Abstract
Purpose
The aim of this study was to analyse a possible correlation between the tibial slope and range of motion (ROM) after implantation of the low-contact-stress (LCS), mobile-bearing, total knee arthroplasty (TKA) after a minimum follow-up of ten years.
Methods
Eighty-three TKAs in 66 patients were investigated in this retrospective correlation analysis at a minimum follow up of ten years. Out of these 66 patients, 50 were women (76 %) and 16 (24 %) were men. The average age of these patients at the time of the examination was 76 years [standard deviation (SD) 11 years, range 37–95 years]. A lateral X-ray was taken at follow-up in order to analyse the tibial slope with respect to inter- and intra-observer agreement. ROM was measured and correlated with the tibial slope.
Results
The mean active ROM was 96.1° (SD 18.8) and the mean tibial slope after four measurements was 7.65° (SD 4.23), with substantial inter- and intra-observer agreement. We found no significant correlation between tibial slope and ROM in patients with a minimum follow-up of ten years [correlation 0.196 (p > 0.05) and 0.152, (p > 0.05), respectively].
Conclusions
Alteration of the tibial slope does not significantly influence ROM after implantation of the LCS TKA at a minimum follow-up of ten years. We conclude that the tibial slope is not the primary influencing factor for ROM in patients ten years after primary TKA and believe that it should not substantially be altered during surgery.
Keywords: Tibial slope, Radiologic measurement, Radiography, Correlation analysis, Range of motion
Introduction
The tibial slope is defined as the angle formed at the intersection of a line parallel to the posterior tibial inclination and a line that bisects the diaphysis of the tibia [16] and has an effect on knee stability, maximal flexion, joint resting position, cruciate ligament tension, pressure on the cartilage and the implant in case of total knee arthroplasty (TKA) [1–5, 16, 19]. In the human knee joint, the average slope is about 8°, with no significant differences among women and men but with differences among ethnic groups [6].
In TKA, an increased posterior slope might responsible for a greater range of motion (ROM). In vitro studies show a correlation between the cutting angle of the tibia and the resulting flexion, as prostheses implanted with 0° tibial slope showed significantly less ROM than knees cut with increased slope of 4° or even 7° [3]. In addition, it was postulated that with every degree of additional slope, 1.7° of flexion might be derived [3]. However, an excessive tibial slope should be avoided, as it might lead to anterior instability because the ACL is resected during surgery. The question remains as to what degree these findings can be applied to in vivo settings and what long-term results will be obtained, considering that after TKA, physiological knee kinematics will not persist, and posterior cruciate ligament (PCL)-retaining TKA shows specific motion patterns [3, 9]. The number of people undergoing TKA is constantly rising, and the expectancy of survival of new prosthesic designs is becoming greater [5, 11, 13,14]. The influence of tibial slope on long-term outcome, with a focus on active and passive ROM, has been poorly studied, even though ROM remains a mandatory outcome parameter for patients’ overall satisfaction.
The aim of this study was to analyse a possible correlation between tibial slope and active and passive ROM after implantation of the low-contact-stress (LCS), mobile-bearing, total knee prosthesis (Johnson & Johnson, New Brunswick, NJ, USA; previously DePuy, Warsaw, IN, USA) after a minimum follow-up of ten years. The study hypothesis was that the tibial slope would correlate with values of active and passive ROM in LCS TKA after a minimum follow-up of ten years.
Patients and methods
This study protocol was approved by the Local Ethics Committee (23-284 ex 10/11). Inclusion criteria were primary LCS TKAs in patients with a minimum follow-up of ten years. Exclusion criteria were all cases of revision surgery; patients having undergone implantation of other designs, such as the LCS TKA system; or patients diagnosed with rheumatoid arthritis. With respect to an a priori sample size calculation, expecting a medium effect size using G*Power 3 [23], an inclusion of 80 prosthesis was sufficient to conclusively analyse a questionable correlation between ROM and tibial slope.
Patients with a minimum follow-up of ten years after implantation of the LCS TKA were screened using our hospital database. After exclusion of revised and deceased patients and those with rheumatoid arthritis and implanted systems other than the LCS TKA, 83 knees in 66 patients were included. Out of these 66 patients, 50 were women (76 %) and 16 men (24 %). Average patient age at the time of follow-up was 76 years [standard deviation (SD) 11.39, range 37–95], and average age at the time of surgery was 62 (SD 11.97, range 21–78) years. Average follow-up was 14.6 (SD 2.83, maximum value 23 years, minimum of 11 years).
A lateral conventional X-ray was taken at the follow-up, and measurement of the tibial slope was performed according to the method published by Utzschneider et al. in 2011 [17]. Two independent and blinded observers undertook these measurements of the tibial slope. Measurement was repeated on a different day, and the intra- and interobserver reliabilities were calculated. By comparing two different observers, the interobserver correlation was measured, whereas the intra-observer correlation was the comparison of data of one and the same observer at two different time points. To measure the tibia slope, the following anatomical references were identified: On the ventral side of the tibia, the anterior tibial cortex (ATC) and on the dorsal side, the posterior tibial cortex (PTC). Two points 5 and 15 cm distal to the tibia plateau were identified, and a connection line between the ATC and the PTC was drawn. Midpoints of these lines were connected and named the tibial proximal anatomical axis (TPAA). Thereafter, the tibial slope was defined as the angle between the TPAA and the tibia plateau. Figure 1 illustrates the proximal tibia and fibula in a lateral view, showing the three anatomical references used to determine the posterior tibial slope: ATC, PTC and TPAA. On the day of the physical examination, active and passive ROM were measured using a standard goniometer. Active ROM was measured first, and assisted passive ROM was consecutively taken. Patients therefore were placed lying down on a standard examination couch to accurately determine ROM. Active ROM was tested before passive ROM in order to observe patients’ own functional limits, without putting stress and pain on the joint by the observer. By measuring passive ROM, the observer administered the utmost flexion tolerated by each patient. The investigation was not carried out to excess in order to limit the patient’s exposure to stress and pain. In addition, we evaluated the Knee Society Score (KSS) for function, and pain and the Western Ontario and McMaster Universities (WOMAC) score at follow-up [22] (Figs. 2 and 3).
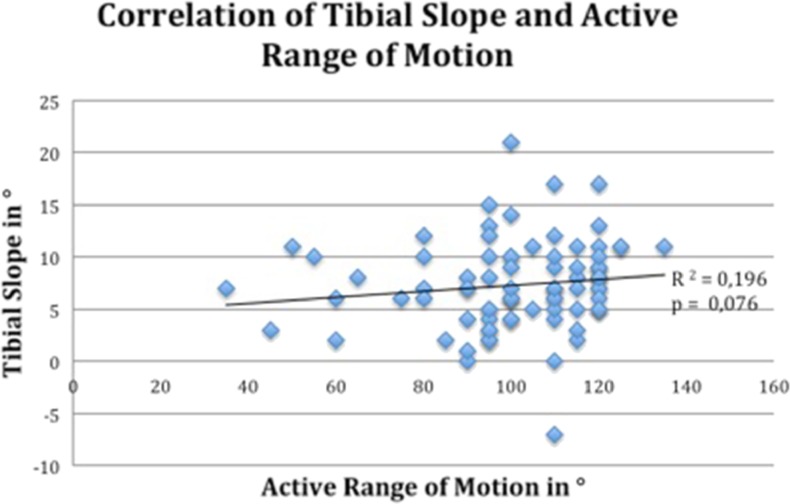
Fig. 2.
Correlation between tibial slope and active range of motion (ROM) 10 years after implantation of the low-contact-stress (LCS) total knee arthroplasty (TKA). Note the slight positive correlation reached no statistical significance
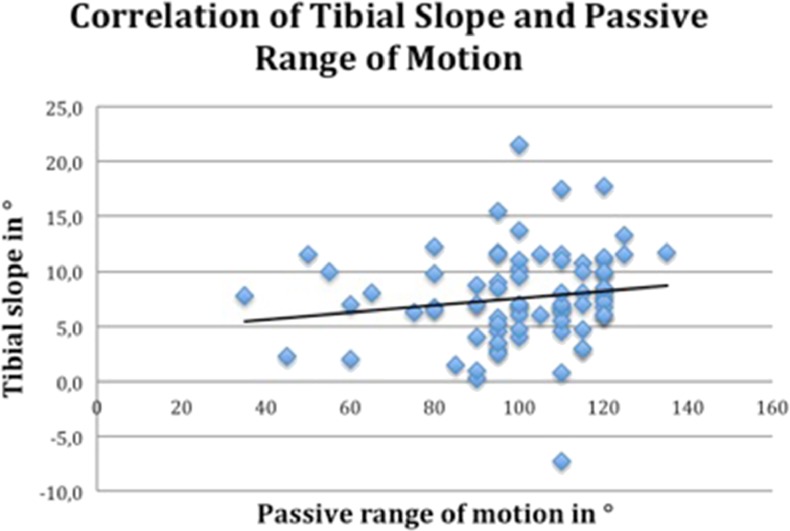
Fig. 3.
Correlation between tibial slope with passive range of motion (ROM) 10 years after implantation of the low-contact-stress (LCS) total knee arthroplasty (TKA). Note the slight positive correlation reached no statistical significance
Fig. 1.
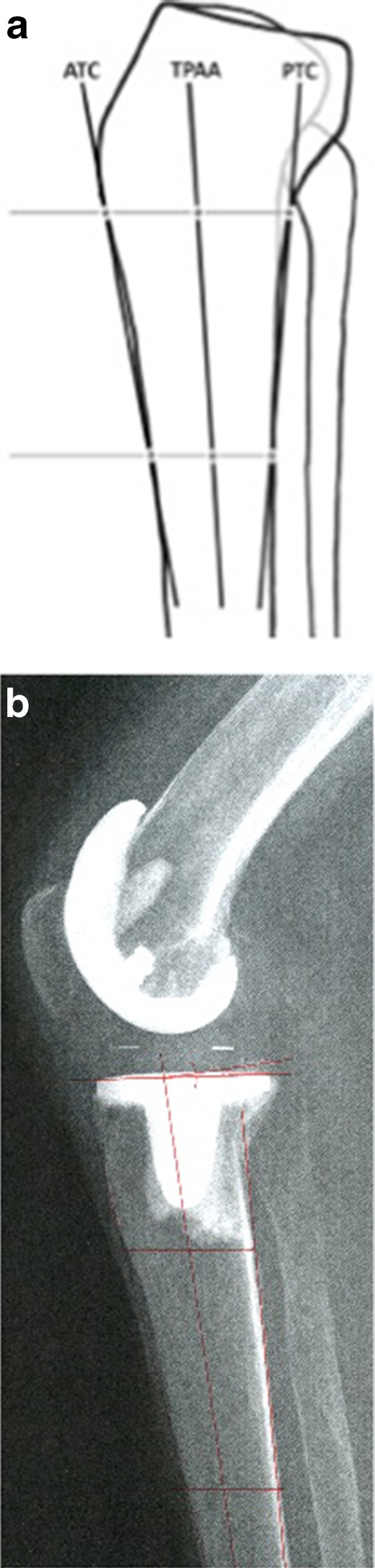
a Anterior tibial cortex (ATC), posterior tibial cortex (PTC) and tibial proximal anatomical axis (TPAA). b Lateral X-ray of a low-contact-stress (LCS) total knee arthroplasty (TKA) and measurement of 8° of tibial slope according to Utzschneider et al. [17]
Statistical analysis
In order to perform an a priori sample size calculation, G*Power 3 [23] was used. With respect to a medium effect size, a sample of at least 80 knees was necessary to receive a power >80 %. Differences in parametric variables were calculated using Student’s t test; nonparametric variables were analysed using Mann–Whitney U test; inter- and intra-observer correlations were calculated according to Cohen’s kappa, and a value >0.8 was considered for a substantial agreement. Regression analysis of ROM and tibial slope was calculated using Spearman’s correlation, and p value <0.05 was considered significant.
Results
Range of Motion
The examined values for passive ROM were 101° (SD 19.4) on average, with a minimum of 35° and an observed maximum of 135°. We observed an average value for active ROM of 96.1° (SD 18.8). Minimum overall ROM was 30° compared with a maximum of 125°.
Tibial Slope
By measuring the lateral X-ray, we found an average tibial slope value of 7.65° (SD 4.23) in 83 knees after four measurements in each knee. Maximum values reached 22° of posterior slope; −10° was the minimum, implying an actual 10° anterior slope. This is illustrated in Table 1.
Table 1.
Inter and intra-observer values of the two investigators who twice measured the tibial slope on 83 lateral X-rays according to Utzschneider et al. [17]. By measuring every X-ray taken on the day of examination four times, we found an average tibial slope value of 7.65° (standard deviation 4.23) in 83 investigated knees. Maximum posterior slope values were 22°; minimum slope value was −10°, implying an actual 10° anterior slope
| Observer 1, time point 1 | Observer 2, time point 1 | Observer 1, time point 2 | Observer 2, time point 2 | Overall mean value | |
|---|---|---|---|---|---|
| Mean value (°) | 8.12 | 7.35 | 7.61 | 7.42 | 7.625 |
| Interobserver correlation | >0.8 | >0.8 | >0.8 | >0.8 | |
| Intra-observer correlation | >0.8 | >0.8 | >0.8 | >0.8 |
Inter- and intra-observer correlation
We calculated observer reliability with inter- and intra-observer correlations. Results measured by hand on the imprinted X-rays showed a substantial correlation of >0.8 each when comparing observers. Comparing results by one and the same observer showed similar a substantial correlation of >0.8 each, respectively, thus indicating a highly reliable value of the further use of tibial slope for investigated patients (Table 1).
Correlation analysis
Regression analysis of measured values indicates no correlation between posterior tibial slope and active ROM (correlation 0.196; p value >0.05), thus showing no significant connection between implantation angle and postoperative active ROM. Similar results were obtained by comparing passive ROM and tibial slope. Correlation coefficient was 0.152 (p > 0.05). Comparing KSS function and pain scores revealed no correlation with tibial slope (0.053 (p > 0.05) and 0.097 (p > 0.05), respectively. In general, we found no significant correlation between posterior tibial slope and ROM or clinical scores of the knee joint after primary TKA. The slightly positive correlation of 0.196 between active ROM and posterior tibial slope ten years after primary TKA revealed no statistically significant value.
Discussion
The aim of this study was to analyse a possible correlation between tibial slope and active and passive ROM after TKA. The study hypothesis was that the tibial slope would correlate with values of active and passive ROM in LCS TKA after a minimum follow-up of ten years. We found that the tibial slope did not correlate with ROM, and we believe that the slope is a system-immanent factor, which should only slightly be altered in TKA.
To the best of our knowledge, this is the first study reported in the literature correlating ROM with tibial slope after LCS TKA and a minimum follow-up of ten years. In vitro studies indicate a connection between posterior tibial slope and ROM, knee-joint stability and PCL tension without proving this in the in vivo setting. The angle of the tibia plateau is an important factor of physiological biomechanics of the knee joint, as it regulates femoral rollback and influences tension on the PCL [2]. Impingement of the posterior femur limits further flexion and can be correct by a steeper tibial cut. Whereas in vitro studies clearly show a connection between tibial slope and postoperative ROM, it remains unclear to what degree patients can benefit in the long term from alteration of the cutting angle. There is no evidence thus far that changing the tibial slope during surgery has any significant influence on postoperative ROM in the long term. An altered angle significantly positively influences neither ROM nor KSS, as shown by Seo et al. [15]. The focus of their study was the absolute change of tibial angle from the pre-operative physiological to the definite cutting angle for prosthesis implantation [15].
In our study, we investigated the absolute posterior tibial slope ten years after surgery and compared it with active and passive ROM, thus providing another perspective to the topic of what extent the cutting angle influences postoperative ROM. Although the physiological process of motion clearly benefits from an increase in posterior slope, the operated knee does not gain any significant benefit from a steeper cutting angle. Apparently, PCL-retaining knees do not demonstrate normal knee kinematics, and the tibial slope is of less importance for active ROM. As postoperative ROM depends on many variables, tibial slope alone cannot be held responsible for satisfying surgical results.
Average patient age at the time of examination was 76 years, which might be considered a limitation of this study. Agility of the elder patient is naturally limited by age, and therefore, ROM of an operated knee strongly depends on patients’ overall health and physical status [10]. By defining the tibial slope, which has a broad physiological range with a mean value of 9°, as the single responsible variable of postoperative ROM, many important influencing factors for mobility, such as obesity or age, are ignored [6, 7, 9, 11, 12, 18–20]. We believe that the immanent tibial slope should only be slightly altered in TKA. Nonetheless, a slight positive correlation might be detected, and the cutting angle might slightly influence the outcome of primary TKA. However, this did not reach statistical significance in our analysis. With respect to the LCS mobile-bearing TKA, the manufacturer describes an ideal slope of 10° in its technical monograph [21].
Bellemans et al. report a gain of 1.7° in flexion for 1° of additional posterior tibial slope [3]. This approach is clinically limited, as an excessive tibial cut might lead to implant loosening in the long run as a technically related complication [21]. In case of a very steep implantation of the tibia plateau, subsequent sinking of the prosthesis can be observed. By conducting revision surgery, this situation can be solved to ease the patient’s pain and inability to fully extend the knee. Thus, an excessive tibial cut is clinically limited by the knee’s kinematics and prosthesis design. As our findings do not support the hypothesis of a gain of flexion by applying steeper tibial cuts, avoiding excessive posterior tibial slopes can diminish the risk of prosthetic loosening.
This study has the following limitations: We analysed the tibial slope on lateral X-rays only and did not use long-leg axis views or X-rays including the ankle joint as in other methods of evaluation [8, 24]. However, Utzschneider et al. demonstrate that measurement on lateral X-rays is a valuable and reproducible method, and we additionally calculated inter- and intra-observer correlations.
We emphasise the significant benefit that our study was sufficiently powered according to an a priori power analysis, that it reports sufficient follow-up of greater than ten years and that our inter- and intra-observer correlations reached substantial agreements. Therefore, the conclusions drawn from our results are statistically valid.
Conclusion
Alteration of the tibial slope does not significantly influence ROM after implantation of the LCS TKA at a minimum follow-up of ten years. We conclude that the tibial slope is not the primary influencing factor for ROM in patients ten years after primary TKA and believe it should not be substantially altered during surgery.
References
- 1.Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124:575–584. doi: 10.1007/s00402-004-0728-8. [DOI] [PubMed] [Google Scholar]
- 2.Aigner C, Windhager R, Pechmann M, Rehak P, Engeleke K. The influence of an anterior-posterior gliding mobile bearing on range of motion after total knee arthroplasty. A prospective, randomized, double-blinded study. J Bone Joint Surg Am. 2004;86:2257–2262. doi: 10.2106/00004623-200410000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H. The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13:193–196. doi: 10.1007/s00167-004-0557-x. [DOI] [PubMed] [Google Scholar]
- 4.Bourne R, Mukhi S. Role of obesity on the risk for total hip or knee arthroplasty. Clin Orthop Relat Res. 2007;465:185–188. doi: 10.1097/BLO.0b013e3181576035. [DOI] [PubMed] [Google Scholar]
- 5.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, et al. Knee replacement. Lancet. 2010;379:1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 6.De Boer JJ, Blankevoort L, Kingma I, Vorster W. In vitro study of inter-individual variation in posterior slope in the knee joint. Clinical Biomechanics. 2009;6:488–492. doi: 10.1016/j.clinbiomech.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 7.Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35:1443–1449. doi: 10.1177/0363546507304665. [DOI] [PubMed] [Google Scholar]
- 8.Han HS, Chang CB, Seong SC, Lee S, Lee MC. Evaluation of anatomic references for tibial sagittal alignment in total kneearthroplasty. Knee Surg Sports Traumatol Arthrosc. 2008;16:373–377. doi: 10.1007/s00167-008-0486-1. [DOI] [PubMed] [Google Scholar]
- 9.Hofmann AA, Bachus KN, Wyatt RW. Effect of the tibial cut on subsidence following total knee arthroplasty. Clin Orthop Relat Res. 1991;269:63–69. [PubMed] [Google Scholar]
- 10.Kastner N, Gruber G, Aigner BA, Friesenbichler J, Pechmann M, Fürst F, Vavken P, Leithner A, Sadoghi P. Sex-related outcome differences after implantation of low-contact stress mobile-bearing total knee arthroplasty. Int Orthop. 2012;36:1393–1397. doi: 10.1007/s00264-012-1486-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kastner N, Gruber G, Sadoghi P. Can we always trust in the computer? Adequate tibial alignment and flexion-gap balancing using personalised knee arthroplasty cutting blocks. Int Orthop. 2012;36:2395. doi: 10.1007/s00264-012-1647-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kennedy JW, Johnston L, Cochrane L, Boscainos PJ (2013) Total knee arthroplasty in the elderly: Does age affect pain, function or complications? Clinical Orthopaedics and Related Research® [Internet]. 2013 Jan 25 [cited 2013 Mar 11] [DOI] [PMC free article] [PubMed]
- 13.Sadoghi P, Kastner N. Size measurement and flexion gap balancing in total knee arthroplasty – new benefits of the AttuneTM system? Int Orthop. 2013;37(10):2105. doi: 10.1007/s00264-013-1953-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, Labek G. Revision surgery after total joint arthroplasty: A complication-based analysis using worldwide arthroplasty registers. J Arthroplasty. 2013 doi: 10.1016/j.arth.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Seo SS, Kim CW, Kim JH, Min YK. Clinical Results Associated with Changes of Posterior Tibial Slope in Total Knee Arthroplasty. Knee Surg Relat Res. 2013;25:25. doi: 10.5792/ksrr.2013.25.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Todd MS, Laliss S, Garcia E, DeBerardino TM, Cameron KL. The Relationship Between Posterior Tibial Slope and Anterior Crucitae Ligament Injuries. Am J Sports Med. 2010;38(1):63–67. doi: 10.1177/0363546509343198. [DOI] [PubMed] [Google Scholar]
- 17.Utzschneider S, Goettinger M, Weber P, Horng A, Glaser C, Jansson V, et al. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011;19:1643–1648. doi: 10.1007/s00167-011-1414-3. [DOI] [PubMed] [Google Scholar]
- 18.Vasarhelyi EM, MacDonald SJ. The influence of obesity on total joint arthroplasty. Journal of Bone and Joint Surgery - British. 2012;94-B(11_Supple_A):100–102. doi: 10.1302/0301-620X.94B11.30619. [DOI] [PubMed] [Google Scholar]
- 19.Whiteside LA, Amador DD. The effect of posterior tibial slope on knee stability after Ortholoc total knee arthroplasty. J Arthroplasty. 1988;3(Suppl):S51–S57. doi: 10.1016/S0883-5403(88)80009-3. [DOI] [PubMed] [Google Scholar]
- 20.Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg. 1998;80:1770–1774. doi: 10.2106/00004623-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 21.www.depuysynthes.com [last accessed the 31st of July 2013]
- 22.www.orthopaedicscores.com [last accessed the 31st of July 2013]
- 23.www.psycho.uni-duesseldorf.de/abteilungen/aap/gpower3 [last accessed the 31st of July 2013]
- 24.Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK. Anatomical references to assess the posterior tibial slope in total knee arthroplasty: A comparison of 5 anatomical axes. J Arthroplasty. 2008;23:586–592. doi: 10.1016/j.arth.2007.05.006. [DOI] [PubMed] [Google Scholar]