Abstract
Purpose
The purpose of this prospective, randomised study was to evaluate long-term clinical results, radiographic findings, complications and revision and survivorship rates in patients <55 years at a minimum of 16 years after undergoing bilateral, sequential, simultaneous, cemented and cementless total knee arthroplasties (TKAs) in the same patients.
Methods
Bilateral, sequential, simultaneous TKAs were performed in 80 patients (160 knees). There were 63 women and 17 men with a mean age of 54.3 years (range 49–55), who received a cementless prosthesis in one knee and a cemented prosthesis in the other. The mean follow-up was 16.6 years (range 16–17).
Results
At final review, the mean Knee Society (KS) knee scores (95.8 versus 96.9), Western Ontario and McMaster Universities (WOMAC) osteoarthritis (OA) index (25.4 versus 25.9), range of motion (ROM) (125°versus 128°), patient satisfaction (8.1 versus 8.3) and radiological results were similar in both groups. Femoral component survival rate was 100 % in both groups at 17 years; at 17 years, the cemented tibial component survival rate was 100 % and the cementless tibial component 98.7 %. No osteolysis was identified in either group.
Conclusion
Long-term results of both cementless and cemented TKAs were encouraging in patients with OA who were <55 years. However, we found no evidence to prove the superiority of cementless over cemented TKAs.
Keywords: Cementless, Cemented, Total knee arthroplasty, Young patients
Introduction
Cemented total knee arthroplasties (TKAs) show low rates of aseptic loosening in long-term follow-up, with good clinical outcomes [1–5]. However, observed signs of osteolysis at the cement–bone interface have raised questions about the long-term durability of cemented TKAs in younger patients [6, 7]. Cementless TKAs have been developed in an attempt to improve the longevity of implants, particularly in younger patients [8]. It is thought that a more physiological bond between bone and implant would result in improved survival from aseptic loosening. Nevertheless, the signs of osteolysis also have been observed with cementless TKAs [9, 10]. Furthermore, early migration seen in cementless TKAs by radiostereometric analysis (RSA) studies has raised concerns about whether the longevity of cemented TKAs could be matched [11].
Although it is now clear that aseptic loosening is mainly related to debris from polyethylene wear rather than failure of cemented fixation [12–15], the question remains whether cementless TKAs have an improved long-term survival. This can only be answered by a randomised trial comparing the two methods of fixation. To date, there are few randomised, prospective trials in which cemented and cementless fixation in primary TKAs are compared in heterogeneous patient groups [12–16]; also, very few studies compare results of cemented and cementless TKAs in the same patient [17]. We previously published our results at 13.6 years using same total knee prosthesis (NexGen posterior-cruciate-retaining implant; Zimmer, Warsaw, IN, USA) in a cohort of 50 patients; the study reported here is a follow-up of 80 patients at a minimum of 16 (mean 16.6) years to determine longer-term clinical results.
The primary purpose of this prospective, randomised study was to evaluate long-term clinical results using validated scoring instruments, radiographic findings, complications and revision and survivorship rates in patients <55 years at minimum of 16 years after undergoing bilateral, simultaneous, sequential cemented and cementless TKA.
Patients and methods
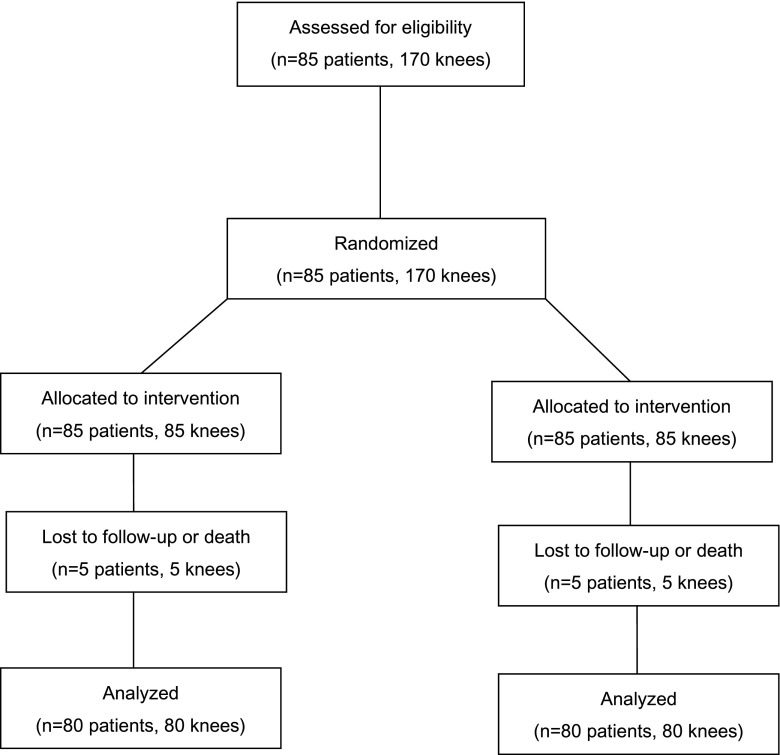
From January 1995 to March 1996, the senior author performed 170 bilateral, sequential, simultaneous TKAs in 85 patients ≤55 years under the same type of anaesthetic. In the interim, two patients died and three were lost to follow-up; thus, 80 patients (160 hips) were available for clinical and radiographic evaluation at a mean of 16.6 (range 16–17) years (Fig. 1). The study was approved by the institutional review board, and all patients provided informed consent.
Fig. 1.
Consolidated Standards of Reporting Trials (CONSORT) flow diagram of patients in the study
Mean patient age at the time of index arthroplasties was 54.3 (range 49–55) years: there were 63 women and 17 men. Mean patient weight was 68.1 (range 51–98) kg, mean height was 156.5 (range 148–180) cm and mean body mass index (BMI) was 27.8 (range 23.3–30.6) kg/m2). All patients had genu varum deformity between 5° and 20° as a result of osteoarthritis (OA) with Albäck grade III, IV or V [18] in both knees. No patient in either group had undergone previous knee surgery. Randomisation to a cemented or cementless NexGen posterior-cruciate-retaining (NexGen CR) prosthesis was accomplished with the use of a sealed, study-number envelope, which was opened in the operating theatre before a skin incision was made. Pre-operatively, there was no significant difference between cohorts in terms of disease extent, pain, deformity, range of motion (ROM) or bone loss (Table 1).
Table 1.
Pre-operative data
| Parameters | Cementless (n = 80) | Cemented (n = 80) | P value* |
|---|---|---|---|
| Mean total knee score (range) | |||
| Knee Society Score | 35.1 (17–51) | 33.9 (9–55) | 0.683 |
| Pain severity (%) | |||
| None | – | – | |
| Mild | – | – | |
| Moderate | 23 (29) | 25 (31) | |
| Severe | 57 (71) | 55 (69) | |
| Walking distance (%) | |||
| Cannot walk | 1 (1) | 1 (1) | |
| < 1 block | 68 (85) | 68 (85) | |
| 1–5 blocks | 11 (14) | 11 (14) | |
| Walking support (%) | |||
| No support | 12 (15) | 12 (15) | |
| 1 cane | 60 (75) | 60 (75) | |
| 2 crutches | 8 (10) | 8 (10) | |
| Stairs | |||
| Normal | 0 (0) | 0 (0) | |
| With support | 80 (100) | 80 (100) | |
| Mean range of motion (°) (range) | 121.9 (79–150) | 125,5 (85–150) | 0.615 |
| Mean WOMAC score (range) | 68.1 (31–98) | 67.8 (29–94) | 0.152 |
| UCLA activity score | 2 (1–3) | 2 (1–3) | – |
WOMAC Western Ontario and McMaster Universities Osteoarthritis index, UCLA University of California, Los Angeles
*Paired t test, unless otherwise stated
All procedures were performed by the senior author (YHK). A tourniquet was used, and an anterior midline incision between 10 cm and 12 cm long was made with a medial parapatellar capsular incision. Femoral preparation was performed first, and the patella was resurfaced using a cemented polyethylene patellar component. In knees with cementless fixation, femoral and tibial components were inserted with a press fit. Component stability was confirmed manually with the leg in full flexion and extension when varus and valgus stress was applied. In cemented fixation, implants were cemented after pulsed lavage and drying and pressurisation of cement. The dedicated cemented femoral component was not available due to inventory problems. The cementless femoral component was used and fixed using cement in the cemented group.
On the second postoperative day, patients were started on continuous passive ROM exercises and began active mobilisation under the supervision of a physiotherapist.
Routine postoperative assessment was undertaken at three months, one year and annually thereafter. Pre- and postoperative Knee Society (KS) [19] knee scores were recorded at each visit, and pre- and postoperative Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores [20] were also determined at each visit. The active ROM of the knee with the patient in the supine position was determined pre-operatively and on the follow-ups by two authors (YHK, JWP) using a standard (60-cm) goniometer; patients were asked to bend their knees as much as possible. Satisfaction was assessed with a visual analogue scale (VAS) ranging from 0 to 10, where 0 was the most dissatisfied and 10 the most satisfied.
At each follow-up visit, we obtained anteroposterior (AP) hip-to-ankle radiographs with the patient standing, anteroposterior radiographs of the knee with the patient supine, lateral radiographs with the patient supine and skyline patellar radiographs. Radiographs were evaluated by one observer (SML) who was not a member of the operating team to determine the femorotibial angle (between the anatomical axis of femur and that of tibia) [19], component alignment (femoral angle and tibial angle) [19], joint line (determined on AP radiographs obtained before and after surgery by measuring the distance between the tip of the fibular head and the distal margin of the lateral femoral condyle pre-operatively and between the tip of the fibular head and the distal margin of the lateral femoral component postoperatively) [19], posterior condylar offset (evaluated on pre- and postoperative lateral radiographs by measuring the maximum thickness of the posterior condyle projected positively to the tangent of the posterior cortex of the femoral shaft) [19], radiolucent lines (RLLs) (depth in millimetres in each zone) [19] and patellar component angle (angle between a line joining the medial and lateral edges of the patella and the horizontal line) [19]. The chance-corrected kappa coefficient [21], calculated to determine intraobserver agreement for measurements for all radiological parameters, ranged from 0.71 to 0.87.
Statistical analysis
To detect an effect size of 0.5—corresponding to an anticipated difference of three points in the KS knee score and a standard deviation (SD) of six points, with a power of 85 % and a level of significance of 5 %—we calculated that 70 patients were required. In anticipation of a small dropout rate, we aimed for 80 patients. We calculated descriptive statistics (mean, SD and proportions) for continuous study variables. KS knee and WOMAC scores were analysed with a paired t test. Pre-operative KS pain score was compared between groups using Fisher’s exact test. Postoperative KS pain score was compared between groups using the Mantel-Haenszel chi-squared test. Knee ROM and radiological data were compared with a paired t test. Complication rates were compared with a chi-squared test; Kaplan–Meier curves were used to analyse the rate of prosthesis survival, with revision for any reason as the end point [22]; the 95 % confidence interval (CI) at certain times was calculated with the formula of Greenwood [23].
Results
Pre- and postoperative KS knee scores, walking distance, ability to negotiate stairs, ROM, WOMAC scores and UCLA activity scores were not significantly different between groups (Tables 1 and 2). At final follow-up, mean KS knee scores (95.8 vs 96.9), ROM (125° vs 128°), WOMAC scores (25.4 vs 25.9) and UCLA activity scores (7 vs 7) improved significantly (P < 0.005) in both groups (Table 2). At final follow-up, patient satisfaction was similar, with a mean of 8.1 (SD 1.9) for the cementless group and 8.3 (SD 1.7) for the cementled group (P = 0.698; paired t test). Sixty-eight patients (85 %) expressed no preference, eight patients preferred the cemented prosthesis and four preferred the cementless prosthesis.
Table 2.
Clinical results at latest follow-up (16.6 years)
| Parameters | Cementless (n = 80) | Cemented (n = 80) | P value* |
|---|---|---|---|
| Mean total knee score (range) | 95.8 (85–100) | 96.7 (79–100) | 0.319 |
| Pain severity (%) | |||
| None | 71 (89) | 70 (88) | |
| Mild | 8 (10) | 8 (10) | |
| Moderate | 1 (1) | 1 (1) | |
| Severe | 0 (0) | 1 (1) | |
| Walking distance (%) | |||
| Cannot walk | – | – | |
| < 1 block | – | – | |
| 1–5 blocks | 11 (14) | 14 (18) | |
| 5–10 blocks | 17 (21) | 17 (21) | |
| Unlimited | 49 (61) | 49 (61) | |
| Walking support (%) | |||
| No support | 75 (94) | 75 (94) | |
| 1 cane | 5 (6) | 5 (6) | |
| 1 crutch | – | – | |
| 2 crutches | – | – | |
| Stairs | |||
| Normal | 34 (42) | 34 (42) | |
| With support | 46 (58) | 46 (58) | |
| Mean range of motion (°) (range) | 125 (98–140) | 128 (100–140) | 0.429 |
| Mean WOMAC score (range) | 25.4 (5–51) | 25.9 (5–59) | 0.189 |
| UCLA activity score | 7 (5–9) | 7 (5–9) | – |
WOMAC Western Ontario and McMaster Universities osteoarthritis index, UCLA University of California, Los Angeles
*Paired t test, unless otherwise stated
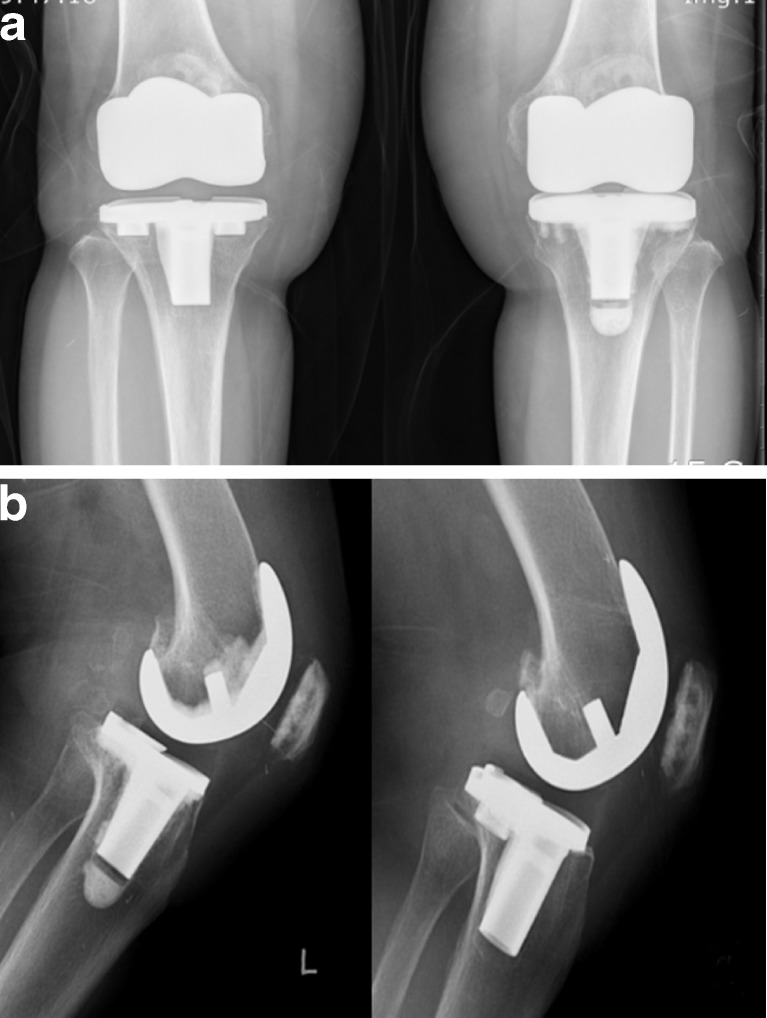
There were no significant differences between groups with regard to radiological parameters (Fig. 2), including limb alignment (femorotibial angle), femoral and tibial component positions, level of the joint line, posterior condylar offset, RLLs and patellar tilt angle (Table 3). No knee had a complete RLL measuring > 1 mm in width around any component in the cemented implant. One knee with cementless TKA had a complete RLL measuring > 2 mm around the tibial component.
Fig. 2.
Radiographs of a 53-year-old woman with bilateral osteoarthritis of the knee in a the supine anteroposterior view and b lateral views 17 years postoperatively. The cementless (right knee) and cemented (left knee) NexGen posterior-cruciate-retaining prostheses firmly embedded in a satisfactory position, with no radiolucent lines and no osteolysis around the component in either knee
Table 3.
Radiographic results
| Parameters | Cementless (n = 80) | Cemented (n = 80) | P value* |
|---|---|---|---|
| Mean knee alignment (°) (range) | |||
| Pre-operative | 10.5 (5–20) | 11.2 (7–20) | 0.615 |
| Postoperative | 5.6 valgus (3–6) | 5.4 valgus (3–7) | 0.152 |
| Mean femoral component position (femoral angle) (°) (range) | |||
| Coronal | 95 (93–103) | 97 (94–101) | 0.265 |
| Sagittal | 3.1 (−0.7 to 9) | 3.6 (1–8) | 0.903 |
| Tibial component position (°) (range) | |||
| Coronal | 91 (85–93) | 89 (86–92) | 0.331 |
| Sagittal | 85 (78–90) | 84 (79–95) | 0.617 |
| Joint line (mm) (range) | |||
| Pre-operative | 15.5 (10–25) | 15.7 (8–24) | 0.776 |
| Postoperative | 14.9 (8–20) | 14.5 (8–20) | 0.739 |
| Posterior condylar offset (mm) (range) | |||
| Pre-operative | 26.1 (21–31) | 25.9 (19–32) | 0.771 |
| Postoperative | 25.9 (18–30) | 25.7 (21–31) | 0.152 |
| Radiolucent line (tibial side) (%) | |||
| Zone 1 ( < 1 mm) | 8 (10) | 10 (13) | – |
| Radiolucent line (<1 mm) (femoral side) (%) | |||
| Anterior flange | 12 (15) | 15 (19) | – |
| Posterior flange | 15 (19) | 13 (16) | |
| Patellar component angle (°) (SD) | |||
| Pre-operative | 11.2 (4.8) | 11.9 (4.5) | 0.665 |
| Postoperative | 3.6 (5.1) | 3.5 (3.3) | 0.897 |
SD standard deviation
*Paired t test
Complication rates were low and similar in both groups. Mean postoperative blood loss (including intra-operative blood loss and blood collected in a suction drain) was 1,686.9 ml (SD 516.8; range 285–2,710) in the cementless group and 1,021.9 ml (SD 328.1; range 215–2,680) in the cemented group. This difference was significant (paired t test, P = 0.005). One knee in each group had a deep infection; both were treated with open débridement followed by intravenous administration of antibiotics for six weeks. There was no subsequent recurrence of infection in either knee. One knee (1.3 %) in the cementless group had aseptic loosening of the tibial component; it was revised to a cemented component 1 year postoperatively. Kaplan–Meier survivorship analysis revealed a femoral component survival rate of 100 % (95 % CI 0.93–1.0) in both groups at 17 years, with loosening or revision considered the end point for failure. Tibial component survival rate was 100 % (95 % CI 0.93–1.0) in the cemented group and 98.7 % (95 % CI 0.92–1.0) in the cementless group at 17 years, with loosening or revision considered the end point for failure.
Discussion
There are very few studies compared midterm results of cemented and cementless TKAs in the same patient [17] and no comparative long-term study of cemented and cementless TKAs in the same patient. Therefore, we evaluate the long-term clinical results, radiographic findings, complications and revision and survivorship rates in patients <55 years at minimum of 15 years after undergoing bilateral, simultaneous, sequential, cementless and cemented TKAs in the same patients. We found gratifying clinical results in both groups, but our data show no evidence of the benefit of cementless over cemented TKAs.
Although TKA is well accepted for patients >65 years, its use is controversial for younger patients (≤ 65 years). Duffy et al. [12] reported a 95 % survival rate at 15 years in patients <55 years, and in a similar age group, Diduch et al. [24] reported a 87 % survival rate at 18 years using revision as an end point. Dixon et al. [25] reported a 92.6 % survival rate at 15 years in patients with an average age of 67 years, using revision as an end point. Dalury et al. [26] found a slight age-related difference. They reported that the ten-year survival rate was 97.5 % for patients <55 years and 98.1 % for older patients; they concluded that survival rate was slightly lower in the younger group. Kim et al. [27] reported that the survivorship of fixed-bearing TKA was 97.1 % at 12.6 years in patients with an average age of 58.6 years and that of mobile-bearing TKA was 97.1 % at 14.1 years in patients with an average age of 55.7 years. Our survival rates are similar to the reported survival rates for TKA in younger patients [12, 24–27]. Baker et al. [14] reported the survival rates of 80.7 % for the cemented press-fit condylar knee (PFC; DePuy, Warsaw, IN, USA) and 75.3 % for the cementless PFC knee (DePuy) at 15 years. The ten-year survival rates for other cemented prostheses range from 92 % to 100 % [13, 17, 28–31] and for other cementless prostheses range from 93.4 % to 98 % [17, 32–39]. Rand [38] reported similar results when comparing the short-term outcome of cemented and cementless PFC knees. However, a longer-term study on these patients [16] showed a significant deterioration in the survival of cementless prostheses, with a ten-year rate of 94.2 % and 72.7 % in the cemented and cementless groups, respectively. These groups, however, contained small numbers of patients who were not well matched with regard to age; the cementless group was significantly younger, by about ten years. Rorabeck et al. [39] reported better results with cemented fixation, but unlike the study we present here, their implants were of two different designs, which might account for the difference in survival. Collins et al. [40] compared the method of fixation using implants of similar design and reported no difference in the short-term outcome. Albrektsson el al. [11] showed significantly less migration of cemented components at one year; a greater number of cementless components required revision at three years in their series. In addition, Chockalingam and Scott [41] reported on the same design in a nonrandomised study and found cemented fixation to be superior for the femoral component. Onsten et al. [42] showed cemented fixation to be superior to porous-coated cementless components at one to two years but equivalent to cementless hydroxyapatite-augmented porous-coated components. Berger et al. [43] reported that at an average of 11 years follow-up, cementless fixation yielded poor results. Accordingly, they abandoned cementless fixation in TKA. Gandhi et al. [44] suggested in their meta-analysis of cemented and cementless TKAs that cemented fixation offers equivalent clinical outcomes and at least as good, if not better, survival than cementless fixation at medium-term follow-up of two to 11 years.
In our series, both cemented and cementless TKAs had improved long-term survival, and there was no significant difference between groups either for survival or clinical outcome at a mean of 16.6 years. Despite patients’ active lifestyles, aseptic loosening that necessitated revision was not a notable problem in either group. We believe that the good results are attributable to the small stature and light weight of our patients, prosthesis design, improved polyethylene quality compared with earlier series and surgical technique used.
Berger et al. [43] reported a 10 % (13 of 131 knees) incidence of osteolytic lesions around cementless tibial components. On the other hand, Kim et al. [27] reported that the incidence of osteolysis (1.6 %, 14 of 894 knees in fixed-bearing knees compared with 2.2 %, 18 of 816 knees in mobile-bearing knees) was very low after contemporary fixed- and mobile-bearing cemented TKAs. Park and Kim [17] reported no osteolysis in either cemented or cementless TKAs 14 years after surgery. In our series reported here, no knee in either group had osteolysis, which we attribute the polyethylene quality.
The strength of this study is the lack of confounding variables, as we examined a single surgeon’s experience with a consecutive group of patients in whom bilateral, sequential, simultaneous TKA was performed. The limitations are that first, differentiation of knee scores in one individual posed some difficulties. The components of pain and ROM were easily differentiated, but those of distance walked and ability to climb stairs were more difficult to separate. In these domains, if patients had difficulties, they could always identify the knee that most limited their activities. Second was the small sample size and lack of interobserver comparisons, which could produce bias in interpreting radiological results. Finally, low patient weight, good pre-operative ROM and young age of this group of patients might limit general applicability to other patient groups. On the other hand, although patients in this study had low weight, daily activities such as farming, squatting and lifting were vigorous.
Long-term results of both cementless and cemented TKAs were encouraging in patients with OA who were <55 years. However, we found no evidence to prove the superiority of the cementless over cemented TKA.
References
- 1.Lombardi AV, Jr, Berasi CC, Berend KR. Evolution of tibial fixation in total knee arthroplasty. J Arthroplast. 2007;22(4 Suppl 1):25–29. doi: 10.1016/j.arth.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Bauer TW, Schils J. The pathology of total joint arthroplasty. I: mechanisms of implant fixation. Skeletal Radiol. 1999;28(8):423–432. doi: 10.1007/s002560050541. [DOI] [PubMed] [Google Scholar]
- 3.Scuderi GR, Insall JN. Total knee arthroplasty: current clinical perspective. Clin Orthop Relat Res. 1992;276:26–32. [PubMed] [Google Scholar]
- 4.Kim Y-H, Kim J-S, Choe J-W, Kim H-J. Long-term comparison of fixed-bearing and mobile-bearing total knee replacements in patients younger than fifty-one years of age with osteoarthritis. J Bone Joint Surg Am. 2012;94(10):866–873. doi: 10.2106/JBJS.K.00884. [DOI] [PubMed] [Google Scholar]
- 5.Kim Y-H, Kim J-S, Park J-W, Joo J-H. Comparison of the Low Contact Stress and Press Fit Condylar Rotating-Platform mobile-bearing prostheses in total knee arthroplasty: a prospective randomized study. J Bone Joint Surg Am. 2011;93(11):1001–1007. doi: 10.2106/JBJS.J.00445. [DOI] [PubMed] [Google Scholar]
- 6.Naudie DD, Ammeen DJ, Engh GA, Rorabeck CH. Wear and osteolysis around total knee arthroplasty. J Am Acad Orthop Surg. 2007;15(1):53–64. doi: 10.5435/00124635-200701000-00006. [DOI] [PubMed] [Google Scholar]
- 7.ƠRourke MR, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Osteolysis associated with a cemented modular posterior –cruciate-substituting total knee design: five to eight- year follow-up. J Bone Joint Surg Am. 2002;84(8):1362–1371. doi: 10.2106/00004623-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Bassett RW. Results of 1,000 performance Knees: cementless versus cemented fixation. J Arthroplasty. 1998;13(4):409–413. doi: 10.1016/S0883-5403(98)90006-7. [DOI] [PubMed] [Google Scholar]
- 9.Nolan JF, Bucknill TM. Aggressive granulomatosis from polyethylene failure in an uncemented knee replacement. J Bone Joint Surg Br. 1992;74(1):23–24. doi: 10.1302/0301-620X.74B1.1732258. [DOI] [PubMed] [Google Scholar]
- 10.Berry DJ, Wold LE, Rand JA. Extensive osteolysis around an aseptic, stable, uncemented total knee replacement. Clin Orthop Relat Res. 1993;293:204–207. [PubMed] [Google Scholar]
- 11.Albrektsson BE, Carlsson LV, Freeman MA, Herberts P, Ryd L. Proximally cemented versus uncemented Freeman-Samuelson knee arthroplasty: a prospective randomized study. J Bone Joint Surg Br. 1992;74(2):233–238. doi: 10.1302/0301-620X.74B2.1544959. [DOI] [PubMed] [Google Scholar]
- 12.Duffy GP, Crowder AR, Trousdale RR, Berry DJ. Cemented total knee arthroplasty using a modern prosthesis in young patients with osteoarthritis. J Arthroplasty. 2007;22(6 Suppl 2):67–70. doi: 10.1016/j.arth.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Khaw FM, Kirk LM, Morris RW, Gregg PJ. A randomised, controlled trial of cemented versus cementless press-fit condular total knee replacement: ten-year survival analysis. J Bone Joint Surg Br. 2002;84(5):658–666. doi: 10.1302/0301-620X.84B5.12692. [DOI] [PubMed] [Google Scholar]
- 14.Baker PN, Khaw FM, Kirk LM, Esler CN, Gregg PJ. A randomised controlled trial of cemented versus cementless press-fit condular total knee replacement: 15- year survival analysis. J Bone Joint Surg Br. 2007;89(12):1608–1614. doi: 10.1302/0301-620X.89B12.19363. [DOI] [PubMed] [Google Scholar]
- 15.McCaskie AW, Deehan DJ, Green TP, Lock KR, Rhompson JR, Harper WM, Gregg PJ. Randomised, prospective study comparing cemented and cementless total knee replacement: results of press-fit condylar total knee replacement at five years. J Bone Joint Surg Br. 1998;80(6):971–975. doi: 10.1302/0301-620X.80B6.8558. [DOI] [PubMed] [Google Scholar]
- 16.Duffy GP, Berry DJ, Rand JA. Cement versus cementless fixation in total knee arthroplasty. Clin Orthop Relat Res. 1998;356:66–72. doi: 10.1097/00003086-199811000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Park J-W, Kim Y-H. Simultaneous cemented and cementless total knee replacement in the same patients: a prospective comparison of long-term outcome using an identical design of NexGen prosthesis. J Bone Joint Surg Br. 2011;93(11):1479–1486. doi: 10.1302/0301-620X.93B11.27507. [DOI] [PubMed] [Google Scholar]
- 18.Ahlbäck S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Diagn (Stockh) 1968;277(Supple):7–72. [PubMed] [Google Scholar]
- 19.Insall JN, Dorr LD, Scott RD, Scott RN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 20.Belllamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patient with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(2):1833–1840. [PubMed] [Google Scholar]
- 21.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 22.Kaplan EL, Meier P (1977) Nonparametric estimation from incomplete observations. JSTOR 53 (282):457–481
- 23.Greenwood M. The natural duration of cancer: Reports on public health and medical subjects. London: Her Majesty’s stationery office; 1926. pp. 1–26. [Google Scholar]
- 24.Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriguez D. Total knee replacement in young, active patients. Long-term follow-up and functional outcome. J Bone Joint Surg Am. 1997;79(4):575–582. doi: 10.2106/00004623-199704000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am. 2005;87(3):598–603. doi: 10.2106/JBJS.C.00591. [DOI] [PubMed] [Google Scholar]
- 26.Dalury DF, Barrett WP, Mason JB, Goldstein WM, Murphy JA, Roche MW. Midterm survival of a contemporary modular total knee replacement: a multicenter study of 1970 knees. J Bone Joint Surg Br. 2008;90(12):1594–1596. doi: 10.1302/0301-620X.90B12.21064. [DOI] [PubMed] [Google Scholar]
- 27.Kim Y-H, Choi Y, Kim JS. Osteolysis in well functioning fixed-and mobile-bearing TKAs in Younger patients. Clin Orthop Relat Res. 2010;468(11):3084–3093. doi: 10.1007/s11999-010-1336-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Emmerson KP, Moran CG, Pinder IM. Survivorship analysis of the kinematic stabilizer total knee replacement: a 10-to 14-year follow-up. J Bone Joint Surg Br. 1996;78(3):441–445. [PubMed] [Google Scholar]
- 29.Ritter MA, Worland R, Saliski J, Helphenstine JV, Edmondson KL, Keating EM, Faris PM, Meding JB. Flat-on-flat, nonconstrained, compression molded polyethylene total knee replacement. Clin Orthop Relat Res. 1995;321:79–85. [PubMed] [Google Scholar]
- 30.Nafei A, Kristensen O, Knudsen HM, Hvid I, Jensen J. Survivorship analysis of cemented total condylar knee arthroplasty : a long-term follow-up report on 348 cases. J Arthroplasty. 1996;11:7–10. doi: 10.1016/S0883-5403(96)80155-0. [DOI] [PubMed] [Google Scholar]
- 31.Ranawat CS, Flynn WF, Jr, Saddler S, Hansrai KK, Maynard MJ. Long-term results of the total condylar knee arthroplasty: a 15-years survivorship study. Clin Orthop Relat Res. 1996;286:94–102. [PubMed] [Google Scholar]
- 32.Hofmaan AA, Evanich JD, Ferguson RP, Camargo MP. Ten-to 14- year clinical followup of the cementless Natural Knee System. Clin Orthop Relat Res. 2001;388:85–94. doi: 10.1097/00003086-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 33.Ritter MA, Meneghini RM. Twenty-year survivorship of cementless anatomic graduated component total knee arthroplasty. J Arthroplasty. 2010;25(4):507–513. doi: 10.1016/j.arth.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 34.Schrøder HM, Berthelsen A, Hassani G, Hansen EB, Solgaard S. Cementless porous-coated total knee arthroplasty: 10-year results in a consecutive series. J Arthroplasty. 2001;16(5):559–567. doi: 10.1054/arth.2001.23565. [DOI] [PubMed] [Google Scholar]
- 35.Whiteside LA. Cementless total knee replacement: nine-to 11-year results and 10-year survivorship analysis. Clin Orthop Relat Res. 1994;309:185–192. [PubMed] [Google Scholar]
- 36.Oliver MC, Keast-Butler OD, Hinves BL, Shepperd JA. A hydroxyapatite-coated Insall-Burstein II total knee replacement: 11-year results. J Bone Joint Surg Br. 2005;87(4):478–482. doi: 10.1302/0301-620X.87B4.15894. [DOI] [PubMed] [Google Scholar]
- 37.Epinette JA, Manley MT. Hydroxyapatite-coated total knee replacement: clinical experience at 10 to 15 years. J Bone Joint Surg Br. 2007;89(1):34–38. doi: 10.1302/0301-620X.89B1.17864. [DOI] [PubMed] [Google Scholar]
- 38.Rand JA. Cement or cementless fixation in total knee arthroplasty? Clin Orthop Relat Res. 1991;273:52–62. [PubMed] [Google Scholar]
- 39.Rorabeck CH, Bourne RB, Nott L. The cemented kinematic- II and the non-cemented porous-coated anatomic prostheses for total knee replacement. A prospective evaluation. J Bone Joint Surg Am. 1988;70(4):483–490. [PubMed] [Google Scholar]
- 40.Collins DN, Heim SA, Nelson CL, Smith P., 3rd Porous-coated anatomic total knee arthroplasty: a prospective analysis comparing cemented and cementless fixation. Clin Orthop Relat Res. 1991;267:128–136. [PubMed] [Google Scholar]
- 41.Chockalingam S, Scott G (2000) The outcome of cemented vs cementless fixation of a femoral component in total knee replacement (TKR) with the identification of radiological signs for the prediction of failure. Knee 7(4):233–238 [DOI] [PubMed]
- 42.Onsten I, Nordqvist A, Carlsson AS, Besjakov J, Shott S. Hydroxyapatite augmentation of the porous coating improves fixation of tibial components: a randomized RSA study in 116 patients. J Bone Joint Surg Br. 1998;80(3):417–425. doi: 10.1302/0301-620X.80B3.7937. [DOI] [PubMed] [Google Scholar]
- 43.Berger RA, Lyon JH, Jacobs JJ, Barden RM, Berkson EM, Sheinkop MB, Rosenberg AG, Galante JO. Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat Res. 2001;392:196–207. doi: 10.1097/00003086-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 44.Gandhi R, Tsvetkov D, Davey JR, Mahomed NN. Survival and clinical function of cemented and uncemented prostheses in total knee replacement: a meta-analysis. J Bone Joint Surg Br. 2009;91(7):889–895. doi: 10.1302/0301-620X.91B7.21702. [DOI] [PubMed] [Google Scholar]