Abstract
Purpose
In recent years, patient-specific instruments (PSI) has been introduced with the aim of reducing the overall costs of the implants, minimising the size and number of instruments required, and also reducing surgery time. The purpose of this study was to perform a review of the current literature, as well as to report about our personal experience, to assess reliability of patient specific instrument system in total knee arthroplasty (TKA).
Methods
A literature review was conducted of PSI system reviewing articles related to coronal alignment, clinical knee and function scores, cost, patient satisfaction and complications.
Results
Studies have reported incidences of coronal alignment ≥3° from neutral in TKAs performed with patient-specific cutting guides ranging from 6 % to 31 %.
Conclusions
PSI seem not to be able to result in the same degree of accuracy as the CAS system, while comparing well with standard manual technique with respect to component positioning and overall lower axis, in particular in the sagittal plane. In cases in which custom-made cutting jigs were used, we recommend performing an accurate control of the alignment before and after any cuts and in any further step of the procedure, in order to avoid possible outliers.
Keywords: Patient-specific instrument, TKA, Computer-assisted surgery
Introduction
Total knee arthroplasty (TKA) is one of the most successful orthopaedics procedures, restoring a significant degree of function in arthritic knees in most cases. However, errors in surgical technique and component placement can compromise the long-term performance [1]. It has been proven that one of the most important factors influencing the longevity of implants in TKA is the restoration of mechanical axis, as deviations of greater than 3° of varus/valgus in the mechanical axis lead to poor survivorship because of the accelerated wear as a result of abnormal stresses at the bearing surfaces [2].
The use of computer-assisted surgery (CAS) in TKA results in better coronal alignment of the leg and the implants compared to TKA performed using the standard technique [3].
However, the majority of published studies have not found statistically significant differences between CAS and conventional TKA based on the Knee Society score (KSS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) or University of California Los Angeles activity score (UCLA). Only one prospective study [4] reported better five-year KSS results in the CAS TKA group.
Moreover, the duration of surgery performed with computer navigation was significantly longer. This is due in part to the surgical technique which requires the placement of the reference arrays, digitization of the knee, and waiting for the computer to work out the algorithms [5].
On the other hand, in recent years, patient-specific instruments (PSI) have been introduced with the aim to reduce the overall costs of the implants, minimising the size and number of instruments required, and also reducing surgery time. PSI uses anatomical data, as detected by pre-operative axial computed tomography (CT) or magnetic resonance imaging (MRI), to create disposable cutting jigs individualized to the patient’s unique anatomy. However, previous studies [6, 7] documented only a fair accuracy of the method with a consistent risk of error of more than 2°, especially in the sagittal plane.
The purpose of this study was to perform a review of the current literature, as well as to report about our personal experience, to assess reliability of a patient-specific instrument system in TKA.
Patient-specific instruments (PSI)
Patient-specific instruments (PSI) were recently introduced as a new technology, to pursue the same goal of navigation in increasing the accuracy of the surgical technique, and avoiding the practical issues related to the complexity of the CAS, such as the costs, surgical time and learning curve related to the procedure.
Pre-operative planning of the TKA procedure is outsourced to engineers who identify the anatomical landmarks needed for component alignment on CT/MRI based 3D models, therefore transferring the information to patient-specific instruments that can be used during surgery. These instruments, created by laser sintering, can be produced in the most complex forms and are thus patient specific [8]. This technology gained widespread acceptance in dental surgery and was gradually introduced in TKA. Using a pre-operative CT or MRI scan, disposable cutting blocks are produced.
Thienpont et al. [9] showed that the total volume of PSI in Europe for 2012 was 17,515 TKAs and 82,556 worldwide. The seven companies which provided PSI are, by alphabetical order, Biomet (Warsaw, USA), DuPuy-Synthes (Warsaw, USA), Medacta (Castel San Pietro, Switzerland), Smith & Nephew (Memphis, USA), Stryker (Mahwah, USA), Wright Medical (Memphis, USA) and Zimmer (Warsaw, USA). Biomet was the number one in volume, both in Europe and worldwide with their Signature system. Biomet represented 27 % of the market share in PSI worldwide.
Our experience
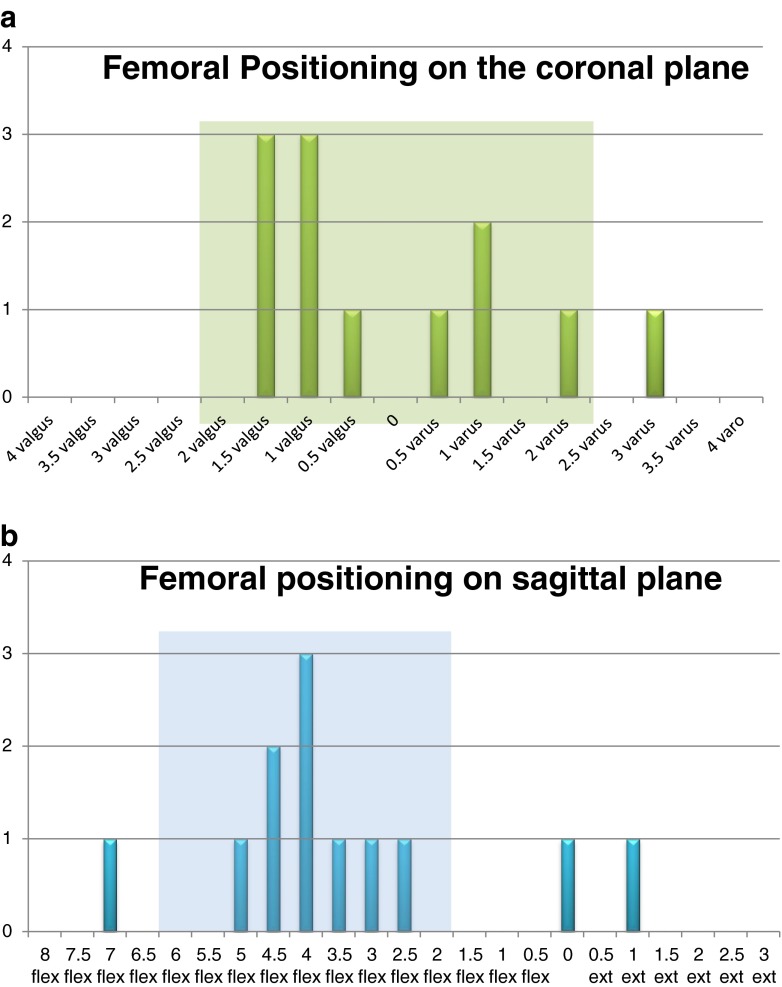
We started using PSI in 2011 after a consistent experience with navigation in TKA [6, 7, 10–12]. In a recent study [7] we evaluated the accuracy of a patient-specific instrumentation as assessed by the intra-operative use of knee navigation software during the surgical procedure. Ten satisfactory alignments (83.3 %) were obtained on the tibial coronal plane. A correct alignment was achieved on the tibial sagittal plane in five patients only (41.6 %). On the femur, a correct alignment was obtained for 11 measurements (92.6 %) in the coronal plane and in 9 (71 %) in the sagittal plane.
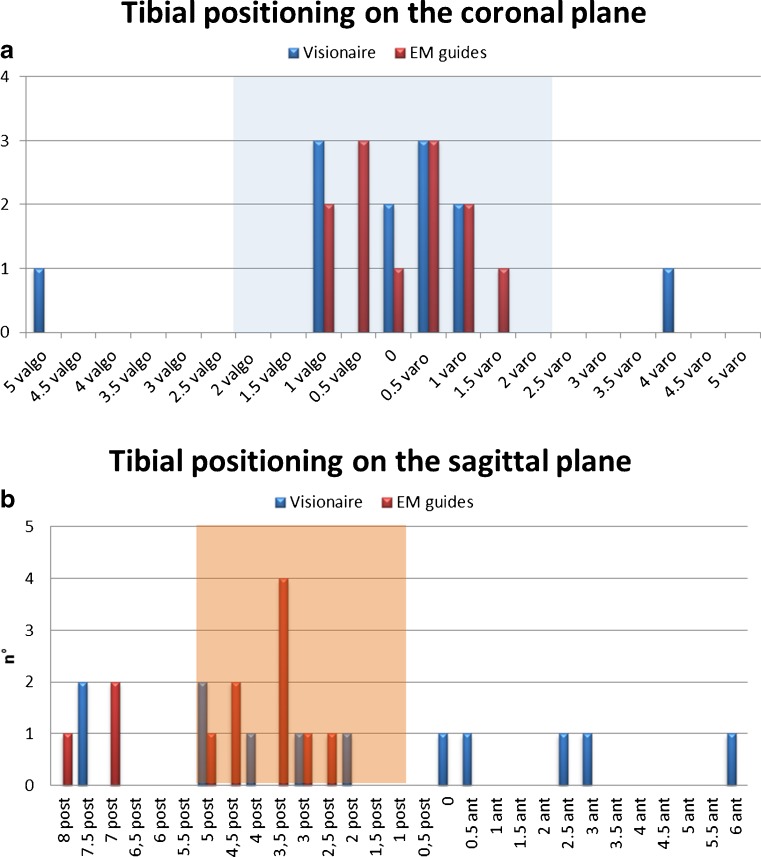
We also evaluated the accuracy of VISIONAIRE (Smith & Nephew Inc., Memphis, TN, USA) in comparison with extra-medullary (EM) tibial instrumentation by analysing data as detected by intra-operative use of knee navigation software. In the coronal plane the mean deviation of the EM tibial guides from the ideal alignment (0°) was 0.7° ± 0.39 and of the VISIONAIRE was 129° ± 1.55 (P = 0.22). In the sagittal plane the mean deviation of the EM tibial guides from 3° of posterior slope was −1.62° ± 1.78° and of the VISIONAIRE was +1.16° ± 4.29 (P < 0.05). Negative values indicate a more posterior slope from the ideal and positive values an anterior slope [6]. All data are shown in Figs. 1 and 2.
Fig. 1.
a EM guide vs VISIONAIRE on the coronal plane. b EM guide vs VISIONAIRE on the sagittal plane
Fig. 2.
a The alignment on the coronal femoral plane. b Alignment on the sagittal femoral plane
These studies documented only a fair accuracy of the method with a consistent risk of error of more of 3° especially in the sagittal plane. We could speculate that the problem in the sagittal plane was due to the fact that the pre-operative protocol does not include a lateral X-ray projection of the knee and only includes an AP standing X-ray of the straight leg and MRI.
Discussion
The peer-reviewed literature on PSI is still limited with only a few high-quality studies available. The initial papers by early adopters of the technology were globally showing a mean mechanical axis comparable to conventional surgery with a lower rate of outliers in the coronal plane, but without significant difference [8, 13]. Subsequently, a few retrospective studies about a MRI-based system [6, 7], and a recent randomized controlled trial, where different PSI systems were controlled with navigation during surgery, did not show convincing evidence for three-plane alignment superiority for PSI in comparison with the standard technique [8].
Previous studies have reported incidences of coronal alignment ≥3° from neutral in TKAs performed with patient-specific cutting guides ranging from 6 % [14] to 31 % [15] (Table 1). Moreover, the PSI system did not demonstrate a marked improvement in the incidence of outliers in final coronal alignment, comparing poorly with computer-assisted navigation (9 %), with rates of outliers to technique (31.8 %) [29].
Table 1.
Comparative studies for patient-specific instruments (PSI) assessments
| Study | Patient | System | Implant | Method | HKA | CTA | CFA | STA | SFA |
|---|---|---|---|---|---|---|---|---|---|
| Nam et al. [16] 2013 | 41 | Signature Biomet (MRI) | Vanguard Complete Knee System (Biomet) | X-rays | 0.8° ± 2.9° 29.3 % outliers |
0.4° ± 1.6° 12.8 % outliers |
0.1° ± 1.5° 9.8 % outliers |
NA | NA |
| Chen et al. [15] 2013 | 29 | Zimmer PSI system (MRI) | Zimmer Nexgen LPS system | X-rays | 179.2 ± 3.4 Nine outliers (31 %) |
89.8 ± 1.9 Three outliers (10 %) |
89.9 ± 2.1 Two outliers (7 %) |
84.2 ± 3.4 Seven outliers (24 %) |
87.7 ± 2.6 Seven outliers (24 %) |
| Boonen et. al [17] 2013 | 45 | Signature Biomet (MRI) | Vanguard Complete Knee System (Biomet) | X-rays | 179° ± 2.8 30 % outliers |
90° ± 2.0 9 % outliers |
89° ± 2.1 13 % outliers |
92° ± 3.2 33 % outliers |
96° ± 5 49 % outliers |
| Parratte et al. [18] 2013 | 20 | Zimmer PSI system (MRI) | Zimmer Nexgen LPS system | X-rays | 179° (171–185) 4 outliers (20 %) |
89.1 (85–96) | 90.1 (84–83) | 5.9 (3–9) | 8.15 (2–14) |
| Pietsch et al. [14] 2013 | 50 | Zimmer PSI system (MRI) | Zimmer Nexgen LPS system | X-rays | 3 outliers (6 %) |
4 outliers (8 %) |
5 outliers (10 %) |
3 outliers (6 %) |
3 outliers (6 %) |
| Daniilidis et al. [19] 2013 | 150 | Visionaire PSI Smith&Nephew (MRI) | Genesis II (Smith and Nephew) | X-rays | 178.4 ± 1.5 14 outliers (9.3 %) |
NA | NA | NA | NA |
| Vundelinckx et al. [20] 2013 | 31 | Visionaire PSI Smith&Nephew (MRI) | Genesis II (Smith and Nephew) | X-rays | 183 ± 2.59 | NA | NA | NA | NA |
| Koch et al. [21] 2013 | 301 | MyKnee Medacta (CT) | GMK (Medacta) | X-rays | 180.1° ± 2.0 34 outliers (11.7 %) |
11 outliers (3.8 %) | 13 outliers (4.5 %) | 37 outliers (12.3 %) | 27 outliers (9 %) |
| Scholes et al. [22] 2013 | 30 | Zimmer PSI system (MRI) | Zimmer Nexgen LPS system | Nav | 179.5° 8 outliers (27 %) |
NA | NA | NA | NA |
| Lustig et al. [23] 2013 | 60 | Visionaire Smith&Nephew (MRI) | Genesis II (S&N) | Nav | 179.8 20.9 % outliers |
NA | NA | NA | NA |
| Daniilidis et al. [24] 2012 | 124 | Visionaire Smith&Nephew (MRI) | Genesis II (Smith and Nephew) | X-rays | 178.5 ± 1.7 11 outliers (11 %) |
NA | NA | NA | NA |
| Bali et al. [13] 2012 | 32 | Visionaire Smith&Nephew (MRI) | Genesis II (Smith and Nephew) | X-rays | 179.9 3 outliers (9.4 %) |
NA | NA | NA | NA |
| Boonen et al. [25] 2012 | 38 | Signature Biomet (MRI) | Vanguard Complete Knee System (Biomet) | X-rays | 181° ± 4 11 outliers (29 %) |
91° ± 2 7 outliers (18 %) |
90° ± 2 2 outliers (5 %) |
94° ± 4 14 outliers (37 %) |
85° ± 4 16 outliers (42 %) |
| Ng et al. [26] 2012 | 569 | Signature Biomet (MRI) | Vanguard Complete Knee System (Biomet) | X-rays | 180.6° 9 % outliers |
89.9° 10 % outliers |
90.7° 22 % outliers |
NA | NA |
| Conteduca et al. [7] 2012 | 12 | Visionaire Smith&Nephew (MRI) | Journey BCS (S&N) | Nav | NA | 1.2° ± 1.5 2 outliers (16 %) |
1.2° ± 0.6 2 outliers (16 %) |
3.8° ± 2.4 9 outliers (75 %) |
+0.5° ± 2.15 3 outliers (25 %) |
| Noble et al. [27] 2012 | 15 | Visionaire Smith&Nephew (MRI) | Legion Total Knee System (Smith & Nephew) | X-rays | 181.7 | NA | NA | NA | NA |
| Nunley et al. [28] 2012 | 57 | Vanguard total knee system (Biomet) (MRI) | Signature system (Biomet) | CT-scan | 26 % outliers | NA | NA | NA | NA |
HKA hip-knee-ankle angle, CTA coronal tibial angle, CFA coronal femoral angle, STA sagittal tibial angle, SFA sagittal femoral angle
Bali et al. [13] shared their initial experience with use of PSI in 32 TKAs. At six weeks, long-leg radiographs were obtained to evaluate the coronal alignment and 29 of the 32 knees (90.6 %) had a mechanical axis restored to within 3° of neutral. The authors concluded that the custom-fit system in TKA was found to be as accurate in restoring the postoperative alignment as the standard TKA.
Noble et al. [27] compared the value of the new mechanically aligned patient-matched instrument system for total knee arthroplasty to that of standard TKA surgical instrumentation. Mechanical alignment was significantly closer to neutral zero in the PSI group (1.7°, range 0°–6° vs 2.8°, range 0°–5°). The results of the this randomized study support the value of patient-matched cutting blocks. However, this study is only representative of one surgeon's experience.
Nam et al. [16] compared the alignment accuracy of PSI to an imageless CAS system in TKA. In the PSI cohort, 70.7 % of patients had an overall alignment within 3° of a neutral mechanical axis (vs. 92.7 % with CAS), 87.8 % had a tibial component alignment within 2° of perpendicular to the tibial mechanical axis (vs. 100 % with CAS), and 90.2 % had a femoral component alignment within 2° of perpendicular to the femoral mechanical axis (vs. 100 % with CAS). The author concluded that, while PSI techniques appear sound in principle, this system did not obtain the same degree of overall mechanical and tibial component alignment accuracy as a CAS technique.
Daniilidis et al. [19] determined whether PSI would lead to a hip-knee-ankle (HKA) angle within ±3° of the ideal alignment of 180°. The average HKA changed from 173.7° ± 3.9 pre-operatively to 178.4 °± 1.5° postoperatively. The rate of ±3° and ±5° HKA outliers was 11 % and 3 %, respectively. On the basis of their data, authors showed that these results also reconfirm the conclusion that this specific technology is effective in addressing the issue of malalignment.
Ng et al. [26] compared the effectiveness of MRI-based patient-specific positioning guides to manual instrumentation with intramedullary femoral and extra-medullary tibial guides in restoring the mechanical axis of the extremity and achieving neutral coronal alignment of the femoral and tibial components. The overall mean HKA angle for patient-specific positioning guides (180.6°) was similar to manual instrumentation (181.1°), but there were statistically fewer ± 3° HKA angle outliers with patient-specific positioning guides (9 %) than with manual instrumentation (22 %).
By our knowledge there is only one study which analysed the CT-based system. Koch et al. [21] showed that the postoperative average HKA angle of a CT-based system was 180.1° ± 2.0°. In the frontal plane a total of 12.4 % of outliers >3°, for the tibial components 4.1 % of outliers >3° and for the femoral components 4.8 % of outliers >3° were measured. Comparing the outcome of this study with the data from the literature [29], there does not seem to be any difference compared to computer-assisted surgery.
Based on these studies we could speculate that the MRI-based PSI system was not able to obtain the same degree of accuracy as the CAS system, with respect to both the tibial component and overall lower extremity axis in particular in the sagittal plane. While the mean values are comparable to most reports of TKAs performed using conventional intramedullary and extra-medullary alignment methods, it falls far below the accuracy reported with CAS techniques [29]. However in most cases the authors failed to report about revision cuts performed during surgery to correct possible misalignment related to inaccuracy of the guided cut.
Moreover these studies only evaluated the alignment in the coronal plane, not considering possible malposition in the sagittal plane that may play a significant role in the maximal post-operative flexion and in the polyethylene wear.
Another limitation of previous studies is that the accuracy of the PSI was evaluated using post-operative X-rays, whose data can be influenced by several factors other than accuracy of the cutting guide (sawing errors, cut adjustment, final impaction technique). Computer navigation provides the only real-time method for assessing alignment of the system and to our knowledge only few studies [6, 7, 22, 23, 30] used this to evaluate the PSI.
Lustig et al. [23] used intra-operative computer navigation to evaluate the accuracy of the cutting blocks in the coronal and sagittal planes. The PSI would have placed 79.3 % of the sample within ±3° of the pre-operative plan in the coronal plane, while the sagittal alignment results within ±3° were 54.5 %. Their results are very similar to the data previously reported by us [6, 7].
Even more disappointing were the results of Klatt et al. [30] who used an image-free computer navigation system to evaluate the alignment of the components that was more than 3° off of the mechanical axis in all cases. On the basis of their data, the author showed that the custom cutting jigs have the potential to place the components outside of the accepted range of alignment and even place the components out of the accepted alignment range.
In a similar study Scholes et al. [22] assessed reliability of PSI in TKA using imageless computer navigation. The error between in-theatre measurements and pre-operative plan for the femoral and tibial components exceeded 3° for 3 % and 17 % of the sample, respectively, while the error for total coronal alignment exceeded 3° for 27 % of the sample. The authors concluded that alignment with PSI patient-specific cutting guides, assessed by computer navigation, is not accurate. To prevent unnecessary increases in the incidence of malalignment in TKA, it is recommended that these devices should not be used without verification of alignment.
Conclusion
Patient specific instruments have been introduced to reduce the surgical time and the overall costs of the implants, minimising the size and number of instruments required. However, current PSI seem not to be able to result in the same degree of accuracy as for the CAS system, while comparing well with standard manual techniques with respect to component positioning and overall lower axis, in particular in the sagittal plane.
Nowadays, in cases in which custom-made cutting jigs were used, we recommend performing an accurate control of the alignment before and after any cuts and in any further step of the procedure, in order to avoid possible outliers.
Therefore even if PSI appears as a promising technology, their accuracy could still be improved, possibly leading to greater reliability.
References
- 1.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73(5):709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 2.Perillo-Marcone A, Barrett DS, Taylor M. The importance of tibial alignment: finite element analysis of tibial malalignment. J Arthroplasty. 2000;15(8):1020–1027. doi: 10.1054/arth.2000.17941. [DOI] [PubMed] [Google Scholar]
- 3.Lützner J, Dexel J, Kirschner S. No difference between computer-assisted and conventional total knee arthroplasty: five-year results of a prospective randomised study. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2241–2247. doi: 10.1007/s00167-013-2608-7. [DOI] [PubMed] [Google Scholar]
- 4.Hoffart HE, Langenstein E, Vasak N. A prospective study comparing the functional outcome of computer-assisted and conventional total knee replacement. J Bone Joint Surg Br. 2012;94(2):194–199. doi: 10.1302/0301-620X.94B2.27454. [DOI] [PubMed] [Google Scholar]
- 5.Chin PL, Yang KY, Yeo SJ, Lo NN. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20(5):618–626. doi: 10.1016/j.arth.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A. Are MRI-based, patient matched cutting jigs as accurate as the tibial guides? Int Orthop. 2012;36(8):1589–1593. doi: 10.1007/s00264-012-1522-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A. Evaluation of the accuracy of a patient-specific instrumentation by navigation. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2194–2199. doi: 10.1007/s00167-012-2098-z. [DOI] [PubMed] [Google Scholar]
- 8.Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J (2013) Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res. 2013 Apr 25. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 9.Thienpont E, Bellemans J, Delport H, Van Overschelde P, Stuyts B, Brabants K, Victor J. Patient-specific instruments: industry's innovation with a surgeon's interest. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2227–2233. doi: 10.1007/s00167-013-2626-5. [DOI] [PubMed] [Google Scholar]
- 10.Conteduca F, Massai F, Iorio R, Zanzotto E, Luzon D, Ferretti A. Blood loss in computer-assisted mobile bearing total knee arthroplasty. A comparison of computer-assisted surgery with a conventional technique. Int Orthop. 2009;33(6):1609–1613. doi: 10.1007/s00264-008-0651-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iorio R, Bolle G, Conteduca F, Valeo L, Conteduca J, Mazza D, Ferretti A. Accuracy of manual instrumentation of tibial cutting guide in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2296–2300. doi: 10.1007/s00167-012-2005-7. [DOI] [PubMed] [Google Scholar]
- 12.Iorio R, Mazza D, Bolle G, Conteduca J, Redler A, Conteduca F, Ferretti A. Computer-assisted surgery: a teacher of TKAs. Knee. 2013;20(4):232–235. doi: 10.1016/j.knee.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 13.Bali K, Walker P, Bruce W. Custom-fit total knee arthroplasty: our initial experience in 32 knees. J Arthroplasty. 2012;27(6):1149–1154. doi: 10.1016/j.arth.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Pietsch M, Djahani O, Hochegger M, Plattner F, Hofmann S. Patient-specific total knee arthroplasty: the importance of planning by the surgeon. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2220–2226. doi: 10.1007/s00167-013-2624-7. [DOI] [PubMed] [Google Scholar]
- 15.Chen JY, Yeo SJ, Yew AK, Tay DK, Chia SL, Lo NN, Chin PL (2013) The radiological outcomes of patient-specific instrumentation versus conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013 Aug 31. [Epub ahead of print]. [DOI] [PubMed]
- 16.Nam D, Maher PA, Rebolledo BJ, Nawabi DH, McLawhorn AS, Pearle AD. Patient specific cutting guides versus an imageless, computer-assisted surgery system in total knee arthroplasty. Knee. 2013;20(4):263–267. doi: 10.1016/j.knee.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Boonen B, Schotanus MG, Kerens B, van der Weegen W, van Drumpt RA, Kort NP. Intra-operative results and radiological outcome of conventional and patient-specific surgery in total knee arthroplasty: a multicentre, randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2206–2212. doi: 10.1007/s00167-013-2620-y. [DOI] [PubMed] [Google Scholar]
- 18.Parratte S, Blanc G, Boussemart T, Ollivier M, Le Corroller T, Argenson JN. Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2213–2219. doi: 10.1007/s00167-013-2623-8. [DOI] [PubMed] [Google Scholar]
- 19.Daniilidis K, Tibesku CO (2013) A comparison of conventional and patient-specific instruments in total knee arthroplasty. Int Orthop. 2013 Jul 31. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 20.Vundelinckx BJ, Bruckers L, De Mulder K, De Schepper J, Van Esbroeck G. Functional and radiographic short-term outcome evaluation of the Visionaire system, a patient-matched instrumentation system for total knee arthroplasty. J Arthroplasty. 2013;28(6):964–970. doi: 10.1016/j.arth.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Koch PP, Müller D, Pisan M, Fucentese SF. Radiographic accuracy in TKA with a CT-based patient-specific cutting block technique. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2200–2205. doi: 10.1007/s00167-013-2625-6. [DOI] [PubMed] [Google Scholar]
- 22.Scholes C, Sahni V, Lustig S, Parker DA, Coolican MR (2013) Patient-specific instrumentation for total knee arthroplasty does not match the pre-operative plan as assessed by intra-operative computer-assisted navigation. Knee Surg Sports Traumatol Arthrosc. 2013 Sep 17. [Epub ahead of print] [DOI] [PubMed]
- 23.Lustig S, Scholes CJ, Oussedik S, Kinzel V, Coolican MR, Parker DA (2013) Unsatisfactory accuracy with VISIONAIRE patient-specific cutting jigs for total knee arthroplasty. J Arthroplasty. 2013 Jul 25. [Epub ahead of print] [DOI] [PubMed]
- 24.Daniilidis K, Tibesku CO. Frontal plane alignment after total knee arthroplasty using patient-specific instruments. Int Orthop. 2013;37(1):45–50. doi: 10.1007/s00264-012-1732-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boonen B, Schotanus MG, Kort NP. Preliminary experience with the patient-specific templating total knee arthroplasty. Acta Orthop. 2012;83(4):387–393. doi: 10.3109/17453674.2012.711700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV., Jr Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470(1):99–107. doi: 10.1007/s11999-011-1996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noble JW, Jr, Moore CA, Liu N. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty. 2012;27(1):153–155. doi: 10.1016/j.arth.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Nunley RM, Ellison BS, Ruh EL, Williams BM, Foreman K, Ford AD, Barrack RL. Are patient-specific cutting blocks cost-effective for total knee arthroplasty? Clin Orthop Relat Res. 2012;470(3):889–894. doi: 10.1007/s11999-011-2221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8):1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 30.Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty. 2008;23(1):26–29. doi: 10.1016/j.arth.2007.10.001. [DOI] [PubMed] [Google Scholar]