Abstract
A recent study reported neutralizing antibodies to West Nile virus (WNV) in horses from four ranches of southern Pantanal. To extend that study, a serosurvey for WNV and 11 Brazilian flaviviruses was conducted with 760 equines, 238 sheep and 61 caimans from 17 local cattle ranches. Among the tested equines, 32 were collected from a ranch where a neurologic disorder outbreak had been recently reported. The sera were initially screened by using a blocking ELISA and then titrated by 90% plaque-reduction neutralization test (PRNT90) for 12 flaviviruses. Employing the criterion of 4-fold greater titer, 78 (10.3%) equines were seropositive for Ilheus virus, 59 (7.8%) for Saint Louis encephalitis virus, 24 (3.2%) for WNV, two (0.3%) for Cacipacore virus and one (0.1%) for Rocio virus. No serological evidence was found linking the neurological disease that affected local equines to WNV. All caimans and sheep were negative by blocking ELISA for flaviviruses. There were no seropositive equines for Bussuquara, Iguape, Yellow fever and all four Dengue virus serotypes. The detection of WNV-seropositive equines in ten ranches and ILHV and SLEV-seropositive equines in fourteen ranches of two different sub-regions of Pantanal is strong evidence of widespread circulation of these flaviviruses in the region.
Author Summary
West Nile virus is maintained in cycles between birds and mosquitoes and recently reemerged as a worldwide major public health and veterinarian concern as the cause of human and equine encephalitis outbreaks. Recent studies have reported serological evidence of West Nile virus circulation in Pantanal, west-central region of Brazil. However, considering the co-circulation of various cross-reactive flaviviruses in Brazil and that most of the flaviviruses isolated in Brazil are unknown or understudied in the Pantanal, serological results should be interpreted with caution. Therefore, we conducted a serosurvey for West Nile virus and the 11 Brazilian flaviviruses of potential medical importance, utilizing equines, sheep and caimans as indicators, including 32 equines collected from a ranch where a neurologic disorder had been recently reported among the equines. We found serological evidence of Ilheus, Saint Louis encephalitis, West Nile, Cacipacore and Rocio viruses in Pantanal equines. West Nile virus infection was not associated with the neurological disease of equines. The detection of WNV-seropositive equines in ten ranches and ILHV- and SLEV-seropositive equines in fourteen ranches of two different sub-regions of Pantanal is strong evidence of widespread circulation of these flaviviruses in the region.
Introduction
Flaviviruses represent a group of mosquito-borne viruses in Brazil that are annually involved in a large number of human cases of dengue fever countrywide and sporadic local outbreaks of sylvatic yellow fever [1], [2]. Outbreaks caused by other flaviviruses have also been reported in the country. In the 1970s, the largest Brazilian epidemic of arbovirus encephalitis was caused by Rocio virus (ROCV) in southeast Brazil [3]. More recently, an outbreak of hemorrhagic manifestations was linked to Saint Louis encephalitis virus (SLEV) [4]. Sporadic human cases caused by other sylvatic flaviviruses, including Bussuquara virus (BSQV), Ilheus virus (ILHV) and Cacipacore virus (CPCV) have also been reported in Brazil [5], [6], [7]. Furthermore, yellow fever epizootics in howler monkeys were reported in 2008 and 2009. Approximately 200 carcasses tested positive for Yellow fever virus (YFV) and about 2000 deaths were reported [8].
Thirteen flaviviruses have been reported in Brazil, listed here in chronological order of discovery: YFV, ILHV, BSQV, SLEV, ROCV, CPCV, Dengue virus 1 (DENV-1) and Dengue virus 4 (DENV-4), Dengue virus 2 (DENV-2), Iguape virus (IGUV), Naranjal-like virus (NJLV), Dengue virus 3 (DENV-3) and Culex flavivirus (CXFV) [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20]. In 2009, serological evidence of West Nile virus (WNV) infection in Brazilian horses, was collected for the first time, in the Pantanal wetland region of Mato Grosso do Sul state (MS) [21].
The Pantanal wetland is a subtropical region of great biodiversity with strong potential for maintenance and evolution of mosquito-borne viruses. Comprising approximately 140,000 km2, the Pantanal is a vast sedimentary floodplain characterized by seasonal flooding which determines specific ecosystem processes, with the occurrence of plants and animals that are adapted to the annual shrinking and expansion of habitats due to the seasonal hydrological regime [22]. The region, which covers mainly Brazilian but also Paraguayan and Bolivian territories, is ecologically classified into 11 sub-regions according to vegetation, flooding and physiography. In Brazil, the Pantanal is located within the states of Mato Grosso (MT) and MS in the west-central region of the country [23].
Most of the flaviviruses isolated in Brazil are unknown or understudied in the Pantanal. A small number of investigations in the Nhecolândia Sub-region of the Pantanal, MS, have detected serological evidence for four flaviviruses, including ILHV, SLEV, WNV and CPCV [21], [24], [25]. Recently, three other serological studies reported the detection of neutralizing antibodies for WNV in equines from MT and again in MS, including from outside the boundaries of the Pantanal [26], [27], [28]. Complete surveys for flaviviruses in the Pantanal have not been reported. Therefore, we conducted a serosurvey for WNV and the 11 Brazilian flaviviruses of potential medical importance, utilizing equines, sheep and caimans as indicators.
Materials and Methods
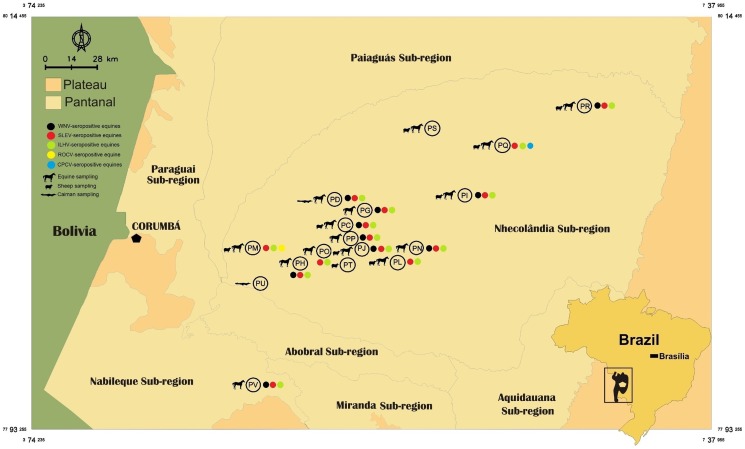
In October 2009, April, September and October 2010, blood samples were taken from 724 equines, 238 sheep and 61 caimans from 16 beef cattle ranches comprising an area of approximately 2,700 square-km in the Nhecolândia Sub-region of Pantanal, MS, west-central Brazil (Figure 1).
Figure 1. Pantanal located in west-central Brazil.
Pantanal located within the states of Mato Grosso (MT) and Mato Grosso do Sul (MS) is shown in light green. Nhecolândia and Nabileque sub-regions, where a serosurvey for flaviviruses was conducted in equines, sheep and caimans in 2009 and 2010 are shown in light and dark blue respectively.
Ethics statement
The collections for this study were approved by the Animal Ethics Committee of Fundação Oswaldo Cruz (License CEUA-Fiocruz LW-1/12, protocol P-74/10-5) in compliance with the requirements of Brazilian Law 11794/2008, which rules on the scientific use of animals, including the principles of the Brazilian society of Science in laboratory animals. The collections were also approved by the Brazilian Institute of Environment and Natural Resources (licenses IBAMA 18363-1/2009 and 18363-2/2010).
Caimans were captured in two ranches from sites where a high concentration of these animals was observed. Caiman blood samples were obtained by puncture of the internal jugular vein between the 1st and 2nd cervical vertebrae as described previously [29]. Information recorded about caimans included gender, weight and snout-vent length.
Blood samples from equines, including horses, donkeys and mules, and from sheep were taken by puncture of the jugular vein in 14 and nine different ranches, respectively. Gender, age, tameness, breed, vaccination status, travel history outside of Pantanal and history of abnormalities, such as clinical signs involving the central or peripheral nervous system, were recorded for each equine sample. Information about gender, age, breed and travel history outside of Pantanal were also recorded for each sheep. All animals sampled appeared healthy except for one horse that presented with clinical signs suggestive of neurological disorder.
Additionally, 36 horse samples collected in February 2010 from a ranch comprising roughly a 900-square-km area in the Nabileque Sub-region of Pantanal, also located in MS (Figure 1) were tested. An outbreak of an undiagnosed neurological syndrome had caused the death of 16 equines at this location from December 2009 to January 2010. All equines here were vaccinated for rabies and tested negative for Trypanosoma evansi, a common pathogen involved in incoordination and instability of hind limbs in Pantanal equines. These equines had not been vaccinated for equine encephalitis viruses at the time of the outbreak. After the first deaths, the herd was vaccinated for eastern and western equine encephalitis viruses.
All samples were initially screened for flavivirus-reactive antibodies by blocking ELISA as described previously [30]. Briefly, the ability of the sera to block the binding of the flavivirus group-reactive monoclonal antibody 6B6C-1 to the cell lysate-derived antigen for WNV was compared to the blocking ability of negative control horse serum. Samples were considered seropositive when the inhibition values produced were ≥30%. Samples with inhibition values between 19 and 29% were repeated twice to confirm the negative results. Blocking ELISA-positive samples were then heat-inactivated and tested by PRNT90, as previously described [31], for WNV and 11 Brazilian flaviviruses. Briefly, serial two-fold dilutions that ranged from 1∶10–1∶320 or 1∶20–1∶640 of each blocking ELISA seropositive sample were tested for their ability to neutralize plaque formation by WNV, SLEV, ILHV, CPCV, BSQV, IGUV, YFV (vaccine strain 17D), ROCV, DENV-1, DENV-2, DENV-3 (recombinant ChimeriVax Dengue 3 virus) and DENV-4. Caiman and sheep samples that were negative by blocking ELISA were also tested by PRNT90 for WNV.
All reference viruses used for PRNT were previously submitted to partial nucleotide sequencing of the N terminal region of NS5 gene to confirm viral identity. High identity scores were obtained with the following sequences deposited at GenBank: DENV-1 (FJ562106), DENV-2 (GQ398257), DENV-3 (recombinant ChimeriVax Dengue 3 virus) (JN811143), DENV-4 (GQ199880), ROCV (AY632542), SLEV (EF158048), ILHV (AY632539), YFV (JN628279), BSQV (AY632536), CPCV (AF013367), IGUV (AY632538), and WNV (JN819325).
Serum was considered seropositive to a virus when it reduced at least 90% of the formation of plaques of this virus and its reciprocal neutralizing antibody titer was at least four-fold greater than what was observed for the other 11 tested flaviviruses. The PRNT is the most specific serological test for the differentiation of flavivirus infections in convalescent serum samples [32]. Type-specific antibodies against flaviviruses can be distinguished using the PRNT [33]. The conservative criterion of four-fold greater titer is based on the results of cross-neutralization tests with flaviviruses and their respective antisera used for studies of antigenic relationships [34], [35]. Two or more flaviviruses are distinct from each other by quantitative serological criteria (four-fold or greater differences between homologous and heterologous titers of both serum samples) [32]. The Cochran-Armitage Trend Test was used to test for positive trends in seroprevalence among age classes (StatXact 10.0, Cytel Software Corporation, Cambridge, MA)
Results
All caiman and sheep serum samples were negative for flaviviruses-specific antibodies using the 6B6C-1 monoclonal antibody by blocking ELISA. When tested by PRNT90 for WNV, all caiman samples confirmed negative. Sixty caiman samples had PRNT90 titer <10 and one <40 for WNV (low sample volume of the latter required testing at a lowest dilution of 1∶40). From 238 sheep samples tested, 235 had PRNT90 titers <10, two showed low neutralizing antibodies titers of 20 and 10 and one <40. From 760 equine samples initially screened for flavivirus-reactive antibodies by blocking ELISA, 396 (52.1%) were positive. When this subset was tested using PRNT90, 332 (43.7%) had neutralizing reactivity (PRNT90 titer ≥10) for ILHV, 251 (33%) for SLEV, 172 (22.6%) for WNV, 139 (18.3%) for CPCV, 130 (17.1%) for ROCV, 62 (8.2%) for IGUV, 14 (1.8%) for YFV, 12 (1.6%) for BSQV, four (0.5%) for DENV-1, three (0.4%) for DENV-2, one (0.1%) for DENV-4 and none for DENV-3 (Table 1). Employing the criterion of 4-fold greater PRNT90 titer, 77 (10.1%) equines were seropositive for ILHV, 59 (7.8%) for SLEV, 24 (3.2%) for WNV (see Table 2), two (0.3%) for CPCV and one (0.1%) for ROCV. From the remaining 232 blocking ELISA positive samples, 227 (29.9%) were considered seropositive for undifferentiated flavivirus due to cross-reactivity and five (0.6%) were considered seronegative with neutralizing antibodies titers <20 or <10 for all of the flaviviruses that were assayed by PRNT90. These five may represent infections by an unknown flavivirus.
Table 1. Results of PRNT90 for WNV and Brazilian flaviviruses in equines (n = 760) of Pantanal, Brazil.
| Flaviviruses tested | Number of equines PRNT90 titer ≥10 (%) | Number of equines seropositive by PRNT90 using four-fold greater titer criterion (%) | ||
| ILHV | 332 | (43.7) | 78 | (10.1) |
| SLEV | 251 | (33) | 59 | (7.8) |
| WNV | 172 | (22.6) | 24 | (3.2) |
| CPCV | 139 | (18.3) | 2 | (0.3) |
| ROCV | 130 | (17.1) | 1 | (0.1) |
| IGUV | 62 | (8.2) | 0 | (0) |
| YFV | 14 | (1.8) | 0 | (0) |
| BSQV | 12 | (1.6) | 0 | (0) |
| DENV-1 | 4 | (0.5) | 0 | (0) |
| DENV-2 | 3 | (0.4) | 0 | (0) |
| DENV-3 | 0 | (0) | 0 | (0) |
| DENV-4 | 1 | (0.1) | 0 | (0) |
BSQV: Bussuquara virus; CPCV: Cacipacore virus; ILHV: Ilheus virus; ROCV: Rocio virus; SLEV: Saint Louis encephalitis virus; WNV: West Nile virus; IGUV: Iguape virus; YFV: Yellow fever virus; DENV: Dengue virus.
Table 2. Comparative PRNT90 titers for 12 flaviviruses among 24 WNV-seropositive equines of the Pantanal, Brazil.
| ID | Age | Ranch | Sub-region | ELISA | WNV | SLEV | ROCV | ILHV | YFV | IGUV | BSQV | CPCV | DENV-1 | DENV-2 | DENV-3 | DENV-4 |
| 316 | UNK | PH | Nhecolândia | 35.5% | 160 | <20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 327 | UNK | PH | Nhecolândia | 65.8% | 40 | <20 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 394 | UNK | PP | Nhecolândia | 56.4% | 160 | 40 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 422 | UNK | PP | Nhecolândia | 37.6% | 40 | <20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 461 | 6 years | PN | Nhecolândia | 73.3% | 80 | <20 | <10 | 20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 664 | 7 years | PR | Nhecolândia | 53.0% | 40 | <20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 687 | 5 years | PI | Nhecolândia | 48.7% | 80 | <20 | <10 | 20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 755 | 8 years | PJ | Nhecolândia | 54.5% | 160 | 20 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 786 | 4 years | PJ | Nhecolândia | 48.8% | 40 | <20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 795 | 2 years | PJ | Nhecolândia | 63.8% | 80 | 20 | 10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 807 | UNK | PJ | Nhecolândia | 54.7% | 160 | <20 | <10 | 10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 |
| 827 | 8 years | PG | Nhecolândia | 45.7% | 160 | <20 | <10 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 |
| 828 | UNK | PG | Nhecolândia | 38.7% | 160 | 40 | <10 | 20 | <10 | <10 | <10 | 40 | <10 | <10 | <10 | <10 |
| 830 | UNK | PG | Nhecolândia | 78.1% | 160 | 40 | <10 | 40 | <10 | 10 | <10 | 10 | <10 | <10 | <10 | <10 |
| 846 | UNK | PG | Nhecolândia | 45.4% | 40 | <20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 879 | 10 years | PG | Nhecolândia | 74.8% | 80 | 20 | <10 | 20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 883 | 10 years | PG | Nhecolândia | 62.1% | 160 | 40 | <10 | 10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 |
| 890 | 7 years | PG | Nhecolândia | 59.0% | 160 | 20 | <10 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 |
| 906 | UNK | PD | Nhecolândia | 47.4% | 320 | 40 | <10 | 10 | <10 | <10 | <10 | 20 | <10 | <10 | <10 | <10 |
| 917 | UNK | PD | Nhecolândia | 39.5% | 40 | <20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
| 921 | UNK | PD | Nhecolândia | 68.1% | 160 | 20 | <10 | 20 | <10 | 10 | <10 | 40 | <10 | <10 | <10 | <10 |
| 940 | 3 years | PC | Nhecolândia | 53.2% | 40 | <20 | <10 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 |
| 1080 | UNK | PV | Nabileque | 58.1% | 320 | 80 | <10 | 20 | <10 | <10 | <10 | 40 | <10 | <10 | <10 | <10 |
| 1088 | UNK | PV | Nabileque | 71.6% | 40 | <20 | <10 | 10 | <10 | 10 | <10 | <10 | <10 | 10 | <10 | <10 |
BSQV: Bussuquara virus; CPCV: Cacipacore virus; ILHV: Ilheus virus; ROCV: Rocio virus; SLEV: Saint Louis encephalitis virus; WNV: West Nile virus; IGUV: Iguape virus; YFV: Yellow fever virus; DENV: Dengue virus; UNK: Unknown.
There were no seropositive equines using the four-fold antibody titer difference criterion for BSQV, YFV, IGUV, DENV-1, DENV-2, DENV-3 and DENV-4. Monotypic neutralization reactions (i.e. a sample that reacted with only one of the 12 flaviviruses in the panel) were detected for ILHV (n = 27), SLEV (n = 11) and WNV (n = 6).
The only horse from Nhecolândia Sub-region that presented neurological signs was seropositive for undifferentiated flavivirus with the following PRNT90 titers: 80 for SLEV, 40 for ILHV, 20 for YFV, 10 for ROCV and <10 for all other flaviviruses tested.
Neutralizing antibodies for WNV were detected in 172 equines from all 15 ranches that equines were tested. Considering the four-fold higher titer criterion as confirmation, the 24 confirmed WNV-seropositive equines were detected in ten ranches comprising an area of approximately 2,500 square-km in the Nhecolândia and Nabileque sub-regions of the Pantanal, located in MS (Figure 2). Besides the 24 WNV-seropositive equines, samples from 37 other equines presented PRNT90 titers for WNV ≥40 and among them 26 showed equal or higher titers for one of the other flaviviruses tested. For these 37 equines, the serology profile could not be interpreted to determine whether WNV reactivity was due to infection with WNV or cross-reactivity from other flavivirus infections. In fact, six of them were considered seropositive for one of the 11 other flavivirus tested (Table 3). Low level of neutralizing antibodies was detected for YFV, BSQV, IGUV, DENV-1, DENV-2 and DENV-4 even though none of the equines were considered infected with these viruses. In some cases, the PRNT90 titers for YFV, BSQV and IGUV exceeded 20.
Figure 2. Pantanal ranches where equines, sheep and caimans were surveyed for flaviviruses in the Pantanal.
Colored dots mark ranches where seropositive equines with four-fold greater PRNT90 titer were detected.
Table 3. PRNT90 titers in WNV-seronegative equines that had titers ≥40 for WNV.
| ID | Ranch | Sub-region | WNV | SLEV | ROCV | ILHV | DENV-1 | YFV | IGUV | BSQV | CPCV | DENV-1 | DENV-2 | DENV-3 | DENV-4 | RESULT |
| 377 | PL | Nhecolândia | 40 | 40 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 319 | PH | Nhecolândia | 40 | <20 | <10 | 40 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | FLAV |
| 900 | PD | Nhecolândia | 40 | 40 | <10 | <10 | <10 | <10 | <10 | <10 | 20 | <10 | <10 | <10 | <10 | FLAV |
| 406 | PP | Nhecolândia | 40 | 20 | <10 | 40 | <10 | <10 | 10 | <10 | 10 | <10 | <10 | <10 | <10 | FLAV |
| 450 | PN | Nhecolândia | 40 | 20 | 10 | 10 | <10 | <10 | <10 | <10 | 40 | <10 | <10 | <10 | <10 | FLAV |
| 672 | PI | Nhecolândia | 40 | <20 | <10 | 40 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 681 | PI | Nhecolândia | 40 | 80 | <10 | 10 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | FLAV |
| 822 | PG | Nhecolândia | 40 | 160 | <10 | 320 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | FLAV |
| 824 | PG | Nhecolândia | 40 | 40 | 10 | 20 | <10 | <10 | 10 | <10 | 10 | <10 | <10 | <10 | <10 | FLAV |
| 842 | PG | Nhecolândia | 40 | 80 | <10 | 10 | <10 | <10 | <10 | <10 | 40 | <10 | <10 | <10 | <10 | FLAV |
| 691 | PJ | Nhecolândia | 40 | 80 | 40 | 40 | <10 | <10 | 10 | <10 | 80 | <10 | <10 | <10 | <10 | FLAV |
| 693 | PJ | Nhecolândia | 40 | 20 | 10 | 40 | <10 | <10 | 10 | <10 | 20 | <10 | <10 | <10 | <10 | FLAV |
| 732 | PJ | Nhecolândia | 40 | <20 | <10 | 40 | <10 | <10 | 10 | <10 | 20 | <10 | <10 | <10 | <10 | FLAV |
| 452 | PN | Nhecolândia | 40 | <20 | <10 | 160 | <10 | <10 | 10 | <10 | 10 | <10 | <10 | <10 | <10 | ILHV |
| 692 | PJ | Nhecolândia | 40 | 40 | 10 | 320 | <10 | <10 | 10 | 10 | 20 | <10 | <10 | <10 | <10 | ILHV |
| 722 | PJ | Nhecolândia | 40 | <20 | <10 | 160 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | ILHV |
| 357 | PM | Nhecolândia | 40 | 40 | 160 | 40 | <10 | <10 | 10 | <10 | 10 | <10 | <10 | <10 | <10 | ROCV |
| 775 | PJ | Nhecolândia | 40 | 640 | <10 | 10 | <10 | <10 | <10 | <10 | 80 | <10 | <10 | <10 | <10 | SLEV |
| 331 | PH | Nhecolândia | 80 | <20 | 10 | 80 | <10 | 10 | 10 | <10 | 160 | <10 | <10 | <10 | <10 | FLAV |
| 453 | PN | Nhecolândia | 80 | <20 | <10 | 80 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 843 | PG | Nhecolândia | 80 | 40 | 40 | 80 | <10 | <10 | 10 | 20 | 80 | <10 | <10 | <10 | <10 | FLAV |
| 891 | PG | Nhecolândia | 80 | <20 | <10 | 80 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 750 | PJ | Nhecolândia | 80 | 160 | <10 | 40 | <10 | <10 | <10 | <10 | 80 | <10 | <10 | <10 | <10 | FLAV |
| 803 | PJ | Nhecolândia | 80 | 80 | 40 | 40 | 10 | <10 | 10 | <10 | <10 | 10 | <10 | <10 | <10 | FLAV |
| 804 | PJ | Nhecolândia | 80 | 20 | <10 | 80 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | FLAV |
| 863 | PG | Nhecolândia | 80 | 40 | <10 | 320 | <10 | <10 | <10 | <10 | 20 | <10 | <10 | <10 | <10 | ILHV |
BSQV: Bussuquara virus; CPCV: Cacipacore virus; ILHV: Ilheus virus; ROCV: Rocio virus; SLEV: Saint Louis encephalitis virus; WNV: West Nile virus; IGUV: Iguape virus; YFV: Yellow fever virus; DENV: Dengue virus.
Both ILHV- and SLEV-seropositive equines were detected in 14 of the 15 ranches that equines were tested, comprising roughly a 3,100-square-km area. The only ranch that had no ILHV- and SLEV-seropositive equines was ranch PS (Figure 2).
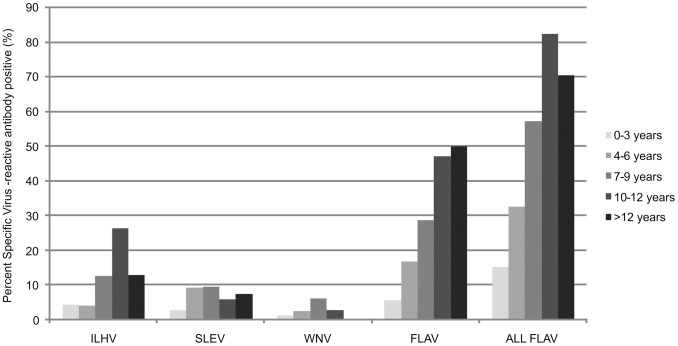
From 760 equines tested, 441 (58%) had date of birth available. Stratifying the serology results by age demonstrated that risk of exposure to flaviviruses increased with age for flaviviruses in general and for ILHV (1-tailed p<0.001 for both), but not for SLEV (p = 0.17) or WNV (p = 0.46) (Figure 3). SLEV and WNV appeared to increase in prevalence with age for equines <9 years of age, but not for older animals.
Figure 3. Positive results of PRNT90 for flaviviruses in Pantanal equines with known age in years.
ILHV: Ilheus virus; SLEV: Saint Louis encephalitis virus; WNV: West Nile virus; FLAV: undifferentiated flavivirus; All FLAV: all flavivirus infections combined; Trends of increasing seroprevalence with age were detected for ILHV and FLAV, but not SLEV and WNV (see text).
Equines seropositive for CPCV and ROCV were sampled in October 2009. The two CPCV-seropositive horses were five and seven years of age and were from ranch PQ, which comprises an area of approximately 140 square-km. The only horse that was seropositive for ROCV had no record of birth date and was from ranch PM that encompasses a 360-square-km area.
At the end of 2009, an outbreak of neurologic disease among horses was reported from ranch PV located in the Nabileque Sub-region. From 36 equines sampled, 23 (63.8%) were seropositive for flavivirus infection by blocking ELISA. When this subset was tested by PRNT90, 11 (30.5%) confirmed seropositive for SLEV, nine (25.0%) for undifferentiated flavivirus(es), two (5.5%) for WNV, and one (2.8%) for ILHV (Table 4). Of the nine undifferentiated flavivirus infections, five had SLEV titers >20 and five had higher SLEV titers than other flaviviruses in the panel, indicating that a majority of these could have had a history of SLEV infection. In addition to the relatively low seroprevalence for WNV of just 5.5% in this sample of 36 equines, four equines from this group that recovered from the recent neurologic syndrome were serologically negative for WNV (Table 4). In spite of recent vaccination against equine encephalitis viruses, most equines had low titers for equine encephalitis viruses. These results will be described separately.
Table 4. Equines of a ranch, where an epizootic of undiagnosed neurological syndrome was reported in 2009 and 2010, located in the Nabileque Sub-region of the Pantanal, Brazil.
| ID | ELISA | WNV | SLEV | ROCV | ILHV | DENV-1 | DENV-4 | YFV | IGUV | BSQV | CPCV | DENV-2 | DENV-3 | RESULT |
| 1039 | 32.3% | <20 | 20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 1046 | 46.6% | <20 | <20 | <10 | 20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 1052 | 57.7% | 40 | 80 | <10 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | <10 | <10 | FLAV |
| 1059 | 30.3% | <20 | <20 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 1060 | 77.4% | 40 | 320 | 80 | 20 | <10 | <10 | <10 | 10 | 10 | 160 | <10 | <10 | FLAV |
| 1061* | 52.2% | <20 | 40 | <10 | 20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 1068 | 58.5% | 20 | 160 | <10 | 80 | <10 | <10 | <10 | 10 | <10 | 10 | <10 | <10 | FLAV |
| 1078 | 39.8% | <20 | 40 | 10 | 80 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | FLAV |
| 1085 | 38.5% | 160 | <20 | <10 | 80 | <10 | <10 | <10 | 10 | <10 | 40 | <10 | <10 | FLAV |
| 1070 | 41.5% | 20 | <20 | <10 | 80 | <10 | <10 | <10 | 10 | <10 | 20 | <10 | <10 | ILHV |
| 1042 | 56.3% | <20 | 160 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | SLEV |
| 1054 | 60.0% | 20 | 160 | 10 | 20 | <10 | <10 | <10 | <10 | <10 | 40 | <10 | <10 | SLEV |
| 1063 | 59.9% | 20 | 160 | 20 | 20 | <10 | <10 | <10 | <10 | <10 | 40 | <10 | <10 | SLEV |
| 1065 | 57.6% | <20 | 80 | 10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | SLEV |
| 1071 | 62.0% | <20 | 40 | <10 | 10 | 10 | <10 | <10 | <10 | <10 | 10 | <10 | <10 | SLEV |
| 1072* | 79.8% | 20 | 1280 | 40 | 40 | <10 | <10 | <10 | 10 | <10 | 40 | 10 | <10 | SLEV |
| 1073* | 41.7% | <20 | 320 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | SLEV |
| 1079 | 37.0% | <20 | 80 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | SLEV |
| 1081 | 38.0% | <20 | 40 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | SLEV |
| 1082 | 46.8% | <20 | 40 | <10 | 10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | SLEV |
| 1084 | 51.2% | <20 | 160 | <10 | 20 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | SLEV |
| 1080 | 58.1% | 320 | 80 | <10 | 20 | <10 | <10 | <10 | <10 | <10 | 40 | <10 | <10 | WNV |
| 1088 | 71.6% | 40 | <20 | <10 | 10 | <10 | <10 | <10 | 10 | <10 | <10 | 10 | <10 | WNV |
| 1041 | 9.2% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1043 | 17.3% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1047 | 13.0% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1048 | 16.2% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1050 | 15.2% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1053 | 8.2% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1056 | 16.8% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1057 | 23.9% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1066 | 11.2% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1069 | 3.0% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1074* | 23.3% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1086 | 12.4% | - | - | - | - | - | - | - | - | - | - | - | - | |
| 1087 | -4.0% | - | - | - | - | - | - | - | - | - | - | - | - |
BSQV, Bussuquara virus; CPCV, Cacipacore virus; ILHV, Ilheus virus; ROCV, Rocio virus; SLEV, Saint Louis encephalitis virus; WNV, West Nile virus; IGUV, Iguape virus; YFV, Yellow fever virus; DENV, Dengue virus; ID: Horse identification; -, Not tested.
Equines that showed disease during the epizootic and survived.
Discussion
In the absence of direct viral detection, diagnosis of arbovirus infections is performed by indirect serological tests. However, cross-reactive antibody responses to closely related flaviviruses can complicate interpretation of serologic test results [36]. In particular, secondary flavivirus infections generate high levels of cross-reactive antibodies, which further complicate the interpretation of flavivirus serology. The cross-reacting antibodies of primary infections typically react with other members of the Japanese encephalitis virus serogroup comprised by WNV, CPCV, SLEV and others principally in Africa and Asia [37], [38], but antibodies generated by secondary flavivirus infections can also bind and neutralize viruses of other serogroups as well. Moreover, some individuals that are sequentially infected by a heterologous flavivirus species can boost antibody levels against the original virus, resulting in a phenomenon known as ‘original antigenic sin’ which can lead to incorrect diagnoses [39]. Finally, the potential circulation of unknown flaviviruses in the region could generate cross-reacting neutralizing antibodies, and lead to misinterpretation. Therefore, we used a conservative threshold for detection of neutralizing antibodies (90%) and we considered homotypic serologic responses to be the most reliable, as these samples reacted with just one of the 12 viruses employed in the tests, with no indication of cross-reaction.
In the present study, serological evidence of ILHV, SLEV, WNV, CPCV and ROCV circulation was detected in the Nhecolândia and Nabileque sub-regions of Pantanal. Nhecolândia is the second largest sub-region of Pantanal comprising roughly 27,000 square-km or 19% of the total Pantanal area and it is the world's largest and most diverse area of subtropical lakes [40], [41]. Nabileque is the fifth largest sub-region comprising roughly 14,000 square-km or 10% of the total Pantanal area. This sub-region is formed by fluvial plains of the Paraguay River and remains flooded for nine months or more during the year [42].
The seroprevalence of ILHV and all flaviviruses combined increased with age in equines (Figure 3). This temporal pattern implies low-level enzootic transmission, where risk of infection increases with time. A drop in seroprevalence in the oldest age category that was observed consistently for all the flaviviruses evaluated may be explained by either waning of detectable antibodies over time, and/or weakening of the humoral immune response in older animals. In the case of SLEV and WNV, seroprevalence appeared to increase with age in the youngest three age categories, through age 9 years old, but the sample sizes were insufficient to detect a statistically significant trend. These increases in the youngest age groups may be explained by one or more introductions with establishment or not of these viruses after 2000 (i.e. within 9 years of the sampling time point in 2009–2010). This finding corroborates the negative results found in a serosurvey conducted with local equines in the 1990s, when no neutralizing antibodies for SLEV were detected [24]. These data also corroborate the results of two other equine serosurveys conducted in the Nhecolândia Sub-region in February 2007 and February 2009, when neutralizing antibodies to SLEV were detected in three and four year old equines, respectively, which suggests that SLEV circulated between 2004–2007 [25] and 2005–2009 [21], coinciding with two human outbreaks caused by SLEV in Argentina in 2005 [43] and southeast Brazil in 2006 [4].
In the present study, the detection of SLEV- and ILHV-seropositive geldings both born in September 26, 2009 and sampled on September 30, 2010 with no history of travel outside of Pantanal indicates that the transmission of SLEV and ILHV had occurred as recently as late 2009 or 2010. The enzootic status of ILHV is corroborated by the concurrent isolation of ILHV from Aedes scapularis specimens captured in the Nhecolândia Sub-region in 2010 [44].
Regarding WNV, the youngest seropositive equine was a 2 year-old untamed mare with no history of travel. Because it was sampled on October 23, 2009, the infection occurred between 2007 and 2009.
The confirmed WNV-seropositive equines were detected in ten ranches comprising an area of approximately 2,500 square-km in the Nhecolândia and Nabileque sub-regions of the Pantanal, located in MS. Monotypic neutralizing reactions for WNV were detected in six ranches encompassing roughly 1,300 square-km, which comprise approximately 20% of the Nhecolândia Sub-region area. WNV-seropositive equines were detected in Nhecolândia and Nabileque ranches located roughly 90 and 100 km distant from the city of Corumbá, MS respectively (Figure 2). Considering the detection of arbovirus activity in the Nabileque Sub-region which borders Bolivia and Paraguay, these two countries should consider our findings for their arbovirus surveillance programs.
The two CPCV-seropositive equines were sampled October 20, 2009 at five years of age and no history of travel outside of Pantanal, which indicates that infection had occurred between 2004 and 2009.
We report here for the first time the detection of ROCV-neutralizing antibodies in the Pantanal region. ROCV, which is an indigenous Brazilian flavivirus, was the causative agent of an extensive encephalitis epidemic in southeastern Brazil in the 1970s [3]. The detection of neutralizing antibodies for ROCV was unexpected, as current transmission events for ROCV are rare. Considering that the only ROCV-seropositive equine had no birth date available, the timing of ROCV transmission could not be clarified. No ROCV-seropositive equines were detected in two previous serosurveys for flaviviruses conducted in the same region [21], [24], which could indicate low circulation or recent introduction of ROCV in the Pantanal.
No seropositivity for BSQV, IGUV, YFV and DENVs was confirmed among the equines tested in the present study. However, except for DENV-3, neutralizing antibodies were found to all the flaviviruses tested. More investigation is needed to understand the potential circulation of these viruses in the Pantanal region, as they may be restricted to ecological cycles for which equines, sheep and caiman fail to serve as indicators. A serosurvey of non-human primates and/or local human residents would be more instructive for these flaviviruses. Testing only equines may provide a biased view of the relative amounts of flavivirus transmission because equines may not mount immune responses to all viruses equally, or they may not attract all vectors equally. For example, they failed to generate primary immune responses to DENV-2 and SLEV [45] and would not attract large numbers of the yellow fever vector mosquitoes, which are primate specialists [46]. However, they are frequently exposed to mosquitoes and often utilized for arbovirus serosurveys elsewhere.
For future flavivirus serosurveys to be held in the Pantanal, not only ILHV, SLEV, WNV, CPCV and ROCV should be included as differential diagnosis, but also those flaviviruses for which neutralizing antibodies titers ≥20 were detected, including BSQV, IGUV and YFV, if a PRNT with a four-fold greater titer criterion is used.
Regarding the 36 equines collected from ranch PV in the Nabileque Sub-region of Pantanal after a neurologic disorder outbreak occurred in 2009 and 2010, no serological evidence was found linking this epizootic to WNV, which is currently the only flavivirus known to be involved in outbreaks of equine neurological disorders in the New World. Three of four survivors of the recent neurologic syndrome had elevated titers for SLEV, and one was the highest SLEV titer detected in the herd, suggesting that the etiologic agent was a flavivirus that triggered a boost of pre-existing SLEV antibody or that SLEV infection may have been associated with the neurologic syndrome as a contributing risk factor perhaps through antibody enhancement. Equines experimentally infected with SLEV have not developed overt disease [47]. However, the possibility that a novel equine-virulent strain of SLEV caused the neurologic disease in horses in Brazil also merits exploration. SLEV genotype VB was recently isolated from the brain of a single horse that died of encephalitis in the state of Minas Gerais, southeast Brazil, in March 2009 [48]. Of the 36 equines tested from ranch PV, 11 (30.6%) were confirmed seropositive for SLEV, the highest seropositivity compared to 13 other ranches where SLEV-seropositive equines were found (and where maximum seroprevalence was 14%) and significantly higher than SLEV seropositivity detected in all Nhecolândia equines combined (48/724, 6.6%) (p<0.001, chi-square test). The true SLEV infection rate is probably underestimated, as several probable SLEV infections could not be differentiated due to masking by cross-reactive antibodies. Ecological differences between Nabileque and Nhecolândia sub-regions, the former formed by fluvial plains of the Paraguay River and the latter mainly comprised of savannah with subtropical lakes, may have contributed to the difference of seroprevalence encountered in these two sub-regions. Also, the Nabileque ranch is the largest ranch sampled encompassing a 900-square-km area, including portions of the plateau bordering the Pantanal. The high seropositivity for SLEV in Nabileque ranch may reflect higher circulation of SLEV in the plateau surrounding Pantanal than in the floodplains of Pantanal.
Amphibians and reptiles may play a larger role in the transmission cycle of arboviruses than previously assumed. Because of their high energy conversion efficiency, ectotherms typically represent a large portion of the vertebrate biomass in many ecosystems, and may therefore greatly influence transmission dynamics, either as virus amplifiers or dilution hosts [49]. Juvenile Alligator mississippiensis has been shown to develop sufficient WNV viremia to infect blood-feeding mosquitoes [50], [51]. A recent study reported the first evidence of WNV exposure in wild Morelet's crocodiles (Crocodylus moreletii) in Mexico [52].
Because of widespread, high prevalence of the yacare caiman (Caiman crocodilus yacare) in the Brazilian Pantanal, about 3.9 million non-hatchling caimans in 1993 [53], and its potential to naturally amplify WNV in the region, in February of 2009 a serosurvey for flaviviruses was conducted with 30 free-ranging caimans and all animals tested negative for flavivirus antibodies. Despite the negative results, in the same study equines temporally and spatially associated with the seronegative caimans showed neutralizing antibodies for ILHV, SLEV, WNV and CPCV [21]. Taking into account these data, in the present study a wider serosurvey for flaviviruses was conducted with 61 free-ranging caimans from the Nhecolândia Sub-region, but all caimans tested negative for flavivirus antibodies by blocking ELISA and also by PRNT90 for WNV. The absence of serological evidence of flavivirus circulation in caimans was unexpected. Possible explanations for these findings are: (i) low circulation of flavivirus in caimans, (ii) caimans may not mount immune responses to flaviviruses and, finally, (iii) caimans may not attract local mosquito vectors of flaviviruses.
In a study conducted also in the Pantanal, but in a different sub-region, 80% of mosquitoes caught blood-feeding on caimans were Culex (Melanoconion) theobaldi and Mansonia spp. [54], species that are not usually reported as flavivirus vectors. However, more recently, ILHV was isolated from Aedes scapularis, which was the most prevalent species caught landing or blood-feeding on caimans from the Nhecolândia Sub-region [44].
The absence of serological evidence of flavivirus circulation in sheep by blocking ELISA and the detection of only two samples with neutralizing antibodies for WNV in very low titers was also an unexpected result, considering that the tested sheep were temporally and spatially associated with equines that were seropositive for various flaviviruses. However, reports of serological evidence of WNV infection in sheep are scarce and have been showing low prevalence [55], [56]. Possible explanations for these findings are the low prevalence of Brazilian flaviviruses in sheep, or that sheep fail to develop antibodies for Brazilian flaviviruses following exposure by mosquito bite, or finally, that sheep may not attract local mosquito flavivirus vectors in the Pantanal region. An entomological study conducted in southeast Brazil in the 1980s showed that sheep was not an attractive host for mosquitoes compared with man, horse and cattle [57].
Conclusion
In the present study, serological evidence of ILHV, SLEV, WNV, CPCV and ROCV circulation was detected in equines of the Pantanal. Severe disease has been linked to these viruses in humans [7], [13], [43], [58], [59] and for WNV also in equines [60]. WNV and SLEV circulation in the Pantanal appears to be a recent phenomenon. In the last three decades, the Pantanal has been impacted by the conversion of natural vegetation into agricultural fields and cattle pasture, with alteration and loss of natural habitats and biodiversity. Moreover, major negative impacts occur in uplands, with drastic deforestation of savanna vegetation, where main rivers feeding the Pantanal have their springs [22], [61]. These environmental changes in the Pantanal environs can directly impact the fluctuations of vector and vertebrate host populations, which could affect arbovirus transmission dynamics in the region. Loss of wetlands and other natural habitats typically leads to reduced biodiversity, and consequently increased risk of outbreaks of vector-borne diseases [62]. Preserving large wetland areas sustains biodiversity and may represent a valuable ecosystem-based approach for controlling WNV outbreaks [63]. Indeed, an outbreak of neurologic disease among equines reported herein occurred in a ranch that encompasses drier plateau ecosystem on the periphery of the Pantanal wetlands. Serology data suggest that an unknown flavivirus closely related to SLEV or a newly recognized equine-virulent strain of SLEV may be associated with this neurologic syndrome.
Considering the highly conservative criteria used in the present study, the detection of seropositive equines for ILHV, SLEV, WNV, CPCV and ROCV is strong evidence for local circulation of these flaviviruses in the Pantanal of MS, Brazil. These flaviviruses should be included as differential diagnosis in future flavivirus serosurveys to be held in the region. For PRNT studies, not only these flaviviruses, but also YFV, BSQV and IGUV should be included.
It appears that WNV circulated recently in the Pantanal. The detection of WNV-seropositive equines in at least ten ranches is strong evidence of recent widespread circulation, but not necessarily establishment of WNV in the region. Circulation of WNV in this area has not yet been confirmed by virus isolation. Because detection of antibodies is indirect evidence of flavivirus circulation and because novel flaviviruses may exist in the region, we encourage efforts to isolate viruses to confirm the circulation of these flaviviruses. In future investigations of equine epizootics, efforts should be concentrated on the collection of samples suitable for viral isolation.
Acknowledgments
We thank the staff of Embrapa Pantanal including Oziel da Silva, Henrique de Jesus, José Augusto da Silva, Cremilson Gonçalves, Murilo Maciel, Márcio da Silva, Marcos José Alves, Nelson Rodrigues, Roberto Rondon, Sebastião de Jesus, Vandir da Silva, Ricardo Oseko, Marcos José, Marcos Tadeu and the researchers Marcia Furlan and Thierry Tomich, as well as the owners and staff of all ranches visited. Special thanks to Luiz Pellegrin of Geoprocessing Laboratory of Embrapa Pantanal, Janeen Laven, Nicholas Panella, Olga Kosoy, Brandy Russell, Alison Johnson and Brad Biggerstaff of Centers for Disease Control and Prevention and Dinair Couto-Lima, Filipe Carvalho-Costa, Heloisa Diniz, Flávia dos Santos and Ana Bispo of Fundação Oswaldo Cruz for technical support.
Funding Statement
Funding was provided by CNPq, CAPES, Fulbright, FIOCRUZ, CDC and FAPERJ. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Nogueira RMR, de Araújo JM, Schatzmayr HG (2007) Dengue viruses in Brazil, 1986–2006. Rev Panam Salud Publica 22 5: 358–363. [DOI] [PubMed] [Google Scholar]
- 2. Câmara FP, de Carvalho LM, Gomes AL (2013) Demographic profile of sylvatic yellow fever (SYF) in Brazil from 1973 to 2008. Trans R Soc Trop Med Hyg 107 5: 324–327. [DOI] [PubMed] [Google Scholar]
- 3. Tiriba AC, Miziara AM, Lourenço R, Costa CRB, Costa CS, et al. (1976) Encefalite humana primária epidêmica por arbovírus observada no litoral sul do Estado de São Paulo. Rev Assoc Med Bras 22: 415–420. [PubMed] [Google Scholar]
- 4. Mondini A, Cardeal IL, Lázaro E, Nunes SH, Moreira CC, et al. (2007) Saint Louis encephalitis virus, Brazil. Emerg Infect Dis 13 1: 176–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Srihongse S, Johnson CM (1971) The first isolation of Bussuquara virus from man. Trans R Soc Trop Med Hyg 65 4: 541–542. [DOI] [PubMed] [Google Scholar]
- 6. Nassar ES, Coimbra TLM, Rocco IM, Pereira LE, Ferreira IB, et al. (1997) Human disease caused by an arbovirus closely related to Ilheus virus: Report of five cases. Intervirology 40: 247–252. [DOI] [PubMed] [Google Scholar]
- 7. Batista WC, Tavares GSB, Vieira DS, Honda ER, Pereira SS, et al. (2011) Notification of the first isolation of Cacipacore virus in a human in the State of Rondônia, Brazil. Revista da Sociedade Brasileira de Medicina Tropical 44 4: 528–530. [DOI] [PubMed] [Google Scholar]
- 8. de Almeida MA, Dos Santos E, da Cruz Cardoso J, da Fonseca DF, Noll CA, et al. (2012) Yellow fever outbreak affecting Alouatta populations in southern Brazil (Rio Grande do Sul State), 2008–2009. Am J Primatol 74 1: 68–76. [DOI] [PubMed] [Google Scholar]
- 9. Davis NC, Burke AW (1929) Studies on South American yellow fever: I. The strains of virus in use at the yellow fever laboratory in Bahia, Brazil. J Exp Med 49 6: 975–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Laemmert HW, Hughes TP (1947) The virus of Ilhéus encephalitis. J Immunol 55: 61–67. [PubMed] [Google Scholar]
- 11. Gomes G, Causey OR (1959) Bussuquara; a new arthropod-borne virus. Proc Soc Exp Biol Med 101 2: 275–279. [DOI] [PubMed] [Google Scholar]
- 12. Causey OR, Shope RE, Theiler M (1964) Isolation of St. Louis encephalitis virus from arthropods in Pará, Brazil. Am J Trop Med Hyg 13: 449. [DOI] [PubMed] [Google Scholar]
- 13. Lopes OS, Coimbra TL, de Abreu Sacchetta L, Calisher CH (1978) Emergence of a new arbovirus disease in Brazil. I. Isolation and characterization of the etiologic agent, Rocio virus. Am J Epidemiol 107 5: 444–449. [DOI] [PubMed] [Google Scholar]
- 14.Karabatsos N (1985) International catalogue of arboviruses including certain other viruses of vertebrates. 3 ed. San Antonio: American Society of Tropical Medicine & Hygiene. 1147 p. [Google Scholar]
- 15. Osanai CH, Rosa APT, Tang A, Amaral R, Passos ADC, et al. (1983) Surto de dengue em Boa Vista, Roraima: Nota previa. Rev Inst Med Trop Sao Paulo 25 1: 53–54. [PubMed] [Google Scholar]
- 16. Nogueira RMR, Miagostovich MP, Lampe E, Schatzmayr HG (1990) Isolation of dengue virus type 2 in Rio de Janeiro. Mem Inst Oswaldo Cruz 85 2: 253. [DOI] [PubMed] [Google Scholar]
- 17. Coimbra TL, Nassar ES, Nagamori AH, Ferreira IB, Pereira LE, et al. (1993) Iguape: a newly recognized flavivirus from São Paulo State, Brazil. Intervirology 36 3: 144–152. [DOI] [PubMed] [Google Scholar]
- 18. Rodrigues SG, Azevedo RSS, Martins LC, Nunes MRT, Araújo GCB, et al. (2004) Estudo eco-epidemiológico na área do projeto salobo, marabá-pará: isolamento e identificação de amostras de arbovírus. III Simpósio internacional sobre arbovírus dos trópicos e febres hemorrágicas, Belém [Google Scholar]
- 19. Nogueira RMR, Miagostovich MP, Filippis AMB, Pereira MAS, Schatzmayr HG (2001) Dengue type 3 in Rio de Janeiro, Brazil. Mem Inst Oswaldo Cruz 96 7: 925–926. [DOI] [PubMed] [Google Scholar]
- 20. Machado DC, Mondini A, Santana Vdos S, Yonamine PT, Chiaravalloti Neto F, et al. (2012) First identification of Culex flavivirus (Flaviviridae) in Brazil. Intervirology 55: 475–483. [DOI] [PubMed] [Google Scholar]
- 21. Pauvolid-Corrêa A, Morales MA, Levis S, Figueiredo LT, Couto-Lima D, et al. (2011) Neutralising antibodies for West Nile virus in horses from Brazilian Pantanal. Mem Inst Oswaldo Cruz 106 4: 467–474. [DOI] [PubMed] [Google Scholar]
- 22. Alho CJR (2011) Concluding remarks: overall impacts on biodiversity and future perspectives for conservation in the Pantanal biome. Braz J Biol 71 1 Suppl 1: 337–341. [DOI] [PubMed] [Google Scholar]
- 23.Alho CJR. (2005) The Pantanal. In: Fraser LH, Keddy PA, eds. The world's largest wetlands: ecology and conservation. New York: Cambridge University Press. pp.203–271. [Google Scholar]
- 24. Iversson LB, Silva RAMS, Travassos da Rosa APA, Barros VLRS (1993) Circulation of eastern equine encephalitis, western equine encephalitis, ilheus, maguari and tacaiuma viruses in equines of the Brazilian Pantanal, South America. Rev Inst Med Trop Sao Paulo 35 4: 355–359. [DOI] [PubMed] [Google Scholar]
- 25. Pauvolid-Corrêa A, Tavares FN, Costa EV, Burlandy FM, Murta M, et al. (2010) Serologic evidence of the recent circulation of Saint Louis encephalitis virus and high prevalence of equine encephalitis viruses in horses in the Nhecolândia sub-region in South Pantanal, Central-West Brazil. Mem Inst Oswaldo Cruz 105: 829–833. [DOI] [PubMed] [Google Scholar]
- 26. Melandri V, Guimarães AÉ, Komar N, Nogueira ML, Mondini A, et al. (2012) Serological detection of West Nile virus in horses and chicken from Pantanal, Brazil. Mem Inst Oswaldo Cruz 107 8: 1073–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Silva JR, Medeiros LC, Reis VP, Chávez JL, Munhoz TD, et al. (2013) Serologic survey of West Nile virus in horses from Central-West, Northeast and Southeast Brazil. Mem Inst Oswaldo Cruz 108 6: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ometto T, Durigon EL, de Araujo J, Aprelon R, de Aguiar DM, et al. (2013) West Nile virus surveillance, Brazil, 2008–2010. Trans R Soc Trop Med Hyg 107 11: 723–730. [DOI] [PubMed] [Google Scholar]
- 29. Olson GA, Hessler JR, Faith RE (1975) Technics for blood collection and intravascular infusion of reptiles. Lab Anim Sci 25: 783–786. [PubMed] [Google Scholar]
- 30. Blitvich BJ, Bowen RA, Marlenee NL, Hall RA, Bunning ML, et al. (2003) Epitope-blocking enzyme-linked immunosorbent assays for detection of West Nile virus antibodies in domestic mammals. J Clin Microbiol 41: 2676–2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Russell PK, Nisalak A, Sukhavachana P, Vivona S (1967) A plaque reduction test for dengue virus neutralizing antibodies. J Immunol 99: 285–290. [PubMed] [Google Scholar]
- 32. Calisher CH, Karabatsos N, Dalrymple JM, Shope RE, Porterfield JS, et al. (1989) Antigenic relationships between flaviviruses as determined by cross-neutralization tests with polyclonal antisera. Journal of General Virology 70: 37–43. [DOI] [PubMed] [Google Scholar]
- 33. Johnson BW, Kosoy O, Hunsperger E, Beltran M, Delorey M, et al. (2009) Evaluation of chimeric Japanese encephalitis and Dengue viruses for use in diagnostic plaque reduction neutralization tests. Clinical Vaccine and Immunology 16: 1052–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. De Madrid AT, Porterfield JS (1974) The flaviviruses (group B arboviruses): a cross-neutralization study. J Gen Virol 23 1: 91–96. [DOI] [PubMed] [Google Scholar]
- 35. Varelas-Wesley I, Calisher CH (1982) Antigenic relationships of flaviviruses with undetermined arthropod-borne status. Am J Trop Med Hyg 31 6: 1273–1284. [DOI] [PubMed] [Google Scholar]
- 36. Góes P, Bruno-Lobo M (1961) Estudos sobre arbovírus: Síntese do problema e plano inicial de trabalho: Diagnóstico das arboviroses. An Microbiol 9 A: 67–79. [Google Scholar]
- 37. Tarr GC, Hammon WM (1974) Cross-protection between group B arboviruses: resistance in mice to Japanese B encephalitis and St. Louis encephalitis viruses induced by Dengue virus immunization. Infect Immun 9 5: 909–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.King AMQ, Adams MJ, Carstens EB, Lefkowitz EJ (2012) Virus Taxonomy: Ninth report of the international committee on taxonomy of viruses. San Diego: Elsevier Academic Press. pp.1327. [Google Scholar]
- 39. Inouye S, Matsuno S, Tsurukubo Y (1984) “Original antigenic sin” phenomenon in experimental flavivirus infections of guinea pigs: studies by enzyme-linked immunosorbent assay. Microbiol Immunol 28: 569–574. [DOI] [PubMed] [Google Scholar]
- 40. Silva JSV, Abdon MM (1988) Delimitação do Pantanal brasileiro e suas sub-regiões. Pesq Agrop Bras 33: 1703–1711. [Google Scholar]
- 41. Almeida TI, Calijuri Mdo C, Falco PB, Casali SP, Kupriyanova E, et al. (2011) Biogeochemical processes and the diversity of Nhecolândia lakes, Brazil. Ann Acad Bras Cienc 83 2: 391–407. [DOI] [PubMed] [Google Scholar]
- 42. Straube FC, Urben-Filho A, Nunes AP, Tomás WM, Vieira-da-Rocha MC (2006) Avifauna do pantanal de nabileque (Mato Grosso do Sul, Brasil). Atualidades ornitológicas 134: 1–22. [Google Scholar]
- 43. Spinsanti LI, Díaz LA, Glatstein N, Arselán S, Morales MA, et al. (2008) Human outbreak of St. Louis encephalitis detected in Argentina, 2005. J Clin Virol 42: 27–33. [DOI] [PubMed] [Google Scholar]
- 44. Pauvolid-Corrêa A, Kenney JL, Couto-Lima D, Campos Z, Schatzmayr HG, et al. (2013) Ilheus virus isolation in the Pantanal, west-central Brazil. PLOS Neg Trop Dis 7 7: e2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ledermann JP, Lorono-Pino MA, Ellis C, Saxton-Shaw KD, Blitvich BJ, et al. (2011) Evaluation of widely used diagnostic tests to detect West Nile virus infections in horses previously infected with St. Louis encephalitis virus or dengue virus type 2. Clin Vaccine Immunol 18 4: 580–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Consoli RAGB, Lourenço-de-Oliveira R (1994) Principais mosquitos de importância sanitária no Brasil. Rio de Janeiro: Editora Fiocruz. pp.228. [Google Scholar]
- 47. Hammon W McD, Carle BN, Izumi EM (1942) Infection of Horses with St. Louis Encephalitis Virus, Experimental and Natural. Exp Biol Med March 49 3: 335–340. [Google Scholar]
- 48. Rosa R, Costa EA, Marques RE, Oliveira TS, Furtini R, et al. (2013) Isolation of Saint Louis encephalitis virus from a horse with neurological disease in Brazil. PLoS Negl Trop Dis 7 11: e2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Graham SP, Hassan HK, Chapman T, White G, Guyer C, et al. (2012) Serosurveillance of eastern equine encephalitis virus in amphibians and reptiles from Alabama, USA. Am J Trop Med Hyg 86 3: 540–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Klenk K, Snow J, Morgan K, Bowen R, Stephens M, et al. (2004) Alligators as West Nile virus amplifiers. Emerg Infect Dis 10: 2150–2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Jacobson ER, Ginn PE, Troutman JM, Farina L, Stark L, et al. (2005) West Nile virus infection in farmed American alligators (Alligator mississippiensis) in Florida. J Wildl Dis 41: 96–106. [DOI] [PubMed] [Google Scholar]
- 52. Machain-Williams C, Padilla-Paz SE, Weber M, Cetina-Trejo R, Juarez-Ordaz JA, et al. (2013) Antibodies to West Nile virus in wild and farmed crocodiles in southeastern Mexico. J Wildl Dis 49 3: 690–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mourão G, Coutinho M, Mauro R, Campos Z, Tomás W, et al. (2000) Aerial surveys of caiman, marsh deer and pampas deer in the Pantanal Wetland of Brazil. Biological Conservation 92: 175–183. [Google Scholar]
- 54. Viana LA, Soares P, Paiva F, Lourenço-De-Oliveira R (2010) Caiman-biting mosquitoes and the natural vectors of Hepatozoon caimani in Brazil. J Med Entomol 47 4: 670–676. [DOI] [PubMed] [Google Scholar]
- 55. Vasil'ev AV, Shchelkanov MIu, Dzharkenov AF, Aristova VA, Galkina IV, et al. (2005) [West Nile virus infection of agricultural animals in the Astrakhan region, as evidenced by the 2001–2004 serological surveys]. Vopr Virusol 50 6: 36–41 [Article in Russian] [PubMed] [Google Scholar]
- 56. Ozkul A, Yildirim Y, Pinar D, Akcali A, Yilmaz V, et al. (2006) Serological evidence of West Nile Virus (WNV) in mammalian species in Turkey. Epidemiol Infect 134 4: 826–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lourenço-de-Oliveira R, Heyden R (1986) [Various aspects of the ecology of mosquitoes (Diptera, Culicidae) from a plains area (Calabria Farms) in Jacarepagua, Rio de Janeiro. V. Breeding grounds]. Mem Inst Oswaldo Cruz 81 1: 15–27 [Article in Portuguese] [DOI] [PubMed] [Google Scholar]
- 58. Venegas EA, Aguilar PV, Cruz C, Guevara C, Kochel TJ, et al. (2012) Ilheus virus infection in human, Bolivia. Emerg Infect Dis 18 3: 516–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Chung WM, Buseman CM, Joyner SN, Hughes SM, Fomby TB, et al. (2013) The 2012 West Nile encephalitis epidemic in Dallas, Texas. JAMA 310 3: 297–307. [DOI] [PubMed] [Google Scholar]
- 60. Ward MP (2005) Epidemic West Nile virus encephalomyelitis: A temperature-dependent, spatial model of disease dynamics. Prev Vet Med 71: 253–264. [DOI] [PubMed] [Google Scholar]
- 61.Silva JSV, Abdon MM, Moraes JA (2010) Desmatamento na bacia do Alto Paraguai no Brasil. In: Anais do III Simpósio de Geotecnologias no Pantanal. Cáceres: Embrapa Informática Agropecuária/INPEp. 458–467. [Google Scholar]
- 62. Ostffeld RS, Keesing F (2000) The function of biodiversity in the ecology of vector-borne zoonotic diseases. Canadian J Zool 78: 2061–2078. [Google Scholar]
- 63. Ezenwa VO, Milheim LE, Coffey MF, Godsey MS, King RJ, Guptill SC (2007) Land cover variation and West Nile virus prevalence: patterns, processes, and implications for disease control. Vector Borne Zoonotic Dis 7 2: 173–180. [DOI] [PubMed] [Google Scholar]