CASE REPORTS
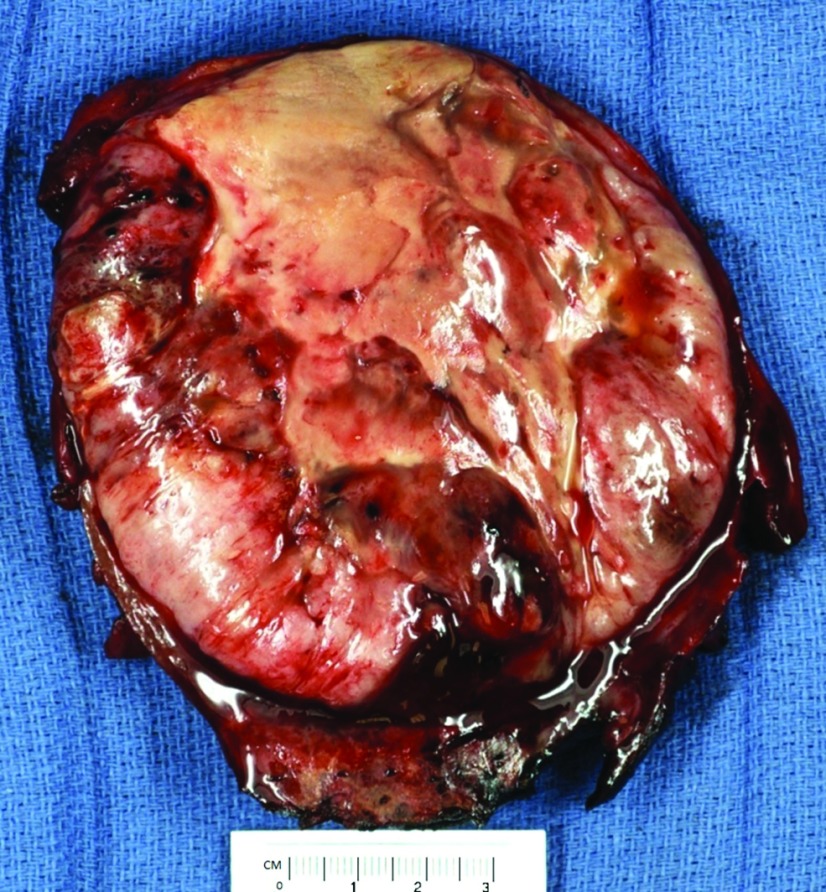
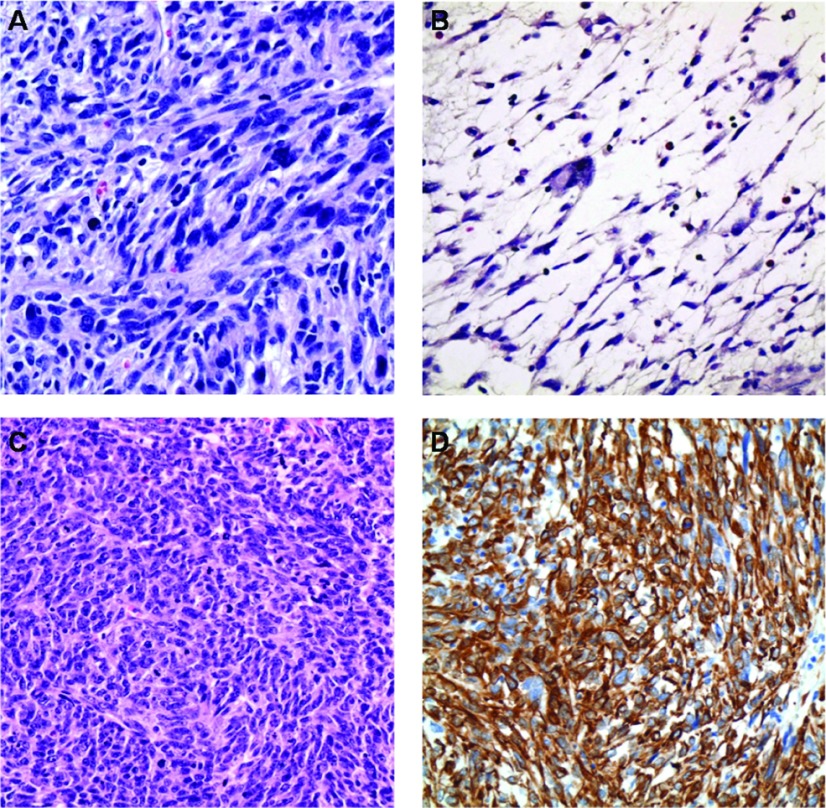
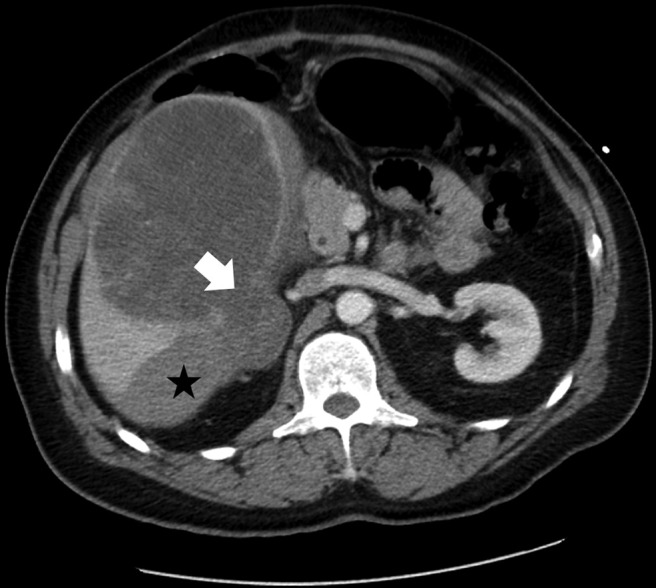
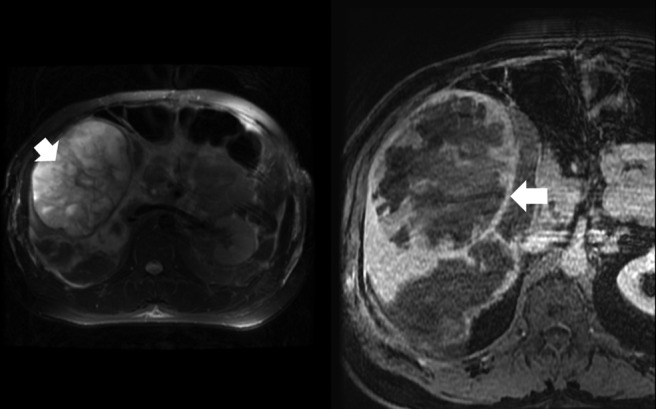
A 42-year-old man presented to the emergency room with right upper quadrant abdominal pain and nausea. An abdominal examination revealed right upper quadrant tenderness and hepatomegaly without peritoneal signs. A contrast-enhanced computed tomographic (CECT) scan of the abdomen showed a 13.7 × 11.4 × 11.8-cm, well-circumscribed, heterogeneously dense mass in the right lobe of the liver. The posterior margin of this mass was interrupted, with evidence of subcapsular hemorrhage (Figure 1). A small volume of free intraperitoneal hemorrhage was also noted. Gadolinium-enhanced magnetic resonance imaging (MRI) showed a centrally increased T1 signal consistent with internal hemorrhage within the mass and a T2 hypointense rim compatible with a capsule or pseudocapsule (Figure 2). No retroperitoneal lymphadenopathy was identified, and the hepatic artery, portal vein, and hepatic veins were patent. Soon after presentation, the patient underwent a segment V hepatectomy with adhesiolysis and evacuation of the hematoma. Gross pathology revealed a firm, gray-white mass measuring 20 × 11 × 10 cm, with areas of necrosis and hemorrhage (Figure 3). Microscopic sections revealed areas of fascicular growth (Figure 4A) in a highly pleomorphic neoplasm with high mitotic count (Figure 4B) and abundant necrosis with focal storiform and myxoid areas (Figure 4C), suggestive of leiomyosarcoma (LMS). Myoid differentiation was supported by strong, diffuse desmin positivity (Figure 4D). The tumor cells were negative for smooth muscle actin (SMA), S-100, DOG-1, CD 117, and epithelial membrane antigen (EMA). The patient had an uneventful postoperative recovery, and 3 months after surgery, there was no tumor recurrence.
Figure 1.
CECT scan of the abdomen showing a heterogeneous mass in the right lobe of the liver with interruption of the posterior margin (arrow) and a subcapsular hemorrhage (star).
Figure 2.
A gadolinium-enhanced MRI of the liver showing (left) a centrally increased T1 signal consistent with an internal hemorrhage (arrow) and (right) a T2 hypointense rim compatible with a capsule or pseudocapsule (arrow).
Figure 3.
A gross cross section of the segment V hepatectomy specimen showing a circumscribed, firm tumor mass with areas of necrosis, myxoid degeneration, and hemorrhage.
Figure 4.
Histopathologic images demonstrating (A) a pleomorphic tumor with fascicular growth pattern suggestive of LMS (×100), (B) high-grade pleomorphic cells with increased mitotic activity (×400), (C) an area of focal myxoid changes (×400), and (D) desmin immunohistochemical staining demonstrating diffuse positivity (3+) (×400).
DISCUSSION
Sarcomas are malignant tumors of mesenchymal origin. Hepatic sarcomas constitute less than 2% of primary liver cancers.1 Primary hepatic LMS is a rare tumor, accounting for less than 10% of all hepatic sarcomas, and tumor bleeding is very uncommon.2 Primary hepatic LMS is an indolent tumor, often attaining a large size without producing symptoms. At diagnosis, the mean tumor size is 14.5 ± 7.1 cm. Despite the large size of the primary tumor, metastatic disease is evident in less than 50% of patients.3 Chi et al,3 in their systematic review, reported bleeding as a clinical manifestation in less than 10% of cases, without any mention of tumor rupture. Although tumor rupture with intraperitoneal bleeding is a known complication of hepatocellular cancer, it is uncommon in hepatic LMS. To the best of our knowledge, this is the first reported case of primary hepatic LMS to present with tumor rupture as the initial manifestation.
Unlike in hepatocellular cancer, imaging and serologic markers are rarely helpful in establishing the diagnosis.3 LMS is exclusively a pathologic diagnosis. However, samples obtained from necrotic areas may yield false-negative results. Exploratory laparotomy with frozen-section biopsies is often an appropriate diagnostic strategy in these patients and allows for staging and therapeutic resection, if indicated. Surgical resection of the primary tumor with a tumor-free margin (R0 resection) offers the best outcome.1,3 A positive tumor margin after resection is associated with a significantly shorter overall survival (hazard ratio = 9.43; p = .0004).3 The role of debulking surgery in patients with multifocal or metastatic disease is poorly defined and the utility of adjuvant chemotherapy and radiation is uncertain.1,4 Liver transplant has been attempted with variable outcomes, and current experience precludes its use outside clinical research settings.4
Primary hepatic LMS is a rare tumor that should be considered in the differential diagnosis of a hepatic mass, especially in the absence of imaging features suggestive of hepatocellular cancer. The option of surgical exploration should be offered to all patients unless there are obvious criteria of irresectability or other comorbid medical conditions that would preclude hepatic resection.
Footnotes
Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
REFERENCES
- 1. Matthaei H, Krieg A, Schmelzle M, et al. : Long-term survival after surgery for primary hepatic sarcoma in adults. Arch Surg 144:339–344, 2009 [DOI] [PubMed] [Google Scholar]
- 2. Weitz J, Klimstra DS, Cymes K, et al. : Management of primary liver sarcomas. Cancer 109:1391–1396, 2007 [DOI] [PubMed] [Google Scholar]
- 3. Chi M, Dudek AZ, Wind KP: Primary hepatic leiomyosarcoma in adults: analysis of prognostic factors. Onkologie 35:210–214, 2012 [DOI] [PubMed] [Google Scholar]
- 4. Shivathirthan N, Kita J, Iso Y, et al. : Primary hepatic leiomyosarcoma: case report and literature review. World J Gastrointest Oncol 3:148–152, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]