Abstract
Purpose
The hypothesis of our study is that a routine tibial cut during cruciate retaining TKA may result in a partial or a total removal of the PCL footprint. Therefore providing a reliable landmark is essential to estimate the probability of PCL damage with a tibial cut and to enable the surgeon to decide pre-operatively whether a cruciate retaining implant design is suitable.
Methods
In a case series of 175 cruciate retaining TKA, the routinely made standing postoperative AP-view radiographs were evaluated to determine the distance between fibula head and tibial cutting plane. In a second case series knee MRI of 223 subjects were consecutively used to measure the vertical distance between tibial attachment of PCL and fibula head. The probability of partial or total PCL damage was calculated for different vertical distances between tibial cut and fibula head.
Results
The vertical distance between the tibial cut and the most proximal point of the fibula head averaged 6.1 mm ±4.8 mm. The mean vertical distance from fibula head to proximal and to distal PCL footprint revealed to be 11.4 mm ±3.7 mm and 5.4 mm ±2.9 mm, respectively. The location of the insertion was not significantly different between subgroups such as age (<50 or >50 years), gender and side. Based on our results 11 (7 %) knees were considered at high risk of an entire PCL removal after implantation of a cruciate retaining TKA design.
Conclusions
Currently available routine tibial preparation techniques result in partial or total posterior cruciate ligament detachment. Fibula head as a landmark aids to predict the PCL location and to estimate its disruption pre- and postoperatively on AP-view radiographs.
Keywords: Cruciate retaining total knee arthroplasty, Posterior cruciate ligament, Tibial cut, Fibula head
Introduction
The role of posterior cruciate ligament in primary total knee arthroplasty has been controversially discussed [5, 8, 12, 13, 31]. According to the reported clinical data, significant outcome differences between cruciate retaining and cruciate substituting total knee replacement does not exist [5, 8, 12, 13]. Possible advantages of the cruciate retaining technique are proprioceptive function [17], physiological kinematics [8, 15] and stabilisation of extension and flexion gap. However, flexion instability after cruciate retaining total knee arthroplasty due to insufficient PCL is associated with pain and poor clinical outcome [20, 33].
Due to the difficult exposure of the PCL with a routine TKA approach, the extension of the PCL-footprint damage can sometimes only be estimated after performing the tibial osteotomy. Providing reliable landmarks seems essential to enable the surgeon to predict preoperatively or intra-operatively the risk of PCL damage with a routine tibial cut during TKA.
Several recent papers described the anatomical characteristics of the femoral and tibial PCL attachments relative to numerous intra-articular landmarks [1, 10, 30]. To our knowledge these intra-articular landmarks have not been evaluated in severe osteoarthritic deformed knees to predict the location of the tibial PCL insertion prior to total knee arthroplasty.
Few authors reported that the PCL footprint is partly or totally removed during a routine tibial cut [7, 26]. Feyen et al. [7] performed a 9-mm tibial cut with 3 degrees of posterior slope in 20 cadaver tibiae and quantified the consecutive PCL attachment resection. On average 68.8 % ± 15.3 % of the PCL footprint area was removed. Shannon et al. [26] described the location of the tibial PCL insertion relative to fibula head on MRI prior to TKA in 22 cases and determined postoperatively the vertical distance between fibula head and tibial cutting plane on lateral view radiographs. One-third of their patients had a complete PCL removal after cruciate retaining total knee replacement. However, the small number of cases included in the previously published studies does not provide a solid base to accurately describe the relative frequency or probability of PCL damage.
Therefore in a large patient collective the first aim of the present study is to quantify the vertical distances between tibial cutting plane and fibula head after cruciate retaining TKA. Our second purpose includes the measurement of the distance between tibial PCL attachment and fibula head. The probability of a partial or a total removal of the PCL footprint with a routine tibial cut was determined.
Patients and Methods
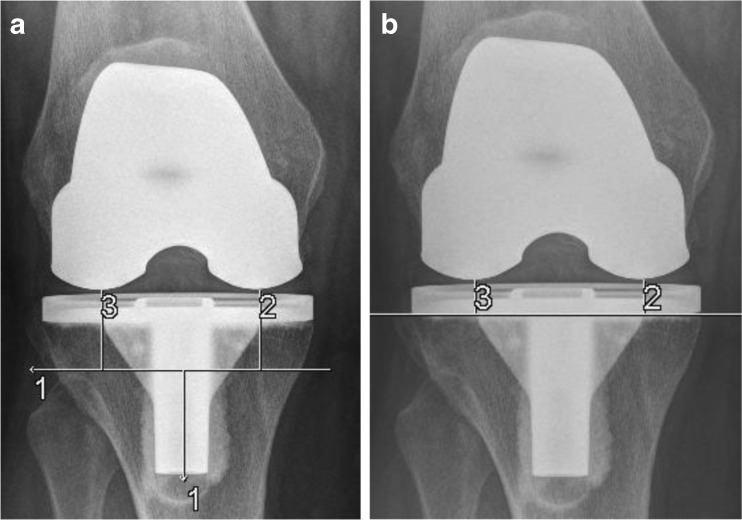
In the first consecutive case series 175 patients were included after undergoing primary cruciate retaining total knee arthroplasty for osteoarthritis. Seven knees were excluded due to inadequate radiographs. A modular cemented PFC cruciate retaining prosthesis design (DePuy Orthopaedics, Inc, Warsaw) was implanted. All procedures were performed with medial parapatellar approach. A fixed posterior slope of 3 degrees was planned for all knees. A standard tibial cut was performed and a specific attention was paid to maintain the joint line and to restore the leg alignment. Within the first postoperative week a standing, calibrated AP view radiograph was performed for each patient. A Syngo fast view software (Siemens AG, Erlangen, Germany) was applied to carry out the measurements. The distance from the most distal point on medial and lateral femoral condyles to the horizontal line passing through the tip of fibula head and perpendicular to the mechanical axis of tibia has been measured on AP view radiographs (Fig. 1a). Out of the medial and lateral distances the average distance between the fibula head and the distal femur component was calculated for each patient, which corresponds well to the middle of the tibial cutting plane. In order to calculate the magnification factor tibial component height provided in the patients electronic file was divided by tibial component height measured on native radiographs (Fig. 1b). The magnification factor averaged 0.95 (SD ± 0.1).
Fig. 1.
a 1 horizontal line perpendicular to tibial mechanical axis, 2 medial and 3 lateral vertical distances between femur condyles and fibula head. b 2 medial and 3 lateral distances between tibial cutting plane and femur condyles which corresponds to height of tibial component
The distance between fibula head and tibial cutting plane was calculated with the following formula:
 |
To evaluate the intra- and interobserver reliability of our native radiographic determination method of the distances between fibula head and tibial cutting plane, each of the two observers conducted their measurements twice independently in 30 cases. The measurement accuracy of the utilized ruler was 1 mm. The intra- and interobserver reliability determined with Cronbach’s α was 0.87 and 0.94, respectively.
In a second series of 223 consecutive knee joints, MR images were analysed in a retrospective study; 23 knees were excluded. Exclusion criteria were PCL tear, fracture, age <18, missing landmark such as fibula head, knee in flexion, poor MRI quality. The demographics are illustrated (Table 1). All patients had undergone MRI according to standards in the supine position and with fully extended knee joints. All MR images were performed between September 2011 and September 2012 using a 1,5-Tesla scanner (Magnetom Avanto, Siemens Healthcare Sector, Erlangen, Germany). The following sequences were available: T1-TSE, T2 and TIRM. For the purpose of this work, T1-TSE with a matrix of 320 × 100 and a resolution of 0.4 × 0.4 × 3.0 was selected to analyse the images in coronal, sagittal and axial view. After uploading the images into the OSIRIX software program the measurements were conducted on a three-dimensional multiplanar reconstruction (MPR) as follows. The axial plane was adjusted parallel to the distal femoral condylar line, whereas the coronal plane was parallel to the posterior condylar line. The longitudinal axis of the PCL was displayed on the sagittal plane. Distances were determined after selecting the landmarks and sequentially moving towards the area of interest within the defined planes. Vertical or horizontal lines were drawn parallel or perpendicular to the tibial longitudinal axis. The vertical distance between the most proximal point of the fibula head to the most distal and most proximal point of the PCL was measured on the sagittal plane (Fig. 2).
Table 1.
Demographics
| Variable | Number of knees | |
|---|---|---|
| Radiographs | MRI | |
| Female:Male | 100:68 | 98:102 |
| Right:Left | 88:80 | 90:110 |
Fig. 2.
a The horizontal line defines the level of the fibula head. b The distance between the most proximal and the most distal point of the PCL footprint to fibula head were measured as illustrated
For the first ten patients two observers performed the measurements on MR images independently twice. The intra- and interobserver measurement reliability was with Cronbach’s-α 0.8 respectively.
Since the evaluated radiological data were collected retrospectively from patients’ electronic records, an ethical approval was not necessary.
The following assumptions were made. If the tibial cut was below the most distal point of the PCL, the tibial footprint was considered totally removed. If the tibial cut was located within the proximal and distal tibial insertion points a partial removal was implied. A tibial cut above the most proximal point of the tibial footprint indicates a total PCL preservation.
Statistical analysis
The SAS software (9.1) and Excel (Version 2007) were used for statistical analysis. Average, median, range, standard deviation and distribution were calculated for each variable. After analysing the data for normal distribution (Excel:Normvert), Student’s t-test was used to evaluate differences between subgroups such as gender (female/male), age (<50y/>50y), and side (right/left). Statistical significance was set at a p-value of < 0.05.
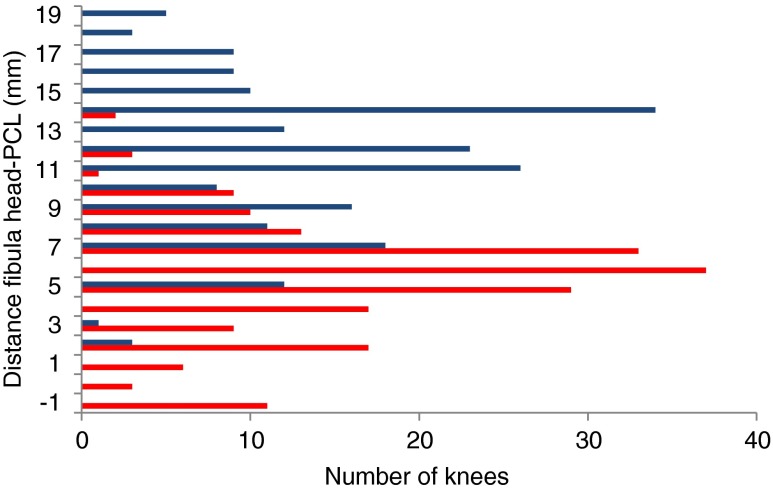
The relative frequency of distances between most proximal/most distal point of the PCL footprint and fibula head was calculated for the patient collective to estimate the probability (P) of partial or total PCL damage with a certain tibial cut. For a tibial cut the probability of the partial (blue) and total (red) PCL damage are visualized (Fig. 5).
Fig. 5.
This diagram was obtained after calculating the relative frequency of distances between proximal, distal PCL footprint and fibula head. The probability (0 to 1) of partial (blue) or total (red) PCL damage depends on the distance between fibula head and level of tibial osteotomy (+ tibial cutting plane above fibula head, − tibial cutting plane below fibula head)
Results
Relationship between tibial cut and fibula head
The vertical distance between the tibial cutting surface and the most proximal point of the fibula head averaged 6.1 mm ±4.8 mm (Fig. 3).
Fig. 3.
Distribution of the vertical distance between fibula head and tibial cutting surface (+ cutting surface above fibula head, − cutting surface below fibula head)
Relationship between PCL footprint and fibula head
The mean vertical distance between the lowest aspect of the tibial PCL insertion and the tip of the fibula head was 5.4 mm ±2.9 mm. The average vertical distance between the most proximal point of the PCL footprint and the tip of the fibula head measured 11.4 mm ±3.7 mm (Fig. 4).
Fig. 4.
Distribution of the vertical distance between fibula head and proximal (blue) or distal (red) aspect of the PCL footprint (+ insertion point above fibula head, - insertion point below fibula head)
Between the subgroups such as age (<50 or >50 years), gender and side, a statistically significant difference of the distance between PCL footprint and fibula head was not found.
Probability of PCL damage
If the tibial cut was 1 mm below the highest point of the fibula head, there is a high probability of removing the PCL entirely. In 11 cases (7 %) the tibial cut was more than 1 mm below the level of the fibula head, suggesting a total PCL removal. On the other hand if the tibial cut was 5.7 mm above the top of the fibula head, there is a 50 % chance of total PCL disruption (Fig. 5).
Discussion
Our main results reveal an average vertical distance between fibula head and PCL footprint to be distally 5.4 mm and proximally 11.4 mm. One of the most important findings of this work is that the location of the PCL footprint relative to fibula head can be well predicted independently of age, gender or side. Therefore it provides the surgeon the ability to estimate the amount of PCL damage with a certain tibial cut preoperatively on native AP radiographs. As in our case series, 11 (7 %) knees had a high probability of complete tibial PCL insertion damage after cruciate retaining TKA.
The question whether to retain, sacrifice or substitute the PCL in primary total knee arthroplasty remains debatable [12]. Comparable excellent clinical results have been published for both cruciate retaining as well as cruciate substituting TKA [3, 4, 6, 12, 14, 18, 21, 25, 27, 28, 33]. Since the PCL preserving TKA-design provides less conformity between the articulating tibial and femoral components, a balanced PCL with sufficient interaction between anterolateral and posteromedial bundles is crucial to prevent a posterior displacement of the tibia and allow for more physiological kinematics of the knee. Yue et al. [34] described the in vivo function of the PCL before and after a cruciate retaining TKA. Their reported data suggest that currently available cruciate retaining implant systems and surgical techniques may not restore the natural biomechanics of the PCL bundles. Balancing of the PCL is technically demanding and it might in certain cases impede equal and rectangular flexion/extension gaps [24]. Tight or imbalanced flexion gap due to unreleased PCL increases the load on the posterior aspect of the polyethylene insert or causes a unilateral femur condyle lift off which might lead to early failure [22, 29]. A stepwise partial release of the PCL after cruciate retaining TKA improved flexion ability and reduced excessive femoral roll-back [2]. In cases of insufficient PCL after cruciate retaining TKA which causes instability at flexion, pain and recurrent effusions, the conversion to a posterior stabilised TKA is an established treatment option [20, 33]. Other authors [18] [6] reported good and excellent clinical results for cruciate retaining TKA regardless of whether the PCL was excised or retained.
The mean tibial cutting error during TKA demonstrated to be 0.5° [11], and the amount of the tibial slope correlates positively with the probability of PCL disruption [7, 16].
In a recent cadaver work on 20 subjects, Feyen et al. showed that 68.8 % of the PCL attachment was removed while performing a tibial cut with 9 mm and 3° of posterior slope [7]. Shannon et al. determined the vertical distance between fibula head and PCL preoperatively on MRI in 22 knees and measured postoperatively on lateral view radiographs the distance between fibula head and tibial cutting surface. They had observed in eight cases (36.4 %) a total and in 9 cases (41 %) a partial PCL detachment [26]. Matziolis et al. simulated a 8-mm tibial resection on knee MRI with 0° or 7° of slope and found 45 % ± 28 % or 69 % ± 24 % disruption of the footprint in men. A significant gender specific difference was not reported [16]. However their findings should be cautiously used for osteoarthritic deformed knees prior to TKA, since intra-articular landmarks were applied and the age of the patients averaged 37.8 years. In 33 cadaver tibia, Takahashi et al. described the location of the anterolateral bundle to be at the level of the tibial articular surface whilst the midpoint of the posteromedial bundle was located 4,6 mm distally [30]. Other authors noted in anatomical studies the vertical distance between the tibia plateaus and the centre of tibial insertion of PCL to be 10 mm [32], 2–3 mm [9] and 1.6 mm [10]. The data above-mentioned confirms the findings of Ochsner et al. who had tested the PCL at physiological tension after performing stepwise tibial cuts [19]. A PCL failure was noted if the resection plane averaged 8.6 mm below the articulating surface. Considering the currently available polyethylene inlays and tibial baseplates mostly with a minimum thickness of 8 mm, a thinner tibial resection would shift the joint line proximally. Avoidance of a possible PCL failure without joint line elevation is achievable, if a bone block is left at the posterior tibial margin. However, this more or less popular surgical technique can sometimes be demanding and increases the risk of avulsion fracture.
In cases of severe knee osteoarthritis the reliability of intra-articular landmarks have not been evaluated in the literature. In massive osteoarthritic deformed knee joints the level of the tibia plateau medially or laterally might be in certain cases below the level of the fibula head. Schnurr et al. [23] observed a significant correlation between required tibial resection and pre-operative leg axis. Based on our results we believe a posterior cruciate retaining TKA design is not suitable for knees with severely deformed tibia plateau, since a correction of the leg alignment and maintaining the joint line without tibial wedge augmentation probably result in a total PCL damage. It was not within the scope of this study to quantify the tibia plateau deformity. The influence of body height on PCL location relative to fibula head was not investigated.
The identification of the most proximal point of the fibula head and the most distal point of femoral condyles as anatomical landmarks in AP view radiographs as well as the determined landmarks on MRI are considered reliable.
Conclusion
We were able to describe the fibula head as a useful landmark to map the PCL location pre-operatively and to estimate the probability of its disruption postoperatively on AP-view radiographs. This data can be used to preoperatively judge the possibility of successfully performing cruciate retaining TKA. Currently available routine tibial preparation techniques result in partial or total posterior cruciate ligament removal. Our results might help to clarify whether the hypothesis underlying cruciate retaining TKA is true and the PCL stays in function.
Acknowledgments
Conflicts of interest
All authors declare that there are no conflicts of interest
References
- 1.Amis AA, Gupte CM, Bull AM, Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):257–263. doi: 10.1007/s00167-005-0686-x. [DOI] [PubMed] [Google Scholar]
- 2.Arima J, Whiteside LA, Martin JW, Miura H, White SE, McCarthy DS. Effect of partial release of the posterior cruciate ligament in total knee arthroplasty. Clin Orthop Relat Res. 1998;353:194–202. doi: 10.1097/00003086-199808000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Becker MW, Insall JN, Faris PM. Bilateral total knee arthroplasty. One cruciate retaining and one cruciate substituting. Clin Orthop Relat Res. 1991;271:122–124. [PubMed] [Google Scholar]
- 4.Bolanos AA, Colizza WA, McCann PD, Gotlin RS, Wootten ME, Kahn BA, Insall JN. A comparison of isokinetic strength testing and gait analysis in patients with posterior cruciate-retaining and substituting knee arthroplasties. J Arthroplasty. 1998;13(8):906–915. doi: 10.1016/S0883-5403(98)90198-X. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhary R, Beaupre LA, Johnston DW. Knee range of motion during the first two years after use of posterior cruciate-stabilizing or posterior cruciate-retaining total knee prostheses. A randomized clinical trial. J Bone Joint Surg Am. 2008;90(12):2579–2586. doi: 10.2106/JBJS.G.00995. [DOI] [PubMed] [Google Scholar]
- 6.Clark CR, Rorabeck CH, MacDonald S, MacDonald D, Swafford J, Cleland D. Posterior-stabilized and cruciate-retaining total knee replacement: A randomized study. Clin Orthop Relat Res. 2001;392:208–212. doi: 10.1097/00003086-200111000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Feyen H, Van Opstal N, Bellemans J (2012) Partial resection of the PCL insertion site during tibial preparation in cruciate-retaining TKA. Knee Surg Sports Traumatol Arthrosc. April 22 [Epub ahead of print] [DOI] [PubMed]
- 8.Freeman MA, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38(2):197–208. doi: 10.1016/j.jbiomech.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;106:216–231. doi: 10.1097/00003086-197501000-00033. [DOI] [PubMed] [Google Scholar]
- 10.Greiner P, Magnussen RA, Lustig S, Demey G, Neyret P, Servien E. Computed tomography evaluation of the femoral and tibial attachments of the posterior cruciate ligament in vitro. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1876–1883. doi: 10.1007/s00167-011-1493-1. [DOI] [PubMed] [Google Scholar]
- 11.Hasegawa M, Yoshida K, Wakabayashi H, Sudo A. Cutting and implanting errors in minimally invasive total knee arthroplasty using a navigation system. Int Orthop. 2013;37(1):27–30. doi: 10.1007/s00264-012-1688-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs WC, Clement DJ, Wymenga AB (2005) Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev (4):CD004803. [DOI] [PubMed]
- 13.Kim YH, Choi Y, Kim JS. Range of motion of standard and high-flexion posterior cruciate-retaining total knee prostheses a prospective randomized study. J Bone Joint Surg Am. 2009;91(8):1874–1881. doi: 10.2106/JBJS.H.00769. [DOI] [PubMed] [Google Scholar]
- 14.Maruyama S, Yoshiya S, Matsui N, Kuroda R, Kurosaka M. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19(3):349–353. doi: 10.1016/j.arth.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Matsuzaki T, Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kawakami Y, Ishida K, Oka S, Kuroda R, Kurosaka M. Kinematic factors affecting postoperative knee flexion after cruciate-retaining total knee arthroplasty. Int Orthop. 2013;37(5):803–808. doi: 10.1007/s00264-013-1803-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matziolis G, Mehlhorn S, Schattat N, Diederichs G, Hube R, Perka C, Matziolis D. How much of the PCL is really preserved during the tibial cut? Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1083–1086. doi: 10.1007/s00167-011-1696-5. [DOI] [PubMed] [Google Scholar]
- 17.Mihalko WM, Creek AT, Mary MN, Williams JL, Komatsu DE. Mechanoreceptors found in a posterior cruciate ligament from a well-functioning total knee arthroplasty retrieval. J Arthroplasty. 2011;26(3):504. doi: 10.1016/j.arth.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 18.Misra AN, Hussain MR, Fiddian NJ, Newton G. The role of the posterior cruciate ligament in total knee replacement. J Bone Joint Surg Br. 2003;85(3):389–392. doi: 10.1302/0301-620X.85B3.13182. [DOI] [PubMed] [Google Scholar]
- 19.Ochsner JL, Jr, McFarland G, Baffes GC, Cook SD. Posterior cruciate ligament avulsion in total knee arthroplasty. Orthop Rev. 1993;22(10):1121–1124. [PubMed] [Google Scholar]
- 20.Pagnano MW, Hanssen AD, Lewallen DG, Stuart MJ. Flexion instability after primary posterior cruciate retaining total knee arthroplasty. Clin Orthop Relat Res. 1998;356:39–46. doi: 10.1097/00003086-199811000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Pereira DS, Jaffe FF, Ortiguera C. Posterior cruciate ligament-sparing versus posterior cruciate ligament-sacrificing arthroplasty. Functional results using the same prosthesis. J Arthroplasty. 1998;13(2):138–144. doi: 10.1016/S0883-5403(98)90091-2. [DOI] [PubMed] [Google Scholar]
- 22.Ritter MA, Faris PM, Keating EM. Posterior cruciate ligament balancing during total knee arthroplasty. J Arthroplasty. 1988;3(4):323–326. doi: 10.1016/S0883-5403(88)80032-9. [DOI] [PubMed] [Google Scholar]
- 23.Schnurr C, Csecsei G, Nessler J, Eysel P, Konig DP. How much tibial resection is required in total knee arthroplasty? Int Orthop. 2011;35(7):989–994. doi: 10.1007/s00264-010-1025-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schnurr C, Eysel P, Konig DP. Is the effect of a posterior cruciate ligament resection in total knee arthroplasty predictable? Int Orthop. 2012;36(1):83–88. doi: 10.1007/s00264-011-1295-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwartz AJ, Della Valle CJ, Rosenberg AG, Jacobs JJ, Berger RA, Galante JO. Cruciate-retaining TKA using a third-generation system with a four-pegged tibial component: a minimum 10-year followup note. Clin Orthop Relat Res. 2010;468(8):2160–2167. doi: 10.1007/s11999-010-1360-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shannon FJ, Cronin JJ, Cleary MS, Eustace SJ, O’Byrne JM. The posterior cruciate ligament-preserving total knee replacement: do we ‘preserve’ it? A radiological study. J Bone Joint Surg Br. 2007;89(6):766–771. doi: 10.1302/0301-620X.89B6.18782. [DOI] [PubMed] [Google Scholar]
- 27.Sorger JI, Federle D, Kirk PG, Grood E, Cochran J, Levy M. The posterior cruciate ligament in total knee arthroplasty. J Arthroplasty. 1997;12(8):869–879. doi: 10.1016/S0883-5403(97)90156-X. [DOI] [PubMed] [Google Scholar]
- 28.Swanik CB, Lephart SM, Rubash HE. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am. 2004;86-A(2):328–334. doi: 10.2106/00004623-200402000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Swany MR, Scott RD. Posterior polyethylene wear in posterior cruciate ligament-retaining total knee arthroplasty. A case study. J Arthroplasty. 1993;8(4):439–446. doi: 10.1016/S0883-5403(06)80045-8. [DOI] [PubMed] [Google Scholar]
- 30.Takahashi M, Matsubara T, Doi M, Suzuki D, Nagano A. Anatomical study of the femoral and tibial insertions of the anterolateral and posteromedial bundles of human posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1055–1059. doi: 10.1007/s00167-006-0192-9. [DOI] [PubMed] [Google Scholar]
- 31.van den Boom LG, Brouwer RW, van den Akker-Scheek I, Bulstra SK, van Raaij JJ. Retention of the posterior cruciate ligament versus the posterior stabilized design in total knee arthroplasty: a prospective randomized controlled clinical trial. BMC Musculoskelet Disord. 2009;10:119. doi: 10.1186/1471-2474-10-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van Dommelen BA, Fowler PJ. Anatomy of the posterior cruciate ligament. A review. Am J Sports Med. 1989;17(1):24–29. doi: 10.1177/036354658901700104. [DOI] [PubMed] [Google Scholar]
- 33.Waslewski GL, Marson BM, Benjamin JB. Early, incapacitating instability of posterior cruciate ligament-retaining total knee arthroplasty. J Arthroplasty. 1998;13(7):763–767. doi: 10.1016/S0883-5403(98)90027-4. [DOI] [PubMed] [Google Scholar]
- 34.Yue B, Varadarajan KM, Rubash HE, Li G. In vivo function of posterior cruciate ligament before and after posterior cruciate ligament-retaining total knee arthroplasty. Int Orthop 36(7):1387–1392 [DOI] [PMC free article] [PubMed]