 5. Kooistra MP, Vos J, Koomans HA, Vos PF. Daily home haemodialysis in The Netherlands: effects on metabolic control, haemodynamics, and quality of life. Nephrol Dial Transplant November 1998; 13(11):2853–60 [DOI] [PubMed] [Google Scholar]
- 6. Fenton SS, Schaubel DE, Desmeules M, Morrison HI, Mao Y, Copleston P, et al. Hemodialysis versus peritoneal dialysis: a comparison of adjusted mortality rates. Am J Kidney Dis September 1997; 30(3):334–42 [DOI] [PubMed] [Google Scholar]
- 7. Mehrotra R, Kermah D, Fried L, Kalantar-Zadeh K, Khawar O, Norris K, et al. Chronic peritoneal dialysis in the United States: declining utilization despite improving outcomes. J Am Soc Nephrol October 2007; 18(10):2781–88 [DOI] [PubMed] [Google Scholar]
- 8. McFarlane PA, Bayoumi AM, Pierratos A, Redelmeier DA. The quality of life and cost utility of home nocturnal and conventional in-center hemodialysis. Kidney Int September 2003; 64(3):1004–11 [DOI] [PubMed] [Google Scholar]
- 9. Culleton BF, Walsh M, Klarenbach SW, Mortis G, Scott-Douglas N, Quinn RR, et al. Effect of frequent nocturnal hemodialysis vs conventional hemodialysis on left ventricular mass and quality of life: a randomized controlled trial. JAMA September 19 2007; 298(11):1291–9 [DOI] [PubMed] [Google Scholar]
- 10. Prakash S. An intercontinental perspective on peritoneal dialysis among indigenous patients. Perit Dial Int 2011;31(4):390–8 [DOI] [PubMed] [Google Scholar]
- 11. Prakash S, Rodriguez RA, Austin PC, Saskin R, Fernandez A, Moist LM, et al. Racial composition of residential areas associates with access to pre-ESRD nephrology care. J Am Soc Nephrol July 2010; 21(7):1192–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rodriguez RA, Sen S, Mehta K, Moody-Ayers S, Bacchetti P, O’Hare AM. Geography matters: relationships among urban residential segregation, dialysis facilities, and patient outcomes. Ann Intern Med April 3 2007; 146(7):493–501 [DOI] [PubMed] [Google Scholar]
- 13. Plypchuk G. Travel Cost Implications of dialysis in Saskatchewan. Prairie Med J 1995; 65:133–4 [Google Scholar]
- 14. Carruthers DM, Whishaw JM, Thomas M, Thatcher G. Planes, kangaroos, and the CAPD manual. Perit Dial Int 1996; 16(Suppl 1):S452–4 [PubMed] [Google Scholar]
- 15. Kneipp E, Murray R, Warr K, Fitzclarence C, Wearne M, Maguire G. Bring me home: renal dialysis in the Kimberley. Nephrology (Carlton) December 2004; 9(Suppl 4):S121–5 [DOI] [PubMed] [Google Scholar]
- 16. Villarba A, Warr K. Home haemodialysis in remote Australia. Nephrology (Carlton) December 2004; 9(Suppl 4):S134–7 [DOI] [PubMed] [Google Scholar]
- 17. Prakash S PA, Lawless ME, Austin PC, Wu F, Sehgal AR. Unpublished data. 2012. [Google Scholar]
- 18. Prakash S, Austin PC, Oliver MJ, Garg AX, Blake PG, Hux JE. Regional effects of satellite haemodialysis units on renal replacement therapy in non-urban Ontario, Canada. Nephrol Dial Transplant August 2007; 22(8):2297–303 [DOI] [PubMed] [Google Scholar]
- 19. Smith MD, Robson AM, Woodward RS, Michelman JE, Valerius TJ, Hong BA. Geographic access to health care services: the case of maintenance hemodialysis. Am J Kidney Dis January 1985; 5(1):19–26 [DOI] [PubMed] [Google Scholar]
- 20. United States Census Bureau. Standard Hierarchy of Census Geographic Entities. 2010; http://www.census.gov/geo/www/geodiagram.pdf Accessed September 4, 2012
- 21. United States Census Bureau. 2010 Census Redistricting Data (Public Law 94-171) Summary File. Geographic Terms and Concepts - Appendix A A4–A30 Available at: http://www.census.gov/geo/www/2010census/GTC_10.pdf
- 22. Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures-the public health disparities geocoding project. Am J Public Health October 2003; 93(10):1655–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. United States, Department of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, US Renal Data System (USRDS). USRDS 2011 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: USRDS; 2011. Table 1a. Patients demographics and adjusted rates by ESRD Network: Incident dialysis patients 2010 http://www.usrds.org/2012/pdf/v2_ch1_12.pdf: page 218 [Google Scholar]
- 24. O’Hare AM, Johansen KL, Rodriguez RA. Dialysis and kidney transplantation among patients living in rural areas of the United States. Kidney Int January 2006; 69(2):343–9 [DOI] [PubMed] [Google Scholar]
- 25. Mehrotra R, Story K, Guest S, Fedunyszyn M. Neighborhood location, rurality, geography, and outcomes of peritoneal dialysis patients in the United States. Perit Dial Int May-Jun 2012; 32(3):322–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pipkin M, Eggers PW, Larive B, Rocco MV, Stokes JB, Suri RS, et al. Recruitment and training for home hemodialysis: experience and lessons from the Nocturnal Dialysis Trial. Clin J Am Soc Nephrol September 2010; 5(9):1614–20 [DOI] [PMC free article] [PubMed] [Google Scholar]


