Abstract
Purpose
There remains controversy as to whether computer-navigated total knee replacement (TKR) improves the overall prosthesis alignment and patient function. The aim of this study was to determine whether computer-assisted total knee arthroplasty provides superior prosthesis positioning when compared to a conventional jig-assisted total knee replacement and whether this affected the functional outcome.
Methods
This prospective, randomised controlled study compared computer navigated and conventional jig-assisted total knee replacement in 37 patients who underwent bilateral TKR. A quantitative assessment of the spatial positioning of the implant in the 74 total knee replacements was determined using a low-dose dual-beam CT scanning technique. This resulted in six parameters of alignment that were compared. Functional outcomes using the high activity arthroplasty score and Knee Society score were assessed pre-operatively, postoperatively, at three years and at five years. Patients also indicated which knee they felt was subjectively the best.
Results
There was no statistically significant difference in the prosthesis alignment between both groups and the number of outliers was not decreased with navigation. All function scores improved from pre-operative to postoperative but there was no statistically significant difference between the groups at five years. At five years, 40.6 % of patients thought their jig-assisted knee was the better knee compared with 21.9 % their computer assisted knee and 37.5 % of patients who felt they were the same.
Conclusion
Computer-assisted implantation of total knee replacements does not offer a significant advantage in prosthesis alignment. There was no difference in functional outcome or subjective “best knee” between the computer-assisted or jig-assisted knee.
Introduction
The treatment of end-stage arthritis by total knee arthroplasty has become a predictable procedure reducing pain and increasing patient’s function. The accurate positioning of total knee prosthetic components has been critical to provide a predictable outcome and in reducing the risks of abnormal wear, instability, loosening and pain [1–6]. Positioning can be affected by a number of factors which are both patient and surgeon related [5, 7]. The ideal position should be aligned with the mechanical axis in both the axial and rotational planes. Patients have been shown to have better functional outcomes when the coronal alignment was within 3° of neutral [3–8].
Computer-assisted surgery has been developed to help the surgeon position the implant in a more accurate position, resulting in better function and improved longevity. Several studies have shown computer-assisted navigation systems increase the precision of implantation in the mechanical axis [9–17]. Other studies have suggested that critical axial alignment may not be essential to produce good clinical results and early results show little clinical difference or implant survival between the two groups [18, 19]. More recently, medium-term results comparing computer-assisted total knee arthroplasty (CATKR) to traditional jig-assisted total knee arthroplasty (JATKR) have shown little difference between the two groups, with outcome scores, survival and patient preference being similar [20, 21]. Computer-assisted surgery has however been shown to take longer than JATKR with an average increase of 13–35 minutes [14, 15, 17, 18, 22] as well as incurring increased costs and requiring further training with a resultant early learning curve.
There are multiple studies looking at alignment and outcomes in patients undergoing CATKR compared with JATKR; however, there are only a few using bilateral knee joint replacements [15, 17, 18]. Many of these studies have measured the mechanical axis by full-length standing radiographs of the lower extremity. This, however, introduces radiographic errors caused by images that deviate from exact frontal or sagittal planes, show extension deficits, and errors of rotation between the tibia and femur [23–25]. Low-dose CT scanning has been shown to produce an accurate three-dimensional model of the lower limb, which allows direct measurement of the alignment of the femoral and tibial components in relation to the mechanical axis or the trans-epicondylar axis [26–28].
The aim of this study was to determine whether CATKR led to improved prosthesis positioning when compared with JATKR in patients undergoing one-stage bilateral replacements using accurate low-dose CT scanning and to determine whether the five-year functional outcome and prosthesis survival were different between the two methods.
Materials and methodology
Patient selection
This study was a prospective, consecutive series of patients enrolled over the course of two years who underwent bilateral TKA at an elective orthopaedic centre between October 2005 and November 2007. All were approached and consented to having one knee replaced using image guidance and the other with traditional JTKR. There were 37 patients (74 TKRs) enrolled and all procedures were performed by a single experienced knee surgeon under the same anaesthetic. The first knee implanted was always the computer-assisted surgery and the side was chosen by the nursing staff depending on how the operating room was setup. There was no input by the surgeon into which side was operated on using image guidance.
All patients underwent identical procedures with the same LCS (De Puy, Leeds) uncemented mobile bearing implant inserted on each side. The CATKR used the Ci Image Guidance (De Puy, Leeds) system and the JATKR used the Complete (De Puy, Leeds) instrument system. Instruments to aid navigation were used internally, therefore creating no external skin markings to affect blinding of patients.
All patients were blinded to which knee used image guidance and were independently assessed preoperatively and postoperatively with a high activity arthroplasty score (developed at our facility in 2005) [29] and the Knee Society score for pain and function. Postoperatively patients also completed a visual analogue scale (form 0–10 with 0 being completely abnormal and 10 a normal knee) comparing each TKR and to also rate which knee they felt was more normal. All were followed for a minimum of five years.
CT was performed in all patients in the early postoperative period and assessed by an experienced, blinded, independent radiologist.
CT evaluation of alignment and rotation
A low-dose CT technique based on the Perth Protocol [27, 28] was used and measured all the parameters which the Ci (DePuy, Leeds) image-guided system aimed to control. In addition we measured the rotation of the femoral and tibial components, and their rotation relative to each other.
A Siemens Definition dual source CT scanner was used for scanning of all patients following a standardized protocol. The patient was positioned supine for the scan, with the legs in neutral position, patellae pointing anteriorly, and knees in maximal extension. No stabilisation of the legs was required due to the speed of scanning. Scanning was performed from superior margin of the acetabulum to the talus.
The centre of the femoral head, the centre of the distal femur, the centre of the tibial plateau, and the centre of the ankle joint were all identified and axial, coronal and sagittal reconstructions of the full leg were produced to give the mechanical axis of the limb in the coronal and sagittal planes. The varus and valgus alignment of the components was calculated by taking a line across the base of each component in the coronal plane and measuring the angle with the mechanical axis.
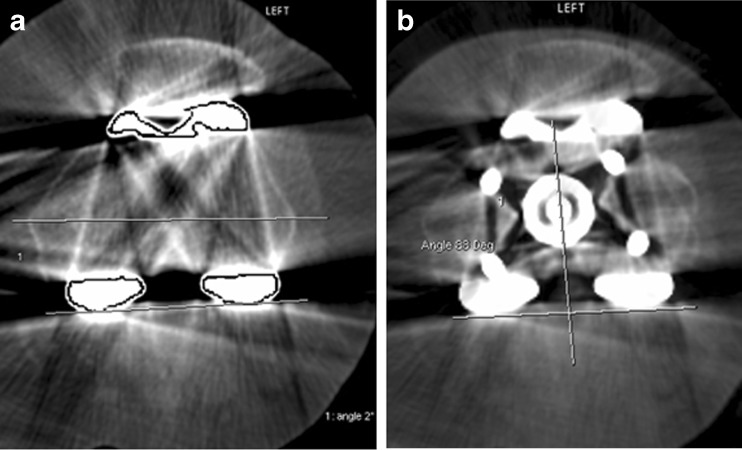
The degree of flexion/extension of the femoral component was calculated by measuring the angle of the posterior flange of femoral component relative to the sagittal femoral anatomical axis. Similarly, the degree of slope of the tibial base plate was measured relative to the tibial sagittal anatomical axis. Femoral component rotation was identified by comparing the angle between the posterior condylar line of the prosthesis relative the epicondylar axis (Fig. 1a). Finally, the degree of femoro-tibial mismatch was identified by superimposing axial images of the femoral component and tibial baseplate. The angle was calculated between posterior condylar line of the femoral prosthesis, and a line through the centre of the stem of the tibial baseplate (Fig. 1b).
Fig. 1.
a Measuring femoral rotation. b Measuring femoro-tibial mismatch
Statistical analysis
For each radiologic measure, means and standard deviations were calculated and distributions were inspected using histograms. As each patient was operated on twice, with a different procedure on each knee, the measures were paired and were analysed using paired t-tests. The procedures were not completely balanced across the left and right legs, with 13 computer-assisted procedures in the left leg and only ten in the right, and the reverse for the conventional jig procedure. Therefore the data was also analysed in an analysis of variance for unbalanced data (PROC GLM in SAS 9.1.2) to check if the same conclusions were reached when the leg involved was taken into account. The significance of the comparisons across the two procedures was similar from both sets of analyses.
Results
There were 37 patients (74 knees) who underwent bilateral TKJR. At the five-year follow-up, three patients were deceased (at six months, two years and five years), two further patients were lost to follow-up as they had emigrated from the country. This left 32 patients (64 knees) with full clinical and radiological details at five years.
The average age was 67.3 years (53–80 years) with a minimum follow up of five years (maximum seven years).
Prosthesis alignment
There was no significant difference in the variability of the radiological outcome across all measures for alignment. The variance of each measure was compared across the two procedures by calculating the correlation between the sum and the difference across the two procedures for each patient [30] (Table 1).
Table 1.
Comparison of outcomes for JATKR and CATKR procedures for 32 patients. All measurements of prosthetic positioning are in degrees
| Measure | CATKR (C) | JATKR (J) | C-J | Significance for C - J |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean difference (95%CI) | df = 22 | |
| External rotationa | −2.6 | −2.9 | 0.3 | 0.67 |
| (3.1) | (3.2) | (−1.2, 1.8) | ||
| Femoral flexionb | 0.1 | −0.5 | 0.6 | 0.22 |
| (2.3) | (2.7) | (−0.4, 1.6) | ||
| Varus/valgus alignment—femoralc | 0.4 | 0.2 | 0.2 | 0.66 |
| (1.8) | (1.7) | (−0.8, 1.2) | ||
| Varus/vagal alignment—tibiald | 0.1 | −0.2 | 0.3 | 0.59 |
| (1.9) | (2.0) | (−0.8, 1.5) | ||
| Tibial prosthetic alignmente | 4.7 | 5.0 | −0.3 | 0.71 |
| (2.7) | (2.9) | (−1.7, 1.2) | ||
| Femorotibial mismatchf | −1.8 | −4.6 | 2.7 | 0.17 |
| (6.2) | (6.3) | (−1.3, 6.8) |
CATKR computer-assisted total knee arthroplasty, JATKR traditional jig-assisted total knee arthroplasty
a External rotation of femoral prosthetic component relative to transepicondylar axis. Positive values imply degrees of external rotation; negative values imply degrees of internal rotation
b Flexion of femoral prosthetic component relative to femoral sagittal anatomical axis. Positive values imply degrees of flexion; negative values imply degrees of extension
c Varus/Valgus alignment of femoral component in relation to mechanical axis of lower limb. Positive values imply degrees of valgus alignment; negative values imply degrees of varus alignment
d Varus/Valgus alignment of tibial component in relation to mechanical axis of lower limb. Positive values imply degrees of valgus alignment; negative values imply degrees of varus alignment
e Flexion of tibial prosthetic component relative to tibial sagittal anatomical axis. Positive values imply degrees of posterior slope; negative values imply degrees of anterior slope
f Femorotibial mismatch—rotation of tibial prosthetic component relative to femoral prosthetic component. Positive values imply degrees of external rotation of tibial prosthesis on femoral prosthesis; negative values imply degrees of internal rotation
Femoral prosthesis alignment
In the coronal plane, the JATKR group showed a range of between 3° varus and 3° valgus alignment, with a mean deviation of 0.2° valgus ±1.7°. The CATKR group showed a range of between 4° varus and 4° valgus alignment, with a mean deviation of 0.4° valgus ±1.8°. Four of the JATKRs achieved neutrality, compared with two CATKRs. If one assumes a tolerance level of 3°, two CATKRs, but no JATKR were outside this limit. The difference between the groups was not statistically significant.
Femoral flexion/extension alignment revealed a variation of between 3° of flexion and 7° of extension for JATKR with a non significant mean deviation of 0.5° of extension ±2.7°. In the CATKR the range was from 4° of flexion to 5° of extension with a mean of 0.1° ±2.3°.
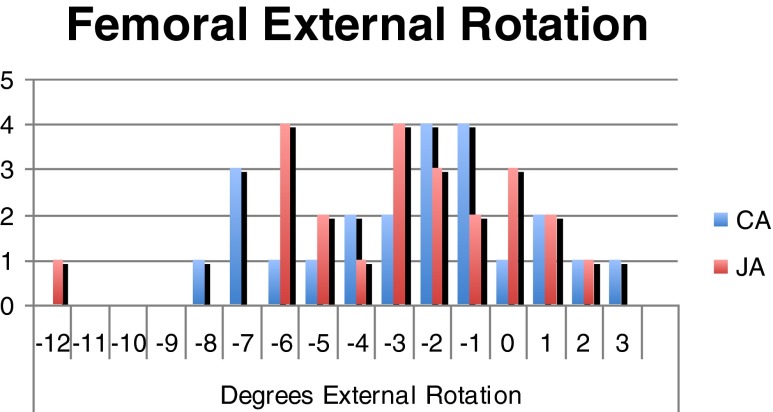
The femoral rotation angle results are shown in Fig. 2 with perfect alignment (0°) achieved in three JATKRs and in one CATKR. The difference between the groups was not statistically significant.
Fig. 2.
Femoral prosthesis external rotation (positive values imply external, negative values imply internal rotation)
Tibial prosthesis alignment
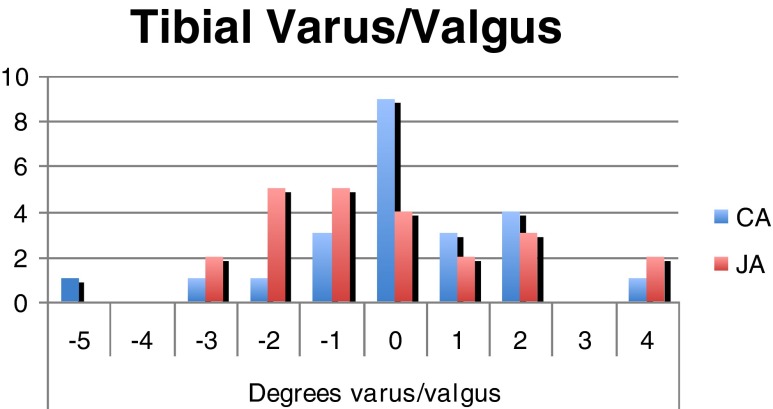
Tibial varus/valgus alignment (Fig. 3) ranged between 4° valgus and 3° varus for the JATKRs (mean deviation of 0.2° varus ±2°) and between 4° valgus and 5° varus for the CATKRs (0.1° valgus 1.9°). Four JATKRs achieved the ideal of 0°, as opposed to nine of the CATKRs. The difference between the groups was not statistically significant.
Fig. 3.
Tibial alignment (positive values imply valgus, negative values imply varus angulation)
The posterior tibial slope demonstrated a non significant mean value of 5° ±2.9° in the JATKRs and 4.7° ±2.7° in the CATKRs.
Femorotibial matching
Matching of the femoral and tibial components was not statistically significant, although this would not be expected given that the computer navigation system does not in fact influence rotation of tibial prosthesis on femoral prosthesis.
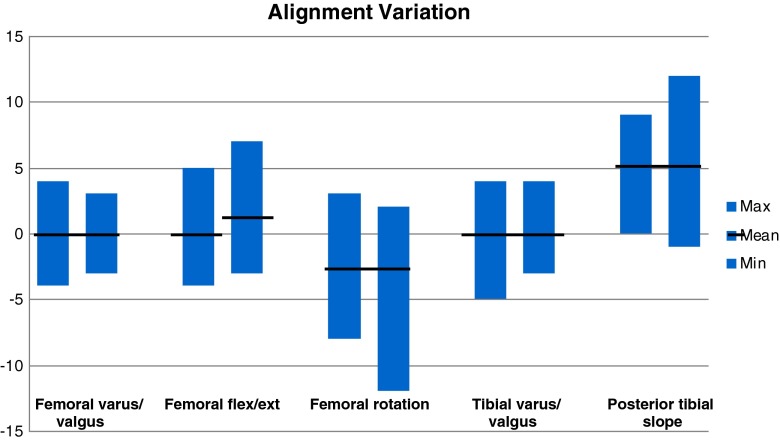
Alignment variation
There was a relatively narrow spread of variation in both groups, particularly in femoral and tibial varus/valgus alignment and femoral flexion/extension (Fig. 4). Trends noticed were a tighter range in the CATKR group compared with the JATKR group in the posterior tibial slope, however this difference was reversed when looking at femoral coronal alignment.
Fig. 4.
Comparison of variation in alignment between jig-assisted (JA) and computer-assisted (CA) TKRs
Despite the outliers being slightly different between the two groups the means remained very similar across all measurements.
Femoral varus/femoral flex/ext femoral rotation tibial varus/posterior tibial valgus valgus slope
Functional outcome
More patients underwent CATKR on the left knee (62.5 %) than the right. The average age was 67 (59–84) in the group that the left knee was computer assisted compared with 68 (50–80) on the right.
The pre-operative scores were similar between the groups with average scores less than one point difference in the HAAS (Table 2).
Table 2.
Pre-operative scores
| Pre-operative scores | |||
|---|---|---|---|
| Measure | Left | Right | |
| Pain | Min | 6 | 7 |
| Max | 14 | 13 | |
| Average | 10 | 9.7 | |
| KS pain | Min | 0 | 0 |
| Max | 30 | 45 | |
| Average | 13 | 15.0 | |
| Function | Min | 17 | 14 |
| Max | 33 | 28 | |
| Average | 24 | 23.4 | |
| KS function | Min | 5 | 0 |
| Max | 80 | 50 | |
| Average | 39 | 35.7 | |
| Activity | Min | 2 | 2 |
| Max | 4 | 4 | |
| Average | 3 | 2.9 | |
All scores improved between pre-operatively and postoperatively with pain and function scores having declined slightly by the five-year assessment.
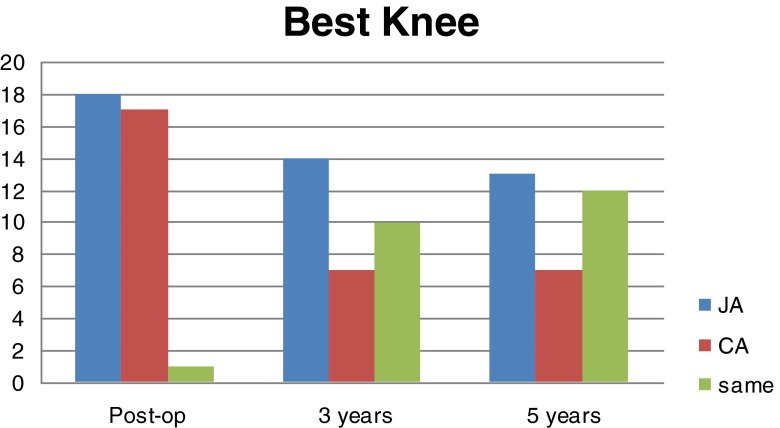
When asked which knee was better, only one patient thought both knees were the same at the first assessment but this number increased to 12 of the 32 patients at the five-year mark (Fig. 5). At five years, 40.6 % of patients thought their jig-assisted knee was the better knee compared with 21.9 % their computer-assisted knee and 37.5 % of patients who felt they were the same.
Fig. 5.
Subjective “best” knee vs computer-assisted total knee revision (CATKR)
When divided into two groups according to which knee was replaced with computer assistance, more patients were found to rate their conventional jig-assisted knee than their computer assisted side (Table 3).
Table 3.
CATKR side vs subjective “best” knee
| CATKR vs best knee | ||||
|---|---|---|---|---|
| CATKR side | Time of evaluation | Right | Left | Same |
| Left | Post-op | 11 | 7 | 11 |
| 2010 | 6 | 3 | 7 | |
| Five years | 7 | 4 | 8 | |
| Right | Post-op | 7 | 9 | 0 |
| 2010 | 4 | 6 | 2 | |
| Five years | 3 | 6 | 3 | |
CATKR computer-assisted total knee revision
Discussion
Total knee arthroplasty is a common operation for the management of osteoarthritis, and the positioning of components and alignment are important fundamentals of the procedure to prevent pain and improve the functional outcome for the patient. Although there is controversy as to what constitutes significant malalignment, it has been generally accepted that alignment within 3° of the neutral axis is likely to lead to improved outcomes [3–6].
Multiple studies have assessed the accuracy of computer assisted procedures over the traditional jig-assisted method in improving component alignment with varying results [17–21]. The results of this study confirm those that have shown no statistically significant difference in implant alignment between CATKR and JATKR [18–20], and as such produces further evidence that the routine use of navigation is not required to improve either implant positioning or functional outcome in patients with knee arthritis.
It may be that computer navigation does have a role in complicated cases where there are angular deformities or retained metalware from other procedures [31].
Ritter et al. [32] reviewed implant survival in relation to pre-operative and postoperative alignment and showed the importance of correct alignment in reducing the risk of implant failure. However they found failure rates only increased if there was greater than 7.4° of valgus malalignment. This study demonstrated a relatively narrow range of alignment outcomes, well below the limits set by Ritter et al. [32], which may in part be due to the single surgeon series, but failed to demonstrate any advantage in CATKR. Although the follow-up period was short we were unable to show any improvement in implant survival with CATKR compared to JATKR.
It could be assumed that alignment closer to neutral would improve functional outcome and pain and give an overall better knee subjectively. The results of this study demonstrated that more patients had a preference for the JATKR (41 % compared to 22 %). The functional results were similar when patients were asked to score each knee independently, which highlights one of the problems of comparing bilateral procedures. Patients have difficultly differentiating knee function when both are functioning satisfactorily. No patient highlighted that one knee was markedly different from the other, confirming that the mid-term outcome from both procedures is reliable for this implant.
The surgeon involved found the side done by computer assistance took longer than the jig-assisted side. This supports the results of other studies which have shown up to a 55 % increase in length of surgery [15, 22, 27], corresponding with increased procedural costs. Other extra costs are also associated with purchasing and training for both surgeons and nursing staff. These increased costs do not seem justified in the current health environment.
This study has limitations in that it was a relatively small group of patients and the side for surgery was “randomly” allocated by the operating room staff to suit their set-up, resulting in a larger number of right compared to left TKRs. However, by performing the procedures in the same patient during one operation and by one experienced surgeon, it helped to remove some of the confounding factors. We believe these limitations are offset by the strength of the study which was the “blinding” of all patients and assessments, and the use of a validated radiological method to give precise implant positioning. The functional outcome scores were an overall score of patient function rather than an assessment of each knee separately as it is difficult for a patient who has undergone bilateral knee joint replacements to score each knee separately in terms of function. We did however assess which was the patient’s better knee by asking them directly.
In conclusion, our study shows no improvement in alignment of the prosthesis with computer-assisted navigation in TKR. More patients noted a subjectively better knee in the conventional jig-assisted knee than in the computer-assisted knee.
Acknowledgments
Conflict of interest
There are no conflicts of interest.
References
- 1.Wasiliewski RC, et al. Wear patterns on retrieved polyethylene inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop. 1995;318:176–181. [PubMed] [Google Scholar]
- 2.Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res. 1988;266:49–64. [PubMed] [Google Scholar]
- 3.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59:77–79. [PubMed] [Google Scholar]
- 4.Ritter MA, et al. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 5.Berend ME, et al. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 6.Jeffery RS, et al. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 7.Rienmüller A, Guggi T, Gruber G, Preiss S, Drobny T. The effect of femoral component rotation on the five-year outcome of cemented mobile bearing total knee arthroplasty. Int Orthop. 2012;36(10):2067–2072. doi: 10.1007/s00264-012-1628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. 2009;24:560–569. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 9.Sparman M, et al. Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br. 2003;85:830–835. [PubMed] [Google Scholar]
- 10.Stulberg SD, et al. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am. 2002;84(Suppl 2):90–98. [PubMed] [Google Scholar]
- 11.Chin PL, et al. Randomised control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20:618–626. doi: 10.1016/j.arth.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 12.Bathis H, et al. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86:682–687. doi: 10.1302/0301-620X.86B5.14927. [DOI] [PubMed] [Google Scholar]
- 13.Haaker RG, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. doi: 10.1097/01.blo.0000150564.31880.c4. [DOI] [PubMed] [Google Scholar]
- 14.Chauhan S, Scott R, Breidahl W, Beaver R. Computer-assisted knee arthroplasty versus a conventional jig-based technique: a randomised, prospective trial. J Bone Joint Surg Br. 2004;86-B:372–377. doi: 10.1302/0301-620X.86B3.14643. [DOI] [PubMed] [Google Scholar]
- 15.Zhang G, Chen J, Chai W, Liu M, Wang Y. Comparison between computer-assisted-navigation and conventional total knee arthroplasties in patients undergoing simultaneous bilateral procedures—a randomized clinical trial. J Bone Joint Surg Am. 2011;93(13):1190–1196. doi: 10.2106/JBJS.I.01778. [DOI] [PubMed] [Google Scholar]
- 16.Mason J, Fehring T, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8):1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Yi-Jan Weng MD, Robert Wen-Wei Hsu MD, Wei-Hsiu Hsu MD. Comparison of computer-assisted navigation and conventional instrumentation for bilateral total knee arthroplasty. J Arthroplasty. 2009;24(5):668–673. doi: 10.1016/j.arth.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Kim Y, Kim J, Choi Y, Kwon O. Computer-assisted surgical navigation does not improve the alignment and orientation of the components in total knee arthroplasty. J Bone Joint Surg Am. 2009;91(1):14–19. doi: 10.2106/JBJS.G.01700. [DOI] [PubMed] [Google Scholar]
- 19.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92(12):2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 20.Kim YH, Park JW, Kim JS. Computer-navigated versus conventional total knee arthroplasty. A prospective randomized trial. J Bone Joint Surg Am. 2012;94:2017–2024. doi: 10.2106/JBJS.L.00142. [DOI] [PubMed] [Google Scholar]
- 21.Cinotti G, Ripani F, Sessa P, Giannicola G. Combining different rotational alignment axes with navigation may reduce the need for lateral retinacular release in total knee arthroplasty. Int Orthop. 2012;36(8):1595–1600. doi: 10.1007/s00264-012-1523-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saragaglia D, Picard F, Chaussard C, Montbarbon E, Leitner F, Cinquin P. Computer-assisted knee arthroplasty: comparison with a conventional procedure. Results of 50 cases in a prospective randomized study. Rev Chir Orthop Reparatrice Appar Mot. 2001;87(1):18–28. [PubMed] [Google Scholar]
- 23.Koshino T, Takeyama M, Jiang LS, Yoshida T, Saito T. Underestimation of varus angulation in knees with flexion deformity. Knee. 2002;9:275–279. doi: 10.1016/S0968-0160(02)00049-2. [DOI] [PubMed] [Google Scholar]
- 24.Krackow KA, Pepe CL, Galloway EJ. A mathematical analysis of the effect of flexion and rotation on apparent varus/valgus alignment at the knee. Orthopaedics. 1990;13:861–868. doi: 10.3928/0147-7447-19900801-09. [DOI] [PubMed] [Google Scholar]
- 25.Kawakami H, Sugano N, Yonenobu K, Yoshikawa H, Ochi T, Hattori A, Suzuki N. Effects of rotation on measurement of lower limb alignment for knee osteotomy. J Othop Res. 2004;22:1248–1253. doi: 10.1016/j.orthres.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 26.Henckel J, Richards R, Lozhkin K, Harris S, Baena FM R y, Barret ARW, Cobb JP. Very low-dose computed tomography for planning and outcome measurement in knee replacement—the imperial knee protocol. J Bone Joint Surg Br. 2006;88-B:1513–1518. doi: 10.1302/0301-620X.88B11.17986. [DOI] [PubMed] [Google Scholar]
- 27.Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM. Computer-assisted total knee replacement. A controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (The Perth CT protocol) J Bone Joint Surg Br. 2004;86-B:818–823. doi: 10.1302/0301-620X.86B6.15456. [DOI] [PubMed] [Google Scholar]
- 28.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomised study of computer-assisted and conventional total knee arthroplasty. Three dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89:236–243. doi: 10.2106/JBJS.F.00386. [DOI] [PubMed] [Google Scholar]
- 29.Talbot S, Hooper G, Stokes A, Zordan R. Use of a new high-activity arthroplasty score to assess function of young patients with total hip or knee arthroplasty. J Arthroplasty. 2010;25(2):268–273. doi: 10.1016/j.arth.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 30.Armitage P, Berry G, Mathews J (2002) Statistical methods in medical research. Oxford, Blackwell
- 31.Tigani D, Masetti G, Sabbioni G, Ben Ayad R, Filanti M, Fosco M. Computer-assisted surgery as indication of choice: total knee arthroplasty in case of retained hardware or extra-articular deformity. Int Orthop. 2012;36(7):1379–1385. doi: 10.1007/s00264-011-1476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ritter M, Davis K, Davis P, Farris A, Malinzak R, Berend M, Meding J. Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am. 2013;95(2):126–131. doi: 10.2106/JBJS.K.00607. [DOI] [PubMed] [Google Scholar]