Abstract
Purpose
So far, controversy still exists regarding the use of non-continuous or continuous wound drainage after total knee arthroplasty. The aim of this study was to assess the efficacy and safety of these two drainage techniques after total knee arthroplasty.
Methods
We searched the established electronic literature databases of Pubmed, Embase, Cochrane Library, CNKI, VIP and WANFANG. Nine RCTs including a total of 761 patients involving 811 knees were eligible for this meta-analysis.
Results
Our results showed that non-continuous drainage was associated with less haemoglobin loss (WMD, −0.43, 95 % CI −0.62 to −0.24; P < 0.00001) and postoperative visible blood loss (WMD, −305.09, 95 % CI −408.10 to −202.08; P < 0.00001) compared with continuous drainage. No significant difference was found between the two groups in terms of range of motion (WMD, 0.99, 95 % CI −1.01 to 2.98; P = 0.33), incidence of blood transfusion (OR, 0.63, 95 % CI 0.38 to 1.06; P = 0.80) or postoperative complications (OR, 1.09, 95 % CI 0.35 to 3.40; P = 0.89).
Conclusion
The existing evidence indicates that non-continuous drainage can achieve less haemoglobin loss (especially the four- to six-hour drain clamping) and postoperative visible blood loss with no increased risk of postoperative complications compared with continuous drainage.
Keywords: Meta-analysis, Drain clamping, Total knee arthroplasty
Introduction
Total knee arthroplasty (TKA), as a major orthopaedic operation, is associated with risks of significant blood loss and need for blood transfusion due to its extensive soft tissue release and bone cuts. A number of methods [3, 5, 10, 11, 13, 14, 18, 20, 21, 25, 31, 33, 35] including drain clamping have been proposed to reduce blood loss and so avoid homologous blood transfusion, which may carry an underlying risk for the transmission of viral infection and immunological reactions [9, 28]. Recently, drain clamping has attracted an increasing amount of attention [1, 2, 23, 27, 32]. However, controversy still exists regarding whether non-continuous drainage (drainage clamping) or continuous drainage (no drainage clamping) is preferable after TKA. On the one hand, continuous drainage (CON) theoretically prevents haematoma formation and thus reduces postoperative pain, swelling and incidence of infection [6, 7], whereas it may lead to increased bleeding. On the other hand, non-continuous drainage (NON) including temporary and intermittent clamping creates a tamponade effect for bleeding control [16, 22], although it may induce immediate wound complications [15].
A previously published systematic review [32] regarding this topic attempted to answer the question. This study compared many variables between the two drainage methods and has four aspects which can be improved. Firstly, a chosen RCT [34] evaluated the efficacy of clamping the drains after intra-articular injection of saline with 1:500,000 adrenaline compared with post-operative blood salvage in reducing blood loss. However, both intra-articular injection of adrenaline and use of blood salvage can bring predictable bias and should not be included. Secondly, “postoperative haemoglobin level”, one of the outcome variables adopted in their analysis, may not be able to precisely reflect the changes between pre- and post-operative haemoglobin. Thirdly, due to the absence of standard deviations in an included trial [8], the authors estimated the standard deviations based on the range of data value, assuming the data as normally distributed data, which will inevitably generate bias. Finally, heterogeneity was not further investigated using subgroup analysis or sensitivity analysis. Therefore, we systematically conducted this meta-analysis with all the up-to-date RCTs concerning the topic of NON versus CON after TKA to compare their effectiveness and safety, with a view to provide more accurate evidence for surgeons when making a clinical decision.
Materials and methods
Search methods
A comprehensive search of unrestricted language literature of all studies comparing NON with CON after primary TKA was conducted through the electronic literature databases of PubMed, EMBase, Cochrane Library, CNKI, VIP, and WANFANG. Retrieval time was from the time when databases were built to May 2013. Manual searches of relevant trials, reviews and related articles were also performed. This process was performed iteratively until no additional articles could be identified.
Inclusion criteria
All randomised controlled trials comparing NON with CON after primary TKA were eligible. All kinds of prostheses were considered for this review. The article published most recently or with the highest quality would be chosen if more than one article of the same study met the criteria. Trials involving haemostasis methods of intra-articular injection of diluted adrenalin solution or tranexamic acid were excluded. All non-randomised trials and quasi-randomised trials were also excluded.
Outcomes of interest and definition
The primary outcomes of interest include haemoglobin loss and range of motion. Haemoglobin loss was calculated by subtracting the postoperative haemoglobin concentration from the preoperative haemoglobin concentration. The secondary outcomes consist of postoperative visible blood loss, incidence of blood transfusion and complications. Complications were further stratified into three categories. The first subgroup is wound infection including stitch abscess, superficial and deep infection. The second subgroup includes other wound complications which consist of bruising, haematoma formation, blistering, serous ooze and stiffness. The third subgroup includes thromboembolic events containing pulmonary embolism and deep venous embolism.
Data extraction
We extracted the following data from the included articles: authors, publication date, number of patients and knees, gender percentage, age, body mass index, diagnosis, description of interventions, methods of non-continuity, total time of drain clamping, time of removing the drain after operation, use of tourniquet, and outcome measures in both control and experiment groups. These data were then compiled into a standard table. Two review authors (Li T and Zhou L) independently extracted the data from all eligible randomised controlled trials. Any disagreement was resolved by discussion with the senior review author (Weng XS). When the available data was not adequate for the meta-analysis, communication with the primary authors was made for more information and clarification of data through e-mail.
Methodological quality assessment
Two review authors (Bian YY and Zhuang QY) independently used the Cochrane Collaboration recommendations [12] to assess methodological quality of clinical trials. The following information was evaluated: random sequence generation, allocation concealment, blinding of outcome assessments, incomplete outcome data, selective reporting and other bias. An arbiter (Weng XS) was consulted to reconcile any disagreement.
Statistical analysis
For each included study, odds ratio (OR) and 95 % confidence intervals (CI) were calculated for dichotomous outcomes, and weighted mean differences (WMD) and 95 % CI were calculated for continuous outcomes. Statistical heterogeneity was assessed using the value of I2 and the result of the chi-squared test. A p value >0.1 and an I2 value ≤50 % were considered suggestive of no statistical heterogeneity and a fixed effect model was used to estimate the overall summary effect sizes. Otherwise, a random effect model was adopted and further subgroup analysis or sensitivity analysis was performed to explore the potential sources of heterogeneity. All analyses were done with Review Manager Software (RevMan5.2) and the level of significance was set at P < 0.05. A funnel plot based on the primary outcome was conducted to assess the publication bias.
Results
Characteristics of selected studies
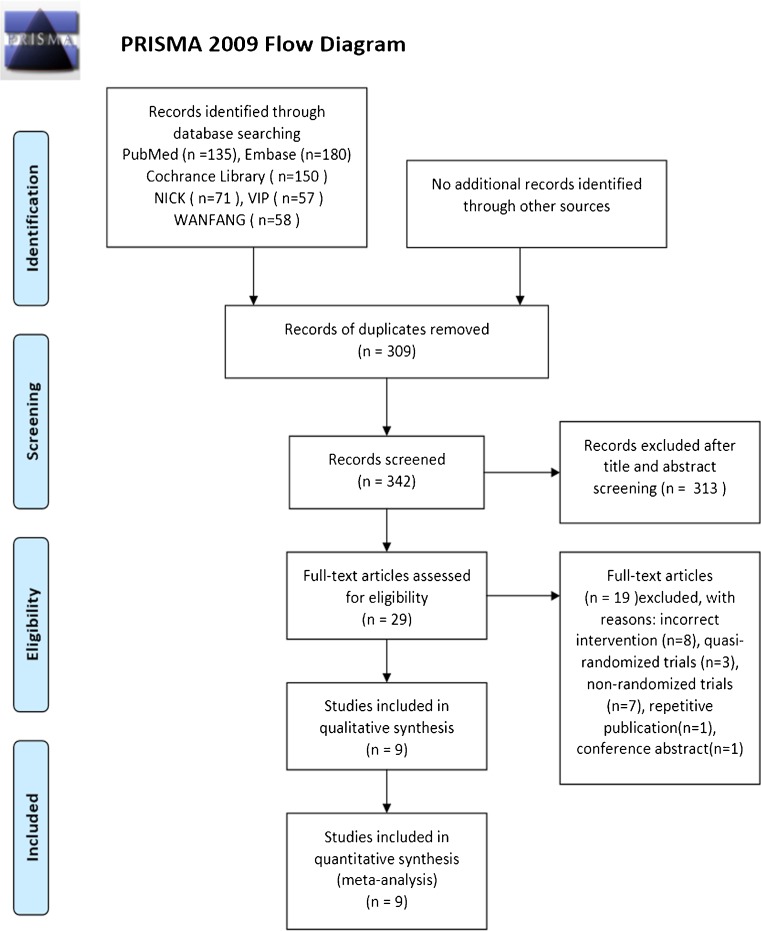
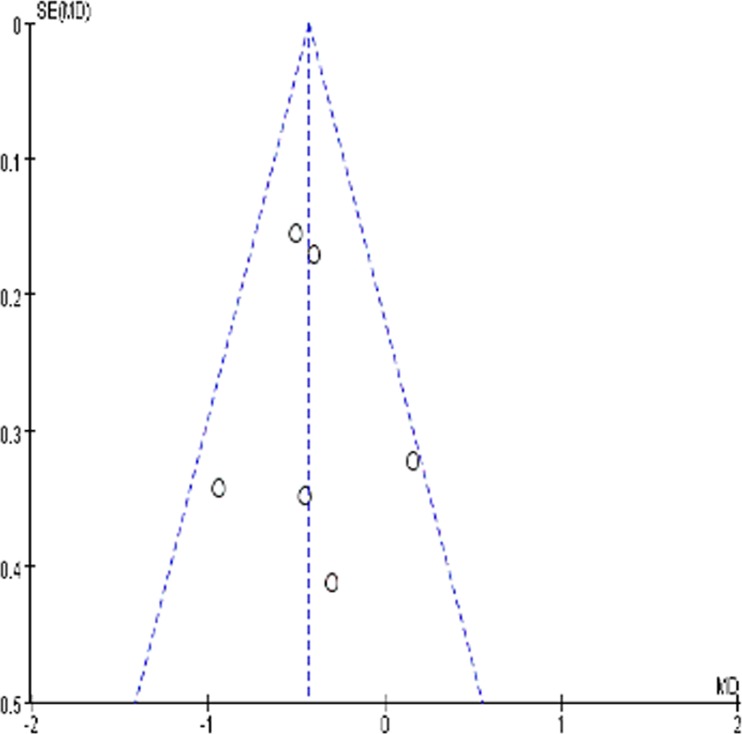
The details of literature search and selection are displayed in the PRISMA 2009 Flow Diagram (Fig. 1). We finally identified nine randomised controlled trials [4, 8, 16, 19, 22, 24, 26, 29, 30] associated with NON versus CON. A total of 761 patients involving 811 knees ranging from 60 to 120 in each trial were included. All selected studies were in English and were published between 2001 and 2012. Temporary drain clamping was adopted by six trials [8, 16, 19, 26, 29, 30] and intermittent drain clamping was used by three trials [4, 22, 24] in the experiment group. The period of drain clamping ranged from one hour to 23 hours and 35 minutes. The detailed characteristics of these studies are demonstrated in Table 1. A funnel plot based on the haemoglobin loss indicated minimal publication bias (Fig. 2).
Fig. 1.
PRISMA 2009 flow diagram
Table 1.
Characteristics of included studies
| Reference | No. of patients | No. of knees | Female (%) | Age (years) | BMI | Diagnosis | Methods of non-continuity | Total time of clamping | Time of removing drain | Use of tourniquet | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NON | CON | NON | CON | NON | CON | NON | CON | |||||||
| Kiely et al. (2001) [16] | 76 | 31 | 45 | NA | NA | NA | NA | NA | NA | NA | Temporary | 2 h | 48 h | Yes |
| Pornrattanamaneewong et al. (2012) [22] | 100 | 50 | 50 | 84 | 88 | 68.2 | 69.5 | 27.9 | 27.3 | OA | Intermittent | 6 h | 48 h | Yes |
| Shen et al. (2005) [29] | 89 | 43 | 46 | 83.7 | 93.5 | 65 | 68 | 26.3 | 27.5 | OA, RA | Temporary | 4 h | 72 h | Yes |
| Eum et al. (2006) [8] | 100 | 50 | 50 | 98 | 98 | 68.1 | 67.9 | NA | NA | OA, ON | Temporary | 1 h | 48 h | Yes |
| Roy et al. (2006) [26] | 100 | 50 | 50 | NA | NA | NA | NA | NA | NA | OA, RA | Temporary | 1 h | 48 h | Yes |
| Raleigh et al. (2007) [24] | 66 | 34 | 32 | 52 | 48–87 | NA | NA | NA | Intermittent | 23 h and 35 m | 24 h | Yes | ||
| Stucinskas et al. (2009) [30] | 60 | 30 | 30 | 76.7 | 90 | 67 | 70 | 32 | 31 | OA | Temporary | 4 h | 48 h | Yes |
| Madadi et al. (2010) [19] | 50 | 50 | 50 | 76 | 60–75 | 23.2 | OA | Temporary | 12 h | 24 h | No | |||
| Chareancholvanich et al. (2012) [4] | 120 | 60 | 60 | 83.3 | 86.7 | 69.8 | 69.8 | NA | NA | OA | Intermittent | 6 h | 48 h | Yes |
NON non-continuous drainage, CON continuous drainage, OA osteoarthritis, RA rheumatoid arthritis, ON osteonecrosis, NA indicates not available, BMI body mass index
Fig. 2.
A funnel plot based on the haemoglobin loss
Risk of bias in included studies
Generally speaking, the methodological quality of all the included trials was found to be moderate risk of bias according to the Cochrane Collaboration recommendations. The adequate randomisation technique including a computer-generated number [4, 22] and a random numbered envelope [16, 19, 24, 26, 30] was mentioned in seven trials, while in one trial [8] it was not reported how the random sequence generation was exactly performed. Allocation concealment was mentioned in six trials [4, 16, 19, 22, 29, 30] and unclear in three studies [8, 24, 26]. Outcome evaluators were blinded in one trial [19], but we could not determine the blinding in the other eight trials. The detailed risk of bias of methodological quality in the included studies is elaborated in Table 2.
Table 2.
Quality assessment of risk of bias in included studies
| References | Random sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Free of selective reporting | Free of other bias |
|---|---|---|---|---|---|---|
| Kiely et al. (2001) [16] | Yes | Yes | Unclear | Yes | Yes | Unclear |
| Pornrattanamaneewong et al. (2012) [22] | Yes | Yes | Unclear | Yes | Yes | Unclear |
| Shen et al. (2005) [29] | No | Yes | Unclear | Yes | Yes | Unclear |
| Eum et al. (2006) [8] | Unclear | Unclear | Unclear | Yes | Yes | Unclear |
| Roy et al. (2006) [26] | Yes | Unclear | Unclear | Yes | Yes | Unclear |
| Raleigh et al. (2007) [24] | Yes | Unclear | Unclear | Yes | Yes | Unclear |
| Stucinskas et al. (2009) [30] | Yes | Yes | Unclear | Yes | Yes | Unclear |
| Madadi et al. (2010) [19] | Yes | Yes | Yes | Yes | Yes | Unclear |
| Chareancholvanich et al. (2012) [4] | Yes | Yes | Unclear | Yes | Yes | No |
‘Yes’ indicates low risk of bias, ‘Unclear’ indicates unclear risk of bias, ‘No’ indicates high risk of bias
Meta-analysis results
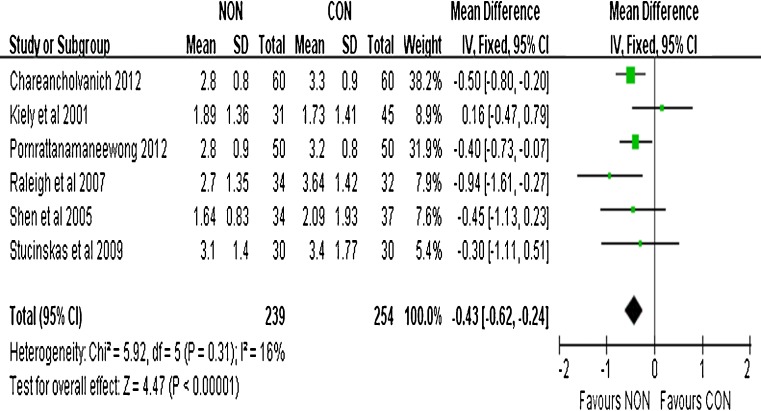
Haemoglobin loss
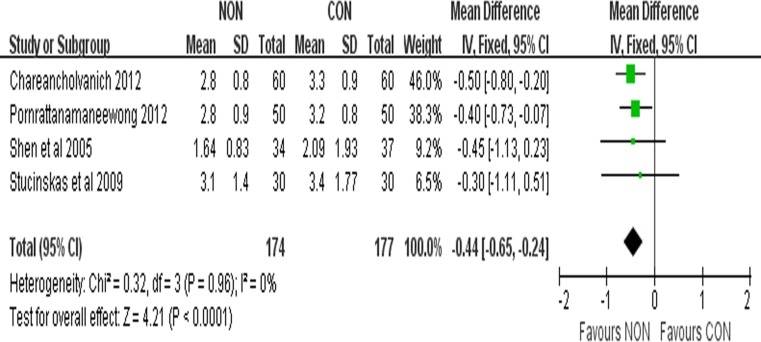
Seven studies consisting of 593 participants reported the results of haemoglobin level before and after operation. Due to the absence of detailed outcomes in one trial [8], we just pool the other six results in this meta-analysis. Pooled analysis shows that NON is associated with less haemoglobin loss compared to CON (WMD, −0.43; 95 % CI −0.62 to −0.24; P < 0.00001; fixed effect model) with low heterogeneity (P = 0.31, I2 = 16 %) (Fig. 3). In order to further eliminate the heterogeneity, a sensitivity analysis was conducted after two RCTs [16, 24] being excluded and the forest plot was present in Fig. 4. The sensitivity analysis also reveals significant difference (WMD, −0.44; 95 % CI −0.65 to −0.24; P < 0.0001; fixed effect model) with no heterogeneity (P = 0.96, I2 = 0 %) between the two groups (Fig. 4), which was in line with our previous analysis.
Fig. 3.
Forest plot of weighted mean differences (WMD) with confidence intervals for haemoglobin loss
Fig. 4.
Forest plot of weighted mean differences (WMD) with confidence intervals for the sensitivity analysis of haemoglobin loss
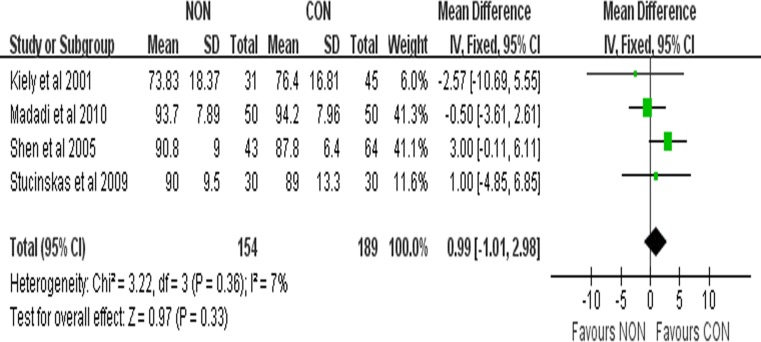
The range of motion
Four studies included in this meta-analysis reported the range of motion of knees in trials. There was no significant difference between the two groups for the range of motion of knees (WMD, 0.99; 95 % CI −1.01 to 2.98; P = 0.33; fixed effect model) with low heterogeneity (P = 0.36, I2 = 7 %) (Fig. 5).
Fig. 5.
Forest plot of weighted mean differences (WMD) with confidence intervals for range of motion
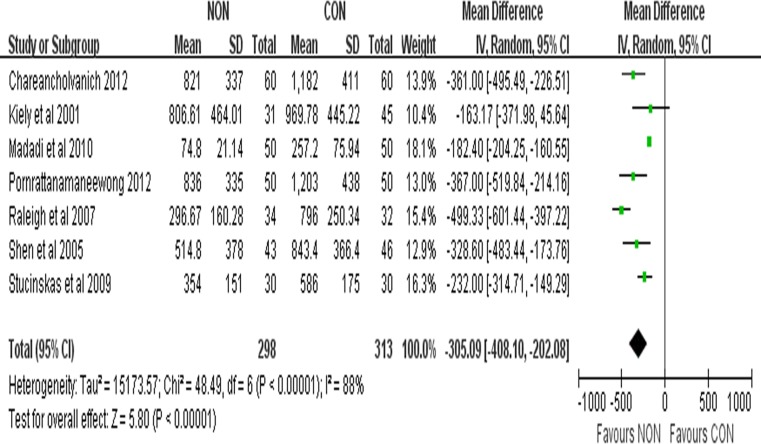
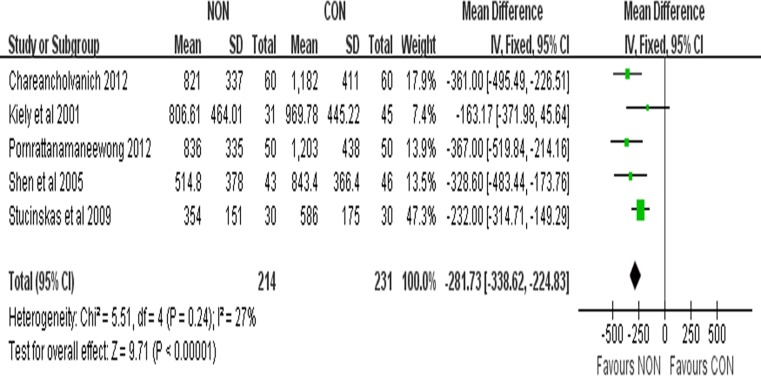
Postoperative visible blood loss
Seven studies consisting of 611 patients reported the results of postoperative visible blood loss. Because of the high heterogeneity (P < 0.00001,< I2 = 88 %), a random effect model was adopted to pool the data. Our pooled results showed that NON can reduce postoperative visible blood loss when compared with CON (WMD, −305.09; 95 % CI −408.10 to −202.08; P < 0.00001) (Fig. 6). A further sensitivity analysis was undertaken after two RCTs [19, 24] were excluded, and the results are presented in Fig. 7. The sensitivity analysis showed a significant difference (WMD, −281.73; 95 % CI −338.62 to −224.83; P < 0.00001; fixed effect model) with low heterogeneity (P = 0.24, I2 = 27 %) between the two groups (Fig. 7), which was consistent with our previous analysis.
Fig. 6.
Forest plot of weighted mean differences (WMD) with confidence intervals for postoperative visible blood loss
Fig. 7.
Forest plot of weighted mean differences (WMD) with confidence intervals for the sensitivity analysis of postoperative visible blood loss
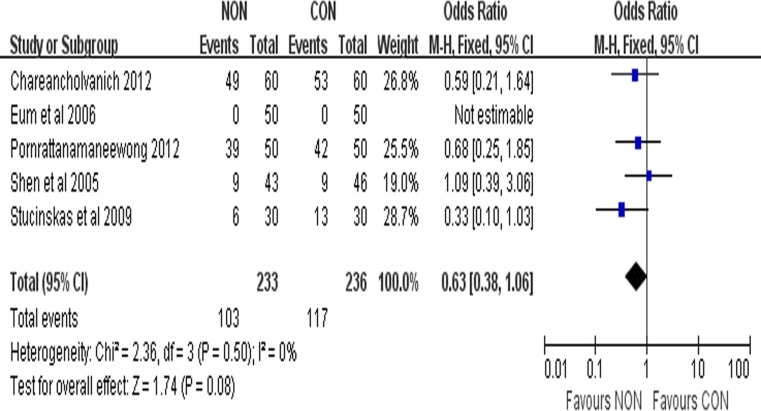
Incidence of blood transfusion
Five studies consisting of 469 participants reported the result of transfusion rate. The incidence of blood transfusion was 44.21 % (103/233) in the NON group and 49.58 % (117/236) in the CON group. There was no significant difference between the two groups (OR, 0.63; 95 % CI 0.38 to 1.06; P = 0.80; fixed effect model) with no heterogeneity (P = 0.50, I2 = 0 %) (Fig. 8).
Fig. 8.
Forest plot of odds ratio (OR) with confidence intervals for the incidence of blood transfusion
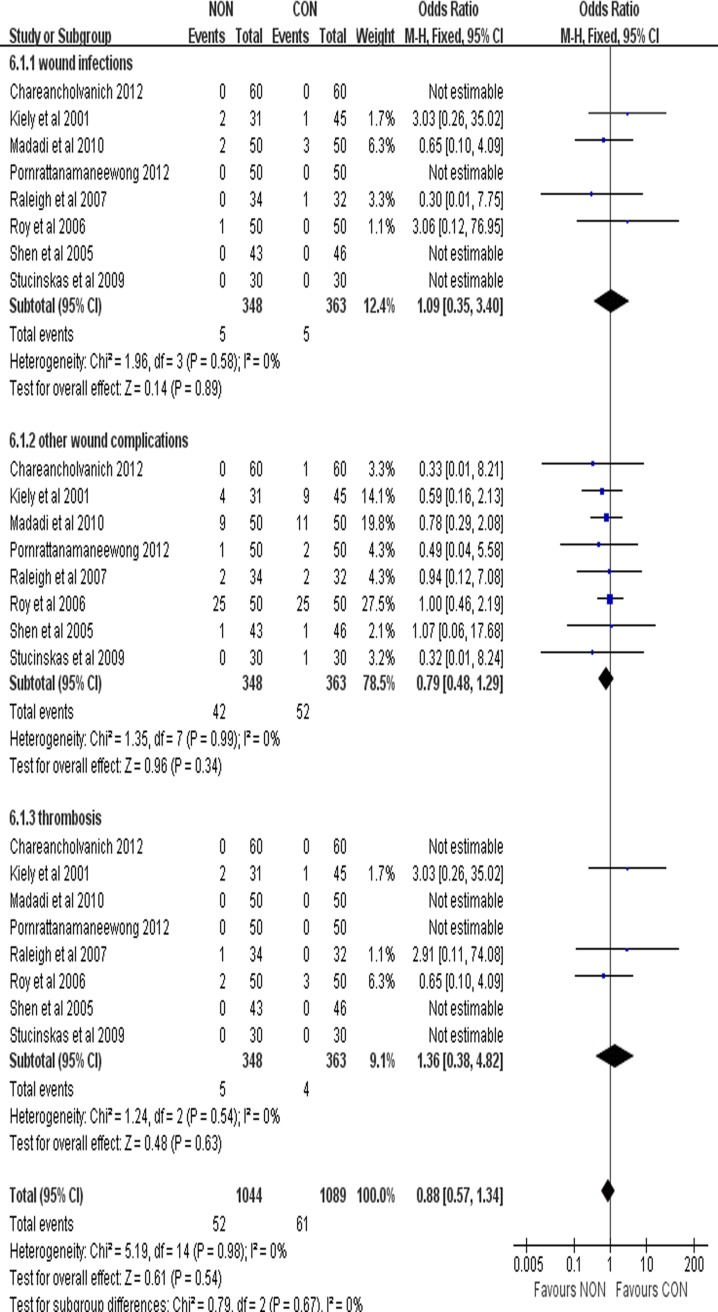
Complications
There was no significant difference between the two groups in terms of wound infection (OR, 1.09; 95 % CI 0.35 to 3.40; P = 0.89; fixed effect model), other wound complications (OR, 0.79; 95 % CI 0.48 to 1.29; P = 0.34; fixed effect model) and thromboembolic events (OR, 1.36; 95 % CI 0.38 to 4.82; P = 0.63; fixed effect model) with no heterogeneity (Fig. 9). The odds ratio (OR) of all complication rates was 0.88 (95 % CI 0.57 to 1.34; P = 0.54; fixed effect model) indicating that complication rate in NON was similar to that in CON (Fig. 9).
Fig. 9.
Forest plot of odds ratio (OR) with confidence intervals for complications
Discussion
While the use of closed suction drains in TKA is quite common at present, controversy still exists regarding the pros and cons of its use. In order to avoid postoperative blood loss and transfusion, more and more surgeons consider the drain clamping approach which may create a tamponade effect and control the postoperative blood loss. Several trials [17, 22, 24, 26, 29, 30] show that clamping the drain can reduce the postoperative blood loss and haemoglobin loss without increasing wound complications and clinical thromboembolic events. Nevertheless, other surgeons found no difference in total blood loss and haemoglobin between non-continuous and continuous wound drainage after TKA [15, 16, 19]. So far, consensus has not been achieved for the use of non-continuous or continuous wound drainage.
A previous systematic review [32] consisting of six randomised controlled trials involving 603 knees was performed concerning the above issue. The results demonstrated that drain clamping could decrease the volume of drainage, but only clamping for no less than four hours could reduce the true blood loss (haemoglobin loss). There was no significant difference between the two groups regarding blood transfusion rate, postoperative range of motion, incidence of thromboembolic events, and wound complications. This study which compared many variables of the two drainages has four limitations as discussed above, which necessitate the analysis in our study. Discussions on the results of our meta-analysis were as follows.
Theoretically, NON can decrease the postoperative haemoglobin drop after TKA because NON can promote haematoma formation which temporarily creates a tamponade effect. However, results of some studies were opposed to this view although some other trials were supportive of the theory. The previous meta-analysis which adopted postoperative haemoglobin level to estimate the haemoglobin loss showed no significant difference between the two groups, but only clamping for no less than four hours could reduce the haemoglobin loss. Unfortunately, postoperative haemoglobin level may not be able to precisely reflect the haemoglobin loss due to the individual variation. In our meta-analysis, we adopted the postoperative haemoglobin change to assess the true blood loss. This variable is obviously more accurate than postoperative haemoglobin level used by Tai et al. [32]. Seven trials reported the results of pre- and post-operative haemoglobin level. Since one article [8] reported data as mean and range rather than standard deviation, we just pooled the other six trials so as to avoid the relevant bias. Compared with the CON, the pooled result showed that NON can significantly decrease the haemoglobin loss (P < 0.00001) with low heterogeneity (P = 0.31, I2 = 16 %), which is different to the previous meta-analysis. In spite of the acceptable heterogeneity as it was, we decided to further eliminate the heterogeneity considering the clinical significance of this variable as our primary outcome. We believed that the various drain clamping methods used in these trials contribute to the heterogeneity. To be specific, the period of drain clamping varied from one hour to 23 hours and 35 minutes in our included studies. Among which, one trial [16] adopted temporary drain clamping for one hour and the other [24] used intermittent drain clamping for 23 hours and 35 minutes (the drains clamped for 115 minutes and released for 5 minutes every two hours until six hours postoperatively, then only unclamped for the last five minutes at 12 and 24 hours). These two studies which used the drain clamping with the period being either too short or too long were thus excluded. We then conducted a sensitivity analysis of the other four trials in which drain clamping was performed for four to six hours. Our pooled results with no heterogeneity (P = 0.96, I2 = 0 %) showed that NON can significantly decrease the haemoglobin loss, which was consistent with our previous analysis. The systematic review conducted by Tai et al. [32] claimed that drain clamping for no less than four hours can decrease the reduction in haemoglobin levels, while not offering the upper limit. Because a recent study [36] reported that there were significantly more complications using the too-long drain clamping method, we regarded it necessary to define an appropriate upper limit in order to avoid unnecessary complications. Based on our results and the above analysis, we believe that four to six hours of drain clamping may be the optimal strategy.
To further investigate the potential blood saving advantage of NON, we explored two secondary outcomes concerning blood loss which include postoperative visible blood loss and incidence of blood transfusion in the included trials. Firstly, with regard to the postoperative visible blood loss, the mean of the total drained blood ranged from 74.8 to 821 ml in the NON group and 257.2 to 1203 ml in the CON group. The pooled results with high heterogeneity (P < 0.00001, I2 = 88 %) showed that there was a significant difference between NON and CON. All trials enrolled in this meta-analysis used the tourniquet to control the intraoperative bleeding except for one [19] which adopted a leg holder instead, keeping the leg in a flexion position (80–110°). We thought that this approach might induce more intraoperative blood loss and contribute to the heterogeneity. Another RCT [24] may have brought in heterogeneity on the ground such that the period of drain clamping was too long, which was different from other trials included. Therefore, a further sensitivity analysis was conducted after these two RCTs [19, 24] were excluded, and the pooled results with low heterogeneity (P = 0.24, I2 = 27 %) were in agreement with our previous analysis—NON can obtain less postoperative visible blood loss compared with CON. Secondly, the incidence of blood transfusion for NON was 44.21 % (103/233) and for CON it was 49.58 % (117/236), and there is no significant difference between NON and CON.
In short, from the above analysis, we can draw a conclusion that NON can achieve less haemoglobin loss, and postoperative visible blood loss when compared with CON, and four to six hours of drain clamping after TKA may be a better choice.
Range of motion is another important concern for both surgeons and patients to evaluate the effectiveness of TKA. Surgeons may assume that NON have inferior joint function due to the swelling of knee after the drain clamping. However, no significant difference between the two groups was found in our meta-analysis, which was in agreement with the previous meta-analysis [16]. It is worth noting that the timing of measuring the range of motion in the pooled data varied from six days to two weeks postoperatively. A study conducted by Madadi et al. [19] showed that the range of motion was not significantly different between the two groups after three months, which was consistent with previous studies [17, 34]. Roy et al. [26] adopted time to regain 80° flexion to assess postoperative range of motion. Their results revealed that average time to regain 80° flexion was 11.5 days in the NON group and 14.3 days in the CON group, with no statistically significant difference between the two groups. Therefore, both our analysis and previous studies suggest that NON can achieve similar postoperative range of motion compared with CON, although NON may lead to initial swelling and blistering of the knee.
Wound infection is a serious complication after TKA, which may prolong the length of hospital stay and even induce the prosthesis infection. It is postulated that the blood deposited in the articular cavity may provide a medium for bacteria breeding, which increase the risk of wound infection. What is more, previous studies [15, 36] have shown that non-continuous wound drainage after TKA increases the risk of postoperative complications. However, no significant difference was found in our analysis between the NON group and the CON group in terms of wound infection and other wound complications, indicating that drain clamping did not significantly increase the risk of wound complication.
Thromboembolism, including pulmonary embolism and deep venous embolism, has been a great concern after TKA because it can lead to high morbidity and mortality. Our analysis found no significant difference between the NON group and the CON group, which indicates that the drain clamping is not a risk factor. In one included trial, a patient [19] experienced an episode of transient hypotension upon release of the drains that resolved spontaneously in the NON group. This might have been due to sudden blood loss occurring from the knee after release of the tamponade effect. Another trial [24] reported that two patients in each group with stiffness required manipulation under anaesthesia.
Compared with the previous systematic review [32], there are several strengths in this meta-analysis. Firstly, this meta-analysis adopted more strict inclusion criteria. Drain clamping with intra-articular injection of diluted adrenalin solution or tranexamic acid were strictly excluded in this study in order to guarantee the reliability and stability of results. Secondly, the variable “postoperative haemoglobin change” adopted in our meta-analysis is more accurate than the “postoperative haemoglobin level” used by Tai et al. [32], which contributes to the strength of conclusions drawn from the meta-analysis. Thirdly, complications were further stratified into wound infection, other wound complications and relevant thromboembolism, avoiding the deviation of all pooled complications. Finally, heterogeneity was further investigated and illustrated using the sensitivity analysis.
Despite these advantages, some limitations of the present meta-analysis were recognised. First, the number of studies included in the meta-analysis was still relatively small. Second, various types of prostheses involved in this study may bring out related performance bias. Third, the results of range of motion measured at different times postoperatively and which varied from six days to two weeks were pooled, which may contribute to relevant detection bias.
In short, as an up-to-date and objective study concerning drain clamping so far, our study suggests that non-continuous drainage can achieve less haemoglobin loss (especially the four- to six-hour drain clamping) and postoperative visible blood loss with no increased risk of postoperative complications compared with continuous drainage. No significant difference was found between the two groups with regard to range of motion and the blood transfusion incidence. Large sample multi-centre randomised controlled studies are required in the future to verify these meta-analysis results.
Acknowledgments
Source of funding
No funding source was involved in this study.
References
- 1.Aksoy Y, Altinel L, Kose KC. The comparison of the effects of intraoperative bleeding control and postoperative drain clamping methods on the postoperative blood loss and the need for transfusion following total knee arthroplasty. Acta Orthop Traumatol Turc. 2011;45:190–194. doi: 10.3944/AOTT.2011.2398. [DOI] [PubMed] [Google Scholar]
- 2.Berman AT, Fabiano D, Bosacco SJ, Weiss AA. Comparison between intermittent and continuous closed suction drainage of orthopedic wounds: a controlled clinical trial. Orthopedics. 1990;13:314–317. doi: 10.3928/0147-7447-19900301-10. [DOI] [PubMed] [Google Scholar]
- 3.Camarasa MA, Olle G, Serra-Prat M, Martin A, Sanchez M, Ricos P, Perez A, Opisso L. Efficacy of aminocaproic, tranexamic acids in the control of bleeding during total knee replacement: a randomized clinical trial. Br J Anaesth. 2006;96:576–582. doi: 10.1093/bja/ael057. [DOI] [PubMed] [Google Scholar]
- 4.Chareancholvanich K, Siriwattanasakul P, Narkbunnam R, Pornrattanamaneewong C. Temporary clamping of drain combined with tranexamic acid reduce blood loss after total knee arthroplasty: a prospective randomized controlled trial. BMC Musculoskelet Disord. 2012;13:124–129. doi: 10.1186/1471-2474-13-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cid J, Lozano M. Tranexamic acid reduces allogeneic red cell transfusions in patients undergoing total knee arthroplasty: results of a meta-analysis of randomized controlled trials. Transfusion. 2005;45:1302–1307. doi: 10.1111/j.1537-2995.2005.00204.x. [DOI] [PubMed] [Google Scholar]
- 6.Crevoisier XM, Reber P, Noesberger B. Is suction drainage necessary after total joint arthroplasty? A prospective study. Arch Orthop Trauma Surg. 1998;117:121–124. doi: 10.1007/s004020050210. [DOI] [PubMed] [Google Scholar]
- 7.Esler CN, Blakeway C, Fiddian NJ. The use of a closed-suction drain in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Br. 2003;85:215–217. doi: 10.1302/0301-620X.85B2.13357. [DOI] [PubMed] [Google Scholar]
- 8.Eum DS, Lee HK, Hwang SY, Park JU. Blood loss after navigation-assisted minimally invasive total knee arthroplasty. Orthopedics. 2006;29:S152–S154. [PubMed] [Google Scholar]
- 9.Gascon P, Zoumbos NC, Young NS. Immunologic abnormalities in patients receiving multiple blood transfusions. Ann Intern Med. 1984;100:173–177. doi: 10.7326/0003-4819-100-2-173. [DOI] [PubMed] [Google Scholar]
- 10.Gibbons CE, Solan MC, Ricketts DM, Patterson M. Cryotherapy compared with Robert Jones bandage after total knee replacement: a prospective randomized trial. Int Orthop. 2001;25:250–252. doi: 10.1007/s002640100227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han CD, Shin DE. Postoperative blood salvage and reinfusion after total joint arthroplasty. J Arthroplasty. 1997;12:511–516. doi: 10.1016/S0883-5403(97)90173-X. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JPT, Altman DG (2008) Assessing risk of bias in included studies. In: Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions. Wiley, pp 187–241
- 13.Ishida K, Tsumura N, Kitagawa A, Hamamura S, Fukuda K, Dogaki Y, Kubo S, Matsumoto T, Matsushita T, Chin T, Iguchi T, Kurosaka M, Kuroda R. Intra-articular injection of tranexamic acid reduces not only blood loss but also knee joint swelling after total knee arthroplasty. Int Orthop. 2011;35(11):1639–1645. doi: 10.1007/s00264-010-1205-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Juelsgaard P, Larsen UT, Sorensen JV, Madsen F, Soballe K. Hypotensive epidural anesthesia in total knee replacement without tourniquet: reduced blood loss and transfusion. Reg Anesth Pain Med. 2001;26:105–110. doi: 10.1053/rapm.2001.21094. [DOI] [PubMed] [Google Scholar]
- 15.Jung WH, Chun CW, Lee JH, Ha JH, Kim JH, Jeong JH (2012) No difference in total blood loss, haemoglobin and haematocrit between continues and intermittent wound drainage after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. Oct 23. [Epub ahead of print] [DOI] [PubMed]
- 16.Kiely N, Hockings M, Gambhir A. Does temporary clamping of drains following knee arthroplasty reduce blood loss? A randomised controlled trial. Knee. 2001;8:325–327. doi: 10.1016/S0968-0160(01)00095-3. [DOI] [PubMed] [Google Scholar]
- 17.Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total knee arthroplasties. Clin Orthop Relat Res. 1998;347:188–193. [PubMed] [Google Scholar]
- 18.Lwai T, Tsuji S, Tomita T, Sugamoto K, Hideki Y, Hamada M. Repeat-dose intravenous tranexamic acid further decreases blood loss in total knee arthroplasty. Int Orthop. 2013;37(3):441–445. doi: 10.1007/s00264-013-1787-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Madadi F, Mehrvarz AS, Madadi F, Boreiri M, Abachizadeh K, Ershadi A. Comparison of drain clamp after bilateral total knee arthroplasty. J Knee Surg. 2010;23:215–222. doi: 10.1055/s-0031-1271891. [DOI] [PubMed] [Google Scholar]
- 20.Martin A, von Strempel A. Transfusion of autologous blood from reinfusion systems in total knee arthroplasty. Int Orthop. 2006;30(6):541–544. doi: 10.1007/s00264-006-0127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orpen NM, Little C, Walker G, Crawfurd E. Tranexamic acid reduces early postoperative blood loss after total knee arthroplasty: a prospective randomized controlled trial of 29 patients. Knee. 2006;13:106–110. doi: 10.1016/j.knee.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Pornrattanamaneewong C, Narkbunnam R, Siriwattanasakul P, Chareancholvanich K. Three-hour interval drain clamping reduces postoperative bleeding in total knee arthroplasty: a prospective randomized controlled trial. Arch Orthop Trauma Surg. 2012;132:1059–1063. doi: 10.1007/s00402-012-1501-z. [DOI] [PubMed] [Google Scholar]
- 23.Prasad N, Padmanabhan V, Mullaji A. Comparison between two methods of drain clamping after total knee arthroplasty. Arch Orthop Trauma Surg. 2005;125:381–384. doi: 10.1007/s00402-005-0813-7. [DOI] [PubMed] [Google Scholar]
- 24.Raleigh E, Hing CB, Hanusiewicz AS, Fletcher SA, Price R. Drain clamping in knee arthroplasty, a randomized controlled trial. ANZ J Surg. 2007;77:333–335. doi: 10.1111/j.1445-2197.2007.04053.x. [DOI] [PubMed] [Google Scholar]
- 25.Raut VV, Stone MH, Wroblewski BM. Reduction of postoperative blood loss after press-fit condylar knee arthroplasty with use of a femoral intramedullary plug. J Bone Joint Surg Am. 1993;75:1356–1357. doi: 10.2106/00004623-199309000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Roy N, Smith M, Anwar M, Elsworth C. Delayed release of drain in total knee replacement reduces blood loss. A prospective randomised study. Acta Orthop Belg. 2006;72:34–38. [PubMed] [Google Scholar]
- 27.Sa-Ngasoongsong P, Channoom T, Kawinwonggowit V, Wora-tanarat P, Chanplakorn P, Wibulpolprasert B, Wongsak S, Udomsubpayakul U, Wechmongkolgorn S, Lekpittaya N. Postoperative blood loss reduction in computer-assisted surgery total knee replacement by low dose intra-articular tranexamic acid injection together with 2-hour clamp drain: a prospective triple-blinded randomized controlled trial. Orthop Rev. 2011;3(e12):51–56. doi: 10.4081/or.2011.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schreiber GB, Busch MP, Kleinman SH, Korelitz JJ. The risk of transfusion transmitted viral infections: the retrovirus epidemiology donor study. N Engl J Med. 1996;334:1685–1690. doi: 10.1056/NEJM199606273342601. [DOI] [PubMed] [Google Scholar]
- 29.Shen PC, Jou IM, Lin YT, Lai KA, Yang CY, Chern TC. Comparison between 4-hour clamping drainage and nonclamping drainage after total knee arthroplasty. J Arthroplasty. 2005;20:909–913. doi: 10.1016/j.arth.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 30.Stucinskas J, Tarasevicius S, Cebatorius A, Robertsson O, Smailys A, Wingstrand H. Conventional drainage versus four hour clamping drainage after total knee arthroplasty in severe osteoarthritis: a prospective, randomised trial. Int Orthop. 2009;33:1275–1278. doi: 10.1007/s00264-008-0662-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sundaram RO, Parkinson RW. Closed suction drains do not increase the blood transfusion rates in patients undergoing total knee arthroplasty. Int Orthop. 2007;31(5):613–616. doi: 10.1007/s00264-006-0232-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tai TW, Yang CY, Jou IM, Lai KA, Chen CH. Temporary drainage clamping after total knee arthroplasty: a meta-analysis of randomized controlled trials. J Arthroplasty. 2010;25:1240–1245. doi: 10.1016/j.arth.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 33.Tanaka N, Sakahashi H, Sato E, Hirose K, Ishima T. Timing of the administration of tranexamic acid for maximum reduction in blood loss in arthroplasty of the knee. J Bone Joint Surg Br. 2001;83:702–705. doi: 10.1302/0301-620X.83B5.11745. [DOI] [PubMed] [Google Scholar]
- 34.Tsumara N, Yoshiya S, Chin T, Shiba R, Kohso K, Doita M. A prospective comparison of clamping the drain or post-operative salvage of blood in reducing blood loss after total knee arthroplasty. J Bone Joint Surg Br. 2006;88:49–53. doi: 10.1302/0301-620X.88B1.16653. [DOI] [PubMed] [Google Scholar]
- 35.Wang GJ, Hungerford DS, Savory CG, Rosenberg AG, Mont MA, Burks SG, Mayers SL, Spotnitz WD. Use of fibrin sealant to reduce bloody drainage and hemoglobin loss after total knee arthroplasty: a brief note on a randomized prospective trial. J Bone Joint Surg Am. 2001;83-A:1503–1505. doi: 10.2106/00004623-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Yamada K, Imaizumi T, Uemura M, Takada N, Kim Y. Comparison between 1-hour and 24-hour drain clamping using diluted epinephrine solution after total knee arthroplasty. J Arthroplasty. 2001;16:458–462. doi: 10.1054/arth.2001.23620. [DOI] [PubMed] [Google Scholar]