Abstract
Purpose
Posterior stabilised (PS) total knee arthroplasty (TKA) design development that focused on restoring normal knee kinematics was followed by the introduction of reason-guided motion designs. Although all PS fixed-bearing knee designs were thought to have similar kinematics, reports show they have differing incidences and magnitudes of posterior femoral rollback and axial rotation. In this retrospective comparative study between two guided-motion total knee systems, we hypothesised that kinematic pattern has an influence on clinical and functional outcomes.
Methods
This study represents the continuation of a previously reported clinical and kinematics analysis. We retrospectively reviewed 347 patients treated with two different TKA designs: Scorpio NRG (Stryker Orthopedics) and Journey Bi-Cruciate Stabilised (BCS) knee system (Smith & Nephew). Two hundred and eighty-one patients were assessed clinically. Patients were divided into groups according to implanted TKA. Clinical evaluation with the Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaire was performed. Fifteen Scorpio NRG and 16 Journey BCS patients underwent video fluoroscopy during stair climbing, chair rising/sitting and step up/down at six months of follow-up.
Results
At an average 29 months of clinical follow-up, patients with Journey BCS TKAs reported better clinical results. Stiffness was more frequently reported in the Journey group (5.2 % vs 1.2 %), whereas anterior knee pain was observed in the Scorpio NRG group (1.9 %) only. Both prosthetic models reported different posterior translation of the medial and lateral contact points (CP) in all analysed motor tasks during knee flexion (BCS 10–18 mm; NRG Scorpio 2–3 mm). Both designs produced progressive external rotation of the femoral component relative to the tibia during flexion.
Conclusions
Journey BCS showed statistically significant better KOOS results. The higher posterior femoral rollback observed in the kinematic assessment of this design, associated with a better patellofemoral design, may be the reason for better clinical outcome. The reported cases of stiffness and anterolateral joint pain could be attributed to excessive medial and lateral tibiofemoral posterior translation. The NRG group demonstrated good axial rotation, but this was not coupled with physiological kinematic patterns. Patellofemoral pain can be explained by a less friendly femoral-groove design. TKA clinical–functional outcome and complications were highly influenced by the bearing geometry and kinematic pattern of prosthetic designs.
Keywords: TKA design, Kinematics, Fluoroscopy, Clinical result
Introduction
Total knee arthroplasty (TKA) is the gold standard for treating symptomatic, late-stage knee osteoarthritis (OA). Although surgical techniques and implant designs have improved through the years, as evidenced by excellent survivorship and long-term results [1], patients’ satisfaction after TKA is still no more than 70–75 % [2, 3].
Changes in component geometry and modularity with the posterior-stabilised (PS) designs permitted greater surgical flexibility in severe OA cases. In the past, implant designs were based on the assumption that the normal distal femur had a changing centre of rotation during knee flexion [4], thus the multiradius femoral component sagittal profile. Nevertheless, studies describing the distal anatomy of the femur reported that the knee flexion–extension axis can be approximated in TKA by the transepicondylar axis [5, 6]. From this assumption came the postulation of a single radius of femoral condyle curvature. Following these biomechanical principles, TKA with a single-radius femoral component design was introduced in an attempt to more accurately reproduce kinematics of the natural knee joint [7–9]. However, in vivo kinematic pattern studies in patients undergoing TKA demonstrated a considerable variation from the normal knee [10]. Different TKA design solutions for simulating physiological knee kinematics were thus investigated using a guided tibiofemoral motion with asymmetric spine-cam mechanism and an anatomic geometry of tibiofemoral articulation, showing axial rotation patterns similar to those of the normal knee [11, 12]. Although PS fixed-bearing knee implants were thought to all have similar kinematic and kinetic patterns, reports show differing incidences and magnitudes of posterior femoral rollback (PFR) and axial rotation when comparing different designs [13, 14]. In this retrospective comparative study, we aimed to evaluate the clinical outcome and in vivo kinematics in a large, homogeneous cohort of patients undergoing primary navigated TKA in order to determine the influence of the kinematic pattern on clinical results and patient satisfaction.
Materials and methods
Patients
The research presented here represents the continuation of a previously reported study [15]. All patients gave informed consent prior to being included in this retrospective study performed in accordance with the Ethical Standards of the 1964 Declaration of Helsinki as revised in 2000. Between January 2007 and August 2011, 347 computer-assisted (CAS) primary TKAs were performed in 320 consecutive patients by three senior surgeons highly experienced in CAS-TKA. Patient exclusion criteria were prior history of joint replacement on the affected side, evidence of neuromuscular or neurosensory deficiency, rheumatic disease or immunologic suppression; 45 patients did not meet inclusion criteria. All operations were performed using a medial parapatellar approach and with the use of a surgical navigation system (Stryker Knee Navigation System, Stryker Leibinger, Software vs 4.0). The patella was resurfaced in all cases.
Implants
Two different guided-motion TKA designs were evaluated in this study: the Scorpio Non-Restrictive Geometry (NRG) PS knee system (Stryker Orthopedics, Mahwah, NJ, USA) and the Journey Bi-Cruciate Stabilised (BCS) knee system (Smith & Nephew, Memphis, TN, USA). These two prosthetic designs were routinely used in our department, and the surgeons had no preference, as both implants were considered effective and comparable for treating primary knee OA. For this reason, the two implants were both used over the same period in all patients. The main kinematic differences between the implants are represented by the fact that the Scorpio NRG knee system has an axial, unconstrained, fixed-bearing design that allows the femur to rotate freely about the tibia in the transverse plane but limits anteroposterior translation of the femur in knee flexion with constrained spine-cam mechanism; the asymmetric shape of condyles and the polyethylene insert of the Journey BCS more closely reproduce the hallmarks of normal knees, with a femoral component that consistently rolls back after engaging the cam and post at 54° of flexion and offers a medial pivot [16].
Clinical assessment
Pre-operative evaluation included demographic data, primary diagnosis, prior treatment of the affected joint and radiographic knee alignment in both the frontal and sagittal planes. Clinical outcome was analysed at a minimum of one year after TKA by an independent observer and included functional status evaluation using the validated Italian version of the Knee Injury and Osteoarthritis Outcome Score (KOOS) [17]. The KOOS subscale for sports and recreation was not included in the assessment. A normalised score (100 indicating no symptoms, 0 indicating extreme symptoms) was calculated for each examined subscale; possible complications requiring additional surgical procedures were also evaluated.
Fluoroscopic assessment
Fifteen patients from the Scorpio NRG group [18] and 16 from the Journey BCS [12] group were analysed postoperatively at six months of follow-up by video fluoroscopic analysis during stair climbing, chair rising/sitting and step up/down. For stair climbing, three 21-cm-high steps were used; to assess stepping up and down, only the first step was used, and four up/down cycles were performed in a single repetition. For the rising and sitting exercise, chair height was set specifically for each patient in order for him or her to begin with the knee flexed at about 80°. Data collection and analysis procedures were previously discussed [12, 18, 19] and included the use of a standard fluoroscope (digital remote-controlled diagnostic Alpha90SX16, CAT Medical System, Rome, Italy). Three-dimensional prostheses component positions and orientations were obtained from each fluoroscopic image by an iterative procedure using a CAD-model-based shape-matching technique [20]. Previous validation showed that 3D position and orientation of the metal prosthetic component, respectively, have an accuracy >0.5 mm and 1° [20]. Relative motion of the tibial and femoral components was represented using a standard convention [21]. Condylar contact was assumed on the medial and lateral compartments, as the two sets of points at minimum distance between the femoral condyles and the tibial base plate. The positions of these contact points (CP) were expressed in the tibial base-plate reference frame in terms of percentage locations over the anteroposterior (AP) length; 0 % and 100 % corresponded to the most posterior and most anterior location, respectively. Patterns of AP motion of the CP were therefore obtained independently for the medial and lateral condyles. Roll-back and screw-home mechanism were also assessed. The difference between AP locations of the CP at maximum extension and flexion was PFR. Contact-line rotation, defined as rotation of the line connecting the medial and lateral CP with respect to the mediolateral axis on the tibial transverse plane, was calculated for each flexion angle, but here, it is reported over predefined flexion angles with 10° increments, starting from 0°. For each predefined angle, the corresponding contact positions were taken from each trial of each patient, and then averaged [12, 18].
Statistical analysis
Continuous data are expressed as means and standard deviations (SD); categorical data are presented as absolute numbers and percentages. In order to compare baseline and follow-up characteristics between groups, an unpaired t test was used for continuous data and chi-square and Fisher’s exact tests for categorical data. P values were two-sided and considered significant if <0.05.
Results
Clinical and functional results and complications
Of the 320 patients included in this analysis, 34 (15 in the Scorpio NRG group and 19 in the Journey BCS group) were lost to follow-up. Five patients in the NRG and two in the BCS group (1.6 % of all cases) were diagnosed with prosthetic joint infection and were excluded from further assessment; 281 patients (297 knees) were therefore assessed and clinically evaluated. No significant pre-operative differences were reported between groups regarding demographic characteristics (e.g. age, body mass index, gender) and knee alignment.
Mean follow-up was similar for both groups: 29 (12–48) months for the Scorpio NRG group and 28 (12–50) months for the Journey BCS group. At final follow-up, the Journey BCS group had higher mean KOOS scores in all subscales than the NRG group. This difference was statistically significant for the KOOS subscales of pain (p = 0.005) and knee-related quality of life (QOL) (p = 0.040).
When analysing complications, stiffness requiring manipulation under anaesthesia and arthroscopic debridement was more frequently reported in the Journey group (5.2 % vs. 1.2 %), whereas anterior knee pain was observed only in the Scorpio group (1.9 % of cases). Other, less frequently observed, complications were represented by synovitis pain treated with arthroscopic debridement in 0.7 % of the BCS group and frontal plane instability corrected with polyethylene liner exchange in 1.1 % vs 0.3 %, respectively, in the BCS and NRG groups.
Fluoroscopic results
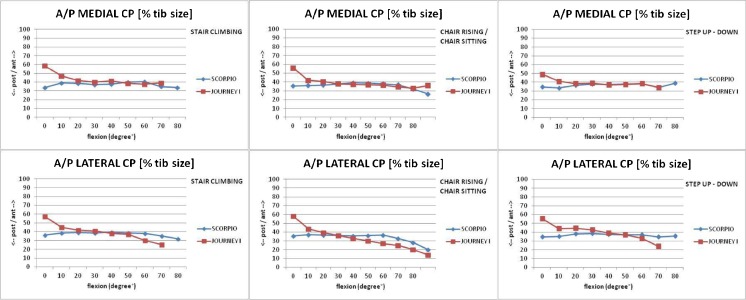
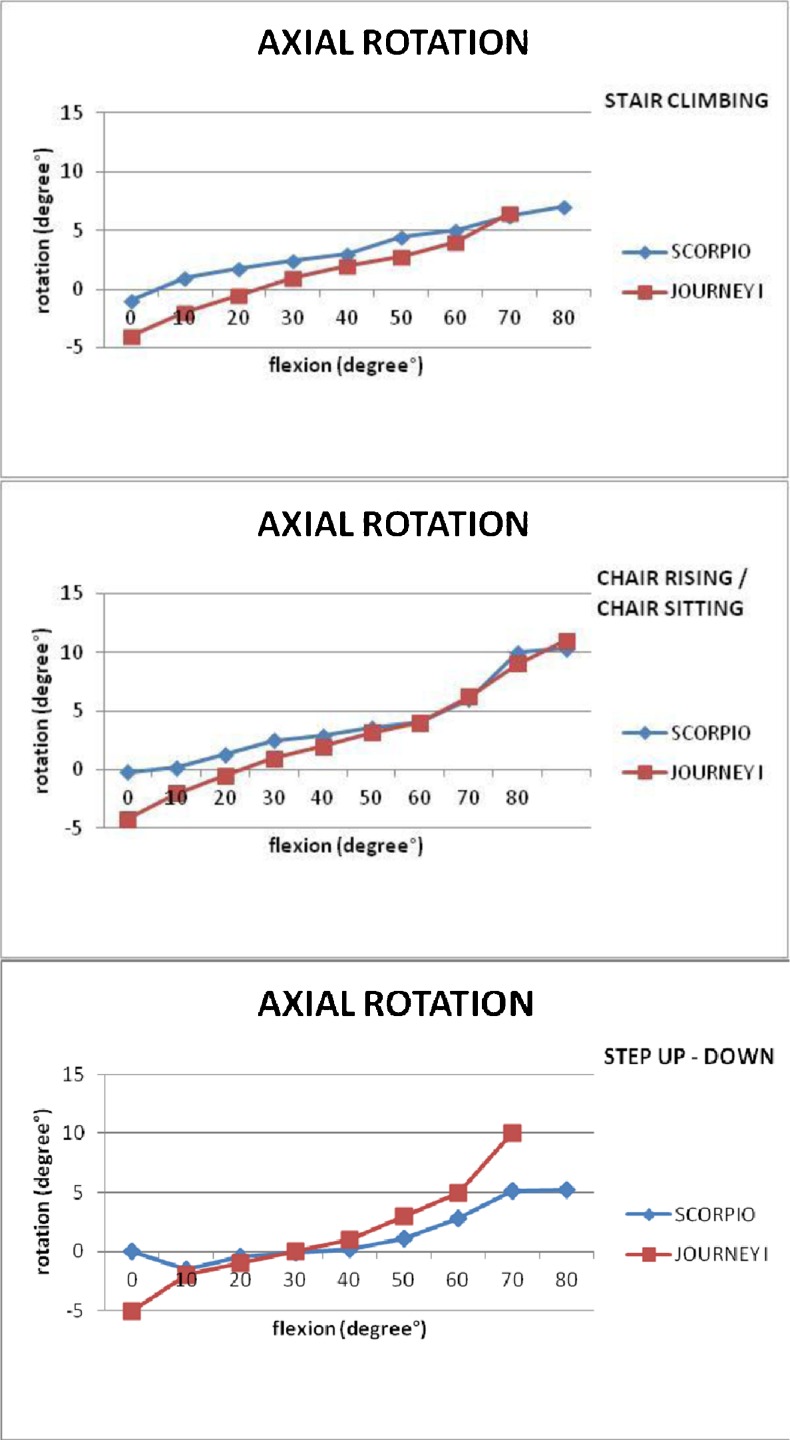
Both prosthetic models reported a posterior translation during knee flexion of the medial and lateral CP in all analysed motor tasks (stair climbing, chair rising/sitting, step up/down): for the medial compartment, 3.1 ± 1.7 mm, 5.5 ± 1.8 mm and 3.6 ± 1.8 mm, respectively, in the Scorpio NRG group, and 9.7 ± 3.0 mm, 10.0 ± 2.6 mm, 6.9 ± 3.5 mm respectively, in the Journey BCS group; for the lateral compartment, 4.8 ± 1.8 mm, 7.5 ± 1.5 mm and 5.2 ± 1.8 mm, respectively, in the NRG group, and 14.3 ± 3.5 mm, 18.5 ± 3.0 mm and 13.9 ± 3.8 mm in the BCS group in the three motor tasks (Tables 1 and 2). In all three motor tasks, medial and lateral CP displacements in the NRG group were generally located posteriorly throughout the flexion arc (between ~30 % and 40 % of the AP tibial plate length); the BCS group showed a coupled posterior translation of the two CPs between 0° and 30° knee flexion (between ~60 % and 40 % of the AP tibial plate length) and higher posterior translation of the lateral than the medial CP for knee flexion >50° (between 40 % and 20 % of AP tibial plate length for the lateral CP and between 40 % and 35 % for the medial CP) (Fig. 1). Both prosthetic designs showed progressive internal rotation of the femoral component relative to the tibial plate during flexion. In the NRG group, the described mechanisms were somewhat limited: the reported range of contact-line rotation was 9.4, 11.4 and 11.3 in stair climbing, chair rising/sitting and step up/down, respectively; medial and lateral CP displacements were generally located posterior throughout the flexion arc, and posterior translation of both occurred at flexion angles > 60°. Consistent with these findings, the pivot point of the contact lines was mostly found in the central area of the base plate. In the BCS group, the mechanisms were more accentuated: the range of contact-line rotation was as great as 21.6, 21.7 and 26.2 in stair climbing, chair rising/sitting, step up/down, respectively. Rollback mainly occurred at small flexion angles, and medial pivoting occurred especially at higher flexion. No evidence of condylar liftoff was observed in any task in any patient (Fig. 2).
Table 1.
Journey Bi-Cruciate Stabilised (BCS) knee system fluoroscopy data [12]
| Stair climbing | Chair rising/sitting | Step up/down | |
|---|---|---|---|
| AP medial CP (mm) | 9.7 (−6.0 to 3.7) ± 3.0 | 10.0 (−7.7 to 2.3) ± 2.6 | 6.9 (−7.4 to ±0.5) ± 3.5 |
| AP lateral CP (mm) | 14.3 (−10.6 to 3.5) ± 3.5 | 18.5 (−15.3 to 3.1) ± 3.0 | 13.9 (−10.8 to 3.1) ± 3.8 |
| AP medial CP (% tibia size) | 23.3 (35.2 to 58.5) ± 6.4 | 23.0 (32.9 to 55.9) ± 6.1 | 16.5 (32.1 to 48.6) ± 7.7 |
| AP lateral CP (% tibia size) | 32.7 (25.1 to 58.8) ± 8.0 | 43.8 (14.0 to 57.8) ± 6.5 | 33.3 (23.6 to 56.9) ± 9.0 |
| AP medial CP (% tibia size) | |||
| At maximum extension | 58.5 ± 4.8 | 55.9 ± 7.9 | 48.7 ± 7.9 |
| At maximum flexion | 38.9 ± 5.9 | 35.8 ± 5.6 | 33.9 ± 6.5 |
| AP lateral CP (% tibia size) | |||
| At maximum extension | 57.3 ± 7.3 | 57.8 ± 6.7 | 55.4 ± 11.0 |
| At maximum flexion | 25.6 ± 6.3 | 14.2 ± 4.7 | 23.8 ± 7.6 |
| Range of contact-line internal rotation | 13.0 (5.6 to 21.6) ± 4.0 | 15.8 (7.3 to 21.7) ± 4.4 | 15.2 (7.9 to 26.2) ± 5.7 |
| Contact-line rotation (+ internal) | |||
| At maximum extension | 4.0 ± 1.0 | 4.2 ± 5.3 | 5.1 ± 8.0 |
| At maximum flexion | −6.5 ± 4.8 | −11.0 ± 6.0 | −10.0 ± 5.6 |
| Medial PFR (mm) | 8.5 ± 2.0 | 8.9 ± 3.5 | 5.6 ± 3.4 |
| Lateral PFR (mm) | 14.3 ± 3.4 | 18.5 ± 2.6 | 13.9 ± 3.2 |
Mean ± standard deviation, range (in parentheses). Translations in percentage and contact-line rotations are values at 0° and maximum flexion
AP anteroposterior, CP contact points, PFR posterior femoral rollback
Table 2.
Scorpio NRG fluoroscopy data [18]
| Stair climbing | Chair rising/sitting | Step up/down | |
|---|---|---|---|
| AP medial CP (mm) | 3.1 (4.2 ,7.3) ± 1.7 | 5.5 (4.9 to 10.4) ± 1.8 | 3.6 (4.7 to 8.3) ± 1.8 |
| AP lateral CP (mm) | 4.8 (4.3 to 9.1) ± 1.8 | 7.5 (5.7 to 13.2) ± 1.5 | 5.2 (5.1 to 10.3) ± 1.8 |
| AP medial CP (% tibia size) | 37.3 (32.0 to 40.5) ± 4.0 | 35.6 (25.5 to 39.0) ± 4.1 | 35.5 (30.8 to 38.8) ± 4.0 |
| AP lateral CP (% tibia size) | 36.5 (27.7 to 40.5) ± 4.1 | 33.1 (18.7 to 36.9) ± 3.4 | 35.4 (26.1 to 37.9) ± 4.1 |
| AP medial CP (% tibia size) | |||
| At maximum extension | 34.0 ± 2.1 | 35.5 ± 6.7 | 34.4 ± 2.2 |
| At maximum flexion | 34.0 ± 1.9 | 26.3 ± 1.2 | 33.8 ± 4.5 |
| AP lateral CP (% tibia size) | |||
| At maximum extension | 36.1 ± 4.6 | 35.7 ± 3.6 | 34.6 ± 3.0 |
| At maximum flexion | 32.0 ± 1.8 | 19.8 ± 1.2 | 33.6 ± 5.5 |
| Range of contact line internal rotation | 9.4 (4.0 to 22.4) ± 4.6 | 11.4 (4.6 to 22.7) ± 4.5 | 11.3 (5.1 to 18.0) ± 4.0 |
| Contact line internal rotation (+ internal) | |||
| At maximum extension | 1.5 ± 3.9 | 1.5 ± 3.2 | 1.3 ± 1.0 |
| At maximum flexion | 1.0 ± 4.2 | 6.5 ± 1.4 | 1.0 ± 3.2 |
| Medial PFR (mm) | 0.5 ± 1.0 | 3.5 ± 1.7 | 2.1 ± 1.5 |
| Lateral PFR (mm) | 1.4 ± 1.8 | 6.7 ± 1.3 | 0.6 ± 1.2 |
Mean ± standard deviation, range (in parentheses). Translations in percentage and contact-line rotations are values at 0° and maximum flexion
AP anteroposterior, CP contact points, PFR posterior femoral rollback
Fig. 1.
Fluoroscopy data: anteroposterior (AP) translation of the medial (up) and lateral (down) contact points (CP) from all patients during the three analysed motor tasks for 10° knee-flexion step
Fig. 2.
Fluoroscopy data: knee axial rotation versus flexion for the three motor tasks. Positive values indicate internal rotation
Discussion
This study indicated that TKA clinical–functional outcome and complications are highly influenced by bearing geometry and kinematic pattern of different guided-motion prosthetic designs. The Journey BCS group obtained significantly better scores in the KOOS subcategories of pain and QOL and showed a statistically significant (p = 0.018),increase in range of motion (ROM) (mean ≥3.5°) with respect to the Scorpio NRG group. We hypothesised that this increased ROM could be due to guided kinematic patterns favouring PFR. In the same way, PFR, associated with better patellofemoral kinematics, could be the reason for better clinical outcome and KOOS scores. Published clinical evidence clearly supports the efficacy of guided motion in restoring physiological knee motion and normal overall function [12]. However, two recent publications emphasised potential complications associated with the Journey BCS: first, some patients presented with an increased incidence of Iliotibial band (ITB) syndrome. Luyckx and colleagues [22] reported outcomes for 1,070 Journey I BCS knees at a mean follow-up of 2.5 years. Overall, clinical outcomes for this cohort were quite good. Device survival of 98 % was reported, with partial or total revision as the primary endpoint. However, symptoms of ITB syndrome were observed in 7.2 % of patients at a mean 6 months of follow-up. After further rehabilitation, pain during flexion persisted in 2 % of these patients, resulting in surgical ITB release. The authors suggest that excessive translation of the femur in flexion can lead to increased eccentric loading of the ITB in some patients, potentially causing pain. In addition to ITB traction, complications associated with dislocation were reported by Arnout et al. [23], who stated that each case demonstrated excellent clinical outcomes at the time of dislocation. However, each of these patients happened to be extremely flexible, achieving deep flexion quickly after surgery. This movement allows the femoral cam to potentially jump over the relatively short tibial post. Considering our cohort’s overall complications, stiffness (6.4 %) and anterior knee pain (1.9 %) were the most common. This finding is confirmed by results of an analysis of 10,188 primary TKAs [24]. In particular, a higher incidence of stiffness was reported in the BCS group (5.2 %) than in the NRG group (1.2 %). Multiple factors can have significant effects on ROM after TKA: PFR, patellofemoral kinematics and posterior condyle offset are the most important ones [25–27]. Prosthetic design may have had a role in knee stiffness in the BCS group, considering other factors affecting clinical outcomes in the same manner in a homogeneous population, such as this series. In particular, we believe that excessive femoral rollback reported for the BCS design could induce excessive mechanical stress on soft tissues. This mechanism may be responsible of fibrous metaplasia [27] and knee-joint synovitis with consequent knee stiffness. Conversely, the NRG group reported a higher rate of anterior knee pain (1.9 %): this was probably related to the use of trochlear flange depth in this design. Impaired patellofemoral tracking of the NRG femoral design could be responsible for the reported symptom.
As reported by several authors [13, 14] and confirmed by our study, PS fixed-bearing TKA designs can differ in kinematic pattern (i.e. posterior femoral rollback, patellofemoral tracking and posterior condyle offset). This report has an influence on clinical outcome and complications. The relevance of this study is the clinical outcome and complication rate in correlation with fluoroscopic assessment: the two designs actually demonstrated different kinematics pattern. Our results suggest that the main features of the BCS design (an asymmetric spine-cam mechanism and an anatomically shaped tibial insert) can result in rollback and screw-home mechanisms in the replaced knee. The NRG group demonstrated consistent axial rotation with a central pivot, explained by the single radius of curvature of the prosthetic model on the frontal plane and a good posterior positioning of the femoral component on the tibial plate. Other kinematic patterns, such as rollback mechanism and femoral external axial rotation, were minimised compared with the BCS group. We believe that these findings are the reason for the poorer clinical outcome reported by this prosthetic design.
We acknowledge that our study has several limitations: results might be impaired by the retrospective analysis and the absence of preoperative KOOS data, which would have provided a more comprehensive evaluation of patient improvement following TKA. The absence of randomisation and the relatively short follow-up could also have weakened our findings. However, the large cohort, the aid of surgical navigation and the nonselective use of both designs in a homogeneous demographic series of patients could reduce the bias of the analysis.
Conclusion
Clinical and functional outcome in primary TKA can be affected by the design and kinematic pattern of different prosthetics, as revealed by coupled analysis of clinical and fluoroscopic outcomes in this large patient cohort.
References
- 1.Jones CA, Beaupre LA, Johnston DW, et al. Total joint arthroplasties: current concepts of patient outcomes after surgery. Rheum Dis Clin N Am. 2007;33:71–86. doi: 10.1016/j.rdc.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Noble PC, Gordon MJ, Weiss JM, et al. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;431:157–165. doi: 10.1097/01.blo.0000150130.03519.fb. [DOI] [PubMed] [Google Scholar]
- 3.Noble PC, Conditt MA, Cook KF, et al. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 4.Gunston FH. Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement. J Bone Joint Surg Br. 1971;53:272–277. [PubMed] [Google Scholar]
- 5.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. 1998;356:111–118. doi: 10.1097/00003086-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J. Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res. 2007;461:238–244. doi: 10.1097/BLO.0b013e318112416b. [DOI] [PubMed] [Google Scholar]
- 7.Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res. 1993;290:259–268. [PubMed] [Google Scholar]
- 8.Kessler O, Durselen L, Banks S, Mannel H, Marin F. Sagittal curvature of total knee replacements predicts in vivo kinematics. Clin Biomech (Bristol, Avon) 2007;22:52–58. doi: 10.1016/j.clinbiomech.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Nogler M, Hozack W, Collopy D, Mayr E, Deirmengian G, Sekyra K (2012) Alignment for total knee replacement: a comparison of kinematic axis versus mechanical axis techniques. A cadaver study. Int Orthop :2249–2253. doi:10.1007/s00264-012-1642-2 [DOI] [PMC free article] [PubMed]
- 10.Matsuzaki T, Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kawakami Y, Ishida K, Oka S, Kuroda R, Kurosaka M (2013) Kinematic factors affecting postoperative knee flexion after cruciate-retaining total knee arthroplasty. Int Orthop :803–808. doi:10.1007/s00264-013-1803-y [DOI] [PMC free article] [PubMed]
- 11.Victor J, Mueller JK, Komistek RD, Sharma A, Nadaud MC, Bellemans J. In vivo kinematics after a cruciate-substituting TKA. Clin Orthop Relat Res. 2010;468(3):807–814. doi: 10.1007/s11999-009-1072-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Catani F, Ensini A, Belvedere C, Feliciangeli A, Benedetti MG, Leardini A, Giannini S. In vivo kinematics and kinetics of a bi-cruciate substituting total knee arthroplasty: a combined fluoroscopic andgait analysis study. J Orthop Res. 2009;27(12):1569–1575. doi: 10.1002/jor.20941. [DOI] [PubMed] [Google Scholar]
- 13.Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB. Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:37–57. doi: 10.1097/01.blo.0000092986.12414.b5. [DOI] [PubMed] [Google Scholar]
- 14.Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A. A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res. 2004;428:180–189. doi: 10.1097/01.blo.0000148777.98244.84. [DOI] [PubMed] [Google Scholar]
- 15.Mugnai R, Digennaro V, Ensini A, Leardini A, Catani F. Can TKA design affect the clinical outcome? Comparison between two guided-motion systems. Knee Surg Sports Traumatol Arthrosc. 2013 doi: 10.1007/s00167-013-2509-9. [DOI] [PubMed] [Google Scholar]
- 16.Catani F, Innocenti B, Belvedere C, Labey L, Ensini A, Leardini A. The Mark Coventry Award: articular contact estimation in TKA using in vivo kinematics and finite element analysis. Clin Orthop Relat Res. 2010;468:19–28. doi: 10.1007/s11999-009-0941-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monticone M, Ferrante S, Salvaderi S, Rocca B, Totti V, Foti C, Roi GS. Development of the Italian version of the knee injury and osteoarthritis outcome score for patients with knee injuries: cross-cultural adaptation, dimensionality, reliability, and validity. Osteoarthr Cartil. 2012;20:330–335. doi: 10.1016/j.joca.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 18.Catani F, Belvedere C, Ensini A, Feliciangeli A, Giannini S, Leardini A. In-vivo knee kinematics in rotationally unconstrained total knee arthroplasty. J Orthop Res. 2011;29(10):1484–1490. doi: 10.1002/jor.21397. [DOI] [PubMed] [Google Scholar]
- 19.Fantozzi S, Catani F, Ensini A, et al. Femoral rollback of cruciate-retaining and posterior-stabilized total knee replacements: in vivo fluoroscopic analysis during activities of daily living. J Orthop Res. 2006;24:2222–2229. doi: 10.1002/jor.20306. [DOI] [PubMed] [Google Scholar]
- 20.Banks SA, Hodge WA. Accurate measurement of threedimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng. 1996;43:638–649. doi: 10.1109/10.495283. [DOI] [PubMed] [Google Scholar]
- 21.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 22.Luyckx L, Luyckx T, Bellemans J, Victor J. Iliotibial band traction syndrome in guided motion TKA: a new clinical entity after TKA. Acta Orthop Belg. 2010;76:507–512. [PubMed] [Google Scholar]
- 23.Arnout N, Vandenneucker H, Bellemans J. Posterior dislocation in total knee replacement: a price for deep flexion? Knee Surg Sports Traumatol Arthrosc. 2006;19(6):911. doi: 10.1007/s00167-010-1258-2. [DOI] [PubMed] [Google Scholar]
- 24.Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53. doi: 10.1302/0301-620X.84B1.12432. [DOI] [PubMed] [Google Scholar]
- 25.Malviya A, Lingard EA, Weir DJ, Deehan DJ. Predicting range of movement after knee replacement: the importance of posterior condylar offset and tibial slope. Knee Surg Sports Traumatol Arthrosc. 2009;17:491–498. doi: 10.1007/s00167-008-0712-x. [DOI] [PubMed] [Google Scholar]
- 26.Massin P, Gournay A. Optimization of the posterior con- dylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty. 2006;21:889–896. doi: 10.1016/j.arth.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 27.Boldt JG, Stiehl JB, Hodler J, Zanetti M, Munzinger U. Femoral component rotation and arthrofibrosis following mobile- bearing total knee arthroplasty. Int Orthop. 2006;30:420–425. doi: 10.1007/s00264-006-0085-z. [DOI] [PMC free article] [PubMed] [Google Scholar]