Abstract
Background
Fractures of acrylic resin dentures are a common occurrence in clinical dentistry. The denture may be fractured accidentally when dropped or while in service in the mouth due to flexural fatigue.
Objectives
The aim of this study was to compare the elastic modulus and the flexural strength between two heat-cured acrylic resins used in denture bases: a high-impact resin (Lucitone 199) and a traditional resin (Rodex).
Materials and methods
Rectangular strips of Lucitone 199 and Rodex (10 samples each) were fabricated and stored in artificial saliva at 37 °C for 2 weeks. The specimens were subjected to a three-point flexural test. The data were statistically analysed with Student’s t-test (p ⩽ .05).
Results
The high-impact acrylic resin had a lower elastic modulus (p = .000) and higher flexural strength (p = .001) compared to the traditional acrylic resin.
Conclusion
Within the limitations of this study, it can be concluded that the high-impact acrylic resin is a suitable denture base material for patients with clinical fracture of the acrylic denture.
Keywords: Denture, Acrylic resin, Fracture, High-impact, Elastic modulus, Flexural strength
1. Introduction
Polymethyl methacrylate (PMMA) resins are commonly used for the fabrication of denture bases, owing to their good aesthetics, simple processing, and relative ease of repair (Cheng et al., 2010; Hirajima et al., 2009). However, insufficient mechanical properties render them non-ideal (Seo et al., 2006). In particular, acrylic resin dentures are prone to fracture, which may occur by impact when the denture is outside the mouth, or while in service in the mouth due to flexural fatigue as the denture base undergoes repeated masticatory loading (Johnston et al., 1981; Hirajima et al., 2009; Kelly, 1969).
High flexural strength is crucial to the success of denture wearing, as alveolar absorption is a gradual and irregular process that causes uneven prosthesis support (Diaz-Arnold et al., 2008). To ensure that the stresses encountered during biting and mastication do not cause permanent deformation, the denture base material should exhibit a high elastic modulus (McCabe and Walls, 1998). Meng and Latta (2005) determined the Izod impact strength, flexural strength, flexural modulus, and yield distance for four denture resins (i.e., Lucitone 199, Fricke Hi-I, ProBase Hot, and Sledgehammer Maxipack). Among the tested resins, Lucitone 199 demonstrated the highest impact strength, flexural strength, and yield distance (p < .05). Moreover, the flexural modulus had an inverse relationship with the impact strength, flexural strength, and yield distance.
Diaz-Arnold et al. (2008) evaluated the flexural strength of four PMMA acrylic resin materials (i.e., Diamond D, Fricke HI-I, Lucitone 199, Nature-Cryl Hi-Plus) and one urethane dimethacrylate material (i.e., Eclipse). The visible light-polymerized Eclipse resin demonstrated a greater flexural strength than all of the PMMA heat-polymerized resins.
Few studies have evaluated the stiffness and flexural strength of high-impact resin. Therefore, the purpose of this paper was to evaluate the elastic modulus and flexural strength of two heat-cured denture base acrylic resins: specifically, a high-impact resin (Lucitone 199) and a traditional resin (Rodex).
2. Materials and methods
Twenty strip patterns (3 × 10 × 60 mm) were made of dental modelling wax (Tenatex Red, Kemdent, UK). Moulds were made by placing the wax patterns in a metal flask with a dental stone (Bego, Germany). The lower half of the flask was filled with mixed dental stone, a glass slab was placed on the surface, and the dental stone was allowed to set. Four wax patterns were placed on the glass slab and fastened with an adhesive. The stone surface was painted with a separating medium (Die Bub, JIM Neg Col. Bloomfield, CT, USA). The upper half of the flask was placed over the lower half, filled with mixed dental stone, and allowed to set. The halves of the flask were separated, the wax patterns were removed, and the stone surface was painted with separating medium.
The high-impact acrylic resin Lucitone 199 (Dentsply International Inc., Degu Dent GmbH, Hanau, Germany) and the traditional acrylic resin Rodex (SPD, Italy) were mixed according to the manufacturers’ instructions and packed during the dough stage into the moulds. The halves of the flask were clamped. The recommended polymerization cycles were followed for each material. Each material was cured by placing the flask in a water bath at 72 °C for 1 h, followed by 100 °C for 30 min. The flask was left in the water overnight before removal. Specimens were finished with 320-grit sandpaper (Rados, Morocco) and a tungsten carbide bur (Strong 204, Microtower, Korea) at 4000 rpm, and stored in artificial saliva at 37 °C for 2 weeks.
The specimens were subjected to the three-point flexural strength test (Fig. 1). Force was applied by a Testometric M350-5CT (Rochdale, England) (Fig. 2) with Win Test software and a 500-kg load cell at a crosshead speed of 5 mm/min. The span length was 46 mm. The flexural strength (FS, in MPa) was calculated by FS = 3PL/2 bd2, where P is the maximum load (N), L is the span length (m), b is the specimen width (m), and d is the specimen thickness (m) (Anusavice and Phillips, 2003). The elastic modulus (E, in MPa) was calculated by E = (P/db)/ (Δl/l), where Δl is the increase in specimen length (m) (Anusavice and Phillips, 2003).
Figure 1.
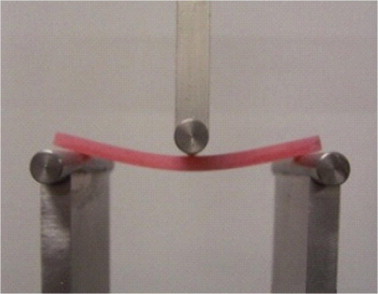
Strip resin specimen during 3-point flexure test.
Figure 2.
The testing machine (Testometric).
The Ethics Committee of the Dental Medicine Faculty of Damascus University approved the research protocol. The data were statistically analysed using Student’s t-test. A level of statistical significance of 0.05 was assumed. The statistical software SPSS version 13.0 was used for data analysis.
3. Results
Table 1 presents the descriptive statistics of the elastic modulus and flexural strength for Lucitone 199 and Rodex. The high-impact resin material (Lucitone 199) exhibited a lower mean elastic modulus and a higher mean flexural strength compared to the traditional resin material (Rodex) (p = .000 and .001, respectively, by Student’s t-test; Table 2).
Table 1.
Mean, standard deviation, minimum and maximum values of elastic modulus (MPa) and flexural strength (MPa) for the two types of acrylic resins.
| Material | N | Studied variable | Mean | Std. deviation | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Lucitone 199 | 10 | Elastic modulus | 1229.68 | 38.82 | 1177.4 | 1304.9 |
| Flexural strength | 82.43 | 6.85 | 66.937 | 89.027 | ||
| Rodex | 10 | Elastic modulus | 1602.68 | 37.18 | 1530.9 | 1667.2 |
| Flexural strength | 69.77 | 7.31 | 58.924 | 82.792 |
Table 2.
Independent sample T-test results.
| Studied variable | t-Value | df | Mean difference | Std. error difference | P-value |
|---|---|---|---|---|---|
| Elastic modulus (Mpa) | 21.944 | 18 | 373.00 | 17.00 | 0.000⁎ |
| Flexure strength (Mpa) | 3.996 | 18 | 12.66 | 3.17 | 0.001⁎ |
The mean difference is significant (P < .05).
4. Discussion
A denture base material with a high elastic modulus can withstand permanent mastication-induced deformation. Fracture of the upper dentures invariably occurs through the midline of the denture, due to flexure. Therefore, the denture base should have sufficient flexural strength to resist fracture (McCabe and Walls, 1998). This study compared the elastic modulus and flexural strength between high-impact and traditional denture base acrylic resins. The experimental circumstances were similar to those of the clinical situation. Specimens were 60 mm in length, similar to the width of the upper denture between the two molars (Stafford et al., 1982), and the specimen thickness (3 mm) was similar to that of the denture.
After immersion in artificial saliva at 37 °C for 2 weeks, the mean elastic modulus of the high-impact resin (Lucitone 199, 1229.68 MPa) was significantly lower than that of the traditional resin (Rodex, 1602.68 MPa). The elastic modulus reflects the stiffness of a material (Craig et al., 2004). Therefore, the high-impact resin exhibited less stiffness than the traditional resin. O’Brien (1997) mentioned that the inclusion of rubber in the high-impact resin improved the impact strength but reduced the stiffness, which might help explain the lower elastic modulus of the high-impact resin. This result is in agreement with Meng and Latta (2005), who found that Lucitone 199 exhibited the lowest elastic modulus when compared to two traditional resins (ProBase Hot, Sledgehammer Maxipack).
The mean flexural strength of the high-impact resin (Lucitone 199, 82.43 MPa) was significantly higher than that of the traditional resin (Rodex, 69.77 MPa). During the three-point flexure test, compressive stresses were generated at the middle of the upper surface of the tested strip, whereas tension stresses were generated at the lower surface (Manappallil, 2003). Fracture of the strips occurred due to the gradual propagation of small cracks at the sites of tension on the lower surface (Kaine et al., 2000). According to O’Brien (1997), the inclusion of rubber in high-impact resin had a craze-inhibiting effect, which could explain the increased flexural strength of Lucitone 199.
Diaz-Arnold et al. (2008) and Meng and Latta (2005) reported mean values for the flexural strength of Lucitone 199 of 83.97 and 99.5 MPa, respectively. The flexural strength is related to the distance between the two supporting bars, test speed, and dimensions (width and thickness) of the tested strip (Anusavice and Phillips, 2003). These aspects differed in the present study compared to previous studies, which might explain the difference in the flexural strength values among the different studies. Meng and Latta (2005) found that the flexural strength of high-impact Lucitone 199 was higher than those of two traditional resins (ProBase Hot, Sledgehammer Maxipack). However, Diaz-Arnold et al. (2008) found no significant difference between the flexural strength of Lucitone 199 compared to three heat-cured acrylic resins (Diamond D, Fricke HI-I, Nature-Cryl Hi-Plus).
5. Conclusion
The high-impact acrylic resin (Lucitone 199) exhibited less stiffness and, therefore, greater deformation compared to the traditional acrylic resin (Rodex). The high-impact resin also showed greater flexural/fracture strength than the traditional acrylic resin. Within the limitations of this study, it can be concluded that the high-impact acrylic resin is a suitable denture base material for patients who are suffering from clinical fracture of the acrylic denture.
Conflict of interest
The current research is free of conflict of interest.
Acknowledgment
The authors would like to thank Damascus University for the financial support of the study.
Footnotes
Peer review under responsibility of King Saud University.
Appendix A.
See Tables 1 and 2.
References
- Anusavice K.J., Phillips R.W. 11th ed. WB Saunders; St. Louis: 2003. Phillips’ Science of Dental Materials. pp. 83–89. [Google Scholar]
- Cheng Y.Y., Cheung W.L., Chow T.W. Strain analysis of maxillary complete denture with three-dimensional finite element method. J. Prosthet. Dent. 2010;103:309–318. doi: 10.1016/S0022-3913(10)60064-9. [DOI] [PubMed] [Google Scholar]
- Craig R.G., Powers J.M., Wataha J.C. 8th ed. Mosby; St. Louis: 2004. Dental Materials, Properties and Manipulation. p. 24. [Google Scholar]
- Diaz-Arnold A.M., Varags M.A., Shaull R.L., Laffoon J.E., Oian F. Flexural and fatigue strengths of denture base resin. J. Prothet. Dent. 2008;100:47–51. doi: 10.1016/S0022-3913(08)60136-5. [DOI] [PubMed] [Google Scholar]
- Hirajima Y., Takahashi H., Minakuchi S. Influence of a denture strengthener on the deformation of a maxillary complete denture. Dent. Mater. 2009;28:507–512. doi: 10.4012/dmj.28.507. [DOI] [PubMed] [Google Scholar]
- Johnston E.P., Nicholls J.I., Smith D.E. Flexure fatigue of 10 commonly used denture base resins. J. Prosthet. Dent. 1981;46:478–483. doi: 10.1016/0022-3913(81)90232-8. [DOI] [PubMed] [Google Scholar]
- Kaine T., Fujii K., Arikawa H., Inoue K. Flexural properties and impact strength of denture base polymer reinforced with woven glass fiber. Dent. Mater. 2000;16:150–158. doi: 10.1016/s0109-5641(99)00097-4. [DOI] [PubMed] [Google Scholar]
- Kelly E. Fatigue failure in denture base polymers. J. Prosthet. Dent. 1969;21:257–266. doi: 10.1016/0022-3913(69)90289-3. [DOI] [PubMed] [Google Scholar]
- Manappallil J.J. second ed. Jaypee Brother Medical Publishers; New Delhi: 2003. Basic Dental Materials. p. 16. [Google Scholar]
- McCabe J.F., Walls A.W.G. 8th ed. Blackwell Science; Oxford: 1998. Applied Dental Materials. p. 97. [Google Scholar]
- Meng T.R., Latta M.A. Physical properties of four acrylic denture base resins. J. Contemp. Dent. Pract. 2005;6:93–100. [PubMed] [Google Scholar]
- O’Brien W.J. Second ed. Quintessence Publishing Co., Inc.; 1997. Dental Materials and Their Selection. pp. 86–94. [Google Scholar]
- Seo R.S., Murata H., Hong G., Vergani C.E., Hamada T. Influence of thermal and mechanical stresses on the strength of intact and relined denture bases. J. Prosthet. Dent. 2006;96:59–67. doi: 10.1016/j.prosdent.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Stafford G.D., Lewis T.T., Huggett R. Fatigue testing of denture base polymers. J. Oral. Rehabil. 1982;9:139–154. doi: 10.1111/j.1365-2842.1982.tb00544.x. [DOI] [PubMed] [Google Scholar]



