Editor:
A 66-year-old woman on peritoneal dialysis (PD) was admitted to our nephrology unit because of acute abdominal pain located near the catheter exit site (left lower quadrant). The pain had started 1 hour before admission. No fever, diarrhea, or vomiting were reported.
Clinical examination revealed increased tenderness in the left lower quadrant on palpation, blood pressure of 100/50 mmHg, and a heart rate of 110 bpm. No obvious abdominal swelling or mass was apparent. The first urgent exchange performed in the unit revealed hemoperitoneum.
This patient had been on a continuous ambulatory PD schedule for 5 years. Her primary renal disease was glomerulonephritis attributable to systemic lupus erythematosus. The patient had experienced an upper respiratory viral infection 10 days earlier, and a persistent dry cough was evident thereafter. No trauma or malfunction of the catheter was reported. Routine medication included furosemide and a beta-blocker; no anticoagulant treatment had ever been administered.
Because of increasing pain and hemodynamic instability, emergent non-contrast computed tomography imaging of the abdomen was performed, revealing a rectus sheath hematoma (Figure 1). Laboratory exams showed an important decline in hematocrit (to 24% from 34%). Platelet count, thrombin time, and partial thromboplastin time were within normal limits. Examination of the effluent showed no leukocytes.
Figure 1 —
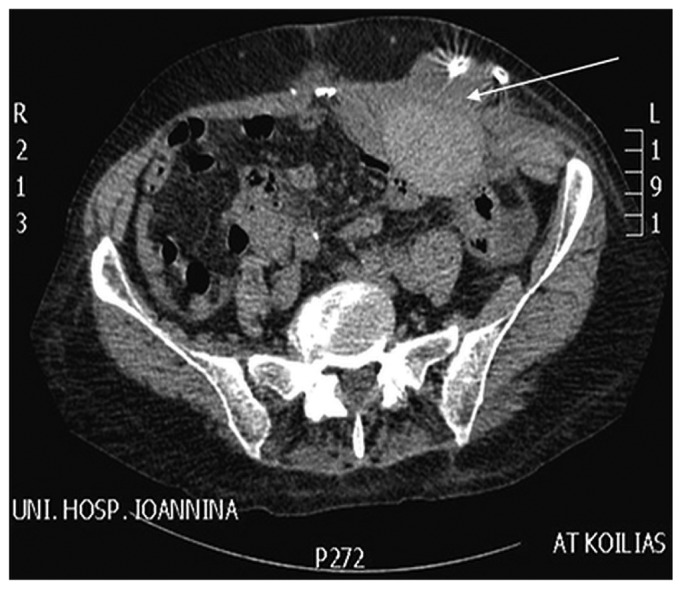
Rectus sheath hematoma (arrow) evident on computed tomography imaging.
The patient was treated conservatively: Vital signs were closely monitored, and 2 transfusions and analgesics were given. Dialysate exchanges remained bloody during the following hours. The next day, an ecchymosis on the abdomen began to be obvious. During the subsequent days, exchanges became clearer, the ecchymosis grew greater (Figure 2), and the patient’s symptoms improved. Her vital signs were stable. On day 5 of hospitalization, the patient was mobilized and discharged.
Figure 2 —
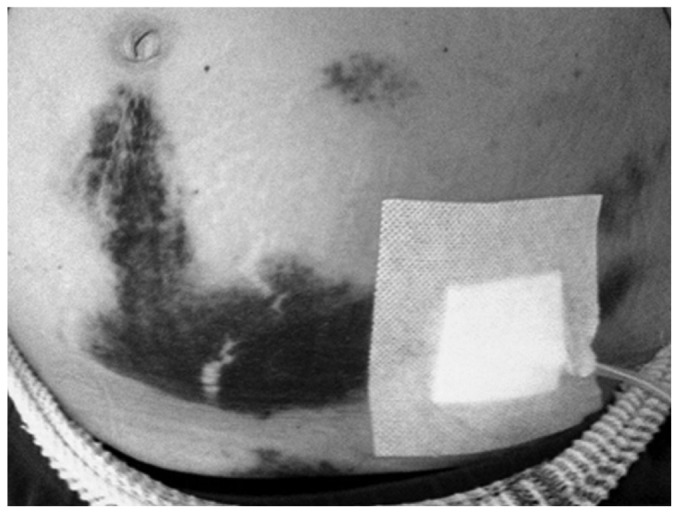
The growing ecchymosis on the patient’s abdomen.
Peritoneal dialysis provides a window to the peritoneum. Hemoperitoneum is a well-recognized complication in PD. Menstruation, catheter-related malfunctions, and intra-abdominal pathology of solid organs and the gastrointestinal tract are the most common causes (1). Rectus sheath hematoma (RSH) is an uncommon condition in the general population, usually being a complication of abdominal trauma or surgery. Spontaneous RSH is often a complication of the increasing use of anti-coagulant therapies combined with excessive strain on the abdominal muscles (2). In PD patients, RSH has only rarely been described as a complication of PD catheter insertion (3). Hemoperitoneum as first presentation of RSH in a prevalent PD patient has not yet been described in the literature.
There were questions about the cause of the hematoma in our patient. She had never received antiplatelet or anticoagulant therapy. Clinically, systemic lupus erythematosus is associated with bleeding when the platelet count is less than 20 000/μL or when antibodies against factor VIII are apparent [in which case, partial thromboplastin time is increased (4)]. In our patient, platelet count and partial thromboplastin time were within normal limits. She had taken corticosteroids for long intervals in the past, but corticosteroids are not associated with bleeding disorders. One common complication of chronic corticosteroid use is myopathy and skin thinning. Although the hematoma was close to the catheter, no trauma to the catheter was reported. That background, plus the increased abdominal strain caused by a tense cough, might explain the hematoma.
Disclosures
The authors have no financial conflicts of interest to declare.
References
- 1. Lew SQ. Hemoperitoneum: bloody peritoneal dialysate in ESRD patients receiving peritoneal dialysis. Perit Dial Int 2007; 27:226–33 [PubMed] [Google Scholar]
- 2. Salemis NS. Spontaneous rectus sheath hematoma presenting as acute surgical abdomen: an important differential in elderly coagulopathic patients. Geriatr Gerontol Int 2009; 9:200–2 [DOI] [PubMed] [Google Scholar]
- 3. Jayawardene SA, Goldsmith DJ. Rectus sheath haematomata in patients with renal disease. Nephrol Dial Transplant 2002; 17:1832–5 [DOI] [PubMed] [Google Scholar]
- 4. Lafferty TE, Smith JB, Schuster SJ, DeHoratius RJ. Treatment of acquired factor VIII inhibitor using intravenous immunoglobulin in two patients with systemic lupus erythematosus. Arthritis Rheum 1997; 40:775–8 [DOI] [PubMed] [Google Scholar]


