Abstract
♦ Background: Previous small studies have reported favorable results of peritoneal dialysis (PD) in the setting of chronic refractory heart failure (CRHF). We evaluated the impact of PD in a larger cohort of patients with CHRF where end-stage renal disease was excluded.
♦ Methods: All patients who received PD therapy for CRHF between January 1995 and December 2010 in two medical centers in France were included in this retrospective study. Baseline characteristics were compared with clinical parameters during the first year after initiation of PD. Mortality, safety, and sustainability of PD were also analyzed.
♦ Results: The 126 patients included had a mean age of 72 ± 11 years and an estimated glomerular filtration rate of 33.5 ± 15.1 mL/min/1.73 m2. Mean time on PD was 16 ± 16.6 months. During the first year, patients with a left ventricular ejection fraction (LVEF) of 30% or less experienced improvement in cardiac function (30% ± 10% vs 20% ± 6%, p < 0.0001). We observed a significant reduction in the number of days of hospitalization for acute decompensated heart failure after PD initiation (3.3 ± 2.6 days/patient-month vs 0.3 ± 0.5 days/patient-month, p < 0.0001). One-year mortality was 42%.
♦ Conclusions: In CRHF, PD significantly reduces the number of days of hospitalization for acute heart failure. Improved LVEF may have led to the comparatively good 1-year survival in this cohort.
Keywords: Cardiorenal syndrome, ultrafiltration, impaired renal function, cardiac failure
Heart failure (HF) affects more than 5.8 million patients in the United States, with 550 000 new cases being diagnosed each year (1). Despite significant progress in management strategies, morbidity and mortality remain high in these patients. The survival rate for patients with refractory HF, defined as resistance to conventional therapies such as diuretics and beta-blockers, is estimated to be less than 50% at 6 months (2,3).
Renal function has been shown to have a profound impact on outcomes in these patients. Elevated serum creatinine on admission to hospital for acute decompensated HF and worsening renal function during hospitalization are both associated with increased mortality. Unfortunately, renal dysfunction is extremely prevalent in patients with HF. Based on data from the Acute Decompensated Heart Failure National Registry (encompassing 105 388 patients), more than one third present with moderate-to-severe chronic kidney disease, and 9% are receiving chronic dialysis therapy (4).
The term “cardiorenal syndrome” has increasingly been used to describe the vast array of interrelated derangements in which simultaneous dysfunctions of kidney and heart are the predominant clinical picture. Although much has been written on the clinical aspects of cardiorenal syndrome, the underlying pathophysiologic mechanisms remain to be fully understood, and implications for management continue to be debated (5-7). Excretion of salt and water is impaired early in the course of the disease for a number of reasons, including low cardiac output, activation of the renin-angiotensin-aldosterone system, activation of the sympathetic nervous system, non-osmotic release of vasopressin, and impairment of the glomerular filtration rate.
Although diuretics remain the mainstay of therapy for symptomatic relief, increased urine output, and reduced total-body fluid volume, a significant subset of patients (up to 20% - 30%) present with diuretic refractoriness. More than 90% of all hospitalizations for acute decompensated HF are attributable to fluid overload (4), and most of those patients have experienced treatment failure with oral diuretics (8).
Patients with diuretic refractoriness may benefit from mechanical removal of fluid (ultrafiltration). Two modalities of renal replacement therapy can be used in these patients: hemodialysis (or isolated ultrafiltration) and peritoneal dialysis (PD). Compared with hemodialysis (which is often used in the acute setting), PD holds a number of advantages such as better preservation of residual renal function, gentle continuous ultrafiltration, and more optimal hemodynamic stability (9,10).
A number of small series on the use of continuous ambulatory PD in the setting of chronic refractory HF (CRHF) have so far been published (9-20). In most of the studies, PD was found to be associated with a significant improvement in symptoms and a decrease in the rate of rehospitalization. Although peritonitis was common in early studies, its frequency decreased with the use of newer techniques and automated devices. Notably, most of the series included very small number of patients, with some of the results being obtained from subgroup analyses.
In the present publication, we present the largest cohort of patients with CRHF for whom PD was initiated to manage volume overload and diuretic refractoriness.
Methods
Study Population
This retrospective chart review includes all patients who were treated with PD for the management of CRHF between January 1995 and December 2010 at two centers in France (Besançon and Dunkerque). The charts of all patients who started PD therapy during the study period in the two centers were initially reviewed with respect to the indication for renal replacement therapy; only patients in whom PD therapy was initiated for management of CRHF were included. During the study period, 749 patients started PD; in 127 patients (17%), the sole indication for PD initiation was CRHF (renal replacement therapy was not required for end-stage renal disease). The diagnosis of CRHF was made by at least one cardiologist, and the decision to start PD therapy was made jointly by the referring cardiologist and the nephrologist after a detailed discussion with the individual patients. These patients were either not candidates for, or did not wish to undergo, transplantation.
Baseline Evaluation
Demographics and Baseline Clinical Characteristics: Clinical parameters such as age, sex, weight, cause of HF, presence of a pacemaker or automatic implantable cardioverter-defibrillator, relevant comorbidities such as diabetes, and a history of cardiovascular events were collected at inclusion. Patients with end-stage renal disease—defined as an estimated glomerular filtration rate (eGFR) less than 15 mL/min/1.73 m2 based on the Modification of Diet in Renal Disease formula—were excluded.
Cause of HF: Heart diseases leading to HF were classified into 4 major categories: ischemic, valvular, dilated cardiomyopathy, and diastolic dysfunction. Diagnostic studies related to cardiovascular disease were obtained from medical charts and were used for classification.
Ischemic heart disease included documented cases of myocardial infarction and coronary revascularization (that is, coronary artery bypass surgery or percutaneous transluminal coronary angioplasty), or a typical history of angina associated with abnormal findings on coronary angiography. Diagnoses of valvular heart disease, dilated cardiomyopathy, and diastolic dysfunction by at least one cardiologist were based on echocardiographic criteria. The valvular heart disease category included patients with prosthetic heart valves (with or without prosthetic valve dysfunction). Various other HF-related data such as left ventricular ejection fraction (LVEF) assessed by echocardiography, medications used for the management of HF, and presence of arrhythmia were all recorded. Moreover, all hospitalizations for episodes of acute decompensated HF during the year preceding the start of PD therapy were reviewed and the length of each stay was recorded.
History of Cardiovascular Risk, Events, and Disease: History of cardiovascular events was defined as one of the following:
Cerebrovascular diseases: ischemic and hemorrhagic cerebrovascular accidents, and carotid endarterectomy
Abdominal aorta or peripheral arterial disease: abdominal aortic surgery, lower extremity amputation, intermittent claudication associated with abnormal findings on Doppler ultrasonography or angiography
Follow-Up
Data were reviewed with respect to the safety (that is, the number and severity of peritonitis episodes) and the sustainability (that is, time on treatment and possible transfer to hemodialysis) of PD therapy. Weight and doses of diuretics were recorded at inclusion and at months 3, 6, and 12 after initiation of PD therapy. Data related to re-evaluation of LVEF within the first year after initiation of PD (ranging from 1 month to 1 year) were also collected.
We recorded all hospitalizations attributable to episodes of acute decompensated HF or peritonitis. Hospital admissions during the first year after initiation of PD were carefully reviewed and the length of each stay was recorded. Data on mortality and causes of death were also recorded.
Statistical Analysis
All data for continuous variables are reported as mean ± standard deviation, unless otherwise indicated as percentages for categorical data. Differences between groups were evaluated using the Fisher exact test or the chi-square test for categorical variables. The Student t-test and Mann-Whitney U-test were used to compare quantitative variables, depending on data distribution. The Kruskal-Wallis test was used to compare quantitative variables for the three groups. Student paired t-tests were used to compare follow-up ejection fraction, body weight, diuretic dose, hospital admission rate, and length of stay. Survival proportions were generated by the Kaplan-Meier method, and between-group comparisons used the log-rank test. A p value (2-tailed) less than 0.05 was considered statistically significant. Data analysis and interpretation were performed using the Prism software application (GraphPad Software, La Jolla, CA, USA).
Results
Demographics
During the study period, 127 patients (70 in Besançon, 57 in Dunkerque) started PD for CRHF. One patient was excluded because of early diaphragmatic breach and leak after initiation of PD. Initially, 11 patients were started on isolated extracorporeal ultrafiltration therapy for acute decompensation of HF; they were then switched to PD for long-term management of their CRHF.
Of the 126 included patients, 87 were men, and 39 were women. The patients from the two centers were fairly similar. Mean age was 72 ± 11 years (range: 30 - 94 years), and mean weight was 74 ± 15.3 kg at initiation of PD therapy. The PD technique used in these patients was mainly intermittent and nocturnal. Number of days spent in hospital for acute decompensated HF in the year preceding PD therapy was, on average, 3.3 ± 2.6 days/patient-month.
Renal Function
At PD initiation, mean eGFR in the group was 33.5 ± 15 mL/min/1.73 m2. Based on eGFR, patients were divided into categories:
69 patients (55%) had an eGFR of 30 mL/min/1.73 m2 (mean: 45.5 ± 12.7 mL/min/1.73 m2);
35 patients (28%) had an eGFR of 20 - 30 mL/min/1.73 m2 (mean: 25 ± 2.8 mL/min/1.73 m2); and
22 patients (17%) had severe renal dysfunction, with an eGFR of 15 - 20 mL/min/1.73 m2 (mean: 17.2 ± 1.4 mL/min/1.73 m2).
Patients with severe renal dysfunction were significantly older (77.3 ± 9 years vs 72.7 ± 12.1 years and 72.6 ± 9.5 years (p = 0.013) for patients with an eGFR of 20 - 30 mL/min/1.73 m2 and of more than 30 mL/min/1.73 m2 respectively). Aldosterone receptor antagonists were significantly less frequently used in the subgroup of patients with severe renal dysfunction (p = 0.02).
Heart Disease
In a significant number of patients, more than one cause of HF was present: ischemic cardiomyopathy in 78 patients (62%), dilated cardiomyopathy in 66 (52%), valvular cardiomyopathy in 36 (29%), and diastolic dysfunction in 13 (10%). Atrial fibrillation was observed in 58 patients (46%). Pacemakers and automatic implanted cardioverter-defibrillators were used in 41% of the patients. The medications used for management of HF included loop diuretics (100%), angiotensin converting-enzyme inhibitors or angiotensin receptor blockers (61%), beta-blockers (28%), aldosterone receptor antagonists (25%), and digoxin (21%). In 21 patients (17%), combination therapy with angiotensin converting-enzyme inhibitor and angiotensin receptor blocker was given.
Baseline echocardiography results were available for 110 patients (87%). Mean LVEF was 38% ± 19% (range: 8 - 87%). Based on LVEF, patients were divided into categories:
36 patients (29%) had HF with preserved ejection fraction, defined as LVEF greater than 45% (mean: 60% ± 10%);
22 patients (17%) had moderate left ventricular dysfunction, defined as LVEF greater than 30% but less than or equal to 45% (mean: 40% ± 4.8%); and
52 patients (41%) had severe left ventricular dysfunction, define as LVEF less than or equal to 30% (mean: 21% ± 6.4%).
The baseline characteristics were similar in those groups.
History of Cardiovascular Events
Of the study patients, 52% had diabetes, and 71% had a history of at least 1 cardiovascular event: peripheral artery disease (17%), cerebrovascular disease (13%), and ischemic heart disease (62%).
Follow-Up
Safety and Sustainability of the Technique: The mean duration of PD therapy was 16 ± 16 months (range: 14 days - 8.4 years). Over the study period, 77 episodes of peritonitis were recorded, corresponding to a peritonitis rate of 1 episode in 26.2 patient-months. Thirteen patients (10%) were transferred to hemodialysis (8 because of refractory peritonitis and 5 because of inadequate ultrafiltration).
Weight Change and Diuretic Use: Body weight declined during the first 3 months after PD initiation (74 ± 15 kg vs 72 ± 15 kg, p = 0.04). That trend did not continue beyond 3 months, and the mean weight of the 68 surviving patients was 75.3 ± 14.9 kg at the end of the first year.
In 61 patients (48%), data on the dose of furosemide during the first year after initiation of PD therapy was adequately recorded. In that group, the daily dose of furosemide did not significantly change for the 31 patients with an eGFR greater than 30 mL/min/1.73 m2 (560 ± 343 mg vs 631 ± 360 mg, p = 0.45), but it increased for the 30 patients with an eGFR below 30 mL/min/1.73 m2 (516 ± 344 mg vs 672 ± 344 mg, p < 0.0001).
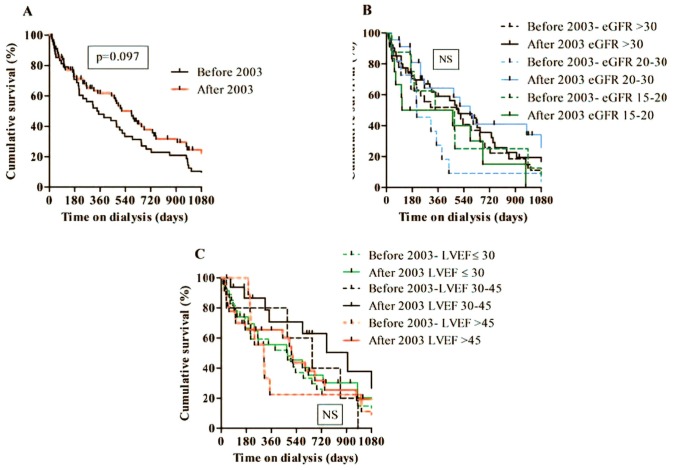
Left Ventricular Function: As shown in Figure 1, LVEF improved significantly during the first year of PD therapy (38% ± 19% at baseline vs 42% ± 17% at 1 year, p = 0.001). Interestingly, the improvement in LVEF was observed mainly in patients with a LVEF of 30% or less (20% ± 6% vs 30% ± 10%, p < 0.0001).
Figure 1 —
(A) Left ventricular ejection fraction (LEVF) improved after peritoneal dialysis (PD) therapy in the study population. (B) Patients with better cardiac function did not have a major change in ejection fraction, (C) but those with a low ejection fraction experienced significant improvement.
Number of Days of Hospitalization: Therapy using PD was associated with a dramatic reduction in the number of days of HF-related hospitalization. During the year before PD initiation, each patient stayed in hospital for an average of 3.3 ± 2.6 days per month; after initiation of PD therapy, the number of hospitalization days declined to 0.3 ± 0.5 days per month (p < 0.0001), corresponding to a 91% reduction in hospital stay. Hospital stays for peritonitis were found to be 0.3 ± 0.6 days per patient-month.
Mortality: During the study period, 100 patients (79%) died. The main causes of death were cardiovascular events [40% (acute decompensated HF 31%, sudden death 8%, cerebrovascular accident 1%)], sepsis (27%), gastrointestinal bleeding (6%), and cancer (2%). Although the cause of death remained unknown in 25 of the 100 patients, complications related to PD treatment were not implicated.
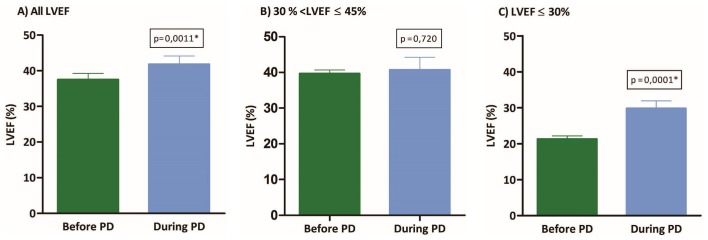
The 1-year mortality rate was 42%, and mean survival duration was 16 ± 16 months. Figure 2 summarizes cumulative survival after initiation of PD and its relationship with the defined categories of renal function and LVEF. Although no relationship was found between survival and eGFR or LVEF, we observed a trend toward lesser survival for patients with a LVEF below 30% and for those with preserved ejection fraction, especially in the first year after initiation of PD therapy (Figure 2).
Figure 2 —
Kaplan-Meier analysis of survival after initiation of peritoneal dialysis (PD) in (A) the entire study population, (B) renal function groups, and (C) cardiac function groups. Although glomerular filtration did not affect mortality, patients with a moderate reduction in left ventricular ejection fraction (LVEF) had a better survival rate. eGFR = estimated glomerular filtration rate; NS = nonsignificant.
Patients were divided into two categories based on median survival duration. Baseline characteristics and comorbidities were not different between the groups. However, among patients who survived beyond 16 months, LVEF improved during the first year after initiation of therapy (35% ± 17% vs 40% ± 15%, p = 0.039); in patients who died prematurely, LVEF remained stable (39% ± 20% vs 33% ± 14%, p = 0.07).
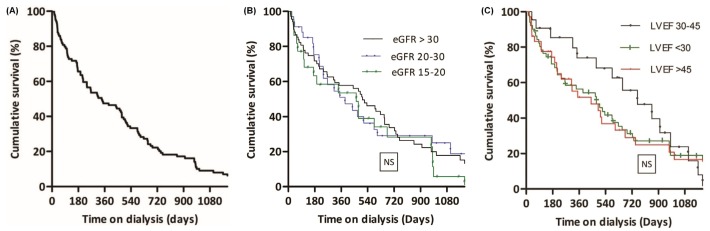
Because the study covered 16 years (1995 - 2010), we analyzed the population for two separate periods: 1995 - 2002 and 2003 - 2010 (Figure 3). We observed a trend toward better survival duration overall after 2003. During the two periods, we observed no relationship between survival and eGFR or LVEF.
Figure 3 —
Kaplan-Meier analysis of survival after initiation of peritoneal dialysis (PD) by (A) treatment period (before and after 2003), and for the same two periods by (B) estimated glomerular filtration rate (eGFR) and (C) left ventricular ejection fraction (LVEF). NS = nonsignificant.
Discussion
Although the pathophysiology of cardiorenal syndrome is not completely understood, previous reports have suggested that selected patients with CRHF can benefit from early initiation of PD. Most of those studies explored the role of PD in patients who presented with both HF and severe renal dysfunction. Moreover, all were small series with study populations of 20 patients or fewer.
To our knowledge, the present study includes the largest cohort of non-end-stage renal disease patients with CRHF in whom PD therapy was used for management of volume overload. Notably, this population represents a significant proportion of patients (17%) who were receiving PD therapy in the two study centers. Our results suggest that PD therapy can lead to a significant reduction in the number of hospitalization days and to a significant improvement in LVEF; they also imply that PD might have a beneficial effect on the financial burden of this public health problem, while improving both quality of life and cardiac function in the patients. Based on our data, PD patients should receive close supervision (for example, checking peritoneal membrane properties and excluding sodium sieving) when approaching their second year of therapy.
Patients with CRHF have a high rate of mortality (17,21). Although the lack of a matched control group in our study makes any appropriate comparison challenging, the 1-year mortality rate in the study seems to be significantly lower than that so far reported for patients with CRHF treated with conventional therapies: 50% at 6 months and 75% at 1 year (3). Given that result, PD therapy might also be associated with an improvement in the survival rate. It should be taken into consideration that, in this precarious clinical setting, PD is offered as the last resort for HF patients who have already exhausted all other therapeutic options. As such, it is difficult, from a practical standpoint, to perform an analysis of mortality using an appropriately-matched control group.
Renal dysfunction is prevalent in patients with HF, and it is an established independent prognostic factor in this population (22). Nevertheless, the degree of renal dysfunction did not affect the survival rate in our study, although we found that PD-related improvement in LEVF was associated with better survival.
It has been a matter of debate whether PD or hemodialysis represents the best dialysis modality for end-stage renal disease patients with HF. Stack et al. (23) reported that HF patients treated with PD are at higher risk of mortality compared with those receiving hemodialysis (23). It should be noted, however, that the follow-up period in that study was short (2 years) and that patients were studied between 1991 and 1997, before the advent of newer PD solutions (for example, icodextrin) and technologies. More recently, Sens et al. (24) used data from the French Renal Epidemiology and Information Network (Réseau epidémiologie et information en néphrologie) to compare survival rates in HF patients treated with PD or hemodialysis (933 and 3468 patients respectively). The authors found a significant difference in the median survival duration in favor of hemodialysis (20.4 months for PD and 36.7 months for hemodialysis; adjusted hazard ratio: 1.48). However, compared with the hemodialysis group, the PD patients were older and had more severe HF (based on New York Heart Association stage). It must be noted that the overall mortality rate of patients with HF in that study was significantly less than the rate we observed in patients with refractory HF without dialysis (about 25%), which may suggest a selection bias and emphasizes the need for more precise characterization of the population and comparison groups in such studies. Moreover, the survival rate was calculated from day 90 after initiation of renal replacement therapy for both groups and did not take into account the first 3 months. That approach might have led to an underestimation of the mortality rate in the hemodialysis group.
We observed a significant reduction in the number of days of HF-related hospitalizations after initiation of PD, which is consistent with the findings of earlier studies (9-18,25-28). That reduction can be considered an indirect marker of improved quality of life in the patients and also a surrogate marker of better control of HF symptoms and signs. As a disease, HF is costly: 2% of the total health care budget in European countries is used for expenses related to its management (25). Rates of re-hospitalization for acute decompensated HF are as high as 20% in 6 months, and costs linked to hospitalizations represent two thirds of the total cost of the disease (2). Because PD therapy is associated with a significant decrease in the number of days of hospitalization, it is conceivable that, compared with conventional therapies, PD might also reduce the expenditure related to the management of patients with HF. Indeed, in a recent study of 17 patients with CRHF, Sánchez et al. (25) reported that the cost-utility for PD is lower than that for conventional management (€305 vs €81 053 per quality-adjusted life year), a finding that needs to be confirmed in larger prospective trials.
Improvement in LVEF after initiation of PD therapy has previously been described by some authors (18,29-31). Although the exact reason for this improvement remains uncertain, correction of fluid overload with peritoneal ultrafiltration has been suggested to play a role in pushing the patient’s hemodynamic status to the left on the Frank-Starling curve. Peritoneal clearance of proinflammatory cytokines (for example, tumor necrosis factor α, interleukin 1, and interleukin 6—all described as potential myocardial depressant factors) is another mechanism by which PD might lead to improvement in LVEF (32).
In our study, PD therapy was not associated with a reduction in the needed dose of diuretics. Moreover, in contrast to previous studies (26,33,34), we did not observe a significant change in weight among our patients. Interestingly, we observed an initial trend toward weight loss that might reflect fluid removal and improvement in congestion through peritoneal ultrafiltration. Weight gain after the initial period might reflect improved clinical and nutrition status. Future studies using objective measures of volume status (for example, impedance cardiography) and specific markers of nutrition (for example, prealbumin and protein catabolic rate) are needed to further explore that hypothesis.
It is important to note that all patients included in this study were referred by cardiologists and were unknown to the nephrologists before initiation of PD. The refractory nature of the HF was therefore confirmed by the cardiologists based on challenges in optimizing conventional therapies—for example, resistance to diuretics, or hyperkalemia and excessive low blood pressure had the dose of HF-related medications been increased. In this setting, it is conceivable that PD allows for reintroduction of certain beneficial medications or the optimization of their dose (for example, aldosterone receptor antagonists) that would otherwise have been held.
The results of our study should be interpreted with due consideration of its limitations, including its retrospective design, lack of a matched control group, and long period of time during which patients were included (that is, 16 years). Also, the means by which adequate ultrafiltration was achieved (that is, use of hypertonic glucose solutions or the colloid osmotic agent icodextrin) and how those means evolved based on changes in residual renal function during the study period could not be precisely explored.
Because of its physiologically-adapted progressive fluid removal and lack of significant adverse impact on hemodynamic status, PD is considered by many nephrologists to be the modality of choice for management of patients with CRHF. Prospective studies are needed to help to further define the details of therapy in this setting (for example, optimal timing of initiation) and more customized PD protocols (for example, efficient removal of sodium through more frequent use of icodextrin solution). Such studies could also help to more precisely evaluate the impact of PD therapy on the mortality of HF patients while conducting a cost-utility analysis for this costly disease.
Conclusions
The population of patients presenting with both HF and chronic kidney disease is large and steadily growing. These patients have an increased risk of mortality; it is essential to identify the therapeutic approaches that can increase their overall survival, reduce their comorbidities, and improve their quality of life. The results of the present study—coupled with those of previously published reports—suggest that PD therapy is an appropriate and feasible option in the setting of CRHF and should be considered for patients in whom conventional therapies have not been associated with the desired therapeutic response.
Disclosures
No specific financial support was obtained for the preparation of this article. The authors have no financial conflicts of interest with regard to the manuscript.
References
- 1. Norton C, Georgiopoulou VV, Kalogeropoulos AP, Butler J. Epidemiology and cost of advanced heart failure. Prog Cardiovasc Dis 2011; 54:78–85 [DOI] [PubMed] [Google Scholar]
- 2. Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. on behalf of the ESC Committee for Practice Guidelines (CPG). ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail 2008; 10:933–89 [Erratum in: Eur J Heart Fail 2010;12:416; dosage error in article text: Eur J Heart Fail 2009; 11:110] [DOI] [PubMed] [Google Scholar]
- 3. Jessup M, Brozena S. Heart failure. N Engl J Med 2003; 348:2007–18 [DOI] [PubMed] [Google Scholar]
- 4. Adams KF Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J 2005; 149:209–16 [DOI] [PubMed] [Google Scholar]
- 5. Bongartz LG, Cramer MJ, Doevendans PA, Joles JA, Braam B. The severe cardiorenal syndrome: “Guyton revisited.” Eur Heart J 2005; 26:11–17 [DOI] [PubMed] [Google Scholar]
- 6. Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol 2008; 52:1527–39 [DOI] [PubMed] [Google Scholar]
- 7. Bock JS, Gottlieb SS. Cardiorenal syndrome: new perspectives. Circulation 2010; 121:2592–600 [DOI] [PubMed] [Google Scholar]
- 8. Ellison DH. Diuretic therapy and resistance in congestive heart failure. Cardiology 2001; 96:132–43 [DOI] [PubMed] [Google Scholar]
- 9. Ryckelynck JP, Lobbedez T, Valette B, Le Goff C, Mazouz O, Levaltier B, et al. Peritoneal ultrafiltration and refractory congestive heart failure. Adv Perit Dial 1997; 13:93–7 [PubMed] [Google Scholar]
- 10. Mehrotra R, Kathuria P. Place of peritoneal dialysis in the management of treatment-resistant congestive heart failure. Kidney Int Suppl 2006; 70:S67–71 [DOI] [PubMed] [Google Scholar]
- 11. Mousson C, Tanter Y, Chalopin JM, Rebibou JM, Dentan G, Morelon P, et al. Treatment of refractory congestive cardiac insufficiency by continuous peritoneal dialysis. Long-term course [French]. Presse Med 1988; 17:1617–20 [PubMed] [Google Scholar]
- 12. König PS, Lhotta K, Kronenberg F, Joannidis M, Herold M. CAPD: a successful treatment in patients suffering from therapy-resistant congestive heart failure. Adv Perit Dial 1991; 7:97–101 [PubMed] [Google Scholar]
- 13. Stegmayr BG, Banga R, Lundberg L, Wikdahl AM, Plum-Wirell M. PD treatment for severe congestive heart failure. Perit Dial Int 1996; 16(Suppl 1):S231–5 [PubMed] [Google Scholar]
- 14. Ortiz AM, Acosta PA, Corbalan R, Jalil JE. Long-term automated peritoneal dialysis in patients with refractory congestive heart failure. Adv Perit Dial 2003; 19:77–80 [PubMed] [Google Scholar]
- 15. Gotloib L, Fudin R, Yakubovich M, Vienken J. Peritoneal dialysis in refractory end-stage congestive heart failure: a challenge facing a no-win situation. Nephrol Dial Transplant 2005; 20(Suppl 7):vii32–6 [DOI] [PubMed] [Google Scholar]
- 16. Nakayama M, Nakano H, Nakayama M. Novel therapeutic option for refractory heart failure in elderly patients with chronic kidney disease by incremental peritoneal dialysis. J Cardiol 2010; 55:49–54 [DOI] [PubMed] [Google Scholar]
- 17. Cnossen TT, Kooman JP, Konings CJ, Uszko-Lencer NH, Leunissen KM, van der Sande FM. Peritoneal dialysis in patients with primary cardiac failure complicated by renal failure. Blood Purif 2010; 30:146–52 [DOI] [PubMed] [Google Scholar]
- 18. Sotirakopoulos NG, Kalogiannidou IM, Tersi ME, Mavromatidis KS. Peritoneal dialysis for patients suffering from severe heart failure. Clin Nephrol 2011; 76:124–9 [DOI] [PubMed] [Google Scholar]
- 19. Koch M, Haastert B, Kohnle M, Rump LC, Kelm M, Trapp R, et al. Peritoneal dialysis relieves clinical symptoms and is well tolerated in patients with refractory heart failure and chronic kidney disease. Eur J Heart Failure 2012; 14:530–9 [DOI] [PubMed] [Google Scholar]
- 20. Núñez J, González M, Miñana G, Garcia-Ramón R, Sanchis J, Bodí V, et al. Continuous ambulatory peritoneal dialysis as a therapeutic alternative in patients with advanced congestive heart failure. Eur J Heart Failure 2012; 14:540–8 [DOI] [PubMed] [Google Scholar]
- 21. Krishnan A, Oreopoulos DG. Peritoneal dialysis in congestive heart failure. Adv Perit Dial 2007; 23:82–9 [PubMed] [Google Scholar]
- 22. McAlister FA, Ezekowitz J, Tonelli M, Armstrong PW. Renal insufficiency and heart failure: prognostic and therapeutic implications from a prospective cohort study. Circulation 2004; 109:1004–9 [DOI] [PubMed] [Google Scholar]
- 23. Stack AG, Molony DA, Rahman NS, Dosekun A, Murthy B. Impact of dialysis modality on survival of new ESRD patients with congestive heart failure in the United States. Kidney Int 2003; 64:1071–9 [DOI] [PubMed] [Google Scholar]
- 24. Sens F, Schott-Pethelaz AM, Labeeuw M, Colin C, Villar E. on behalf of REIN registry. Survival advantage of hemodialysis relative to peritoneal dialysis in patients with end-stage renal disease and congestive heart failure. Kidney Int 2011; 80:970–7 [DOI] [PubMed] [Google Scholar]
- 25. Sánchez JE, Ortega T, Rodríguez C, Díaz-Molina B, Martín M, Garcia-Cueto C, et al. Efficacy of peritoneal ultrafiltration in the treatment of refractory congestive heart failure. Nephrol Dial Transplant 2010; 25:605–10 [DOI] [PubMed] [Google Scholar]
- 26. Basile C, Chimienti D, Bruno A, Cocola S, Libutti P, Teutonico A, et al. Efficacy of peritoneal dialysis with icodextrin in the long-term treatment of refractory congestive heart failure. Perit Dial Int 2009; 29:116–18 [PubMed] [Google Scholar]
- 27. Bertoli SV, Ciurlino D, Maccario M, Martino S, Bigatti G, Traversi L, et al. Home peritoneal ultrafiltration in patients with severe congestive heart failure without end-stage renal disease. Adv Perit Dial 2005; 21:123–7 [PubMed] [Google Scholar]
- 28. Elhalel-Dranitzki M, Rubinger D, Moscovici A, Haviv YS, Friedlaender MM, Silver J, et al. CAPD to improve quality of life in patients with refractory heart failure. Nephrol Dial Transplant 1998; 13:3041–2 [DOI] [PubMed] [Google Scholar]
- 29. Hébert MJ, Falardeau M, Pichette V, Houde M, Nolin L, Cardinal J, et al. Continuous ambulatory peritoneal dialysis for patients with severe left ventricular systolic dysfunction and end-stage renal disease. Am J Kidney Dis 1995; 25:761–8 [DOI] [PubMed] [Google Scholar]
- 30. Kagan A, Rapoport J. The role of peritoneal dialysis in the treatment of refractory heart failure. Nephrol Dial Transplant 2005; 20(Suppl 7):vii28–31 [DOI] [PubMed] [Google Scholar]
- 31. Takane H, Nakamoto H, Arima H, Shoda J, Moriwaki K, Ikeda N, et al. Continuous ambulatory peritoneal dialysis is effective for patients with severe congestive heart failure. Adv Perit Dial 2006; 22:141–6 [PubMed] [Google Scholar]
- 32. Zemel D, Imholz AL, de Waart DR, Dinkla C, Struijk DG, Krediet RT. Appearance of tumor necrosis factor-alpha and soluble TNF-receptors I and II in peritoneal effluent of CAPD. Kidney Int 1994; 46:1422–30 [DOI] [PubMed] [Google Scholar]
- 33. Tormey V, Conlon PJ, Farrell J, Horgan J, Walshe JJ. Long-term successful management of refractory congestive cardiac failure by intermittent ambulatory peritoneal ultrafiltration. QJM 1996; 89:681–3 [DOI] [PubMed] [Google Scholar]
- 34. Shapira J, Lang R, Jutrin I, Robson M, Ravid M. Peritoneal dialysis in refractory congestive failure part I: intermittent peritoneal dialysis (IPD). Perit Dial Int 1983; 3:130–1 [Google Scholar]