Abstract
Objective
To describe longitudinal change in child behavior problems associated with resolution of intimate partner violence (IPV) after an investigation for suspected child maltreatment.
Design
Retrospective cohort study.
Data Source
The National Survey of Child and Adolescent Well-Being, a nationally representative longitudinal sample of U.S. households investigated for suspected child maltreatment.
Participants
320 school-aged NSCAW subjects with caregiver-reported IPV in the year prior to baseline interview. Caregivers were interviewed an average of 3, 20, 36, and 81 months following investigation.
Main Exposure
Resolution vs. persistence of baseline IPV. Persistence defined by report of IPV during any follow-up interview.
Outcome Measures
Clinically significant internalizing or externalizing child behavior problems.
Results
44.6% of caregivers reporting IPV at the baseline interview reported persistent IPV. After adjusting for significant covariates, IPV resolution was associated with an 11.9% reduction in internalizing problems by 81 months (p=0.03); IPV persistence was associated with persistence in baseline problems. IPV resolution was associated with an 18.5% reduction in externalizing problems by 20 months that was sustained at 36 and 81 months (all p<0.05). IPV persistence was associated with a steady but non-significant increase in externalizing behavior problems over 81 months (10.1%, p=0.07). Adjusted relative risk of internalizing and externalizing behavior problems 81 months following CPS investigation for children exposed to persistent vs resolved IPV was 1.79 (0.91, 3.52) and 1.88 (1.12, 3.18), respectively.
Conclusions
Resolution of IPV after a CPS investigation for suspected child maltreatment is associated with meaningful, sustained reductions in clinically significant child behavior problems.
Background
Intimate partner violence (IPV) is a common reality for many families in the United States. More than one in twenty women experience some form of IPV annually, and more than one in twenty children witness IPV in their homes every year.1,2 The prevalence of IPV in households involved with child protective services (CPS) may be six-fold higher, with a third of these households reporting IPV in the 12 months preceding CPS investigation.3,4
As with children who experience maltreatment, children who witness IPV have a high risk for behavioral and mental health problems.5–8 Prior authors have described a “double-whammy” effect for children who experience maltreatment and witness IPV, with outcomes significantly worse than those described in children living with maltreatment or IPV alone.9,10 It is unknown, however, whether resolution of IPV in a home can change the negative outcomes commonly described for children living with family violence. Evidence that resolution of IPV could result in meaningful improvements in child outcomes would strengthen and support the efforts of CPS caseworkers, mental health providers and pediatricians to identify and address this issue.11–14
The goal of this study is to examine the association between resolution of IPV and child behavior problems in a nationally representative sample of households investigated by CPS for suspected maltreatment. Our hypotheses are that resolution of IPV after a CPS investigation is associated with reduction of child behavior problems over time, and that persistence of IPV is associated with persistence of child behavior problems over time.
Methods
Design
This is a retrospective cohort study including children with a recent CPS investigation for suspected maltreatment and a primary caregiver with a report of IPV in the preceding 12 months.
Data Source
We drew our study population from the CPS component of the National Survey of Child and Adolescent Well-Being (NSCAW). The CPS component of NSCAW is a longitudinal sample of 5,501 children aged 0 to 14 years followed prospectively after a CPS investigation for suspected abuse or neglect between October 1999 and December 2000. NSCAW selected 8,961 subjects from 92 social service agencies in 36 U.S. states, using a sampling strategy to provide national estimates of characteristics of the children and families involved with CPS.15 Of this sample, 1,151 (14%) could not be contacted, 1,014 were ineligible (11%), and 1,028 (13%) refused to participate.16 NSCAW conducted face-to-face interviews with consenting participants over 4 waves between 1999 and 2007. Audio-Computer Assisted Self Interview (A-CASI) was used to collect sensitive data regarding IPV, mental health, substance abuse, and corporal punishment. Study-developed probabilistic weights allow national estimates to be generated for selected subpopulations within and across survey waves.17
NSCAW data were made available by the National Data Archive on Child Abuse and Neglect, Cornell University, Ithaca, NY and are used with Archive permission. The University of Utah IRB granted approval for analysis of NSCAW data.
Study population
We restricted the NSCAW sample to subjects with interview data from each NSCAW wave (n= 3,802, unweighted). We excluded children under 2 years of age at the baseline interview or above 18 years of age at the final interview as the child behavior measure used for this analysis was not collected for these children (n=1,763). Within this eligible sample, we identified a cohort of children with a permanent primary caregiver who reported IPV in the 12 months prior to the baseline interview (n=389). Finally, we excluded children in out of home placements at any interview, as NSCAW collected IPV data only from permanent caregivers (n=320). On average, NSCAW interviewed these caregivers at 3, 20, 36, and 81 months following CPS investigation. This subsample represented approximately 12.6% (n~295,051) of all CPS-involved children during the study period.
Exposure
The exposure of interest was persistent IPV after a CPS investigation for suspected child maltreatment. Children with caregivers reporting IPV at any of the following NSCAW interviews were defined as having persistent IPV (exposed). Children with caregivers with no report of IPV at any of the following NSCAW interviews were defined as having resolved IPV (unexposed).
NSCAW used the Conflict Tactics Scale-1 (CTS-1) to measure caregiver-reported IPV in households with a CPS investigation for suspected child maltreatment. The CTS-1 captures12-month prevalence of physical violence between partners, including minor (pushing, shoving, or slapping) and severe (choking, beating, or threatening with weapons) forms of violence.16 At each timepoint, we defined presence of IPV as any positive response on the CTS-1 physical violence subscale.
Outcomes
We defined the outcome as the presence of a clinically significant behavioral problem at each interview. We modeled internalizing (shy, depressive, or withdrawn) and externalizing (aggressive or oppositional) behavior problems controlling for IPV exposure.
NSCAW administered the Child Behavioral Checklist (CBCL) to caregivers of children between 2 and 18 years of age at each interview. The CBCL is a measure of behavioral problems in children with both research and clinical applications. Raw CBCL scores are normed on age and sex to provide a standardized T-score. T-scores above 63 are observed in less than 10% of a normative sample and reflect clinically significant behavior problems.18,19
Covariates
IPV and child maltreatment are associated with a range of characteristics that may modify or explain any observed associations between IPV persistence and child behavior problems over time. For our analysis, we defined covariates as demographics, risk factors, and CPS case information potentially associated with our primary exposure (IPV)or outcomes (child behavior problems)(eTable 1).
Missing data
There are three levels of missing data in the NSCAW dataset: wave-based non-response (missing due to subject drop-out), design based non-response (missing due to a priori study design), and item-based non-response (missing due to subject choice or study error). We selected probability weights developed by NSCAW investigators for subjects interviewed across all waves to adjust for wave-based non-response.17 We identified our study sample to address possible limitations associated with NSCAW’s design-based non-response.
Item-based non-response was rare in our sample. Exposure data (persistent vs. resolved IPV over all surveys) were missing in 6 of 320 (1.9%) study subjects. Outcome data (internalizing and externalizing behavior problems) were missing in none of 320 subjects at the 3, 20, and 36-month surveys and in one subject (0.3%) at the 81-month survey.
Analysis
We compared baseline demographics, risk factors, and CPS case information for our study population to the full NSCAW population to identify differences between our study population and other CPS-involved families. We conducted bivariate analyses of demographics, risk factors, and CPS case information for children in our study population based on the IPV persistence after CPS involvement. Finally, we examined bivariate associations between these same variables and baseline internalizing and externalizing behavior problems in our study population.
Covariates associated with IPV persistence after CPS involvement or with baseline child behavior problems were included in both multivariable models (p<0.1 in bivariate comparisons). In addition, each model included our exposure variable (resolved vs. persistent IPV), a categorical time variable (3, 20, 36, or 81 months since CPS investigation), and an interaction between IPV persistence and time since CPS investigation. With each model, we determined the adjusted probabilities for internalizing or externalizing behavior problems at each timepoint, and compared changes in these probabilities over time.20 At each of these timepoints, we calculated adjusted risk ratios (ARR) to compare the relative risk of clinically significant behavior problems in children living in households with persistent IPV to children in households with resolved IPV.21
Finally, we conducted exploratory bivariate analyses of IPV and mental health referrals and resources provided by investigative CPS caseworkers and the services utilized by caregivers to examine factors associated with resolution of IPV following CPS investigation.
All analyses were conducted with the survey (svy) analysis package in STATA 12.0 (Statacorp, College Station, TX), using subpopulation commands and NSCAW-developed probability weights to assure appropriate probability weighting for our study population. This provides robust standard errors to account for stratification, clustering, and weighting in the NSCAW sampling design. Using this approach, our results provide a national estimate of the experiences of CPS-involved children with caregiver-reported IPV present in the home in the year preceding CPS investigation.17
Results
Subjects
Children in the study population were younger (6.2 vs. 7.6 years, p<0.01) than the excluded NSCAW population but were similar in sex, race, ethnicity, and baseline behavioral problems. Similarly, caregivers in the study population were younger(30.3 vs. 34.3 years, p<0.01) than caregivers in the excluded population. All primary caregivers in our study population were female (maternal) caregivers, compared to 10.1% of male caregivers in the excluded population (p<0.01). These women were more likely to have baseline depression (41.5% vs. 25.2%, p<0.01), acknowledge drug and/or alcohol abuse (8.8% vs. 3.4%, p=0.01), or use corporal punishment (84.3% vs. 66.2%, p<0.01) when compared with caregivers in the excluded population. There were no significant differences in CPS case characteristics between the study and the excluded population.
Persistence of IPV exposure after a CPS investigation
Almost half (44.6%)of caregivers identifying recent IPV at the baseline interview reported persistent IPV during at least one follow-up interview. Although 55.7% of caregivers with persistent IPV reported IPV at only one other interview, 31.1% reported IPV at two interviews, and 13.2% reported IPV at every interview.
Baseline demographics, risk factors, and CPS involvement (Table 1)
Table 1.
Estimates of baseline demographics, risk factors, and CPS case characteristics in children with and without persistent IPV exposure after CPS involvement
| Resolved IPV* n=131 % (95% CI) | Persistent IPV* n=183 % (95% CI) | |
|---|---|---|
| Estimated population** | ||
| ≈ estimated sample size | 154,458 | 124,554 |
| ≈ estimated proportion | 55.7 (46.1, 64.6) | 44.6 (35.4, 53.9) |
| Child | ||
| Femalea | 52.1 (34.7, 69.4) | 51.4 (37.5, 65.2) |
| Age 2–5 yearsa | 39.6 (45.8, 74.8) | 65.8 (54.6, 77.0) |
| Minority racea | 40.2 (24.0, 56.4) | 38.7 (25.0, 52.4) |
| Hispanic ethnicitya | 22.1 (6.8, 37.3) | 9.0 (2.8, 15.1) |
| Internalizing behavior problemb | 20.0 (8.2, 31.8) | 26.2 (13.1, 39.2) |
| Externalizing behavior problemc | 37.9 (19.8, 56.1) | 32.5 (17.8, 47.2) |
| Caregiver | ||
| Female | 100 | 100 |
| Age: <30 years a | 51.8 (35.8, 67.9) | 58.4 (45.9, 70.9) |
| 30–39 yearsa | 37.3 (23.1, 51.5) | 35.1 (22.0, 48.3) |
| 40+ yearsa | 10.8 (1.5, 20.2) | 6.4 (1.5, 11.2) |
| No high school diploma | 22.4 (10.1, 34.8) | 25.8 (14.5, 37.1) |
| Partnereda | 44.5 (26.7, 62.2) | 62.3 (50.0, 74.6) |
| Poverty | 54.0 (38.2, 69.7) | 55.7 (41.5, 69.8) |
| Low social support | 33.2 (17.5, 49.1) | 33.2 (17.5, 49.1) |
| Depressiona | 44.4 (26.3, 62.5) | 40.7 (26.6, 54.8) |
| Drug or alcohol dependencea | 3.4 (0, 7.2) | 16.2 (5.3, 27.1) |
| Corporal punishment | 83.6 (72.0, 95.1) | 88.0 (80.1, 95.9) |
| Severe IPV (such as being choked, beaten, threatened with a knife or gun)a | 62.8 (48.8, 76.8) | 60.8 (48.3, 73.2) |
| CPS case characteristics | ||
| Prior CPS investigationa | 53.2 (36.5, 69.8) | 48.3 (36.3, 60.3) |
| Maltreatment type: Physical abuse | 23.9 (10.7, 37.1) | 23.8 (9.9, 37.7) |
| Sexual abuse | 16.1 (4.9, 27.3) | 7.9 (2.2, 13.7) |
| Neglect | 37.9 (20.1, 55.6) | 48.4 (35.7, 61.0) |
| Substantiated | 39.9 (23.3, 56.6) | 35.0 (23.4, 46.6) |
| Post-investigation servicesd | 53.1 (37.9, 68.3) | 38.9 (28.1, 49.7) |
Bolded variables reflect difference (p<0.05) based on persistence of IPV.
All subjects had report of recent IPV at baseline interview (3 months after CPS investigation). Resolved IPV indicates no caregiver-reported IPV at 20, 36, and 81 month interviews; Persistent IPV reflects caregiver-reported IPV during at least of these interviews.
Raw sample numbers are provided only for reference.. The estimated proportion is the weighted proportion of all U.S. children with caregiver-reported IPV around the time of CPS investigation and is calculated using NSCAW-developed probability weights to account for oversampling and non-response.
Included in all multivariable models based on association (p<0.1) with IPV resolution (child age and ethnicity; caregiver substance abuse and partner status), internalizing behavior problems (child sex), or externalizing behavior problems (use of corporal punishment)
Baseline internalizing behavior problems included in multivariable model for internalizing behavior problems
Baseline externalizing behavior problems included in multivariable model for externalizing behavior problem
CPS caseworker reports that “Regardless of the outcome of the investigation, services have been provided to or arranged for the family”
Children with persistent IPV exposure were younger (65.8% vs. 39.6% under 6 years of age, p<0.01) and less likely to be Hispanic (9.0% vs. 22.1%, p=0.04)compared to those with resolution of baseline IPV. Persistence of IPV was more common for partnered caregivers(62.3% vs. 44.5%, p=0.09) and for caregivers with drug or alcohol dependence(80.4% vs. 42.6%, p<0.01)
Internalizing child behavior problems were present in 18.9% of the study population. They were more common in boys than girls (29.0% vs. 13.9%, p=0.05) and in children of non-Hispanic ethnicity (24.5% vs. 5.8%, p<0.01). Caregiver report of more severe IPV at baseline (such as being choked, beaten, or threatened with a knife or gun) was associated with increased prevalence of internalizing child behavior problems (26.9% vs. 14.0%, p=0.08).
Externalizing child behavior problems were present in 32.3% of the population, and were more common in white children (39.4% vs. 25.1%, p=0.09) and in children with depressed caregivers at baseline (46.4% vs. 23.2%, p=0.02). Children with caregivers aged 30–39 had more externalizing behavior problems than those with either younger or older caregivers (46.6% vs. 15.0% and 27.7%, respectively, p=0.07). Finally, children with prior CPS investigations were more likely to have baseline externalizing behavior problems than those with no prior investigation (69.6% vs. 43.3%, p=0.02).
Baseline internalizing or externalizing behavior problems were similar for children with resolved vs. persistent IPV(20.0% vs. 26.3%, p=0.47; 37.9% vs. 32.5%, p=0.64). The presence of internalizing or externalizing behavior problems at baseline significantly predicted the same behavior problem at each subsequent wave (p<0.01 for all comparisons).
Multivariable models
We developed two multivariable logistic regression models to describe the pattern of internalizing or externalizing behavior problems at each survey timepoint based on the pattern of IPV exposure after CPS investigation. Baseline covariates associated with IPV persistence (child age and ethnicity; caregiver partner status and substance abuse) or child behavior problems (child sex, caregiver age, caregiver depression, IPV severity, and baseline behavior problems) were included in each model. Adjusted probabilities and ARR were calculated for each outcome over time(Table 2).
Table 2.
Adjusted probability (%) and adjusted risk ratio (ARR) for clinically significant child behavior problem based on persistence of caregiver reported IPV*
| Months since CPS investigation | |||||
|---|---|---|---|---|---|
| 3 | 20 | 36 | 81 | ||
| Internalizing behavior problem | Persistent IPV % (95%CI) | 21.6 (11.4, 31.8) | 24.2 (13.9, 34.5) | 22.8 (12.3, 33.4) | 24.4 (13.4, 35.4) |
| Resolved IPV % (95%CI) | 25.5 (15.5, 35.5) | 20.9 (5.1, 36.6) | 17.2 (5.5, 28.8) | 13.6 (3.7, 23.5) | |
| Risk ratio (95%CI) | 0.84 (0.61, 1.18) | 1.16 (0.61, 2.19) | 1.33 (0.74, 2.39) | 1.79 (0.91, 3.52) | |
| Externalizing behavior problem | Persistent IPV % (95%CI) | 35.1 (22.5, 47.7) | 37.3 (25.0, 49.6) | 39.6 (25.4, 53.8) | 45.2 (31.8, 58.7) |
| Resolved IPV % (95%CI) | 39.2 (25.3, 53.1) | 20.7 (10.0, 31.5) | 23.0 (12.0, 34.0) | 24.0 (10.3, 37.7) | |
| Risk ratio (95%CI) | 0.89 (0.75, 1.07) | 1.80 (1.15, 2.80) | 1.72 (1.10, 2.68) | 1.88 (1.11, 3.18) | |
Bolded probabilities reflect significant difference from baseline probability (p<0.05)
Bolded risk ratios reflect elevated risk of behavior problems in children exposed to persistent IPV (95% CI does not cross 1.0)
all results adjusted for baseline measures of child age, sex, minority race and ethnicity; caregiver age, partner status, depression and substance abuse; prior CPS investigations, IPV severity and pre-existing internalizing or externalizing child behavior problems.
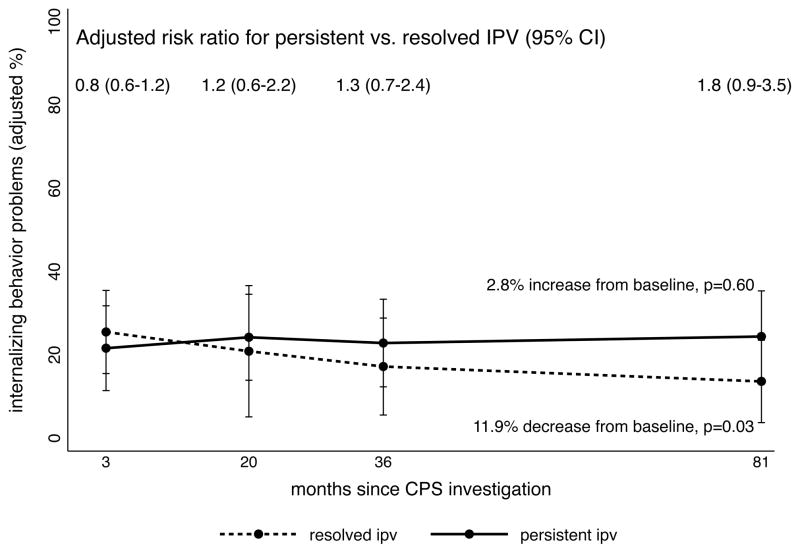
Eighty-one months after CPS involvement, children living with caregivers reporting IPV resolution had a significant reduction in the adjusted probability of internalizing child behavior problems (−11.9%, p=0.03) (figure 1). In contrast, children living with caregivers reporting persistence of IPV had persistence in internalizing behavior problems (+2.8%, p=0.6). At 81 months, the ARR for internalizing behavior problems of children with persistent vs. resolved IPV was 1.79 (95%CI 0.91, 3.52).
Figure 1.
Adjusted probability (%) and adjusted risk ratios (ARR) of clinically significant internalizing child behavior problems after a CPS investigation for suspected child maltreatment among children with and without persistence of caregiver-reported IPV
Significant reduction in the adjusted probability of externalizing behavior problems associated with IPV resolution was seen by 20 months (−18.5%, p<0.01)after CPS involvement in the home (figure 2). This reduction was sustained at 36 and 81 months (−16.2% and −15.2%, all p<0.05). Persistence of IPV was associated with persistence of externalizing behavior problems at 20(+2.2%, p=0.42) and 36 months (+4.5%, p=0.24) after CPS involvement, and with a non-significant increase after 81 months (+10.1%, p=0.07). ARR for externalizing behavior problems in children with persistent vs. resolved IPV was 1.80 (95% CI 1.15, 2.80), 1.72 (95% CI 1.10, 2.68) and 1.88 (95% CI 1.12, 3.18) at 20, 36, and 81 months following CPS involvement, respectively.
Figure 2.
Adjusted probability (%) and adjusted risk ratio (ARR) of clinically significant externalizing child behavior problems after a CPS investigation for suspected child maltreatment among children with and without persistence of caregiver-reported IPV
Resources and referrals associated with IPV resolution
At baseline, 291 of 320 caseworkers in our study sample were asked about any services that they provided, arranged for, or referred caregivers to as part of CPS involvement in the home. Although all caregivers in the study sample reported recent IPV in the baseline NSCAW survey, only 11.5% were referred to IPV services by caseworkers. One-quarter (25.9%)of caregivers were referred to mental health services by caseworkers. Caregivers with resolved IPV were more likely to have been referred for IPV services (17.4% vs. 6.0%, p=0.01) or mental health services (39.2% vs. 12.7%, p<0.001) by CPS caseworkers. Although caregiver utilization of IPV services after CPS involvement was more common among women with IPV resolution, this difference was not statistically significant (23.0% vs. 14.3%, p=0.3). Accessing mental health services was significantly more common among caregivers with IPV resolution (15.0% vs. 4.4%, p=0.02).
Comment
Over the past 2 decades, researchers have described negative long-term physical and behavioral outcomes associated with a range of adverse childhood experiences.22–26 Repeated studies have identified behavioral problems seen in children exposed to both child maltreatment and IPV.6,7,9,10 This study finds that children with recent exposure to both suspected child maltreatment and IPV have high rates of serious behavioral problems, and that resolution of IPV is associated with a clinically and statistically significant reduction in the prevalence of these behavioral problems over time. To our knowledge, this is the first study to examine the reversibility of outcomes associated with adverse experiences in childhood without explicit mental health interventions.
Our results are consistent with prior research suggesting that a CPS investigation does not routinely result in referrals to or engagement with needed services.27–29 In this nationally representative sample, just12% of women identifying recent IPV in the home were referred for IPV services; only 26% were referred for mental health services. It is important to note, however, that women who received referrals and women who accessed services were more likely to report resolution of IPV over time.
In contrast with prior research in a general medical setting, our results support broad screening and referral for IPV in households with a history of CPS involvement.13,30 Pediatricians working with these high-risk families may be able to support long-term improvements for children exposed to violence and abuse by providing caregivers with information and resources that promote violence-free homes. Collaboration with community mental health providers and IPV resources may strengthen these efforts.
The findings presented must be interpreted in the context of important limitations. As a retrospective analysis of a secondary database, we cannot assume a causal relationship between resolution of IPV and reduction in child behavior problems after CPS involvement in the home. We used multivariable modeling to adjust for recognized covariates significantly associated with our outcome and exposure variables, but acknowledge the possibility that unmeasured covariates may modify or explain the relationship between IPV resolution and child behavior problems.
Our results cannot be generalized to very young children involved with CPS or to children removed from the home during or after CPS involvement. Although prior research has described trauma symptoms in infants exposed to IPV, NSCAW does not have comparable measures of child behavior problems for children under 2 years of age at baseline.31 NSCAW interviewers did not measure IPV exposure in out-of-home settings, limiting our analysis to those children remaining in the home at all contact points. The experiences of these populations may be different from the population presented in this study.
The timing of the NSCAW surveys introduces limitations. Baseline interviews occurred an average of 3 months following CPS involvement and may not reflect the reality of a household at the time of CPS involvement. As such, our findings may be most relevant for pediatricians and other professionals who continue to work with families after CPS investigation. At subsequent interviews, caregivers were asked to report IPV for the 12 months prior to each interview, which may have resulted in misclassification of some children. It is likely that this misclassification would lead to an underestimate of the effects of IPV resolution on child behavior problems.
We relied upon caregiver-reported child behavior problems for our primary outcome. Although the parent-report CBCL is a common measure of behavior problems, prior research suggests that caregiver perception of behavior problems may be biased in the context of IPV.32 It is possible that the observed persistence of child behavior problems reflects, to some extent, caregiver distress in the setting of ongoing IPV. Future studies should include both child self-report and outside observations to confirm these findings. Despite this limitation, maternal perception of a child’s behavior problems, biased or not, is a meaningful outcome for children living in these households.
Finally, we recognize that the NSCAW dataset does not reflect important changes to CPS policies that have occurred in the 12 years since these data were collected. Increased attention to the role of IPV in child and family outcomes has undoubtedly improved CPS identification and response to IPV during investigations for suspected child maltreatment.12,33 We believe that the primary findings of our study support these efforts.
Despite these limitations, we believe that this study has meaningful implications for professionals working with children and families. Researchers across disciplines must collaborate to evaluate the effectiveness and efficacy of interventions for families living within the intersecting worlds of child maltreatment and IPV. CPS caseworkers should continue to be encouraged to identify IPV during CPS investigations, and supported in efforts to provide referrals and services to caregivers reporting a history of IPV.12 Finally, pediatricians must recognize the potential to improve outcomes for children with a history of CPS involvement and play an active role in providing education and resources to these high-risk families.
Supplementary Material
Acknowledgments
The NSCAW data were made available by the National Data Archive on Child Abuse and Neglect, Cornell University, Ithaca, NY and are used with Archive permission. Dr. Campbell had full access to the data and takes responsibility for the accuracy of the data analysis.
Footnotes
FINANCIAL DISCLOSURE: Dr. Campbell is supported by a Mentored Career Development Award (5K23HD59850) from the NICHD.
Contributor Information
Kristine A. Campbell, University of Utah, Department of Pediatrics, Intermountain Injury Control and Research Center, PO Box 581289, 295 Chipeta Way, Salt Lake City, UT 84158.
Andrea M. Thomas, University of Utah, Department of Pediatrics.
Lawrence J. Cook, University of Utah, Department of Pediatrics.
Heather T. Keenan, University of Utah, Department of Pediatrics.
References
- 1.Black MC, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. National Center for Injury Prevention and Control, National Center for Disease Control and Prevention; Atlanta, GA: 2011. [Google Scholar]
- 2.Finkelhor D, Turner H, Ormrod R, Hamby SL. Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics. 2009 Nov;124(5):1411–1423. doi: 10.1542/peds.2009-0467. [DOI] [PubMed] [Google Scholar]
- 3.Hazen AL, Connelly CD, Kelleher KJ, Barth RP, Landsverk JA. Female caregivers’ experiences with intimate partner violence and behavior problems in children investigated as victims of maltreatment. Pediatrics. 2006 Jan;117(1):99–109. doi: 10.1542/peds.2004-2542. [DOI] [PubMed] [Google Scholar]
- 4.Hamby S, Finkelhor D, Turner H, Ormrod R. The overlap of witnessing partner violence with child maltreatment and other victimizations in a nationally representative survey of youth. Child Abuse Negl. 2010 Oct;34(10):734–741. doi: 10.1016/j.chiabu.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Bair-Merritt MH, Blackstone M, Feudtner C. Physical health outcomes of childhood exposure to intimate partner violence: a systematic review. Pediatrics. 2006 Feb;117(2):e278–290. doi: 10.1542/peds.2005-1473. [DOI] [PubMed] [Google Scholar]
- 6.Evans SE, Davies C, DiLillo D. Exposure to domestic violence: A meta-analysis of child and adolescent outcomes. Aggression & Violent Behavior. 2008;13(2):131–140. [Google Scholar]
- 7.Kitzmann KM, Gaylord NK, Holt AR, Kenny ED. Child witnesses to domestic violence: a meta-analytic review. J Consult Clin Psychol. 2003 Apr;71(2):339–352. doi: 10.1037/0022-006x.71.2.339. [DOI] [PubMed] [Google Scholar]
- 8.Rivara FP, Anderson ML, Fishman P, et al. Intimate partner violence and health care costs and utilization for children living in the home. Pediatrics. 2007 Dec;120(6):1270–1277. doi: 10.1542/peds.2007-1148. [DOI] [PubMed] [Google Scholar]
- 9.Sternberg KJ, Baradaran LP, Abbott CB, Lamb ME, Guterman E. Type of violence, age, and gender differences in the effects of family violence on children’s behavior problems: A mega-analysis. Developmental Review. 2006;26(1):89–112. [Google Scholar]
- 10.Kernic MA, Wolf ME, Holt VL, McKnight B, Huebner CE, Rivara FP. Behavioral problems among children whose mothers are abused by an intimate partner. Child Abuse Negl. 2003 Nov;27(11):1231–1246. doi: 10.1016/j.chiabu.2002.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Bair-Merritt MH. Intimate partner violence. Pediatr Rev. 2010 Apr;31(4):145–150. doi: 10.1542/pir.31-4-145. quiz 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Banks D, Landsverk J, Wang K. Changing policy and practice in the child welfare system through collaborative efforts to identify and respond effectively to family violence. J Interpers Violence. 2008 Jul;23(7):903–932. doi: 10.1177/0886260508314693. [DOI] [PubMed] [Google Scholar]
- 13.Nygren P, Nelson HD, Klein J. Screening children for family violence: a review of the evidence for the US Preventive Services Task Force. Ann Fam Med. 2004 Mar-Apr;2(2):161–169. doi: 10.1370/afm.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thackeray JD, Hibbard R, Dowd MD. Intimate partner violence: the role of the pediatrician. Pediatrics. 2010 May;125(5):1094–1100. doi: 10.1542/peds.2010-0451. [DOI] [PubMed] [Google Scholar]
- 15.Dowd KL, Kinsey S, Wheeless S, et al. National Survey of Child Abuse and Adolescent Well- Being (Combined Waves 1–5): Data File User’s Manual (Restricted Release Version) National Data Archive on Child Abuse and Neglect (Ithaca, NY) 2008 [Google Scholar]
- 16.National Survey of Child Abuse and Neglect. CPS Sample Component. Administration for Children and Families, Department of Health and Human Services; 2005. ( http://www.acf.hhs.gov/programs/opre/abuse_neglect/nscaw/reports/cps_sample/cps_report_revised_090105.pdf.) [Google Scholar]
- 17.Biemer P, Christ S, Wheeless S, et al. National Survey of Child Abuse and Adolescent Well- Being: Statistical Analysis Manual. National Data Archive on Child Abuse and Neglect (Ithaca, NY) 2005 [Google Scholar]
- 18.Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 19.Achenbach TM. Manual for the Child Behavior Checklist/2–3. Burlington, VT: University of Vermont Department of Psychiatry; 1992. [Google Scholar]
- 20.Stata Quick Reference and Index: Release 12. College Station, TX: Stata Press; 2011. Marginal means, predictive margins, and marginal effects; pp. 1027–79. [Google Scholar]
- 21.Cummings P. Estimating adjusted risk ratios for matched and unmatched data: An update. The Stata Journal. 2011;11(2):290–298. [Google Scholar]
- 22.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998 May;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 23.Flaherty EG, Thompson R, Litrownik AJ, et al. Effect of early childhood adversity on child health. Arch Pediatr Adolesc Med. 2006 Dec;160(12):1232–1238. doi: 10.1001/archpedi.160.12.1232. [DOI] [PubMed] [Google Scholar]
- 24.Bonomi AE, Anderson ML, Rivara FP, et al. Health care utilization and costs associated with childhood abuse. J Gen Intern Med. 2008 Mar;23(3):294–299. doi: 10.1007/s11606-008-0516-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chartier MJ, Walker JR, Naimark B. Childhood abuse, adult health, and health care utilization: results from a representative community sample. Am J Epidemiol. 2007 May;165(9):1031–1038. doi: 10.1093/aje/kwk113. [DOI] [PubMed] [Google Scholar]
- 26.MacMillan HL, Fleming JE, Streiner DL, et al. Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiatry. 2001 Nov;158(11):1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- 27.Campbell KA, Thomas AM, Cook LJ, Keenan HT. Longitudinal Experiences of Children Remaining at Home after a First-Time Investigation for Suspected Maltreatment. J Pediatr. 2012 Aug;161(2):340–347. doi: 10.1016/j.jpeds.2012.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hazen AL, Connelly CD, Edleson JL, et al. Assessment of intimate partner violence by child welfare services. Child Youth Serv Rev. 2007 Apr;29(4):490–500. doi: 10.1016/j.childyouth.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hurlburt MS, Leslie LK, Landsverk J, et al. Contextual predictors of mental health service use among children open to child welfare. Arch Gen Psychiatry. 2004 Dec;61(12):1217–1224. doi: 10.1001/archpsyc.61.12.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacMillan HL, Wathen CN, Jamieson E, et al. Screening for intimate partner violence in health care settings: a randomized trial. JAMA. 2009 Aug 5;302(5):493–501. doi: 10.1001/jama.2009.1089. [DOI] [PubMed] [Google Scholar]
- 31.Bogat GA, DeJonghe E, Levendosky AA, Davidson WS, von Eye A. Trauma symptoms among infants exposed to intimate partner violence. Child Abuse Negl. 2006 Feb;30(2):109–125. doi: 10.1016/j.chiabu.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Clements CM, Oxtoby C, Ogle RL. Methodological issues in assessing psychological adjustment in child witnesses of intimate partner violence. Trauma Violence Abuse. 2008 Apr;9(2):114–127. doi: 10.1177/1524838008315870. [DOI] [PubMed] [Google Scholar]
- 33.Hazen AL, Connelly CD, Kelleher KJ, Landsverk JA, Barth RP. Intimate partner violence in the child welfare system: Findings from the National Survey of Child and Adolescent Well-Being. In: Haskins R, Wulczyn F, Webb MB, editors. Child protection: Using research to improve policy and protection. Washington, D.C: The Brookings Institute; 2007. pp. 44–61. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.