Abstract
Purpose
Navigation-based total knee arthroplasty (TKA) has proven its value for restoration of the limb axis. However, patient-orientated results after TKA show a wide variation from the correct implantation technique. Nonphysiological kinematics without posterior femoral rollback and tibial internal rotation in flexion could be one reason for this. We postulated that a modified gap-balancing technique with navigation of the tibia alone, in comparison to a conventional navigated technique, would: (1) obtain lateral femoral rollback, (2) alter condylar liftoff without midflexion instability, (3) significantly differ in femoral and tibial cuts, (4) not be inferior in leg-axis restoration and (5) be comparable in clinical short-term scores.
Methods
In this prospective study, we compared in vivo navigation-based kinematics pre- and postoperatively of 40 consecutive TKA comprising 21 conventional navigation-based TKA and 19 TKA with the modified gap-balancing technique and a reduced navigation workflow. All cuts were double checked and compared with cuts proposed by the navigation system. Clinical results were assessed preoperatively and six months postoperatively.
Results
The modified gap-balancing technique resulted in significantly increased lateral femoral rollback (mean 16.3 mm) and lateral condylar liftoff (mean 1.3 mm) compared to the conventional group. The modified technique comprised an average of 2.1 mm less distal femoral resection and an average of 4° less external rotation and 3.5° more flexion of the femoral component compared with the control group. Average tibial resection height was 1.1 mm greater and average tibial slope was 0.5° elevated compared to the control group. A neutral leg axis was achieved in all cases. Results showed no significant differences in clinical scores between groups.
Conclusion
A partial navigation solely of the tibial cut can securely restore the leg axis. Modification of the surgical technique can possibly reproduce more physiological knee kinematics with higher lateral femoral rollback in flexion without midflexion instability. This might help reduce postoperative problems with the new implant and thus reduce the amount of unsatisfactory results. Despite equal short-term results, mid- to long-term results are needed to prove whether or not this correlates with better clinical results and at least equal implant longevity.
Keywords: Knee kinematics, Gap-balancing technique, Partial navigation
Introduction
Nowadays, surgeons must deal with a relatively high number of unsatisfied patients after total knee arthroplasty (TKA); Bourne et al. [8] indicate 11–18 %. Direct patient-dependent coefficients and patient-independent factors are held responsible for this: for example, body mass index (BMI), activity level and preoperative expectations [11, 24, 27], on the one hand, and surgical technique [10], restoration of limb axis [5] and implant design [23] on the other hand. Few studies have focussed on knee kinematics, which, however, might be one reason for improving postoperative problems with the operated joint. Pre- and postoperative knee kinematics show a wide variety of results, including mostly paradoxical forward slide of the femur during flexion [6, 25, 32], whereas normal knee kinematics describe a predominantly lateral femoral rollback during flexion [17, 18, 21].
The purpose of this prospective, randomised study was to combine the advantages of navigated TKA with a modified gap-balancing technique, and to compare and double check bony cuts and the results of the modified technique to conventionally navigated TKA. We tested the hypotheses that: (1) the modified surgical technique with reduced navigation workflow approaches natural knee kinematics with lateral femoral rollback and tibial internal rotation with flexion; (2) alter condylar liftoff without midflexion instability; (3) significantly differ in femoral and tibial cuts, (4) restore the limb axis, and (5) there would be no differences in clinical outcome measures [Knee Society Scores (KSS), Western Ontario and McMaster Osteoarthritis Index (WOMAC)] prior to and at the latest follow-up between groups.
Materials and methods
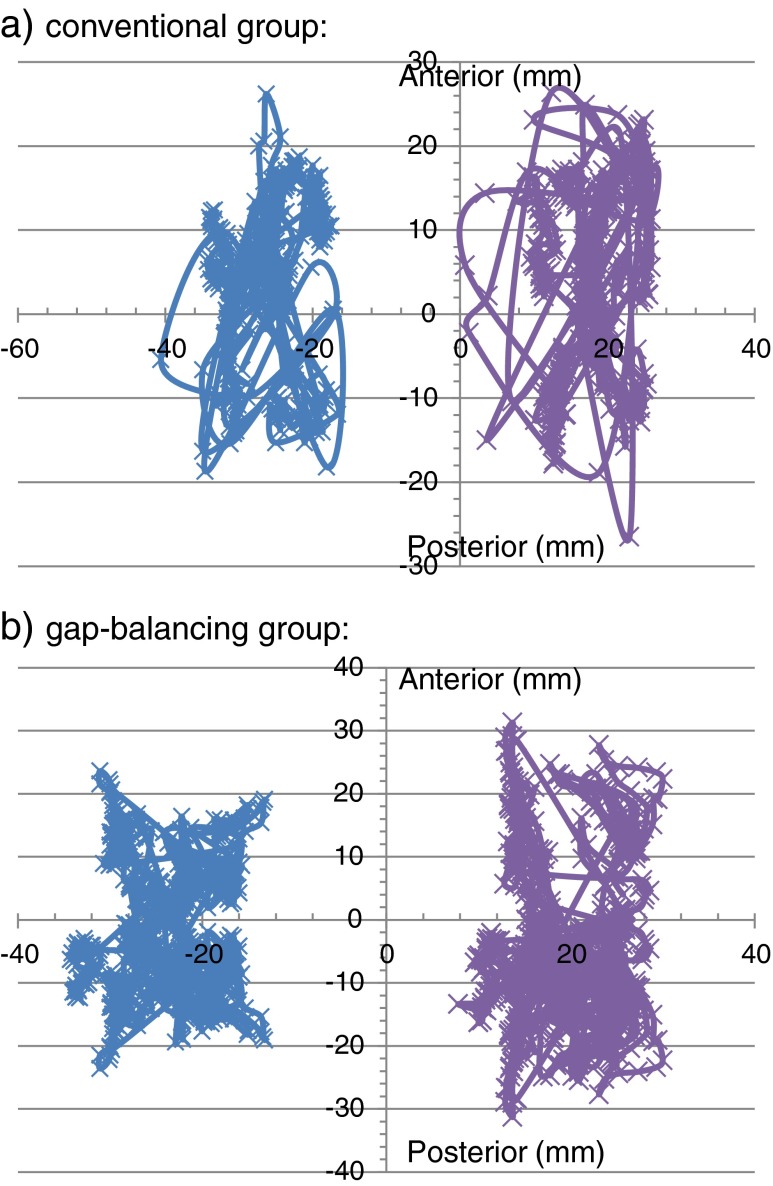
In this prospective study, we recruited 40 patients with primary osteoarthritis of the knee designated for TKA in a three-month period. Patients over 85 years, with secondary osteoarthritis of the knee, severe varus or valgus deformity (more than 15°) requiring a hinged implant or not willing to participate were excluded; four patients were excluded for these reasons. Patients provided informed consent to this study, which was approved by the ethics committee (Ethic Committee Approv. Number: 11-101-0135). All 40 patients received a standard, cemented, cruciate-retaining (CR) condylar prosthesis with fixed platform (PFC Sigma, DePuy, Warsaw, IN, USA), either with the conventional navigation technique (21 knees, controls; group 1) or with the modified gap-balancing technique with a reduced navigation workflow (19 knees, group 2), depending on computerised randomisation. No patella replacements were used. All operations were performed under the direction of the senior author using a standard medial parapatellar approach. After exposing the knee, two passive optical reference arrays were attached on the medial distal femur and the medial proximal tibia. After determining the centre of the hip joint by circumduction, the required anatomical landmarks (femoral epicondyles, anterior femoral cortex, medial and lateral malleolus, tibial plateau magnitude and anterior tibial cortex) were acquired. The following kinematic test included passive range of motion (ROM) from maximum extension to maximum flexion, during which the relative orientation between femur and tibia was displayed in real time. Furthermore, the height of the medial and lateral gap was recorded, measuring the deepest points of the medial and lateral condyles in relationship to the tibial component. The difference between medial and lateral measurements was considered to represent condylar liftoff if it was over one millimetre. The gaps were analysed every 10° between 0° and 130° of flexion. This first kinematic test was performed before cutting the anterior cruciate ligament (preimplantation kinematic). After prosthesis implantation, the kinematic test was repeated (postimplantation kinematic). Kinematic elaboration was based on the analysis of passive ROM. For each patient, the combination of movements was registered three times. Intraoperative passive kinematics were measured using the BrainLab surgical navigation system (Knee 2.5.1 BrainLab, Feldkirchen, Germany) and analysed by the corresponding software. The system includes an optoelectronic localiser, two removable reference arrays (fixed on the femur and tibia using seven millimetre Schanz screws) and a probe, all of which are equipped with passive optical markers. The software allows anatomical and kinematic data acquisitions that separately monitor movement of the medial and lateral femoral condyle on the tibial plateau (Fig. 1). It provides real-time display of knee alignment during surgery and standard kinematic evaluations. All kinematic analyses were recorded after temporarily occlusion of the joint capsule by clamping jaws.
Fig. 1.
Movement of the medial (segment left, blue) and lateral (segment right, purple) femoral condyle on the tibial plateau during knee flexion. a Conventional group. b Gap-balancing group
The modified gap-balancing technique was based on the principles of John Insall’s classic gap-balancing technique [19], modified by Fitz et al., resulting in a medial pivoting knee kinematic [16]. It comprised restoration of the medial condylar J curve with less distal femoral resection (to result in a “true” cut of eight millimetres representing implant thickness, a strict cut of eight millimetres, but the assumed cartilage and bone loss of the affected condyle was subtracted from this cut). To compensate for this reduced distal femoral resection, more tibial resection had to be performed. After osteophyte removal and ligament release, femoral rotation was established using a double tensiometer inserted in 90° flexion. After distraction to 90 N medially and laterally, the posterior femoral component thickness of eight millimetres (again, including assumed cartilage and bone loss, if applicable) was taken off the posterior medial condyle. Femoral sizing was adjusted using anterior referencing off the deepest point of the trochlear groove.
Navigation workflow in group 2 consisted solely of a navigation-controlled tibial resection. All other bone cuts were performed by the above-mentioned technique. However, all bone cuts were double checked and compared with the cuts proposed by the navigation system and documented by screenshot. Kinematic tests were performed, as described before. For the conventionally navigated group, a ligament-balanced implantation technique was performed according to the manufacturer’s advice (Depuy and Brainlab), which has been standardised and previously published [4]. Patients were evaluated preoperatively and six months postoperatively according to the KSS [20] and WOMAC rating system [5]. Results were assessed at the outpatient clinic by an independent, blinded investigator. No patient was lost during follow-up.
Statistical analysis
We used the Sigma Plot statistical software version (Systat Software Inc., San Jose, CA, USA). For within-group comparisons, we performed a paired t test or a Wilcoxon signed-rank test. A p value < 0.05 was considered to be of statistical significance.
Results
Demographic data
The patient population consisted of 25 women and 15 men, with an average age of 70.0 (range 49–87) years. The average follow-up was six (range five to eight) months. There were no statistically significant differences between groups regarding demographic data (Table 1). All arthritic knees had varus malalignment. Clinical scores (KSS, WOMAC) showed no significant differences preoperatively or at the latest follow-up (Tables 2 and 3).
Table 1.
Patient demographic data and range of motion (ROM)
| Conventional group | Gap-balancing group | P value | |
|---|---|---|---|
| Age at index operation | 70.0 min 49, max 87 |
72.4 min 56, max 86 |
>0.05 |
| ROM preoperatively | 0°/8°/102° (min 0° extension, max 115° flexion) |
0°/9°/102° (min 0° extension, max 112° flexion) |
>0.05 |
| ROM 6 months postoperatively | 0°/4°/110° (min 0° extension, max 130° flexion) |
0°/1°/108° (min 0° extension, max 130° flexion) |
>0.05 |
Table 2.
Knee Society Score (KSS)
| Conventional group | Gap-balancing group | P value | |
|---|---|---|---|
| Preoperatively | 49.3 (min 0, max 77) | 53.9 (min 24, max 88) | >0.05 |
| 6 months postoperatively | 82.1 (min 45, max 94) | 78.9 (min 64, max. 93) | >0.05 |
| Function score preoperatively | 51.7 (min 0 max 70) | 47.5 (min 25, max 80) | >0.05 |
| Function score 6 months postoperatively | 72.9 (min 35, max 100) | 65.5 (min 20, max 100) | >0.05 |
Table 3.
Western Ontario and McMaster Osteoarthritis Score (WOMAC) score
| WOMAC | Conventional group | Gap-balancing group | P value |
|---|---|---|---|
| Preoperatively | 45.6 (min 20, max 76) | 53.2 (min 22, max 82) | >0.05 |
| 6 months postoperatively | 20.6 (min 6, max 54) | 18.8 (min 0, max 50) | >0.05 |
There were no direct surgical-related complications during the follow-up period. One patient developed a urinary tract infection four days postoperatively, which was successfully treated with antibiotics for five days. Another patient had an ischaemic stroke six weeks postoperatively, with full recovery after neurological treatment.
Kinematics
In the control group (group 1), lateral femoral condyle rollback movement compared with that of the medial femoral condyle was increased (mean 4.5 mm); the difference was not statistically significant. Overall movement of the medial femoral condyle during knee flexion up to 130° was a mean of 13.1 mm compared with a mean of 17.6 mm for the lateral femoral condyle (Table 4).
Table 4.
Anteroposterior (AP) rollback movement of medial and lateral femoral condyles
| Patient number | Medial femoral condyle | Lateral femoral condyle |
|---|---|---|
| Gap-balancing technique | ||
| 1 | 10.3 | 11.5 |
| 2 | 6.4 | 9.3 |
| 3 | 9.8 | 15.3 |
| 4 | 6.3 | 12.8 |
| 5 | 9.1 | 12.8 |
| 6 | 8.8 | 16.8 |
| 7 | 5.7 | 17.9 |
| 8 | 6.2 | 12.1 |
| 9 | 13.0 | 18.0 |
| 10 | 17.4 | 27.3 |
| 11 | 4.4 | 9.0 |
| 12 | 9.3 | 14.2 |
| 13 | 21.0 | 26.4 |
| 14 | 9.8 | 19.1 |
| 15 | 9.6 | 11.5 |
| 16 | 4.1 | 21.7 |
| 17 | 8.5 | 20.1 |
| 18 | 11.2 | 16.7 |
| 19 | 12.7 | 16.3 |
| Conventional technique | ||
| 1 | 11.7 | 9.3 |
| 2 | 15.7 | 10.4 |
| 3 | 18.1 | 17 |
| 4 | 12.9 | 10.5 |
| 5 | 14.6 | 11.0 |
| 6 | 6.6 | 10.3 |
| 7 | 6.1 | 19.8 |
| 8 | 5.6 | 10.2 |
| 9 | 13.0 | 19.0 |
| 10 | 9.9 | 16.2 |
| 11 | 28.3 | 52.9 |
| 12 | 6.0 | 18.6 |
| 13 | 23.6 | 25.1 |
| 14 | 10.9 | 16.1 |
| 15 | 6.9 | 7.7 |
| 16 | 11.3 | 18.0 |
| 17 | 20.7 | 21.4 |
| 18 | 12.2 | 17.9 |
| 19 | 17.1 | 17.8 |
| 20 | 16.0 | 25.8 |
| 21 | 8.2 | 15.3 |
The modified gap-balancing technique with limited navigation workflow (group 2) resulted in increased lateral femoral rollback and tibial internal rotation with flexion. The difference was statistically significant (p < 0.05) (Fig. 1a, b). In the gap-balancing group, the lateral femoral condyle underwent increased rollback movement compared with the medial femoral condyle (mean 6.6 mm). Mean overall movement of the medial femoral condyle during knee flexion up to 130° was 9.7 mm compared with 16.3 mm of the lateral femoral condyle (Table 4), with a statistically significant difference.
Gaps
In our conventional cohort, the medial gap increased from 7.0 (±0.8) to 11.6 (±1.0) mm after the implantation, which was attributable to medial release, with a statistically significant difference (p < 0.05). The lateral gap changed from 11.2 (±0.9) preoperatively to 11.7 (±1.1) mm postimplantation, which was also statistically significant (p < 0.05). In our gap-balancing cohort, the medial gap increased from 6.8 (±0.9) to 10.5 (±0.5) mm after implantation, attributable to medial release, with a statistical significance (p < 0.05). The lateral gap changed from 11.2 (±0.6) mm to postimplantation 11.8 (±0.6) mm, also statistically significant (p < 0.05).
Condylar liftoff
Comparing gaps at different degrees of flexion and extension, no condylar liftoff was seen in the conventional group throughout the entire ROM. After implantation in the gap-balancing group, we found a condylar liftoff with an increased lateral gap between 10° and 120° of flexion. Mean difference between medial and lateral gaps was 1.3 mm in the gap-balancing group and 0.2 mm in the conventional group, a significant difference (p < 0.05) (Table 5).
Table 5.
Condylar liftoff in medial and lateral gap
| Gap-balancing technique | Conventional technique | |||||
|---|---|---|---|---|---|---|
| Degree of flexion | Medial gap | Lateral gap | Condylar liftoff | Medial gap | Lateral gap | Condylar liftoff |
| 0° | 9.6 | 10.5 | 0.9 | 10.3 | 10.5 | 0.2 |
| 10° | 9.8 | 10.9 | 1.1 | 10.4 | 10.7 | 0.3 |
| 20° | 10 | 11.3 | 1.3 | 10.7 | 11 | 0.3 |
| 30° | 10.2 | 11.6 | 1.4 | 11 | 11.1 | 0.1 |
| 40° | 10.4 | 11.8 | 1.4 | 11 | 11 | 0 |
| 50° | 10.4 | 11.8 | 1.4 | 11.2 | 11.3 | 0.1 |
| 60° | 10.7 | 12.1 | 1.4 | 11.2 | 11.1 | 0.1 |
| 70° | 10.8 | 12.1 | 1.3 | 11.4 | 11.2 | 0.2 |
| 80° | 10.8 | 12.2 | 1.4 | 11.7 | 11.5 | 0.2 |
| 90° | 10.9 | 12.1 | 1.2 | 12.2 | 12.2 | 0 |
| 100° | 11 | 12.2 | 1.2 | 12.1 | 12.1 | 0 |
| 110° | 11.1 | 12.2 | 1.1 | 12.3 | 12.4 | 0.1 |
| 120° | 11.1 | 12.2 | 1.1 | 12.6 | 12.9 | 0.3 |
Cut deviation
Distal femoral resection in group 2 was less compared with group 1 (mean 2.1 mm), a statistically significant difference (p < 0.05); femoral external rotation in group 2 was less compared with group 1 (mean 4°), a statistically significant difference (p < 0.05); mean femoral external rotation in group 2 was 2.3° and 6.3° in group 1. Femoral component flexion in group 2 was higher compared with group 1 (mean 3.5°), a statistically significant difference (p < 0.05). Tibial resection in group 2 was higher compared with group 1 (mean 1.1 mm), which was not statistically significant (p > 0.05), and tibial slope in group 2 was higher compared with group 1 (mean 0.5°), also not statistically significant (p > 0.05).
Leg alignment
Postoperative mechanical leg axis was within the threshold of 3° in all patients. Also, radiological femoral flexion and tibial slope matched with the obtained navigational values.
Discussion
Up to 20 % of patients after TKA complain of persistent pain or difficulties with their new joint [8]. Besides direct patient-dependent coefficients and preoperative expectations, patient-independent factors, such as joint kinematics, are held responsible for this. With regard to our hypotheses, the modified surgical technique with gap balancing and restoration of the distal (mean 2.1 mm less, p < 0.05) and posterior femur showed more physiological knee kinematics, with higher lateral femoral rollback in flexion (mean 6.6 mm compared with 4.5 mm, p < 0.05) and without midflexion instability. The leg axis could be restored also by navigation of the tibial cut exclusively.
Healthy knee kinematics show a rollback movement of the femur during flexion, particularly of the lateral femoral condyle, concomitant with tibial internal rotation [15, 18, 28]. Most studies show that the medial femoral condyle hardly moves anteroposteriorly from full extension to 120° of flexion, whereas the lateral femoral condyle moves posteriorly to a variable extent. From 120° to full flexion, both condyles roll back onto the posterior horn [16, 17]. Knees with a unicondylar TKA show an almost physiological combination of movements, with a primarily rollback mechanism of the lateral femoral condyle during weight-bearing flexion. This motion sequence could, however, only be tracked when the anterior-cruciate ligament was intact [1]. Knee kinematics after TKA revealed a variety of movement patterns, including almost physiological sequences but also paradoxical forward slide of the femoral condyles during flexion [3, 13, 22]. Regardless of cruciate-retaining or cruciate-substituting implants, normal knee kinematics are rarely observed [13, 31]. Intra-operative knee kinematics can be influenced by implant design and surgical technique. Asymmetric or medial-pivoting TKAs show promising results [7, 29] but lack long-term results.
Gap-balancing implant techniques in TKA are based on more anatomical restoration of femoral condyles concomitant with a ligament-balanced orientation of femoral component rotation. The modified gap-balancing technique we used in this study was based on the protocol of Fitz et al. [16], which takes into account the estimated bone and cartilage loss before the bony resections. With their technique, they found tibial internal rotation with flexion and lateral rollback of the femoral condyles during flexion, with a greater amount of lateral condyle movement. Their results were fluoroscopically confirmed. Our intraoperative kinematic results emphasise the possibility of restoring physiological knee kinematics intraoperatively using a gap-balancing technique. Although we detected a femoral rollback mechanism concomitant with tibial internal rotation during knee flexion in both groups, we found significantly more lateral rollback and tibial internal rotation in flexion in our gap-balancing group. Our preliminary findings with a symmetrical implant show parallelism to kinematic data from study groups using asymmetric total knee implants [7].
In line with Insall et al. [19] and Fitz et al. [16], we found less distal femoral resection, more femoral flexion and more tibial resection and slope in the gap-balancing group. Less femoral external rotation with the modified implant technique is generated by ligament tension. Pre- and postoperatively, we achieved balanced medial and lateral gaps in flexion and extension. However, condylar liftoff was detected throughout almost the entire ROM in the gap-balancing group beginning at 10° of flexion, reflecting the more physiological situation with greater laxity of the lateral compartment leading to rollback. In the conventional group, no condylar liftoff was detected throughout the entire ROM. Previous studies observed liftoff from 50 % to 86 % of cruciate-retaining TKA [7, 14, 26]. The average amount of condylar liftoff in the gap-balancing group was 1.3 mm, which is comparable with other study groups [7, 14], in which an average liftoff between one and two millimetres is described. An increased midflexion instability in the gap-balancing group, however, could not be detected clinically up to the latest follow-up. In this context, the physiological condylar liftoff should be mentioned, with the lateral joint gap showing 6.7 mm ± 1.9 mm (2.1–9.2 mm) and the medial joint gap showing just 2.1 ± 1.1 mm (0.2–4.2 mm) during varus–valgus stress [30]. The postoperative mechanical leg axis was within the threshold of 3° in all patients. Navigation solely of the tibial cut would therefore be sufficient to securely restore leg axis, with concomitant enormous saving in additional time needed for navigation. Furthermore, this partial navigation technique can also be performed using a reduced, pinless, navigational workflow with high accuracy, which further reduces complications of pin placement [2].
There are several limitations of our study. Overall, our results did not include weightbearing, and we lack additional confirmation due to missing fluoroscopic investigations. Much published data concerning knee kinematics is based on weightbearing trials, making it difficult to compare our results. Using MRI, Johal et al. [21] compared tibiofemoral movement in ten weightbearing and nonweightbearing Caucasian knees and found tibial internal rotation during flexion in both groups but with an earlier and greater magnitude of rotation in the weightbearing group. Our results, however, are in line with previously described studies [16, 19], and we used a navigation-based visualisation technique that has not been described thus far. Furthermore we advise caution comparing our condylar liftoff results with other study groups [7, 15, 29]. Differences might be attributable to the nonweightbearing situation intraoperatively and to our definition of condylar liftoff beginning at a difference of over one millimetre between medial and lateral gaps. There is no common definition of condylar liftoff, which is diversely described as being between 0.75 and two millimetres [7, 12]. Also, different measuring techniques from the distance of the lowest point of the medial and lateral condyle to the closest point on the tibial polyethylene insert or to the tibial plateau are described [7, 9, 12]. Condylar liftoff, however, does not correlate with pain or instability [14] but is supposed to improve functional performance [12].
Partial navigation solely of the tibial cut can securely restore the leg axis. Modification of the surgical technique can possibly reproduce more physiological knee kinematics with higher lateral femoral rollback in flexion without midflexion instability. This might help reduce postoperative problems with the new implant and thus the number of unsatisfactory results. Despite equal short-term results, mid- to long-term results are needed to confirm whether or not this technique correlates with better clinical results and at least equal implant longevity.
Acknowledgment
We thank Mr. Quirin Hartmann-Guendel for his valuable support and work throughout the project.
References
- 1.Argenson J-NA, Komistek RD, Akizuki S. In vivo biomechanics of unicondylar knee replacement performed using minimally invasive technique. Orthop. 2007;36:1100–1105. doi: 10.1007/s00132-007-1170-8. [DOI] [PubMed] [Google Scholar]
- 2.Baier C, Maderbacher G, Springorum HR, Zeman F, Fitz W, Schaumburger J, Grifka J, Beckmann J (2013) No difference in accuracy between pinless and conventional computer-assisted surgery in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. Off. J. Esska [DOI] [PubMed]
- 3.Baier C, Springorum H-R, Götz J, Schaumburger J, Lüring C, Grifka J, Beckmann J. Comparing navigation-based in vivo knee kinematics pre- and postoperatively between a cruciate-retaining and a cruciate-substituting implant. Int Orthop. 2013;37:407–414. doi: 10.1007/s00264-013-1798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bäthis H, Shafizadeh S, Paffrath T, Simanski C, Grifka J, Lüring C. Are computer assisted total knee replacements more accurately placed? A meta-analysis of comparative studies. Orthop. 2006;35:1056–1065. doi: 10.1007/s00132-006-1001-3. [DOI] [PubMed] [Google Scholar]
- 5.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 6.Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53. doi: 10.1302/0301-620X.84B1.12432. [DOI] [PubMed] [Google Scholar]
- 7.Bertin KC, Komistek RD, Dennis DA, Hoff WA, Anderson DT, Langer T. In vivo determination of posterior femoral rollback for subjects having a NexGen posterior cruciate-retaining total knee arthroplasty. J Arthroplasty. 2002;17:1040–1048. doi: 10.1054/arth.2002.35793. [DOI] [PubMed] [Google Scholar]
- 8.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cates HE, Komistek RD, Mahfouz MR, Schmidt MA, Anderle M. In vivo comparison of knee kinematics for subjects having either a posterior stabilized or cruciate retaining high-flexion total knee arthroplasty. J Arthroplasty. 2008;23:1057–1067. doi: 10.1016/j.arth.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Clarke HD, Scuderi GR. Flexion instability in primary total knee replacement. J Knee Surg. 2003;16:123–128. [PubMed] [Google Scholar]
- 11.Culliton SE, Bryant DM, Overend TJ, Macdonald SJ, Chesworth BM (2011) The relationship between expectations and satisfaction in patients undergoing primary total knee arthroplasty. J Arthroplasty [DOI] [PubMed]
- 12.Dennis DA, Komistek RD, Kim RH, Sharma A. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop. 2010;468:102–107. doi: 10.1007/s11999-009-1112-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB (2003) Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop 37–57 [DOI] [PubMed]
- 14.Dennis DA, Komistek RD, Walker SA, Cheal EJ, Stiehl JB. Femoral condylar liftoff in vivo in total knee arthroplasty. J Bone Joint Surg Br. 2001;83:33–39. doi: 10.1302/0301-620X.83B1.10632. [DOI] [PubMed] [Google Scholar]
- 15.Dennis DA, Mahfouz MR, Komistek RD, Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech. 2005;38:241–253. doi: 10.1016/j.jbiomech.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 16.Fitz W, Sodha S, Reichmann W, Minas T. Does a modified gap-balancing technique result in medial-pivot knee kinematics in cruciate-retaining total knee arthroplasty? A pilot study. Clin Orthop. 2012;470:91–98. doi: 10.1007/s11999-011-2121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freeman MAR, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38:197–208. doi: 10.1016/j.jbiomech.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 18.Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br. 2000;82:1196–1198. doi: 10.1302/0301-620X.82B8.10716. [DOI] [PubMed] [Google Scholar]
- 19.Insall J, Ranawat CS, Scott WN, Walker P (1976) Total condylar knee replacement: preliminary report. Clin Orthop 149–154 [DOI] [PubMed]
- 20.Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop 13–14 [PubMed]
- 21.Johal P, Williams A, Wragg P, Hunt D, Gedroyc W. Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using “interventional” MRI. J Biomech. 2005;38:269–276. doi: 10.1016/j.jbiomech.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 22.Li G, Most E, Sultan PG, Schule S, Zayontz S, Park SE, Rubash HE. Knee kinematics with a high-flexion posterior stabilized total knee prosthesis: an in vitro robotic experimental investigation. J Bone Joint Surg Am. 2004;86-A:1721–1729. doi: 10.2106/00004623-200408000-00017. [DOI] [PubMed] [Google Scholar]
- 23.Liu Y-L, Chen W-C, Yeh W-L, McClean CJ, Huang C-H, Lin K-J, Cheng C-K (2011) Mimicking anatomical condylar configuration into knee prosthesis could improve knee kinematics after TKA—a computational simulation. Clin Biomech. Bristol Avon [DOI] [PubMed]
- 24.Lopez-Olivo MA, Landon GC, Siff SJ, Edelstein D, Pak C, Kallen MA, Stanley M, Zhang H, Robinson KC, Suarez-Almazor ME. Psychosocial determinants of outcomes in knee replacement. Ann Rheum Dis. 2011;70:1775–1781. doi: 10.1136/ard.2010.146423. [DOI] [PubMed] [Google Scholar]
- 25.Massin P, Boyer P, Sabourin M (2011) Less femorotibial rotation and AP translation in deep-dished total knee arthroplasty. An intraoperative kinematic study using navigation. Knee Surg Sports Traumatol Arthrosc. Off. J. Esska [DOI] [PubMed]
- 26.Moynihan AL, Varadarajan KM, Hanson GR, Park S-E, Nha KW, Suggs JF, Johnson T, Li G. In vivo knee kinematics during high flexion after a posterior-substituting total knee arthroplasty. Int Orthop. 2010;34:497–503. doi: 10.1007/s00264-009-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Connor MI. Implant survival, knee function, and pain relief after TKA: are there differences between men and women? Clin Orthop. 2011;469:1846–1851. doi: 10.1007/s11999-011-1782-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pinskerova V, Johal P, Nakagawa S, Sosna A, Williams A, Gedroyc W, Freeman MAR. Does the femur rollback with flexion? J Bone Joint Surg Br. 2004;86:925–931. doi: 10.1302/0301-620X.86B6.14589. [DOI] [PubMed] [Google Scholar]
- 29.Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ (2003) Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop 139–147 [DOI] [PubMed]
- 30.Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K. The flexion gap in normal knees. An MRI study. J Bone Joint Surg Br. 2004;86:1133–1136. doi: 10.1302/0301-620X.86B8.15246. [DOI] [PubMed] [Google Scholar]
- 31.Wünschel M, Leasure JM, Dalheimer P, Kraft N, Wülker N, Müller O (2013) Differences in knee joint kinematics and forces after posterior cruciate retaining and stabilized total knee arthroplasty. Knee [DOI] [PubMed]
- 32.Yue B, Varadarajan KM, Rubash HE, Li G. In vivo function of posterior cruciate ligament before and after posterior cruciate ligament-retaining total knee arthroplasty. Int Orthop. 2012;36:1387–1392. doi: 10.1007/s00264-011-1481-6. [DOI] [PMC free article] [PubMed] [Google Scholar]