Abstract
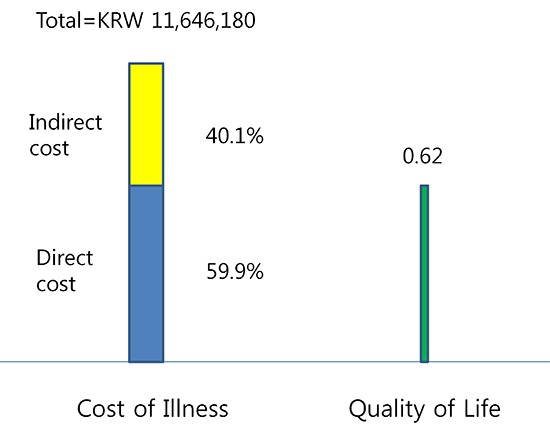
The objectives of this study were to estimate the cost-of-illness (COI) and health-related quality of life (HRQOL) in patients with ankylosing spondylitis (AS) in Korea and to evaluate the effects of socio-demographic and clinical factors on the COI and the HRQOL. Face-to-face interview surveys were taken from patients with AS at the Rheumatology Clinic of Seoul National University Hospital. Direct medical and non-medical costs, indirect costs (productivity loss due to job loss and sick leave), and deterioration of HRQOL in patients with AS were measured. Factors associated with COI and HRQOL were analyzed with multiple regression and multivariate logistic regression. A total of 191 patients with AS was enrolled in the study. The COI in patients with AS amounted to 11,646,180 Korean Won (KRW) per patient, and their HRQOL was 0.62. As functional severity worsened, the total costs increased (class I, KRW 7.7 million; class II, KRW 12.9 million; classes III & IV, KRW 25.2 million) and the HRQOL scores decreased (class I, 0.72; class II, 0.61; classes III & IV, 0.24). Functional severity is the major determinant of the COI and HRQOL in patients with AS.
Graphical Abstract
Keywords: Spondylitis, Ankylosing; Arthritis, Rheumatoid; Cost; Quality of Life
INTRODUCTION
Ankylosing spondylitis (AS) is a chronic, progressive inflammatory disease characterized by structural changes accompanied by pain and stiffness of the back, peripheral joints and inflammation of extra-articular sites such as the eyes, heart and lungs (1, 2). The prognosis for AS varies, and management centers on controlling pain and improving physical function (3). The prevalence of AS varies between 0.21% and 1.9% worldwide, and 1% and 2% within Europe (4). The prevalence of AS in Korea is about 0.4% (5), which is a little higher than that (0.2%-0.3%) in China (6). The disease is diagnosed in early adulthood and functional limitations may lead to work capacity impairment and increased consumption of healthcare resources, as well as reduced quality of life (QOL) as a result of disability and pain (7-9).
Increased healthcare utilization or need for formal and informal care, and decreased working capability of patients due to structural changes, pain, stiffness, and functional limitation, have an impact on not only the patients or their families but also on society as a whole (10). Recently, new drug compounds such as tumor necrosis factor-α (TNF-α) inhibitors have been introduced with strong therapeutic effects on AS to reduce pain and functional impairment. However, their use is constrained by high medication costs, around USD 15,000-25,000 per patient per year (11, 12). This implies that consideration of cost-of-illness (COI) has become increasingly important in decisions regarding resource allocation, intervention design and use of biologic agents in such individuals with chronic inflammatory disabling conditions.
With regard to functional limitation, QOL and COI, AS is often compared to rheumatoid arthritis (RA), another common type of chronic inflammatory arthritis. It is generally known that patients with RA are more limited in physical function than patients with AS (13), and that physical health-related QOL of patients with RA is lower than that of patients with AS (14) while mental health-related QOL of patients with RA and AS shows mixed results (14, 15). It is also known that COI of patients with RA is higher than that of patients with AS (10, 16, 17), and that the proportion of indirect costs is larger than that of the direct costs in both diseases, reflecting the high burden of the diseases on work participation (10, 17). However, the differences in functional limitation, QOL and COI between patients with AS and RA may be affected by potential confounding factors such as age, gender, or disease duration since the two diseases affect different patient populations (13).
Korean studies on the health-related quality of life (HRQOL) of inflammatory arthritides show similar results to studies in other countries: when evaluated using SF-36, the physical HRQOL of patients with RA was lower than that of patients with AS while the mental HRQOL of patients with the two diseases was similar, and when using Korean version of European Quality of Life-5 Dimension (KEQ-5D), the HRQOL of patients with RA (0.58) was lower than that of patients with AS (0.63) (18, 19). In contrast, there are few studies that examined the COI of patients with AS in the Korean healthcare setting, though there is one recent study on the COI of patients with RA (20).
The results of burden-of-disease studies can be used for prioritizing healthcare resources and justifying the needs for spending on disease prevention, management, and social intervention. This can be achieved, in particular, through studies comparing COI and HRQOL between diseases. Given that few such studies have been carried out in Korea, the aims of the current study were to estimate the COI and HRQOL among patients with AS, and to evaluate the effects of socio-demographic and clinical factors on the COI and the HRQOL.
MATERIALS AND METHODS
The following data sources were used to estimate the COI and HRQOL of patients with AS: patient surveys, medical chart reviews and reviews of electronic hospital records.
Patients
The patients were enrolled at the Rheumatology Clinic of Seoul National University Hospital located in Seoul, Korea between July 19, 2010 and October 22, 2010. The inclusion criteria were as follows: 1) The patient should meet the 1984 modified New York criteria for AS (21), and 2) the patient must have visited the medical institution at least once before the interview. Functional status was assessed according to the American College of Rheumatology (ACR) 1991 revised criteria for the classification of global functional status in RA (22).
Socio-demographic and clinical characteristics
Socio-demographic characteristics such as age, gender, marital status, education, household income, employment status and health insurance type were collected from the patient surveys. Clinical features were collected from the reviews of the medical charts, which included information pertaining to comorbidity and medication including biologic agents. Diseases assessed as comorbidity included diabetes mellitus, hypertension, pulmonary tuberculosis, dermatitis, Behcet's disease.
Cost of illness (COI)
The COI of patients with AS was estimated from a societal perspective. Taking into consideration of Korean circumstances, direct medical costs included in-hospital costs, prescription drugs, private physiotherapy, oriental medicine and other alternative medicine costs, whereas direct non-medical costs included travel, auxiliary devices, dietary supplements, and home assistance costs. Indirect costs included productivity loss from job loss and sick leave (23, 24). Since it was impossible to estimate the mortality rate of patients with AS, lost productivity from premature death was not included in this study.
In-hospital costs were estimated from hospital electronic data records including expenses for physician visits, treatments, hospitalization, and monitoring. Out-of-hospital medical costs, direct non-medical costs, and indirect costs were estimated based on patient surveys from face-to-face interviews. The reference period for out-of-hospital medical costs, direct non-medical costs, and sick leave costs was 1 yr. Productivity loss caused by disease-related job loss was estimated by applying the duration of the patient's unemployment until the normal retirement age and annual increase in wages to the wage they received prior to the loss of work. It was assumed that the age at retirement was 60 yr for both genders. The annual wage increase rate was obtained from the Korean Statistical Information Service (25).
Health-related quality of life (HRQOL)
The HRQOL of the patients was analyzed based on face-to-face interview questionnaires using KEQ-5D. Utility values were obtained through a tariff system developed in Korea, which applied a time trade-off method to derive preferences on different health statuses from 287 adults residing in urban areas (26).
Data analysis
Descriptive statistics (frequency, percentage, mean and standard deviation) were used to analyze the patient characteristics, costs and HRQOL. To identify factors affecting the total costs, direct costs and HRQOL, multiple regression analysis was used, and to identify factors affecting the incidence of indirect costs, multivariate logistic regression was used. Among those factors are age, gender, marital status, education and household income of the patients as well as comorbidity and functional status.
Ethics statement
This study was carried out with the approval of the institutional review board of Seoul National University Hospital (IRB No. H-1007-167-325). Informed consent was confirmed by the board.
RESULTS
Patient demographics and clinical characteristics
In total, 191 patients with AS were consecutively enrolled in this study. The majority of patients with AS were men (164 patients, 85.9%), and the mean age (SD) was 39.3 (12.3) yr. Additionally, 57.6% of the patients received education at a college level or higher and 37.7% were unemployed. The monthly average household income of the patients with AS was 4.1 million Korean Won (KRW) (Table 1).
Table 1.
Socio-demographic and clinical characteristics of patients with ankylosing spondylitis (n=191)
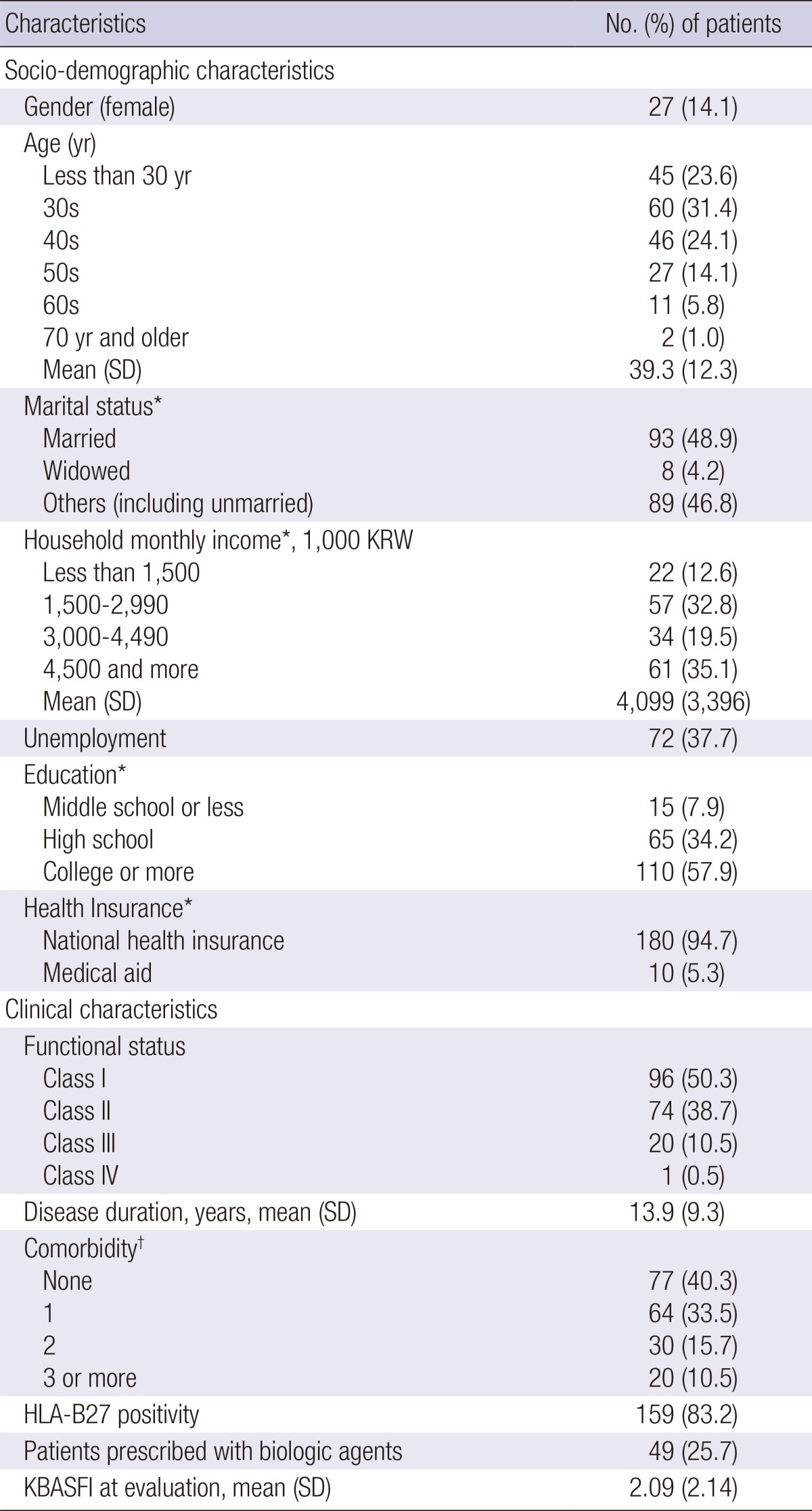
*Individuals with missing values are excluded. †Including diabetes mellitus, hypertension, pulmonary tuberculosis, dermatitis, Behcet's disease etc. SD, standard deviation; KRW, Korean Won; KBASFI, Korean Bath Ankylosing Spondylitis Functional Index.
In terms of functional status classified by ACR, 50.3% (96 patients) and 38.7% (74 patients) of patients with AS were class I and II, respectively. The mean disease duration of patients with AS was 13.9 yr. About 60% of the patients had at least one comorbidity. With respect to disease-modifying anti-rheumatic drugs, 25.7% (49 patients) with AS were treated with TNF-α inhibitors such as etanercept, infliximab, adalimumab etc. (Table 1).
Cost of illness
The total COI for patients with AS amounted to KRW 11.6 million per patient per year. Of the total, direct costs amounted to KRW 7.0 million (59.9%) while indirect costs amounted to KRW 4.7 million (40.1%). Loss of work as an indirect cost accounted for the largest proportion of the total costs (34.5%), followed by two items within the direct cost category, in-hospital costs (29.7%) and prescription drug costs (16.7%) (Table 2).
Table 2.
Direct and indirect costs per patient per year in patients with ankylosing spondylitis
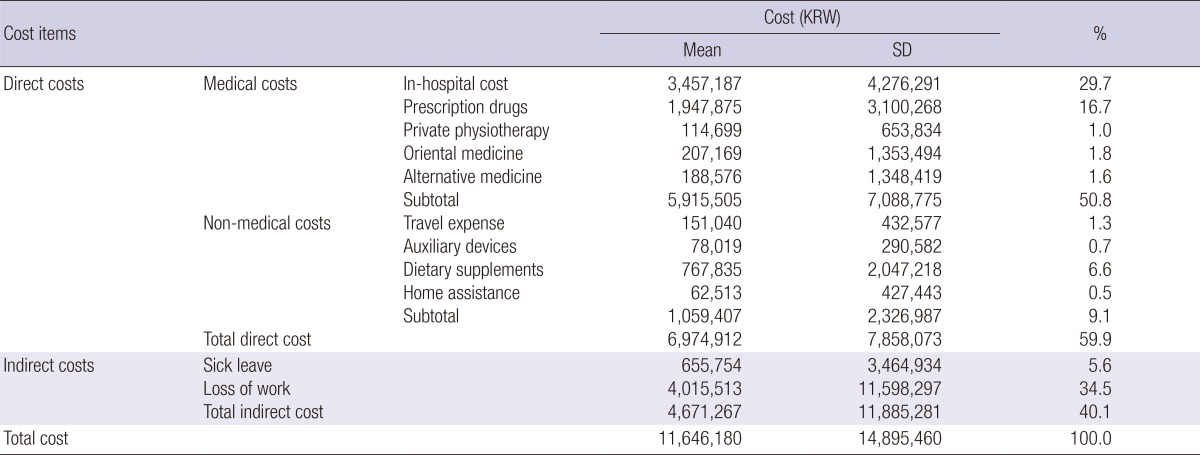
KRW, Korean Won; SD, standard deviation.
Analyzing the COI by the characteristics of the patients, the COI for female patients (KRW 13.1 million) was higher than that for male patients (KRW 11.4 million) and the proportion of direct costs in male patients with AS was as high as 64.4% of the total COI. The COI of patients with AS increased with age until their 50s, after which it decreased dramatically since indirect costs were less likely to occur. The decrease in the COI of old patients may be related to reduced disease activity. The higher the level of education received by the patients, the lower their COI was. This was due to the decrease in the proportion of indirect costs among those patients with higher education. In terms of household income, there were no regular trends observed in the total COI and in the proportion of direct costs. Unemployment contributed to a substantial increase in total COI for patients with AS, which was due to increased indirect costs (Table 3).
Table 3.
Cost-of-illness (COI) and proportion of direct costs in ankylosing spondylitis by patient characteristics
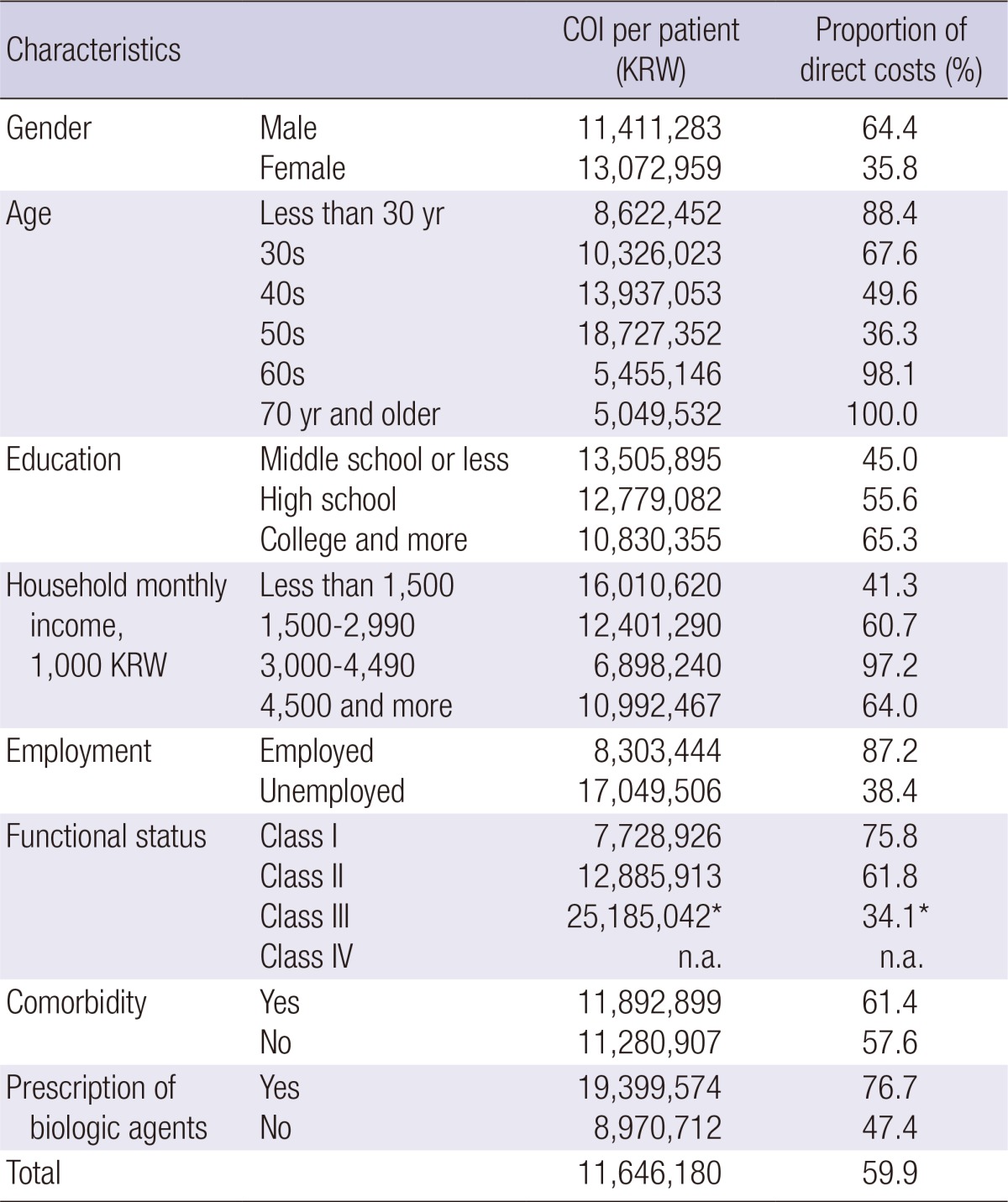
*Including 1 patient with functional class IV. KRW, Korean Won; n.a., not applicable.
With regard to the clinical characteristics of patients with AS, the COI increased with functional deterioration (FC I, KRW 7.7 million; FC II, KRW 12.9 million; FC III & IV, KRW 25.2 million) and the proportion of direct costs was high among class I (75.8%) and II (61.8%) patients while it was low among class III & IV (34.1%) patients. The difference in the COI between patients with and without comorbidity was not evident. In addition, the COI for patients treated with biologic agents including TNF-α inhibitors (KRW 19.4 million) was twice as high as that of patients who were not treated with biologic agents (KRW 9.0 million) (Table 3).
Health-related quality of life
The overall HRQOL of patients with AS was estimated to be 0.62. The HRQOL of patients with AS decreased with age and increased with education and household income. The HRQOL of unemployed patients was lower than that of employed patients. Moreover, the HRQOL deteriorated as their functional severity worsened (FC I, 0.72; FC II, 0.61; FC III & IV, 0.24). Given that 0 indicates death and 1 indicates perfect health (KEQ-5D anchors), the progression of AS resulted in a substantial deterioration in the HRQOL. The HRQOL decreased with comorbidity, whereas it showed no difference between patients treated with and without biologic agents (Table 4). Considering that TNF-α inhibitors are not generally administered to the patients with low disease activity, their HRQOL was similar to the HRQOL of patients with high disease activity to whom TNF-α inhibitors are often administered.
Table 4.
Health-related quality of life (HRQOL) in ankylosing spondylitis by patient characteristics
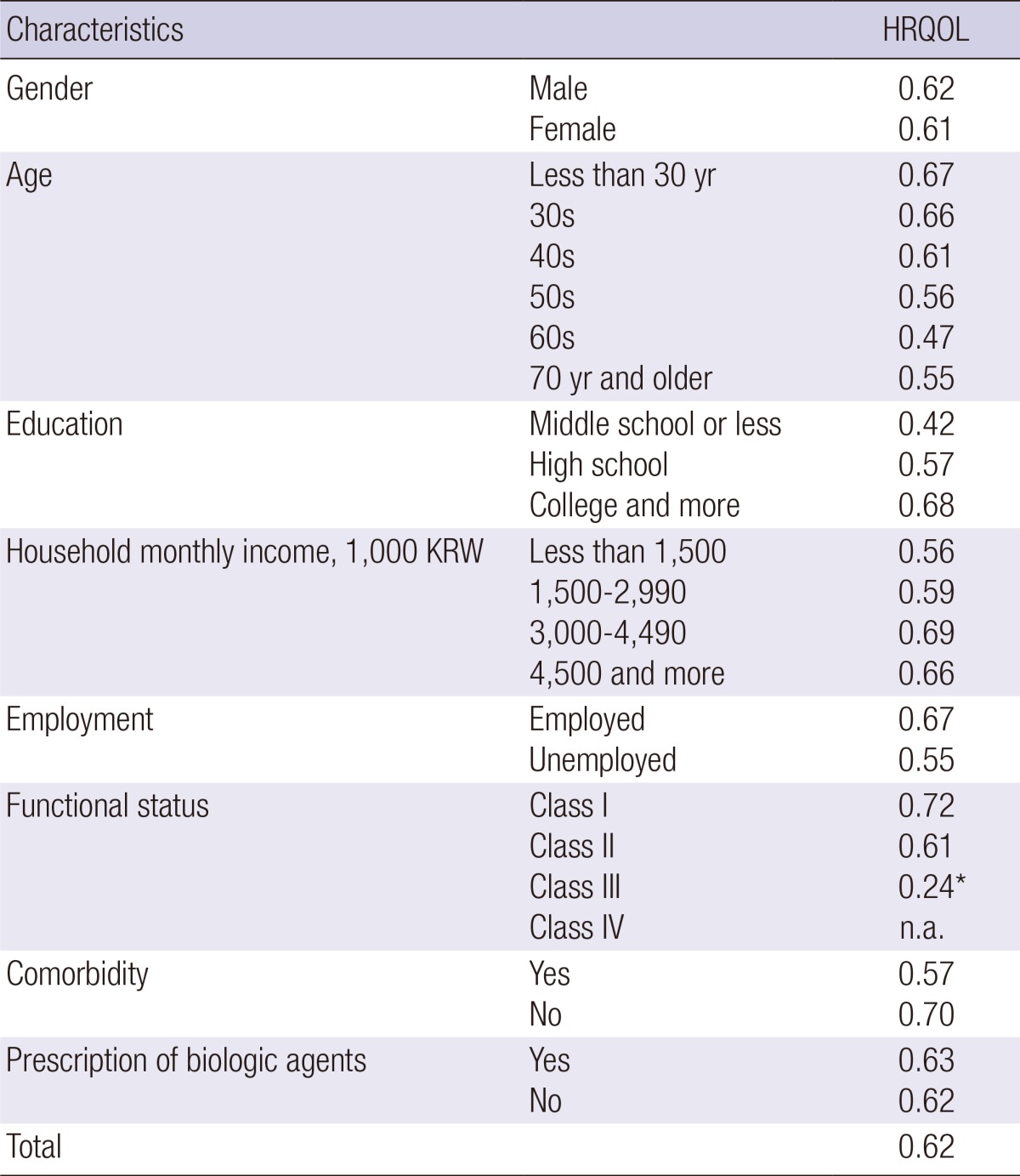
*Including 1 patient with functional class IV. KRW, Korean Won; n.a., not applicable.
Factors affecting the COI and HRQOL
The results of multiple regression and multivariate logistic regression showed that functional severity was the most significant determinant of the COI; FC I and II showed lower total and direct costs compared to FC III and IV. The probability of patients with FC I incurring indirect costs was significantly lower than that of patients with FC III and IV in AS (P=0.039). Comorbidity tended to be associated with direct costs (P=0.088). Apart from functional severity, residential area (P=0.012), marital status (P=0.011) and education (P=0.026) significantly affected the occurrence of indirect costs among patients with AS while household income tended to be associated with indirect costs (P=0.099) (Table 5).
Table 5.
Multiple regression and multivariate logistic regression models for cost-of-illness in patients with ankylosing spondylitis
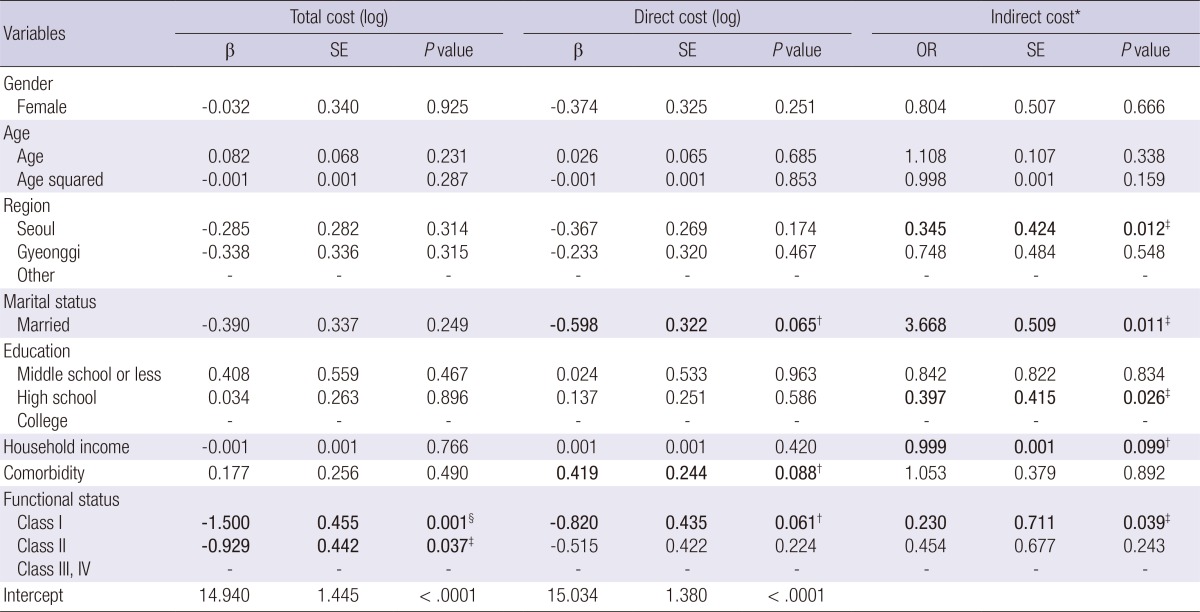
*Indirect cost occurred, 1; not occurred, 0.†P<0.1, ‡P<0.05, §P<0.01. SE, standard error; OR, odds ratio.
The factors affecting the HRQOL of patients with AS were the functional status and residential area. In terms of functional severity, classes I (P<0.001) and II (P=0.022) showed a higher HRQOL compared to classes III and IV (Table 6).
Table 6.
Multiple regression model for quality of life in patients with ankylosing spondylitis
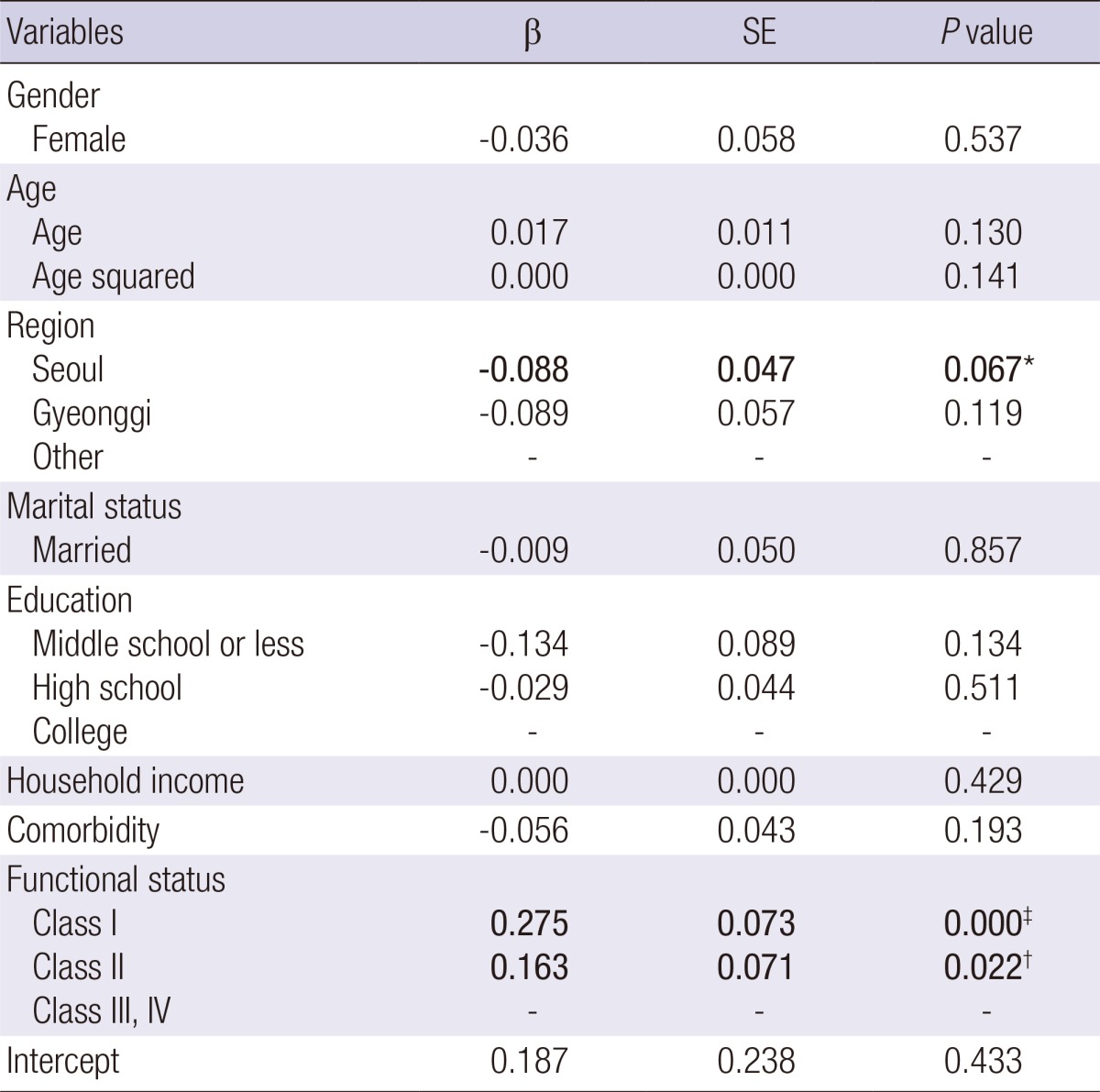
*P<0.1, †P<0.05, ‡P<0.01. SE, standard error.
DISCUSSION
This study was carried out to estimate the COI and HRQOL of patients with AS, and it would be informative to compare them with those of patients with RA, which is one of the common types of inflammatory arthritis. There is one recent study on the COI and HRQOL in patients with RA in the same clinical setting in Korea, carried out from a societal perspective (20), which made it feasible to compare the two diseases. In comparison with the results of this recent study of patients with RA, the COI of patients with AS was almost twice as high as that of patients with RA (AS, KRW 11.6 million; RA, KRW 6.7 million). The costs of patients with RA were collected throughout 2009 while those of patients with AS were collected in 2010. For a better comparison of the COI between AS and RA, the costs of patients with RA were adjusted for inflation.
This is in stark contrast with previous studies in other countries, which showed that the annual COI of patients with RA was higher than that of patients with AS (10, 17). If we break down the COI in the current study, the direct cost for patients with AS (KRW 7.0 million) was more than twice as high as that for patients with RA (KRW 3.2 million), while the indirect cost for patients with AS (KRW 4.7 million) was only about 34% higher than that for patients with RA (KRW 3.5 million). In other words, the difference in the COI between the two diseases was attributable mainly to the difference in direct costs, which was in turn incurred by the difference in in-hospital costs; the proportion of in-hospital costs amounted to 29.7% in patients with AS while it was only 10.5% in patients with RA (20). The high proportion of in-hospital costs in AS has to do with the relatively high prescription rate of expensive TNF-α inhibitors, which are mainly injected at hospitals in Korea.
In terms of functional status, half of the patients with AS belonged to FC I and almost 90% belonged to FC I or II. Taking into account their functional status, it was anticipated that patients with AS would show a higher HRQOL and lower COI than patients with RA. On the contrary, the COI of patients with AS was almost two times higher than that of patients with RA in Korea due to the greater use of expensive biologics. This can be explained by the following. First, there are disparities in the socio-economic characteristics between patients with AS and RA. About 86% of the patients with AS were men and the mean age was 39.3 yr while about 81% of the patients with RA were women and the mean age was 62.5 yr (20). Besides, patients with AS had longer schooling years, were less unemployed, and reported a higher monthly household income than patients with RA. These socio-economic characteristics seem to explain partly why AS patients whose functional status was not so poor were prescribed expensive biologics at a tertiary university hospital.
Second, the high COI of patients with AS compared to patients with RA could be partly related to the reimbursement policy for biologics issued by the Health Insurance Review and Assessment Service (HIRA). HIRA has allowed TNF-α inhibitors to be used in AS patients with high disease activity once they fail 2 nonsteroidal anti-inflammatory agents in 3 months. Therefore, severely ill AS patients can have access to expensive TNF-α inhibitors with a copayment rate of 10% at a relatively earlier (6 months for RA patients) time point throughout their treatment. The prescription rate of TNF-α inhibitors was also influenced by the patients' socio-economic status; as seen in the results of this study, patients with AS whose income and education level were higher than patients with RA were prescribed biologic agents more frequently (20).
The results also showed that the proportion of indirect costs was 40.1% for AS while it was 52.7% for RA (20). This means that, in the case of AS, the proportion of indirect costs was smaller than that of direct costs while the opposite was true in the case of RA. Boonen and Mau (16) reported that the unemployment rate was higher among patients with RA than that of patients with AS, which was particularly the case in females and less educated patients. This is consistent with the results from the Korean studies. Since less educated patients were more likely to be involved in manual work, functional deterioration resulting from rheumatic diseases tended to hinder them from maintaining their jobs. This is the reason why the proportion of indirect costs among patients with RA of whom the majority were female and less educated was much higher than that of patients with AS in Korea.
Meanwhile, it was revealed that the HRQOL of patients with AS (0.62) was higher than that of patients with RA (0.49) and that this was also the case across functional status. Salaffi et al. (15) showed that the physical health- and mental health-related QOL of patients with RA were lower than those of patients with AS in Italy, which is consistent with the findings of the current study. However, it is not necessarily the case with German patients. Chorus et al. (14) showed that patients with RA had a lower physical health-related QOL and a higher mental health-related QOL than patients with AS in Germany and that there were no significant differences in somatic pain, physical role functioning, social functioning, emotional role functioning, vitality or general health perception between patients with RA and AS. Zink et al. (27) also reported that the extent to which patients with RA and AS complained of disability and pain was similar until the age of 70 yr, after which patients with RA complained of pain more frequently than patients with AS.
The functional status of patients was the most significant factor associated with the HRQOL of patients with AS as well as the HRQOL of patients with RA (20), which is consistent with findings from previous studies carried out in Korea and other countries (18, 19, 28-31). Salaffi et al. (15) found that comorbidity influenced the HRQOL of patients with RA and AS; however, it did not affect the HRQOL of patients with AS in the current study. Further analyses taking into account the number and mix of comorbidities are necessary in future studies.
There are a few limitations to this study. First, the COI and HRQOL of patients with AS were estimated based on data obtained from one large university hospital, so the study results need to be generalized with caution. Second, the results from the current study on AS were compared to those from the previous study on RA in the discussion, though there was an eight-month time lag between the two studies. However, there was no noticeable event in between that may have influenced the COI and HRQOL in patients with AS and RA. In fact, recruiting patients from the same clinical setting may have helped further comparison of the two diseases.
In conclusion, this study, when compared with the previous study on RA, indicates that the COI of patients with AS is much higher than that of RA while the HRQOL of patients with AS is higher than that of RA. Further studies that examine the causes and solution of the disparity between HRQOL and medical costs in AS versus RA in the Korean healthcare setting are called for.
ACKNOWLEDGMENTS
We would like to thank Hye-Kyung Son at Hallym Medical Foundation who participated in data collection and statistical analysis.
Footnotes
This research was funded by a grant of the Korea Healthcare Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI10C2020) and by grant No. R31-2008-000-10103-0 from the World Class University program of the Ministry of Education, Science and Technology and the National Research Foundation of Republic of Korea.
The authors have no conflicts of interest to disclose.
References
- 1.Russell A. Ankylosing spondylitis: history. London: Mosby; 2007. pp. 1–2. [Google Scholar]
- 2.Sieper J, Braun J, Rudwaleit M, Boonen A, Zink A. Ankylosing spondylitis: an overview. Ann Rheum Dis. 2002;61:iii8–iii18. doi: 10.1136/ard.61.suppl_3.iii8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boonen A, de Vet H, van der Heijde D, van der Linden S. Work status and its determinants among patients with ankylosing spondylitis: a systematic literature review. J Rheumatol. 2001;28:1056–1062. [PubMed] [Google Scholar]
- 4.Glasnović M. Epidemiology of spondylarthritides. Reumatizam. 2011;58:24–35. [PubMed] [Google Scholar]
- 5.Korea Center for Disease Control & Prevention. 2006 prevalence survey of rare refractory diseases. [accessed on 28 April 2010]. Available at http://helpline.nih.go.kr/cdchelp/cyber.gst?method=detailView&ctype=c&cateCode=11&searchKind=&searchWord=&curPage=1&NO_CYBER_IDX=533.
- 6.Zhu TY, Tam LS, Lee VW, Hwang WW, Li TK, Lee KK, Li EK. Costs and quality of life of patients with ankylosing spondylitis in Hong Kong. Rheumatology (Oxford) 2008;47:1422–1425. doi: 10.1093/rheumatology/ken287. [DOI] [PubMed] [Google Scholar]
- 7.Boonen A, van der Heijde D, Landewé R, Guillemin F, Rutten-van Mölken M, Dougados M, Mielants H, de Vlam K, van der Tempel H, Boesen S, et al. Direct costs of ankylosing spondylitis and its determinants: an analysis among three European countries. Ann Rheum Dis. 2003;62:732–740. doi: 10.1136/ard.62.8.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boonen A, van der Heijde D, Landewé R, Spoorenberg A, Schouten H, Rutten-van Mölken M, Guillemin F, Dougados M, Mielants H, de Vlam K, et al. Work status and productivity costs due to ankylosing spondylitis: comparison of three European countries. Ann Rheum Dis. 2002;61:429–437. doi: 10.1136/ard.61.5.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ward MM. Health-related quality of life in ankylosing spondylitis: a survey of 175 patients. Arthritis Care Res. 1999;12:247–255. [PubMed] [Google Scholar]
- 10.Franke LC, Ament AJ, van de Laar MA, Boonen A, Severens JL. Cost-of-illness of rheumatoid arthritis and ankylosing spondylitis. Clin Exp Rheumatol. 2009;27:S118–S123. [PubMed] [Google Scholar]
- 11.Ara RM, Reynolds AV, Conway P. The cost-effectiveness of etanercept in patients with severe ankylosing spondylitis in the UK. Rheumatology (Oxford) 2007;46:1338–1344. doi: 10.1093/rheumatology/kem133. [DOI] [PubMed] [Google Scholar]
- 12.Bonafede MM, Gandra SR, Watson C, Princic N, Fox KM. Cost per treated patient for etanercept, adalimumab, and infliximab across adult indications: a claims analysis. Adv Ther. 2012;29:234–248. doi: 10.1007/s12325-012-0007-y. [DOI] [PubMed] [Google Scholar]
- 13.Louie GH, Reveille JD, Ward MM. Challenges comparing functional limitations in rheumatoid arthritis and ankylosing spondylitis. Clin Exp Rheumatol. 2009;27:S83–S91. [PMC free article] [PubMed] [Google Scholar]
- 14.Chorus AM, Miedema HS, Boonen A, van der Linden S. Quality of life and work in patients with rheumatoid arthritis and ankylosing spondylitis of working age. Ann Rheum Dis. 2003;62:1178–1184. doi: 10.1136/ard.2002.004861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salaffi F, Carotti M, Gasparini S, Intorcia M, Grassi W. The health-related quality of life in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis: a comparison with a selected sample of healthy people. Health Qual Life Outcomes. 2009;7:25. doi: 10.1186/1477-7525-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boonen A, Mau W. The economic burden of disease: comparison between rheumatoid arthritis and ankylosing spondylitis. Clin Exp Rheumatol. 2009;27:S112–S117. [PubMed] [Google Scholar]
- 17.Huscher D, Merkesdal S, Thiele K, Zeidler H, Schneider M, Zink A German Collaborative Arthritis Centres. Cost of illness in rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and systemic lupus erythematosus in Germany. Ann Rheum Dis. 2006;65:1175–1183. doi: 10.1136/ard.2005.046367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim TJ, Oh GT, Ju EK, Lee HS, Kim TH, Jun JB, Jung SS, Yu DH, Bae SC. Health-related quality of life in Korean patients with ankylosing spondylitis spndylitis [in Korean] J Korean Rheum Assoc. 2002;9:S106–S116. [Google Scholar]
- 19.Kim CG, Oh KT, Choe JY, Bae SC. Health-related quality of life Korean patients with rheumatoid arthritis. J Korean Rheum Assoc. 2002;9:S60–S72. [Google Scholar]
- 20.Lee TJ, Park BH, Son HK, Song R, Shin KC, Lee EB, Song YW. Cost of illness and quality of life of patients with rheumatoid arthritis in South Korea. Value Health. 2012;15:S43–S49. doi: 10.1016/j.jval.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 21.Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum. 1984;27:361–368. doi: 10.1002/art.1780270401. [DOI] [PubMed] [Google Scholar]
- 22.Hochberg MC, Chang RW, Dwosh I, Lindsey S, Pincus T, Wolfe F. The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheum. 1992;35:498–502. doi: 10.1002/art.1780350502. [DOI] [PubMed] [Google Scholar]
- 23.Merkesdal S, Ruof J, Huelsemann JL, Schoeffski O, Maetzel A, Mau W, Zeidler H. Development of a matrix of cost domains in economic evaluation of rheumatoid arthritis. J Rheumatol. 2001;28:657–661. [PubMed] [Google Scholar]
- 24.Drummund MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005. [Google Scholar]
- 25.Korean Statistical Information Service. [accessed on 30 April 2010]. Available at http://www.kosis.kr.
- 26.Kang EJ, Shin HS, Park HJ, Jo MW, Kim NY. A valuation of health status using EQ-5D. Korean J Health Econ Policy. 2006;12:19–43. [Google Scholar]
- 27.Zink A, Braun J, Listing J, Wollenhaupt J. Disability and handicap in rheumatoid arthritis and ankylosing spondylitis: results from the German rheumatological database: German Collaborative Arthritis Centers. J Rheumatol. 2000;27:613–622. [PubMed] [Google Scholar]
- 28.Kojima M, Kojima T, Ishiguro N, Oguchi T, Oba M, Tsuchiya H, Sugiura F, Furukawa TA, Suzuki S, Tokudome S. Psychosocial factors, disease status, and quality of life in patients with rheumatoid arthritis. J Psychosom Res. 2009;67:425–431. doi: 10.1016/j.jpsychores.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 29.Alishiri GH, Bayat N, Fathi Ashtiani A, Tavallaii SA, Assari S, Moharamzad Y. Logistic regression models for predicting physical and mental health-related quality of life in rheumatoid arthritis patients. Mod Rheumatol. 2008;18:601–608. doi: 10.1007/s10165-008-0092-6. [DOI] [PubMed] [Google Scholar]
- 30.Ariza-Ariza R, Hernández-Cruz B, Navarro-Sarabia F. Physical function and health-related quality of life of Spanish patients with ankylosing spondylitis. Arthritis Rheum. 2003;49:483–487. doi: 10.1002/art.11197. [DOI] [PubMed] [Google Scholar]
- 31.Ozdemir O. Quality of life in patients with ankylosing spondylitis: relationships with spinal mobility, disease activity and functional status. Rheumatol Int. 2011;31:605–610. doi: 10.1007/s00296-009-1328-2. [DOI] [PubMed] [Google Scholar]


