Abstract
Purpose
Evaluations for knee osteoarthritis (OA) or post-operative total knee arthroplasty (TKA) have mainly been assessed by objective scales. Though the Knee injury and Osteoarthritis Outcome Score (KOOS) is attracting attention as a patient-based outcome score, the relationship with conventional objective scales after TKA remains controversial. The purpose of this study was to investigate the relationship between KOOS and conventional objective scales and evaluate the features of patient-based outcome scores.
Methods
Subjects were 130 post-operative patients involving 186 knees treated with TKA. Their mean age was 74.0 ± 8.0 years, and the follow-up period was 43 months. Japanese Orthopaedic Association (JOA) score, original Knee Society Score (KSS) and surgeon’s satisfaction score were scored as conventional objective scales besides KOOS. Spearman’s correlation coefficient was estimated between these scales. Comparisons between OA and rheumatoid arthritis (RA) as well as primary and revision surgery were performed by the Mann–Whitney U test.
Results
There were strong correlations between KOOS activities of daily living (ADL) and JOA score (r = 0.806), KSS function score (r = 0.803) and between KOOS pain and KSS knee score (r = 0.689). However, there was a poor correlation between KOOS and surgeon’s satisfaction score (r = 0.188-0.321). TKA for RA showed poorer results only in KOOS pain (p = 0.003), and revision surgery showed poorer results in KSS function, KOOS symptoms and KOOS quality of life (QOL).
Conclusions
This study suggested that conventional objective scales reflected mainly ADL disturbances in post-operative TKA patients. Furthermore, patient-based outcome scores made it possible to evaluate and detect a minute change of knee pain and QOL in TKA patients. The Japanese KOOS was a useful tool to evaluate conditions after TKA.
Keywords: Patient-based outcome score, Knee injury and Osteoarthritis Outcome Score (KOOS), Total knee arthroplasty (TKA), Japanese
Introduction
Knee osteoarthritis (OA) is common in the elderly population, and 25.3 million people have knee OA in Japan [1]. This prevalence is higher than in other countries by approximately 30 % in patients over 65 years old [2]. Knee OA causes chronic pain, disabilities and falls and leads to confinement to bed [3]. Furthermore, severe and painful knee OA often needs total knee arthroplasty (TKA) as the operative option to relieve pain and recover knee function. The Osteoarthritis Research Society International recommends this treatment which has advantages in cost-effectiveness [4]. Previous post-operative observational studies have shown excellent implant survival rates and good doctor-based objective outcomes [5], even in severely deformed varus knees [6], younger patients with intense activity [7, 8], rheumatoid arthritis [9] and revision surgery [10].
Clinical evaluation of the patients’ symptoms, activities of daily living (ADL) and quality of life (QOL) are mainly performed by the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [11] and Knee injury and Osteoarthritis Outcome Score (KOOS) [12]. In Japan, available criteria for evaluating patients’ subjective symptoms have mainly been the 36-Item Short Form (SF-36) [13, 14] or the Japanese Knee Osteoarthritis Measure (JKOM) [15]. Recently, the Japanese KOOS was confirmed for its validity and reliability regarding patient-based outcome scores through cross-cultural adaptation [16]. However, application of its features in Japanese TKA patients has been unclear. Whereas objective scales such as the Knee Society Score (KSS) and Japanese Orthopaedic Association (JOA) score have well-established validation and response rates [17, 18], the Japanese KOOS has shown little correlation with objective scales for patient-based outcome scores in previous studies [19]. Furthermore, the normal variability and responses of KOOS in Japanese patients and the general population are unknown. In evaluating patients related to knee surgery, each domain consists of items based on ADL. However, there are some differences in lifestyle between Japan and Western countries, making it necessary to investigate the suitability of the Japanese KOOS in evaluating patients regionally. Relationships and differences between these conventional objective scales and the Japanese KOOS in post-operative TKA patients also need to be clarified in order to investigate their correspondence and interchangeability.
The purpose of this study was to investigate the relationship between conventional objective scales and patient-based outcome scores. Furthermore, this study aimed to reveal the normal variability and features of the Japanese KOOS in the post-operative TKA patients. We postulated that conventional objective scales could reflect only a part of the post-operative symptoms and conditions evaluated by the patient-based outcome score.
Materials and methods
Subjects
Subjects were patients who had TKA performed in our institution from May 2002 to April 2010 and had been followed up for more than two years. A total of 219 knees in 156 patients had undergone TKA. Post-operative knee symptoms were evaluated by self-reported questionnaires sent by mail, besides the observation of physical examinations and radiographs in final follow-ups. The response rate of questionnaires sent by mail was 130 of 156 patients (83.3 %). Finally, a total of 130 patients (16 men and 114 women) and 186 knees (20 knees in men and 166 knees in women) were used for statistical analysis of this retrospective study. All participants provided written informed consent for this, and the study was conducted with the approval of the ethics Committee of Hirosaki University School of Medicine. The mean age of patients was 74.0 ± 8.0 years old and follow-up duration was 49 (24–120) months (Table 1). TKA was the primary surgery in 170 patients (91.4 %) and revision surgery in 16 patients (8.6 %). In our institution, causative diseases for TKA were OA (174 patients, 93.5 %), rheumatoid arthritis (RA) (ten patients, 5.4 %) and osteonecrosis (two patients, 1.1 %).
Table 1.
Brief summary of participants
| Men (n = 20) | Women (n = 166) | |
|---|---|---|
| Age (years) | 73.6 ± 4.7 | 71.1 ± 7.8 |
| Height (cm) | 156.0 ± 10.6* | 149.3 ± 7.3* |
| BW (kg) | 60.8 ± 6.9 | 60.5 ± 11.0 |
| BMI (kg/m2) | 25.2 ± 3.1 | 27.0 ± 4.3 |
| Preoperative ROM (°) | 118.2 ± 12.7 | 101.4 ± 20.4* |
| Post-operative ROM (°) | 118.0 ± 12.4 | 110.9 ± 19.3 |
| Preoperative FTA (°) | 183.1 ± 5.6 | 182.3 ± 6.9 |
| Post-operative FTA (°) | 174.8 ± 2.2 | 174.7 ± 2.4 |
All values were mean ± standard deviations. Differences between men and women were compared by Mann–Whitney U test
BW body weight, BMI body mass index, ROM range of motion, FTA femorotibial angle
*A p value below 0.05 was considered significant
Patient evaluations
Subjective evaluation was performed by using KOOS which is representative of patient-based outcome score. KOOS consisted of 42 knee-related items, and each item was scored from 0 to 4. Five subscales of symptoms, pain, ADL, sports and QOL were converted to 100 points. Decreasing scores indicate worsening of knee symptoms. JOA score and KSS knee score and function score were used as conventional objective scales [20]. Each scale was scored from 0 to 100 points, and 0 points indicate the worst condition of the knee. In addition, surgeons scored the surgeon’s satisfaction score based on a post-operative feeling of the surgeon. This surgeon’s satisfaction score was scored as a total of 10 points, according to diagnostic impression and post-operative radiographs.
X-ray findings
As an additional objective scale, weight-bearing anteroposterior knee radiographs were taken in all patients. Radiographic examination was performed by standard protocol, and radiographs were converted into Digital Imaging and Communications in Medicine (DICOM) data. Femorotibial angles (FTA) were measured before surgery and at final follow-up, and the corrected angle was calculated. FTA was determined as an angle formed by a line passing through the midpoint of the femoral cortex and the midpoint of the tibial cortex.
Surgical procedures
TKA was performed with the image-free navigated system (OrthoPilot TKA ver. 4.2, B. Braun Aesculap, Tuttlingen, Germany). A parapatellar approach was performed to expose the knee. Tracker diodes were positioned and fixed to the proximal tibia and distal femur to induce the navigation system. After registration of kinematic data, anatomical landmarks were registered. The tibia was cut with a varus/valgus and anterior/posterior slope of 0˚. The overall soft tissue balance was adjusted and measured for straight alignment. The gap distance was then analysed with the navigation computer. Medial release was then performed in a step-by-step manner such that the medial and lateral gap difference was less than three millimetres at both full extension and 90° flexion [6, 21, 22]. Following tibial and femoral trials, the components e.motion or Columbus Total Knee System (B. Braun Aesculap, Tuttlingen, Germany) were implanted.
Statistical analysis
Data input and statistical calculation were performed by SPSS ver. 12.0 J (SPSS Inc., Chicago, IL, USA). Spearman’s correlation coefficients were estimated to investigate the relationship between the Japanese KOOS as patient-based outcome scores and JOA score, KSS knee, KSS function and satisfaction scores as conventional objective scales. Also, the correlation with KOOS and corrected FTA were investigated by Spearman’s correlation coefficients. Comparisons of corrected values between primary and revision surgery as well as OA and RA patients were performed by analysis of covariance. Each score was correlated by age at surgery, gender and body mass index (BMI), and multiple comparisons were performed by the Bonferroni method. A p value below 0.05 was considered to be statistically significant.
Results
Patient evaluations
Mean values for all participants were 76.5 ± 14.2 (35–100) for JOA score, 88.4 ± 13.1 (45–100) for KSS knee score, 74.4 ± 21.7 (15–100) for KSS function score and 8.6 ± 1.1 [6–10] for surgeon’s satisfaction score. KOOS symptoms was 90.8 ± 12.5, KOOS pain was 93.0 ± 11.4, KOOS ADL was 88.0 ± 13.0, KOOS sports was 40.5 ± 30.6 and KOOS QOL was 77.7 ± 24.6. All of the objective scales of JOA score and KSS were significantly correlated with subscales of KOOS (Table 1). Surgeon’s satisfaction score, JOA score and KSS function were strongly correlated with KOOS ADL, and their correlation coefficients were 0.806 and 0.830, respectively. Also, KSS knee score correlated with KOOS pain most strongly, and the correlation coefficient was 0.689. However, JOA score and KSS only had moderate correlation with KOOS symptoms, sports and QOL. Furthermore, correlation coefficients with surgeon’s satisfaction score were weak from 0.188 to 0.321 (Table 2).
Table 2.
Correlation coefficients between patient-based outcome scales and conventional objective scales
| JOA score | KSS knee | KSS function | Satisfaction score | |
|---|---|---|---|---|
| KOOS symptoms | 0.499* | 0.502* | 0.454* | 0.287* |
| KOOS pain | 0.478* | 0.689* | 0.406* | 0.092 |
| KOOS ADL | 0.806* | 0.655* | 0.830* | 0.241* |
| KOOS sports | 0.630* | 0.493* | 0.673* | 0.188* |
| KOOS QOL | 0.489* | 0.523* | 0.476* | 0.321* |
Values were correlation coefficients between KOOS and objective scales such as JOA score, KSS knee, KSS function and satisfaction score. Spearman’s correlation coefficients were calculated
*A p value below 0.05 was considered significant
X-ray findings
The overall mean value of corrected FTA was 7.6 ± 7.2°. Post-operative FTA was significantly correlated with satisfactory score (r = −0.302). By contrast, increasing corrected angle affected the patient’s subjective score, especially KOOS QOL (r = 0.250, p = 0.002) (Table 3).
Table 3.
Correlation coefficients between preoperative FTA and their correction angles and outcome scales
| Post-operative FTA | Correction angle | |||
|---|---|---|---|---|
| r | p value | r | p value | |
| KOOS symptoms | −0.015 | 0.851 | 0.168* | 0.040 |
| KOOS pain | 0.115 | 0.145 | 0.090 | 0.270 |
| KOOS ADL | −0.059 | 0.455 | 0.195* | 0.016 |
| KOOS sports | −0.046 | 0.565 | 0.266* | 0.001 |
| KOOS QOL | −0.072 | 0.367 | 0.250* | 0.002 |
| JOA score | −0.091 | 0.259 | 0.180* | 0.030 |
| KSS knee | 0.015 | 0.853 | 0.160 | 0.055 |
| KSS function | −0.145 | 0.072 | 0.251* | 0.002 |
| Satisfaction score | −0.302* | 0.000 | 0.230* | 0.002 |
Values were Spearman’s correlation coefficients between each scale and femorotibial angle (FTA) and their correction angle
*A p value below 0.05 was considered significant
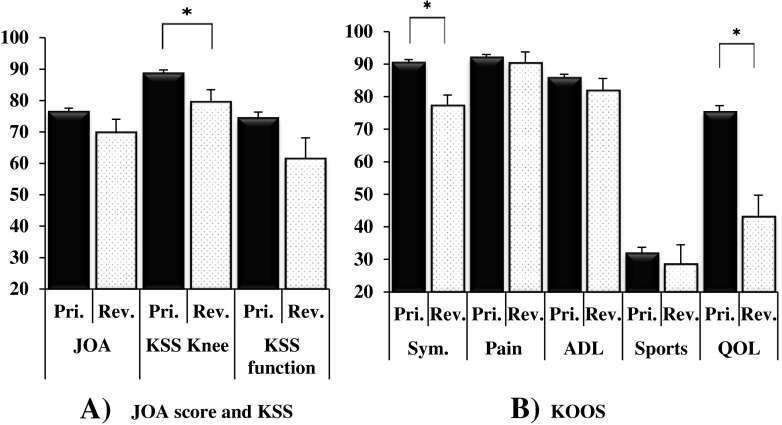
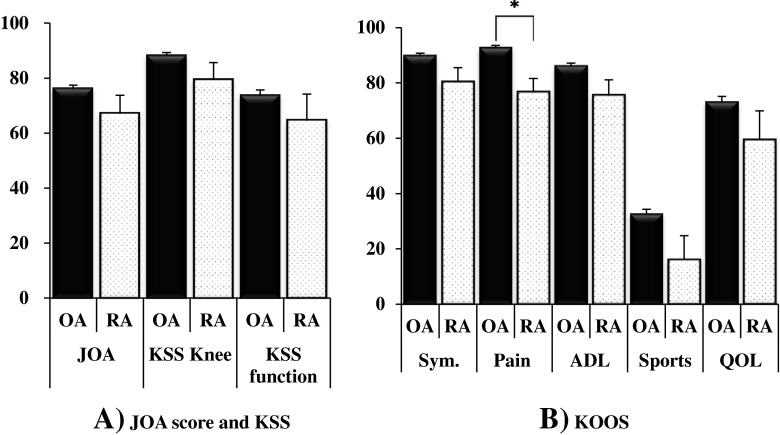
Comparison between primary and revision surgery, OA and RA patients
JOA score of the revision group did not show a significantly low value (p = 0.151). While KOOS QOL was 75.2 in the primary group, the corresponding value in the revision group was 43.1, which was a significantly lower value (p < 0.001) (Fig. 1). There was no significant reference between the OA group and RA group in JOA score and KSS, respectively. Though KOOS pain of the OA group was 92.5, that of the RA group was 76.6 and showed a significantly low value (p = 0.003) (Fig. 2).
Fig. 1.
Comparison of post-operative symptoms by a JOA score and KSS and b KOOS between primary and revision TKA in each scale. Values were corrected means and standard errors adjusted by age at surgery, gender and BMI. Comparisons between primary and revision TKA were performed by the Bonferroni method. *A p value below 0.05 was considered to be statistically significant
Fig. 2.
Comparison of post-operative symptoms by a JOA score and KSS and b KOOS between TKA for OA and RA in each scale. Values were corrected means and standard errors adjusted by age at surgery, gender and BMI. Comparisons between OA and RA were performed by the Bonferroni method. *A p value below 0.05 was considered to be statistically significant
Discussion
This study focused on the patient-based outcome scales of post-operative TKA patients. Symptoms and conditions in post-operative TKA patients were successfully evaluated by the Japanese KOOS. Although conventional objective scales indicated simply low scores, patient-based outcome scales showed good condition in regard to post-operative pain and symptoms. Regarding post-operative activity, while patients maintained knee function normally in their daily life, they could not perform high-performance activities needed for competitive sports. Also, post-operative knee-related QOL was low.
The results of this study suggested that it is necessary to use other types of measurement besides conventional objective scales in order to evaluate knee-related QOL and their satisfaction for post-operative patients. Post-operative TKA patients had their pain relieved and maintained their ADL, but showed low QOL in the Japanese KOOS. Correlation analysis showed that conventional objective scales such as JOA score and KSS were representative of mainly ADL or pain in patient-based related outcome scales; however post-operative patients’ QOL showed weak correlation with objective scales. This study showed that it is difficult to evaluate the TKA patients only by objective scales, and KOOS provides useful scores for this aspect, because the Japanese KOOS is strongly correlated with SF-36[16].
The KSS knee score correlated strongly with KOOS pain. The results of this study showed that RA patients complained of pain, and in RA patients KOOS pain was lower than that of OA patients. A previous study reported that post-operative recovery rate in KSS knee score of RA patients was lower than that of OA patients [6]. However, it is not a simple process to compare the conditions of RA and OA exactly if the prosthesis, disease population, age at surgery and usual patients’ activity levels are considered [5]. Regarding questionnaires for evaluation of pain, the JOA score consisted of two items with seven answer options, KSS consisted of one item with seven answer options and KOOS pain consisted of nine items with five answer options. This is one of the reasons why these detailed evaluation questionnaires may contribute to identifying the differences between these conditions.
It was a very important finding that the strength of correlation between KOOS sports and conventional objective scales was limited to moderate in evaluating post-operative TKA patients. Recently it was shown that TKA improved the participation of patients in sports activities after surgery; it was reported that approximately 65 % of patients after TKA had returned to their sports activities [23]. However, increasing activities after TKA may potentially have negative effects that increase the risk of wear and tear and loosening of the implants. As careful follow-up is needed in these high activity patients, the Knee Society added evaluation items for patients with sports activities in the new Knee Society Knee Scoring System [24]. KOOS sports activities consist of “jumping” and “running”, and these items made it possible to evaluate the knee function and symptoms in high activity patients which KOOS ADL could not [25]. KOOS would be a good parameter for activities in highly active patients such as younger patients after TKA.
There were several limitations to this study. First, patients with severe OA causing stiffness and post-operative TKA patients have difficulty in deep flexion of the knee and a restricted range of motion. In those with knee stiffness, scores of items like “bending to floor/picking up an object” and “squatting” become higher spontaneously. Second, differences in lifestyle affect their understanding. In Japan, the Japanese low level styles of bed and toilet are preferred especially by elderly people, unlike in Western countries. Slight differences would occur in the results of “rising from bed” and “getting on/off toilet” [16]. Third, one of the purposes of TKA was returning to work such as agriculture, which is a prevalent requirement in this region. However, there were no questionnaires about work-related motion such as “climbing up and down ladder” and “carrying heavy load”. Fourth, this study had a small number of male patients, revision TKA and RA patients, which is less than optimal for comparative results. Finally, we could not compare the immediate change after surgery, because there were no preoperative data for the Japanese KOOS. However, preoperative evaluation is also necessary for further extensive understanding of symptoms after TKA. Currently a study to investigate perioperative changes of patient-based scores is now running to assess this point.
Conclusions
The Japanese KOOS detected low QOL besides relief of pain and maintaining ADL after TKA surgery. Conventional objective scales reflected mainly knee-related low activity and were correlated strongly to ADL disturbances. This result suggested that it is necessary to use the patient-based outcome scores to evaluate knee-related QOL and level of satisfaction with TKA. This study showed that KOOS is useful to acquire extensive information about OA patients’ conditions.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M, Saika A, Yoshida H, Suzuki T, Yamamoto S, Ishibashi H, Kawaguchi H, Nakamura K, Akune T. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab. 2009;27:620–628. doi: 10.1007/s00774-009-0080-8. [DOI] [PubMed] [Google Scholar]
- 2.Felson DT. Epidemiology of hip and knee osteoarthritis. Epidemiol Rev. 1988;10:1–28. doi: 10.1093/oxfordjournals.epirev.a036019. [DOI] [PubMed] [Google Scholar]
- 3.Muraki S, Akune T, Oka H, Ishimoto Y, Nagata K, Yoshida M, Tokimura F, Nakamura K, Kawaguchi H, Yoshimura N. Physical performance, bone and joint diseases, and incidence of falls in Japanese men and women: a longitudinal cohort study. Osteoporos Int. 2012;24:459–466. doi: 10.1007/s00198-012-1967-0. [DOI] [PubMed] [Google Scholar]
- 4.Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18:476–499. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Gill GS, Chan KC, Mills DM. 5- to 18-year follow-up study of cemented total knee arthroplasty for patients 55 years old or younger. J Arthroplasty. 1997;12:49–54. doi: 10.1016/S0883-5403(97)90046-2. [DOI] [PubMed] [Google Scholar]
- 6.Maniwa K, Ishibashi Y, Tsuda E, Yamamoto Y, Inoue R, Otsuka H. Accuracy of image-free computer navigated total knee arthroplasty is not compromised in severely deformed varus knees. J Arthroplasty. 2013;28:802–806. doi: 10.1016/j.arth.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Dalury DF, Ewald FC, Christie MJ, Scott RD. Total knee arthroplasty in a group of patients less than 45 years of age. J Arthroplasty. 1995;10:598–602. doi: 10.1016/S0883-5403(05)80202-5. [DOI] [PubMed] [Google Scholar]
- 8.Keenan AC, Wood AM, Arthur CA, Jenkins PJ, Brenkel IJ, Walmsley PJ. Ten-year survival of cemented total knee replacement in patients aged less than 55 years. J Bone Joint Surg Br. 2012;94:928–931. doi: 10.1302/0301-620X.94B7.27031. [DOI] [PubMed] [Google Scholar]
- 9.Schai PA, Scott RD, Thornhill TS. Total knee arthroplasty with posterior cruciate retention in patients with rheumatoid arthritis. Clin Orthop Relat Res. 1999;367:96–106. [PubMed] [Google Scholar]
- 10.Manopoulos P, Havet E, Pearce O, Lardanchet JF, Mertl P. Mid- to long-term results of revision total knee replacement using press-fit intramedullary stems with cemented femoral and tibial components. J Bone Joint Surg Br. 2012;94:937–940. doi: 10.1302/0301-620X.94B7.26943. [DOI] [PubMed] [Google Scholar]
- 11.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 12.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17–26. doi: 10.1186/1477-7525-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akai M, Doi T, Fujino K, Iwaya T, Kurosawa H, Nasu T. An outcome measure for Japanese people with knee osteoarthritis. J Rheumatol. 2005;32:1524–1532. [PubMed] [Google Scholar]
- 16.Nakamura N, Takeuchi R, Sawaguchi T, Ishikawa H, Saito T, Goldhahn S. Cross-cultural adaptation and validation of the Japanese Knee Injury and Osteoarthritis Outcome Score (KOOS) J Orthop Sci. 2011;16:516–523. doi: 10.1007/s00776-011-0112-9. [DOI] [PubMed] [Google Scholar]
- 17.Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB, Kinemax Outcomes Group Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am. 2001;83-A:1856–1864. doi: 10.2106/00004623-200112000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Okuda M, Omokawa S, Okahashi K, Akahane M, Tanaka Y. Validity and reliability of the Japanese Orthopaedic Association score for osteoarthritic knees. J Orthop Sci. 2012;17:750–756. doi: 10.1007/s00776-012-0274-0. [DOI] [PubMed] [Google Scholar]
- 19.Ghanem E, Pawasarat I, Lindsay A, May L, Azzam K, Joshi A, Parvizi J. Limitations of the Knee Society Score in evaluating outcomes following revision total knee arthroplasty. J Bone Joint Surg Am. 2010;92:2445–2451. doi: 10.2106/JBJS.I.00252. [DOI] [PubMed] [Google Scholar]
- 20.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 21.Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985;192:13–22. [PubMed] [Google Scholar]
- 22.Yagishita K, Muneta T, Ikeda H. Step-by-step measurements of soft tissue balancing during total knee arthroplasty for patients with varus knees. J Arthroplasty. 2003;18:313–320. doi: 10.1054/arth.2003.50088. [DOI] [PubMed] [Google Scholar]
- 23.Bradbury N, Borton D, Spoo G, Cross MJ. Participation in sports after total knee replacement. Am J Sports Med. 1998;26:530–535. doi: 10.1177/03635465980260041001. [DOI] [PubMed] [Google Scholar]
- 24.Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The new Knee Society Knee Scoring System. Clin Orthop Relat Res. 2012;470:3–19. doi: 10.1007/s11999-011-2135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nilsdotter AK, Toksvig-Larsen S, Roos EM. A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthritis Cartilage. 2009;17:601–606. doi: 10.1016/j.joca.2008.11.007. [DOI] [PubMed] [Google Scholar]