Abstract
Background
The association between air pollution and cardiovascular diseases is well known, but previous studies only assessed mortality and hospital admissions in North America, Europe, and Northeast Asia. Few studies have been conducted in less-developed countries in regions with a tropical climate. This study evaluated whether short-term exposures to fine particulate matter (PM10) and ozone (O3) were associated with hospital visits for cardiovascular diseases (CVD; ICD-10th, I00–I99) in central Bangkok, Thailand.
Methods
Data from hospital records were obtained from 3 major government hospitals. All hospital visits were stratified by age group and category of CVD. Daily PM10 and O3 levels reported by the Pollution Control Department from April 2002 to December 2006 (1736 days) were used in a time-series analysis with a generalized additive model procedure.
Results
Exposure on the previous day to PM10 and O3 had a positive association with hospital visits for CVD among elderly (≥65 years) individuals. The increase in CVD hospital visits in this age group was 0.10% (95% CI, 0.03–0.19) with a 10 µg/m3 increase in PM10, and 0.50% (95% CI, 0.19–0.81) with an increase in O3.
Conclusions
In central Bangkok, a short-term association was observed between increases in daily levels of PM10 and O3 and the number of daily emergency hospital visits for CVD, particularly among individuals aged ≥65 years.
Key words: PM10, ozone, cardiovascular diseases, hospital visits, Bangkok, air pollution
INTRODUCTION
In recent decades, epidemiologic studies conducted worldwide have shown that short- and long-term exposure to air pollutants, especially particulate matter, is associated with a consistently higher risk for respiratory and cardiovascular events, including heart attacks and stroke deaths.1–7 The Bangkok metropolitan area has a very high population density (4051 persons per km2) and 6.12 million registered motor vehicles. Problems related to traffic-related air pollution in Bangkok are becoming more frequent because of the limited number of transport routes and the rapidly increasing number of vehicles on the roads. High concentrations of particulate matter with a diameter of less than 10 µm (PM10) from automobile exhaust and a secondary pollutant, ozone (O3), may cause health problems. Bangkok air quality has been monitored by 32 Pollution Control Department (PCD) monitoring stations for several years. Between 2004 and 2006 the daily average PM10 and O3 concentrations in some areas were higher than the National Ambient Air Quality Standard. There have been many reports implicating PM10 and O3 as risk factors for heart disease.4–7 Kodavanti et al8 found an association between combustion particles and both reduced heart rate variability (HRV) and increased fibrinogen levels in rats. These relations have been confirmed in several human studies, which have shown that airborne particles are associated with increased plasma viscosity,9–11 decreased HRV,12–14 and the onset of myocardial infarction.7,9 Ozone, an oxidant gas, can cause respiratory tract damage that may induce pulmonary inflammation and edema10,15; it has also been found to have a direct bradycardiac effect in animal studies.16 Similar to PM10, exposure to O3 in humans has been associated with a decrease in HRV13 and an increase in the risk of hospitalization for heart disease.17
Cardiovascular disease (CVD) is the most common cause of morbidity and mortality in the developed world. Accumulating evidence shows that traffic-induced air pollution increases damage to the heart. However, the results of experimental studies of the mechanisms involved are inconclusive.18–21 There have been several reports worldwide on the short-term effects of air pollution and the increased risk of hospital admission or death from CVD22–26; however, almost all these epidemiologic studies have been performed in Europe24,26 and North America.1,2
In Thailand, PM10 was found to be associated with increased mortality in Bangkok.25 An association was also reported between air pollution and both chronic respiratory symptoms and impaired respiratory function among traffic policemen27,28 and their families.29,30 Thus, although previous studies have found a statistically significant relation between the chronic respiratory effects of ambient PM10 in Bangkok, little has been reported on the association with hospital visits for CVD after exposure to fluctuating PM10 and O3 concentrations. Such a study would provide further insight into the health effects of air pollution in a tropical developing country, where seasonal patterns of illness differ from those in Western countries. In the present study, we examined the associations between daily PM10 and O3 concentrations and daily hospital visits for CVD.
METHODS
Air quality and meteorological data
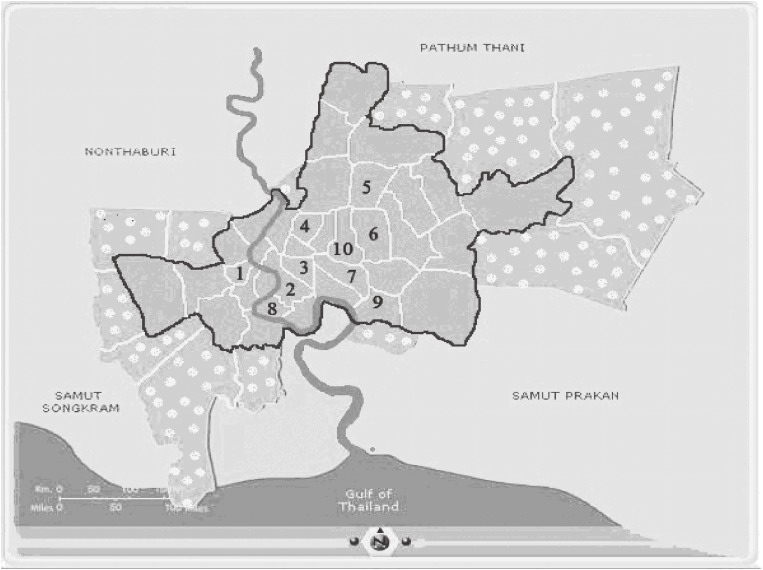
Air quality data in Bangkok were obtained from network monitoring stations of the Pollution Control Department.31 From 2002 to 2006, daily PM10 concentrations at site 4 (Figure 1) were measured by using a tapered element oscillating microbalance, and data from other sites were measured by using a beta-attenuation mass monitor. (www.aqnis.pcd.go.th/station/allstation.htm)
Figure 1. Map of Bangkok:
 Unstudied area;
Unstudied area;
 Studied area. Nos. 1–10 indicate the locations of the Pollution Control Department (PCD) ambient monitoring stations: (1) Thonburi Power Substation, Intrapitak Road; (2) 22 Odien Circle, Sampantawong; (3) Ministry of Science and Technology; (4) Dindaeng-National Housing Authority; (5) Chokchai 4 Police Box; (6) Land and Transport Department; (7) Chulalongkorn Hospital. (8) Rat-Burana Post Office; (9) Thai Meteorological Department, Bangna; and (10) Chandrakasem Rajabhat University; Jatujak (Stations 1–7 for PM10 and 1–10 for Ozone).
Studied area. Nos. 1–10 indicate the locations of the Pollution Control Department (PCD) ambient monitoring stations: (1) Thonburi Power Substation, Intrapitak Road; (2) 22 Odien Circle, Sampantawong; (3) Ministry of Science and Technology; (4) Dindaeng-National Housing Authority; (5) Chokchai 4 Police Box; (6) Land and Transport Department; (7) Chulalongkorn Hospital. (8) Rat-Burana Post Office; (9) Thai Meteorological Department, Bangna; and (10) Chandrakasem Rajabhat University; Jatujak (Stations 1–7 for PM10 and 1–10 for Ozone).
Ozone was measured by ultraviolet absorption photometry. We used the daily (24-hr) data for PM10 at 7 of 13 sites and the average daily (1-hr) O3 at 10 of 11 fixed ambient monitoring Pollution Control Department stations in central Bangkok (Figure 1); only stations with data for more than 75% of the entire study period were included in the analysis. Daily weather data from April 2002 and December 2006 were obtained from the Bangkok Meteorology Department. These data included daily average temperature, dew point, wind speed, and daily rainfall.
Hospital data
Data on hospital visits between 2000 and 2006 were collected using the records of first acute cardiovascular diseases from the 3 government hospitals in Bangkok ie, Ramathibodi, Siriraj, and Chulalongkorn hospitals to represent the population of central Bangkok. The Primary Care Unit System, which requires a fee of only 30 Thai baht (US$ 0.80) per visit for low-income patients, was launched in 2001.32 During the period of the introduction of this fee, in the beginning of 2002, there was an unusual fluctuation in the numbers of hospital visits; therefore, we excluded data from before April 2002. Daily counts of total hospital visits were aggregated by age, sex, patient address (zip code), date of hospital visit, and first diagnosis of CVD (ICD-10th code I00–I99).
Study subjects
Bangkok is divided into 50 districts, with a total registered population in 2007 of 6.6 million.33 In these 50 districts, the residential zip codes range from 10002 to 10800. The study subjects were selected from only the 25 innermost districts of Bangkok, where 2 693 292 residents live (Figure 1). The total number of hospital visits for CVD between April 2002 and December 2006 was 33 458. The study protocol was approved by the Institutional Review Board of the Faculty of Medicine; Chulalongkorn University reviewed the protocol based on the international guidelines for human research protection and ICH/GCP.
Statistical analysis
Time-series data on health outcome and air pollutants were analyzed for the period from 1 April 2002 to 31 December 2006. The Poisson regression model was applied, and the relative risk of a hospital visit was estimated with regression, after controlling for seasonal pattern, effect of the day of week, temperature, and dew point. This was done to control for factors beside air pollutants, which vary on a daily basis and might explain variations in daily hospital visits. We used the Loess smoothing technique to adjust for temperature and dew point. This is a flexible nonparametric modeling tool that can accommodate nonlinear and nonmonotonic patterns between time and health outcome. We also accounted for possible serial correlation in daily hospital visits by using a locally weighted smoothing function of the daily visit count over time.34 The smoothing parameters were selected by optimizing the generalized cross-validation criterion. Generalized additive models (GAM) were applied to identify predictor–response relationships among the many types of data, without using a specific model. GAM combine the ability to explore many nonparametric relationships simultaneously with the distributional flexibility of generalized linear models.35 Time-series analysis reduces the potential impact of confounding factors and other risk factors that do not vary significantly day-to-day. This model is suitable for exploring the short-term health effects of daily average levels of air pollutants.36,37 The dependent variable was the natural logarithm of the expected hospital visit count, and the regression coefficients were the natural logarithms of the rate ratio. The GAM was estimated as follows.
Where,
The associations between daily levels of pollutants and hospital visit variables (Tables 1, 2) were analyzed. Individual lag pollutant exposures on the concurrent day (lag 0), previous day (lag 1), and the 2-day and 3-day averages (lag 0+1 and lag 0+1+2, respectively) were examined. PM10 and O3 were fitted as linear terms. This statistical analysis provided a relative risk estimate for PM10 and O3 with a 95% confidence interval (CI).38,39 The relative risks of CVD subsets associated with a 10-µg/m3 increase in PM10 and O3 are presented as the percentage change in daily hospital visits.
Table 1. Daily average PM10 and O3 and related meteorological data for Bangkok from April 2002 to December 2006.
| Daily average variables | Mean | Minimum | Maximum |
| 24-hour PM10 (µg/m3) | 48.9 | 19.3 | 154.9 |
| Hourly O3 (ppb) | 14.4 | 3.2 | 41.9 |
| Dew point (°C) | 23.7 | 11.4 | 28.1 |
| Wind (km/h) | 4.1 | 0.0 | 12.1 |
| Temperature (°C) | 29.1 | 21.6 | 39.9 |
*National Ambient Air Quality Standards (NAAQS) of 0.10 ppm averaged over 1 hour and 0.07 ppm averaged over 8 hours.
Table 2. Descriptive data on hospital visits for cardiovascular diseases (I00–I99).
| Variables | Number of visits (cases) |
Mean number of visits (cases/day) |
Range of cases/day (min–max) |
| 1) All, I code (I00–I99) | 33 458 | 19 | 0–50 |
| 1.1) Age < 15 years | 681 | 1 | 0–4 |
| 1.2) Age 15–64 years | 16 710 | 10 | 0–25 |
| 1.3) Age ≥ 65 years | 16 067 | 10 | 0–23 |
| 2) Arrhythmia (I46–I49) | 1876 | 1 | 0–8 |
| 3) MI (I21) | 2566 | 2 | 0–8 |
| 4) IHD (I20–I25) | 10 158 | 6 | 0–19 |
MI, Myocardial Infarction; IHD, Ischemic Heart Disease
RESULTS
Air quality and meteorological data
The data for daily average PM10 and O3 concentrations for more than 75% of the entire study period were obtained from an average of 7 of 13 stations for PM10 and 10 of 11 stations for O3. The mean level (range) of daily PM10 and daily O3 (1-hr) was 48.9 µg/m3 (19.3–154.9 µg/m3) and 14.4 ppb (3.2–41.9 ppb), respectively. The daily weather data showed temperature seasonality: daily average temperatures were lower in November, December, and January. The mean (range) of daily temperature, dew point, and wind speed during the study period were 29.1 °C (21.6–39.9 °C), 23.7 °C (11.4–28.1 °C), and 4 km/h (0–12 km/h), respectively (Table 1). Normally, high summer temperatures occur during the period from February through May, and the rainy season is between May and October. These patterns and seasonal definitions are consistent with those specified by the Meteorology Department of Thailand.40
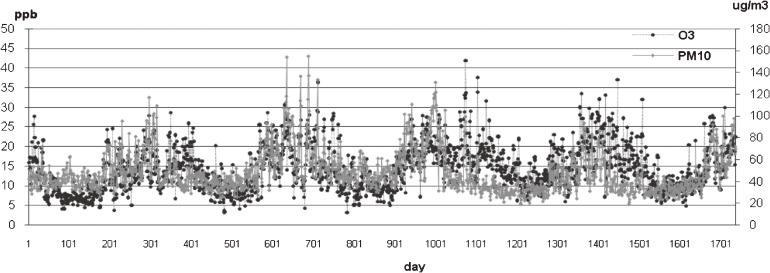
Ozone is a photochemical reaction product formed in heavy traffic areas. Production of this co-pollutant is related to many primary pollutants such as hydrocarbons, CO, and NOx. An urban environment with high levels of air pollutants can result in high O3 formation.41 Ambient daily O3 and PM10 profiles from 2002 to 2006 are shown in Figure 2. The colinearity between PM10 and O3 were significant in pairwise correlation tests (r2 = 0.25, P < 0.001). The ambient air quality data for 2005 showed that although PM10 decreased, O3 continued to increase, suggesting that sources other than PM10 influence O3 formation. However, there was a positive association between daily number of hospital visits and air pollution levels.
Figure 2. Daily averages of ambient air pollutants (O3 and PM10 levels) in central Bangkok, from 1 April 2002 to 31 December 2006. (Total number of days = 1736).
The association between PM10 and hospital visits for cardiovascular diseases
The descriptive data on hospital visits for CVD are summarized in Table 2. No significant association was found between PM10 exposure and total visits for CVD (or for arrhythmia, MI, or IHD), either on the concurrent day (lag 0) or the previous day (lag 1). However, after controlling for covariate factors, daily PM10 concentration was positively associated with hospital visits for CVD among elderly (≥65 years) individuals. Among this group, a 0.10% (95% CI, 0.03–0.19) increase in visits for CVD was associated with a 10-µg/m3 increase in PM10. The 2-day average PM10 concentration was associated with a 0.09% (95% CI, 0.00–0.20) increase in hospital visits for CVD among elderly patients for each 10-µg/m3 increase in PM10 (Table 3).
Table 3. Percentage change in daily hospital visits for cardiovascular diseases (CVD) by 10-µg/m3 increase in PM10 or O3 .
| Number of Patients (NPT) |
Day | PM10 | O3 | ||
| NPT change % |
95% CI | NPT change % |
95% CI | ||
| Total CVD; I00–I99 | Concurrent | 0.01 | −0.05 to 0.07 | −0.01 | −0.23 to 0.20 |
| 33 458 | Previous day | 0.05 | −0.01 to 0.11 | 0.23 | 0.02 to 0.44 |
| 2 Cumulative* | 0.03 | −0.03 to 0.10 | 0.17 | −0.06 to 0.40 | |
| 3 Cumulative† | 0.04 | −0.01 to 0.09 | 0.10 | −0.15 to 0.35 | |
| -age < 15 year | Concurrent | −0.27 | −0.76 to 0.19 | −0.49 | −2.05 to 1.07 |
| 681 | Previous day | −0.15 | −0.64 to 0.34 | −1.06 | −2.66 to 0.54 |
| 2 Cumulative | −0.24 | −0.76 to 0.28 | −1.00 | −2.80 to 0.80 | |
| 3 Cumulative | −0.09 | −0.63 to 0.44 | −0.82 | −2.74 to 1.10 | |
| -age 15–64 year | Concurrent | −0.02 | −0.12 to 0.07 | −0.16 | −0.47 to 0.15 |
| 16 710 | Previous day | 0.01 | −0.08 to 0.10 | 0.01 | −0.28 to 0.14 |
| 2 Cumulative | −0.01 | −0.10 to 0.09 | −0.08 | −0.43 to 0.26 | |
| 3 Cumulative | 0.00 | −0.09 to 0.10 | −0.10 | −0.47 to 0.27 | |
| -age ≥ 65 year | Concurrent | 0.06 | −0.03 to 0.16 | 0.15 | −0.16 to 0.46 |
| 16 067 | Previous day | 0.10 | 0.03 to 0.19 | 0.50 | 0.19 to 0.81 |
| 2 Cumulative | 0.09 | 0.00 to 0.20 | 0.48 | 0.13 to 0.83 | |
| 3 Cumulative | 0.08 | −0.01 to 0.18 | 0.36 | −0.01 to 0.73 | |
| Arrhythmia, I46–I49 | Concurrent | −0.01 | −0.30 to 0.29 | −0.26 | −1.24 to 0.72 |
| 1557 | Previous day | −0.08 | −0.37 to 0.21 | −0.06 | −1.00 to 0.88 |
| 2 Cumulative | −0.05 | −0.36 to 0.26 | −0.20 | −1.27 to 0.87 | |
| 3 Cumulative | −0.02 | −0.34 to 0.29 | −0.28 | −1.43 to 0.87 | |
| Myocardial Infarction | Concurrent | 0.12 | −0.11 to 0.36 | −0.30 | −1.08 to 0.48 |
| MI, I21 | Previous day | 0.00 | −0.24 to 0.24 | −0.68 | −1.48 to 0.12 |
| 2566 | 2 Cumulative | 0.06 | −0.18 to 0.32 | −0.68 | −1.58 to 0.22 |
| 3 Cumulative | −0.02 | −0.27 to 0.22 | −0.97 | −1.95 to 0.01 | |
| Ischemic Heart Disease | Concurrent | 0.02 | −0.10 to 0.14 | −0.30 | −0.69 to 0.09 |
| IHD, I20–I25 | Previous day | 0.07 | −0.04 to 0.19 | 0.27 | −0.12 to 0.66 |
| 10 158 | 2 Cumulative | 0.05 | −0.07 to 0.18 | 0.00 | −0.45 to 0.45 |
| 3 Cumulative | 0.09 | −0.01 to 0.20 | −0.08 | −0.57 to 0.41 | |
*2cumulative = (lag0 + lag1)/2
†3cumulative = (lag0 + lag1 + lag2)/3
The association between O3 and hospital visits for cardiovascular diseases
No association was found between ozone exposure and visits for total CVD (or for the arrhythmia, MI, or IHD) on the concurrent day (lag 0). However, after controlling for covariate factors, the total number of CVD visits increased by 0.23% (95% CI, 0.02–0.44) when the level of O3 was elevated on the previous day (lag 1). In addition, daily O3 concentration was positively associated with hospital visits for CVD among the elderly (≥65 years): a 0.50% (95% CI, 0.19–0.81) increase in hospital visits for CVD was associated with an increase in O3 during the previous day, and a 0.48% (95% CI, 0.13, 0.83) increase in hospital visits was associated with an elevation in the 2-day average O3 concentration (Table 3). We found no evidence of modifying effects on the results due to weather conditions.
DISCUSSION
A large number of epidemiologic studies support an association between air pollution and hospitalization for CVD; however, most of these were conducted in cold or temperate climates with distinct seasonality.1,2,6,22–24 Few studies have been conducted in tropical climates with little seasonality. This study conducted in Bangkok is unique in its use of diagnostic codes to categorize patients with CVD who might be at heightened risk for hospital admission after exposure to pollutants. This study used time-series data on the health effects of PM10 and O3 concentrations associated with hospital visits in central Bangkok. The results demonstrated that exposure during the previous day to PM10 and O3 was positively associated with hospital visits for CVD among elderly patients.
A 10-µg/m3 increase in PM10 during the previous day was associated with a 0.10% (95% CI, 0.03–0.19) increase in daily hospital visits for CVD among elderly patients. The same increase in the 2-day average was associated with a 0.09% (95% CI, 0.00–0.20) increase in hospital visits among the elderly. In addition, a 10-µg/m3 increase in O3 during the previous day (lag 1) was associated with a 0.23% (95% CI, 0.02–0.44) increase in the total number of CVD visits and, among the elderly, a 0.50% (95% CI, 0.19–0.81) increase in daily hospital visits for CVD was observed after an increase in O3 during the previous day. The 2-day average level of O3 was more strongly associated with hospital visits among the elderly than was concurrent-day exposure (0.48% [95% CI, 0.13–0.83] vs 0.15% [95% CI, −0.16–0.46]) (Table 3).
Daily NOx and CO concentrations in Bangkok during the period from 2002–2006 were obtained from PCD; these were far below levels believed to cause health effects and did not cause confounding.42 We also evaluated the effects of including NOx or CO in multivariate analysis to examine the relation between hospital visits and PM10. The changes in the percentage increase in hospital visits for each 10-µg/m3 increase in PM10 were small, which suggests that the possibility of confounding by NOx or CO was limited.43
The association between air pollution (PM10 and O3) and hospital visits for CVD in the elderly may be due to the fact that this group tends to be frail and may have pre-existing heart problems.44,45 The increase in hospital visits for CVD after a 10-µg/m3 increase in PM10 in elderly patients was lower than that found in cooler climates. Barnett et al45 studied 7 cities in Australia and New Zealand and reported a 1.1% (95% CI, 0.20–2.00) increase in hospital visits by the elderly after a 10-µg/m3 increase in PM10 and a 0.3% (95% CI, 0.10–1.00) increase in adult patients. A 2002 European Study (part of the Air Pollution and Health: A European Approach Project) examined the association between airborne particles and CVD hospital admissions (ICD 9th, 360–429), and found that the percentage increase in hospital admissions for a 10-µg/m3 increase in PM10 was 0.7% in the elderly (95% CI, 0.4–1.0).24 Unlike the majority of previous studies on air pollution and morbidity conducted in cities in the United States and Western Europe, which have relatively cold winters and strong seasonal patterns in daily morbidity, the present study was conducted in a tropical region and therefore excluded the effects of seasonal variation in climate. The replication in a tropical climate of findings obtained in cooler areas, albeit to a lesser extent, is noteworthy. In general, the level of air pollution and its effects on health are strongly associated with weather. In Japan, for example, mortality from CVD is 50% higher in the winter months than in the summer months.46 The results of the present study therefore show the net effect of air pollution, by excluding the effects of seasonality. However, human O3 exposure has been associated with a decrease in HRV,13 but there have been conflicting reports on O3 exposure and hospital admissions for CVD. Koken et al17 compared air pollution exposure with daily CVD hospital admissions among elderly people in Denver, Colorado in the United States. The results suggested that O3 is associated with an increased risk of hospitalization for acute myocardial infarction, coronary atherosclerosis, and pulmonary heart disease. The results show that there was no significant association between air pollution (PM10 and O3) and patients treated for the diagnostic subcodes for arrhythmia, MI, and IHD. This may be due to the limited number under subcodes for CVD. In fact IHD, which is the largest component of CVD, was weakly associated with PM10 exposure during the previous day.
Wong et al22 conducted parallel analyses of the short-term association between air pollution and daily hospital admissions in Hong Kong and London. The association between O3 and cardiac admissions was negative in London but positive in Hong Kong. In general, the effects of gaseous pollutants on CVD have not been systematically examined, and the mechanisms by which pollutants affect cardiovascular health continue to be a matter of speculation.
There were some limitations in the current study. First, although PM10 data were used in this time-series analysis, PM2.5 particulate matter with an aerodynamic diameter of less than 2.5 µm is more toxic and should therefore be analyzed in future studies. Second, we considered ambient environmental pollution rather than individual exposure levels in a cross-sectional study of a wide range of populations, which may have resulted in the omission of some extreme exposure incidents in our study. The use of ambient PM10 levels from PCD stations, rather than levels of personal exposure to PM10, may result in misclassification of exposure. This possible misclassification may not differentiate between those visiting hospitals and those not visiting, so that estimation of the association between air pollution and hospital visits may be biased toward null and thus underestimate the effects.38 Despite this possible bias, we nevertheless found effects due to exposure to PM10 and O3 and perhaps these would have been stronger had we been able to measure the actual individual exposure for each. Third, when looking at the acute health effects of air pollution using hospital visits, the availability and accessibility of health services often distort the real picture and this may have happened in the present study. However, in 2001, the Primary Care Unit System (with visits fixed at 30 Thai baht per hospital visit) was introduced in Thailand. This reduced the economic barrier to hospital treatment and allowed the number of hospital visits caused by air pollution to be assessed more directly. There may be still other limitations inherent to epidemiologic studies using government and hospital statistics; however, we believe that the present study showed a credible association between hospital visits for CVD and air pollution.
In conclusion, we found that PM10 and O3 were associated with cardiovascular diseases, particularly among elderly patients living in central Bangkok. There was a short-term association between increases in daily levels of air pollutants and the number of emergency hospital visits for CVD per day, particularly among individuals aged 65 years or older.
ACKNOWLEDGMENTS
This study was supported by the Royal Golden Jubilee (RGJ) PhD program, the Thai Research Fund, and the Graduate School, Chulalongkorn University. None of the authors have conflicts of interest of any kind. The authors are very grateful for support from several government authorities, the Ramathibodi, Siriraj, and Chulalongkorn hospitals, the Pollution Control Department, and the Bangkok Meteorology Department, for providing valuable information.
REFERENCES
- 1.Anderson HR , Bremner SA , Atkinson RW , Harrison RM , Walters S. Particulate matter and daily mortality and hospital admissions in the west midlands conurbation of the United Kingdom: associations with fine and coarse particles, black smoke and sulphate . Occup Environ Med. 2001;58:504–10 10.1136/oem.58.8.504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dominici F , Peng RD , Bell ML , Pham L , McDermott A , Zegar SL , et al. . Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. American Medical Association . JAMA. 2006;295:1127–34 10.1001/jama.295.10.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma L , Shima M , Yoda Y , Yamamoto H , Nakai S , Tamura K , et al. . Effects of airborne particulate matter on respiratory morbidity in asthmatic children . J Epidemiol. 2008;18:97–110 10.2188/jea.JE2007432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zareba W , Nomura A , Couderc JP. Cardiovascular effects of air pollution: What to measure in ECG? Environ Health Perspect. 2001;109:533–8 10.2307/3454665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zanobetti A , Schwartz J , Dockery DW. Airborne particles are a risk factor for hospital admissions for heart and lung disease . Environ Health Perspect. 2000;108:1071–7 10.2307/3434961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zanobetti A , Schwartz J. Air pollution and emergency admission in Boston, MA . J Epidemiol Community Health. 2006;60:890–5 10.1136/jech.2005.039834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zanobetti A , Schwartz J. The effect of particulate air pollution on emergency admission for myocardial infarction: a multi-city case-crossover analysis . Environ Health Perspect. 2005;113:978–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kodavanti UP , Moyer CF , Ledbetter AD , Schladweiler MC , Costa DL , Hauser R , et al. . Inhaled environmental combustion particles cause myocardial injury in the Wistar Kyoto Rat . Toxicol Sci. 2003;71:237–45 10.1093/toxsci/71.2.237 [DOI] [PubMed] [Google Scholar]
- 9.Peters A , Dockery DW , Muller JE , Mittleman MA. Increased particulate air pollution and the triggering of myocardial infarction . Circulation. 2001;103:2810–5 [DOI] [PubMed] [Google Scholar]
- 10.Bhatnagar A Cardiovascular pathophysiology of environmental pollutants . Am J Physiol Heart Circ Physiol. 2004;286:H479–85 10.1152/ajpheart.00817.2003 [DOI] [PubMed] [Google Scholar]
- 11.Bhatnagar A Environmental cardiology: Studying mechanistic links between pollution and heart disease . Circ Res. 2006;99:692–705 10.1161/01.RES.0000243586.99701.cf [DOI] [PubMed] [Google Scholar]
- 12.Pope CA III , Verrier RL , Lovett EG , Larson AC , Raizenne ME , Kanner RE , et al. . Heart rate variability associated with particulate air pollution . Am Heart J. 1999;138:890–9 10.1016/S0002-8703(99)70014-1 [DOI] [PubMed] [Google Scholar]
- 13.Gold DR , Litonjua A , Schwartz J , Lovett E , Larson A , Nearing B , et al. . Ambient Pollution and Heart Rate Variability . Circulation. 2000;101(11):1267–73 [DOI] [PubMed] [Google Scholar]
- 14.Magari SR , Hauser R , Schwartz J , Williams PL , Smith TJ , Christiani DC. Association of heart rate variability with occupational and environmental exposure to particulate air pollution . Circulation. 2001;104:986–91 10.1161/hc3401.095038 [DOI] [PubMed] [Google Scholar]
- 15.Chang LY , Huang Y , Stockstill BL , Graham JA , Grose EC , Menache MG , et al. . Epithelial injury and interstitial fibrosis in the proximal alveolar regions of rats chronically exposed to a simulated pattern of urban ambient ozone . Toxicol Appl Pharmacol. 1992;115:241–52 10.1016/0041-008X(92)90329-Q [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arito H , Uchiyama I , Arakawa H , Yokoyama E. Ozone-induced bradycardia and arrhythmia and their relation to sleep-wakefulness in rats . Toxicol Lett. 1990;52:169–78 10.1016/0378-4274(90)90151-B [DOI] [PubMed] [Google Scholar]
- 17.Koken PJ , Piver WT , Ye F , Elixhauser A , Olsen LM , Portier CJ. Temperature, air pollution, and hospitalization for cardiovascular diseases among elderly people in Denver . Environ Health Perspect. 2003;111:1312–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brook RD , Franklin B , Cascio W , Hong Y , Howard G , Lipsett M , et al. . Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association . Circulation. 2004;109:2655–71 10.1161/01.CIR.0000128587.30041.C8 [DOI] [PubMed] [Google Scholar]
- 19.Kunzli N , Tager IB. Air pollution: From Lung to Heart . Swiss Med Wkly. 2005;135:697–702 [DOI] [PubMed] [Google Scholar]
- 20.Tager IB , Lurmann F , Ngo L , Alcorn S , Kunzli N. Effect of chronic exposure to ambient ozone on lung function in young adults . Epidemiology. 2005;16:751–9 10.1097/01.ede.0000183166.68809.b0 [DOI] [PubMed] [Google Scholar]
- 21.Brook RD , Brook JR , Urch B , Vincent R , Rajagopalan S , Silver F. Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adult . Circulation. 2002;105:1534–6 10.1161/01.CIR.0000013838.94747.64 [DOI] [PubMed] [Google Scholar]
- 22.Wong CM , Atkinson RW , Anderson HR , Hedley AJ , Ma S , Chau PY , et al. . A tale of two cities: effects of air pollution on hospital admissions in Hong Kong and London compared . Environ Health Perspect. 2002;110(1):67–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piver WT , Ando M , Ye F , Portier CJ. Temperature and air pollution as risk factors for heart stroke in Tokyo, July and August 1980–1995 . Environ Health Perspect. 1999;107:911–6 10.2307/3454480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le Tertre A , Medina S , Samoli E , Forsberg B , Michelozzi P , Boumghar A , et al. . Short term effects of particulate air pollution on cardiovascular diseases in eight European cities . J Epidemiol Community Health. 2002;56:773–9 10.1136/jech.56.10.773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ostro B , Chestnut L , Vichit-Vadakan N , Laixuthai A. The impact of particulate matter on daily mortality in Bangkok, Thailand . J Air Waste Manage Assoc. 1999;49:100–7 [PubMed] [Google Scholar]
- 26.Ballester F , Rodríguez P , Iñíguez C , Saez M , Daponte A , Galán I , et al. . Air pollution and cardiovascular admissions association in Spain: results from the EMECAS project . J Epidemiol Community Health. 2006;60:328–36 10.1136/jech.2005.037978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karita K , Yano E , Jinsart W , Boudoung D , Tamura K. Respiratory symptoms and pulmonary function among traffic policemen in Bangkok . Arch Environ Health. 2001;56(5):467–70 [DOI] [PubMed] [Google Scholar]
- 28.Jinsart W , Tamura K , Loetkamonwit S , Thepanondh S , Karita K , Yano E. Roadside particulate air pollution in Bangkok . J Air Waste Manage Assoc. 2002;52:1102–10 [DOI] [PubMed] [Google Scholar]
- 29.Karita K , Yano E , Tamura K , Jinsart W. Effect of working and residential location areas on air pollution-related respiratory symptoms in policemen and their wives in Bangkok, Thailand . Eur J Public Health. 2004;14(1):24–6 10.1093/eurpub/14.1.24 [DOI] [PubMed] [Google Scholar]
- 30.Langkulsen U , Jinsart W , Karita K , Yano E. Respiratory symptoms and lung function in Bangkok school children . Eur J Public Health. 2006;16(6):676–81 10.1093/eurpub/ckl061 [DOI] [PubMed] [Google Scholar]
- 31.State of Thailand Pollution Report 2006. Pollution Control Department (PCD) Bangkok, Thailand 2007.
- 32.Pongsupap Y , Boonyapaisarncharoen T , Lerberghe WV. The perception of patients using Primary Care Units in comparison with conventional Public Hospital outpatient departments and “Prime Mover Family Practices”: An Exit Survey . J Health Sci. 2005;14:475–83 [Google Scholar]
- 33.Bangkok Metropolitan Administration Thailand 2007.
- 34.Hastie T, Tibshirani R. Generalized Additive Model; Chapman and Hall; London, 1990. [Google Scholar]
- 35.Dominici F , McDermott A , Zeger SL , Samet JM. On the use of the generalized additive model in time-series studies of air pollution and health . Am J Epidemiol. 2002;156:193–203 10.1093/aje/kwf062 [DOI] [PubMed] [Google Scholar]
- 36.Bowerman BL, O’Connell RT, Koehler AB. Forecasting, Time Series and Regression. Thomson Books/Cole.USA: 2005;279–400. [Google Scholar]
- 37.Wood SN, Augustin HN. GAMs with integrated model selection using penalized regression splines and applications to environmental modeling. Ecological Modeling 2002; 157–177. [Google Scholar]
- 38.Aschengrau A, Seage GR III. Essentials of Epidemiology in Public Health. Jones and Bartlett Publishers Inc, Boston 2008; 310–321. [Google Scholar]
- 39.Martins LC , Pereira LA , Lin CA , Santos UP , Prioli G , do Carmo Luiz O , et al. . The effects of air pollution on cardiovascular diseases: lag structures . Rev Saude Publica. 2006;40(4):677–83 [DOI] [PubMed] [Google Scholar]
- 40.Meteorology Department Bangkok , Thailand, 2007 [Google Scholar]
- 41.Colls J. Air Pollution: Gaseous air pollution: source and control. Spon Press 2002; 47–56. [Google Scholar]
- 42.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology 3rd edition Walters Kluwer/Lippincott Williams & Wilkins Philadelphia. 2008; p. 132. [Google Scholar]
- 43.Rothman KJ. Epidemiology An Introduction. Oxford University Press, Oxford 2002; p. 164. [Google Scholar]
- 44.Cowie MR , Wood DA , Coats AJ , Thompson SG , Poole-Wilson PA , Suresh V , et al. . Incidence and aetiology of heart failure: a population-based study . Eur Heart J. 1999;20:421–8 10.1053/euhj.1998.1280 [DOI] [PubMed] [Google Scholar]
- 45.Barnett AG , Williams GM , Schwartz J , Best TL , Neller AH , Petroeschevsky AL , et al. . The effects of air pollution on hospitalizations for cardiovascular disease in elderly people in Australian and New Zealand cities . Environ Health Perspect. 2006;114:1018–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Statistics and Information Department Minister’s Secretariat. Ministry of Health, Labour and Welfare. Vital Statistics of Japan 2006. Vol. 3 p 402–403. Health and Welfare Statistics Association. Tokyo 2008. [Google Scholar]