Abstract
Objective
To investigate the ability of 28 blind subjects implanted with a 60-electrode Argus II (Second Sight Medical Products Inc) retinal prosthesis system to detect the direction of a moving object.
Methods
Blind subjects (bare light perception or worse in both eyes) with retinitis pigmentosa were implanted with the Argus II prosthesis as part of a phase 1/2 feasibility study at multiple clinical sites worldwide. The experiment measured their ability to detect the direction of motion of a high-contrast moving bar on a flatscreen monitor in 3 conditions: with the prosthesis system on and a 1-to-1 mapping of spatial information, with the system off, and with the system on but with randomly scrambled spatial information.
Results
Fifteen subjects (54%) were able to perform the task significantly better with their prosthesis system than they were with their residual vision, 2 subjects had significantly better performance with their residual vision, and no difference was found for 11 subjects. Of the 15 better-performing subjects, 11 were available for follow-up testing, and 10 of them had significantly better performance with normal rather than with scrambled spatial information.
Conclusions
This work demonstrates that blind subjects implanted with the Argus II retinal prosthesis were able to perform a motion detection task they could not do with their native vision, confirming that electrical stimulation of the retina provides spatial information from synchronized activation of multiple electrodes.
The feasibility of using a retinal prosthesis to restore partial (useful) sight to people blinded by outer retinal degenerative diseases is being investigated by several research groups worldwide.1-3 Diseases such as retinitis pigmentosa and age-related macular degeneration destroy photoreceptors but leave a significant percentage of inner retinal cells (ganglion and bipolar cells) intact and functional.4 Direct electrical stimulation of these remaining inner retinal cells via an implanted array of electrodes provides some rudimentary vision to patients who have these diseases. Despite extensive investigation of retinal prostheses by multiple groups, to our knowledge, it has proven difficult to use the individual stimulating electrodes to produce the perception of spatial patterns.
The Argus II retinal prosthesis system (Second Sight Medical Products Inc) consists of an array of 60 independently controlled electrodes implanted epiretinally, an inductive coil to wirelessly relay data and power to extraocular driver circuitry, an external video processing unit, and a miniature video camera mounted on a pair of glasses. The camera acquires a video signal; in real time, the video processing unit digitizes the image, applies image-processing filters, and down samples the resolution to a 6 × 10 grid. The 60-pixel image is mapped to stimulation amplitudes on the corresponding electrodes using look-up tables that have been customized for each subject's local sensitivity to electrical stimulation.
Here, we investigated the performance of subjects implanted with an Argus II retinal prosthesis on a task that requires spatialvision—identifying the direction of motion of a high-contrast bar moving across a computer monitor.
METHODS
SUBJECTS
Thirty blind subjects (bare light perception or worse in both eyes) with retinitis pigmentosa were implanted with the Argus II prosthesis as part of a phase 1/2 feasibility study (clinicaltrials.gov identifier: NCT00407602; active, not recruiting) at multiple clinical sites worldwide. The study was approved by institutional review boards and ethics committees at each site and respected the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects.
Subjects’ (monocular) residual vision was assessed before implantation; for inclusion in the clinical trial, subjects were required to have visual acuity worse than 2.9 logMAR (Snellen, 20/15887) in both eyes as measured by a custom-developed 4-alternative forced-choice square wave grating acuity test. They were also required to have bare light perception in at least 1 eye (ensuring that the optic nerve was functional) as measured by a full-field stimulus threshold test (comparable to those used in similar studies5) or a photographic flash test.
The experiments described in this article were run on all Argus II subjects who were available for regular testing, a total of 28 as of July 30, 2010. All subjects had been implanted at least 6 months and were fitted and trained with the device. Of the remaining 2 subjects enrolled in the trial, 1 was explanted before this study commenced owing to recurrent conjunctival erosion, and 1 was unavailable for this test during the study period owing to the site's institutional review board not having approved the test at that time. Table 1 lists the subjects included in the study along with some demographic factors including the number of months postsurgery as of July 30, 2010.
Table 1.
Subject Demographics and Experiment Factors
| Subject No. | Eye Implanted | Sex | Age at Implant,y | Duration of Blindness (self-report), y | Time Postimplant, mo | Bar Speed, degrees/s |
|---|---|---|---|---|---|---|
| 11-001 | OD | Woman | 55 | 26 | 38.3 | 31.6 |
| 11-002 | OD | Woman | 61 | 21 | 36.9 | 31.6 |
| 12-001 | OD | Man | 52 | 23 | 37.6 | 31.6 |
| 12-002 | OD | Woman | 60 | 38.0 | 31.6 | |
| 12-003 | OD | Man | 75 | 36 | 38.0 | 31.6 |
| 12-004 | OD | Man | 52 | 23 | 37.6 | 31.6 |
| 12-005 | OD | Man | 70 | 13.2 | 31.6 | |
| 13-001 | OS | Man | 49 | 13.2 | 15.8 | |
| 13-002 | OS | Woman | 52 | 12.7 | 31.6 | |
| 14-001 | OS | Woman | 56 | 13.3 | 31.6 | |
| 15-001 | OD | Man | 58 | 38 | 35.0 | 7.9 |
| 15-003 | OD | Woman | 77 | 58 | 28.2 | 7.9 |
| 17-002 | OD | Man | 66 | 62 | 37.2 | 31.6 |
| 51-001 | OD | Man | 70 | 61 | 27.9 | 31.6 |
| 51-002 | OD | Man | 51 | 21 | 27.9 | 31.6 |
| 51-003 | OD | Man | 72 | 52 | 26.2 | 31.6 |
| 51-005 | OD | Man | 55 | 36 | 16.4 | 31.6 |
| 51-006 | OD | Man | 60 | 51 | 15.5 | 31.6 |
| 51-007 | OD | Man | 62 | 25 | 13.6 | 31.6 |
| 51-009 | OD | Woman | 45 | 15 | 11.8 | 31.6 |
| 52-001 | OD | Man | 50 | 23 | 14.1 | 31.6 |
| 52-002 | OD | Man | 65 | 46 | 14.5 | 31.6 |
| 52-003 | OD | Man | 60 | 30 | 12.0 | 31.6 |
| 61-001 | OD | Man | 52 | 23 | 29.9 | 31.6 |
| 61-003 | OD | Man | 57 | 28 | 18.5 | 31.6 |
| 61-004 | OD | Man | 59 | 21 | 16.4 | 7.9 |
| 61-005 | OD | Man | 49 | 32 | 14.3 | 31.6 |
| 71-003 | OS | Woman | 27 | 23 | 17.1 | 31.6 |
Abbreviations: OD, right eye; OS, left eye.
THE ARGUS II SYSTEM
The Argus II system, shown in Figure 1, is an epiretinal prosthesis that was fully implanted on and in the eye, with an external unit worn by the subject (Figure 1A). The implanted portion consisted of a receiving and transmitting coil and electronics case (which were fixed to the sclera outside of the eye) and an electrode array that was surgically positioned onto the surface of the retina, fixed by a retinal tack, and connected to the electronics case by a transscleral ribbon cable (Figure 1B). Surgeons were instructed to place the array centered over the macula. Each of the 60 electrodes (in a 6 × 10 grid) were 200 μm in diameter and were made of platinum gray, a high surface-area platinum developed by Second Sight Medical Products (US Patent no. 6 974 533). The array (along the diagonal) covered an area of retina corresponding to about 20° in visual angle, assuming 293 μm on the retina equates to 1° of visual angle.6
Figure 1.
The Argus II system. A, The external parts of the Argus II system including glasses and the video processing unit (VPU). B, The internal parts of the system including the electrode array and electronics case.
The camera captured video and sent the information to the processor, which converted the image to electronic signals and sent them to the transmitter coil on the glasses. The episcleral implanted receiver coil wirelessly received these data and sent the signals to the electrode array, where electrical stimulation pulses were emitted. This spatially mapped microelectrode stimulation of the retinal ganglion cells induced localized cellular responses in the retina that traveled through the optic nerve to the central visual system, resulting in visual percepts.
Stimulation settings were custom fitted for each subject. These settings mapped onto the subject's electrode-specific current amplitudes such that bright areas in the real-time video image (white) created bright percepts (high stimulation current), while dim areas (gray) corresponded to a dim percept (low stimulation current). The current amplitude values were based on the subject's perceptual thresholds for each electrode. Stimulation parameters were chosen such that they maximized the subject's performance on previous assessments during the clinical trial, while remaining within the safety and technical limits of the system. Stimulation parameters used for all subjects were charge-balanced cathodic-first pulses with a pulse width of 0.46 milliseconds, except for a single subject (61-001), who used settings with a pulse width of 0.97 milliseconds. The pulse frequency was fixed for each subject, ranging from 3 Hz to 60 Hz.
DIRECTION OF MOTION TEST
Subjects were instructed to maintain eye and camera (head) fixation on the center of a 19-inch touchscreen monitor (AccuTouch; Elo TouchSystems) located 12 inches in front of them. After an audio prompt, a 1.4-inch white bar swept across the screen at a randomly chosen angle (0°-360° in 1° increments). The orientation of the bar was orthogonal to the direction of motion, and its length spanned the full extent of the screen. The speed of the bar was constant throughout the test and across conditions but varied across subjects according to their best performance (from 7.9° of the visual angle/s to 31.6°/s). Bar speeds used for each subject are listed in Table 1. After each stimulus, the subjects drew the direction of motion they perceived on the touchscreen. A full run consisted of 80 trials; each run was completed in a single session, with no breaks between trials. Automated audio feedback was given after each response; feedback indicated whether the subject's response was within 15° of the stimulus angle in either direction (“correct”) or, if not, provided some general corrective feedback (such as “it moved up and right”). Feedback was given mostly for motivational purposes and to notify the subject that his or her touchscreen response had been recorded. Subjects could not use feedback to correct their responses on the current trial because the next stimulus was randomly chosen.
On each trial, the error (the angular difference between the stimulus direction and response direction) was calculated. Mean errors were compared across conditions with a 2-tailed t test assuming unequal variances. Statistical significance was P < .05.
This study consists of 2 experiments. In the first experiment, 2 conditions were compared: (1) the performance of the task when the subjects used only their residual vision (system off; no glasses were worn) and (2) their performance with the system on and a 1-to-1 spatial mapping (normal mapping). Data were gathered during each of the subject's regular end point testing sessions for the clinical trial (at 3 months, 6 months, 12 months, 18 months, 24 months, and 36 months postimplant). Data reported here were the latest available for each subject, ranging from 6 months for 1 subject to 36 months for those who had been implanted longest at the time of analysis. The end point session for each subject was directly related to the months postimplant, listed in Table 1 (r2 = 0.91). Both 80-trial runs for experiment 1 (with the system on and off) were completed on the same day for each subject, although the subjects may have been given a break between runs. The exception is subject 61-001, who completed the on and off runs 2 weeks apart.
The second experiment was carried out (on a different day) only on those subjects whose data showed a significant difference between the 2 conditions in the first experiment and who were available for testing during the study period (N = 11). In this experiment, the system was on, but the 60 pixels in the down-sampled video image were mapped randomly to the electrode locations (scrambled).7 This control condition ensured that while the field of view (and overall current) of the system remained identical to the normal condition, the spatial structure in the video image was eliminated. The random mapping data from the second experiment was then compared with the system on, normal mapping data, and system off data from the first experiment.
RESULTS
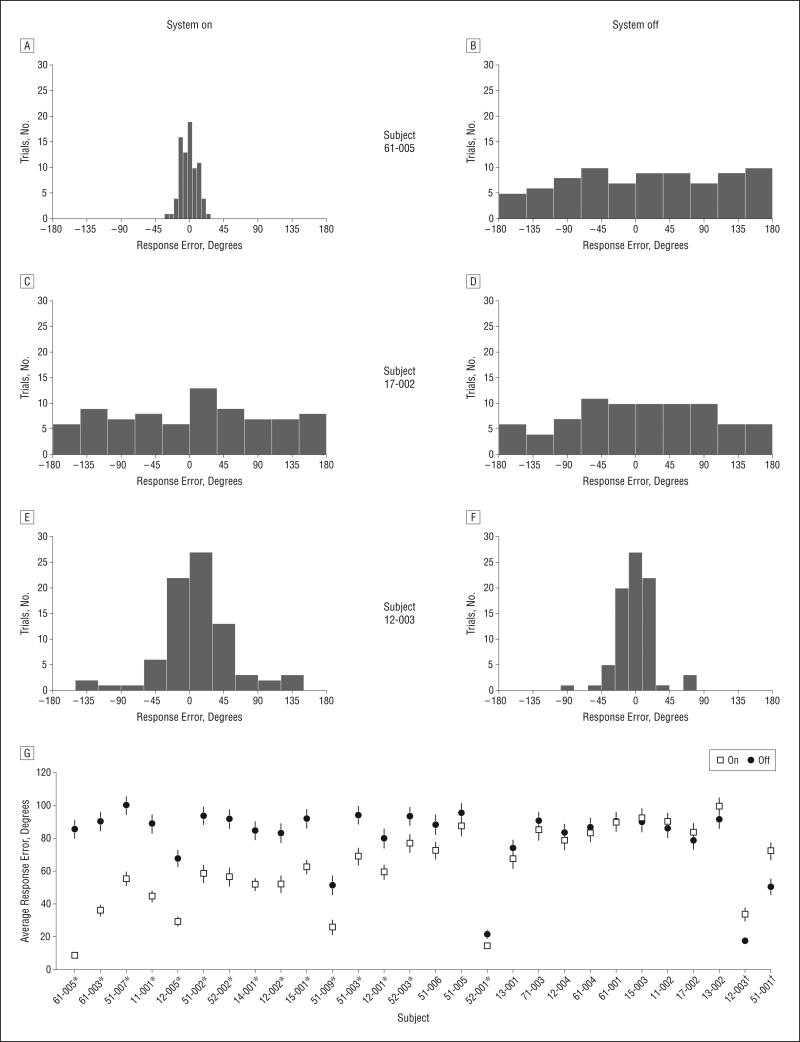
Fifteen of 28 subjects (54%) had a significantly smaller mean error with the system on than when using their residual vision (Figure 2). Eleven subjects were not able to perform the task with or without the system, and 2 subjects had significantly smaller errors with the system off than on.
Figure 2.
Graphs of response error distributions. Example distributions of the response error with the system on and off from 3 subjects (A-F). G, Mean response error for all subjects. * Indicates significant differences between mean response errors with the system on and off (t test; P < .05); † indicates subjects who had significantly better performance with the system off vs on. Error bars indicate standard error of the mean.
Of the 15 subjects who had performed better with the system on in the first experiment, 11 were available for experiment 2. Ten of these (91%) had significantly smaller mean errors with normal spatial mapping than with scrambled spatial mapping; 1 subject showed no significant difference between normal and scrambled mapping performance (Figure 3).
Figure 3.
Graphs of response error distributions. Example distributions of the response error with normal mapping (A), scrambled spatial mapping (B), and with the system off (C). D, Average response error with normal mapping and scrambled mapping. * Indicates significance; error bars indicate standard error of the mean.
Multiple regression analysis was performed to identify whether any of the factors listed in Table 1 (age at implant, self-reported years blind, months implanted, and bar speed) were significantly related to the mean error in experiment 1. None of the factors were significantly related to the mean error with the system on; P values from the multiple regression analysis are shown in Table 2. The analysis was also carried out on the mean error with the system off and the difference between the error with the system off and on. None of these relationships were significant; P values are shown in Table 2.
Table 2.
P values From Multiple Regression Analysis in Which Age at Implant, Months Implanted, Self-Reported Years Blind, and Bar Speed Were the Independent Variables
|
P Valuea |
|||
|---|---|---|---|
| Independent Variable | System On | System Off | Off and On |
| Age at implant, y | .53 | .42 | .87 |
| Time postimplant, mo | .27 | .85 | .18 |
| Duration of self-reported blindness, yb | .26 | .59 | .52 |
| Bar speed, degrees/s | .27 | .38 | .79 |
P values are shown for the dependent variables: mean error with the system on, mean error with the system off, and the difference between the mean errors with the system off and on.
Some data regarding number of years blind were not available owing to a gradual loss of vision.
COMMENT
We demonstrated the ability of blind subjects to determine the direction of motion of an object using the Argus II retinal prosthesis system; more than half of the subjects could perform the task more accurately with the system on than with their residual vision. Two subjects, 12-003 and 51-001, had enough residual vision to perform the task significantly better without the system.
We have also shown that the task requires some spatial vision ability, as strongly supported by the comparative study of normal vs scrambled spatial mapping. These data show that the retinotopic electrode mapping normally used by the system allows subjects to perform significantly better in 91% of cases compared with arbitrary scrambled mapping. The level of spatial vision demonstrated here does not necessarily allow the subjects to distinguish the bar from any other shape, but it clearly allows them to assign direction of motion, a spatial stimulus property.
Performance variability of Argus II subjects is an active area of research. In this study, we did not find significant relationships between mean error on the direction of motion task and any demographic or experiment variable examined. As more data are collected—in this ongoing clinical trial, in patients implanted with the commercially available Argus II, and in patients in future trials—we expect to arrive at a greater understanding of the factors underlying performance differences between patients on this and other visual tasks. Other variables that will be explored are surgeon experience and surgical technique, array placement, and the extent of disease progression.
While the ability to elicit phosphenes through implanted electrode arrays has been demonstrated by several groups,8,9 establishing that retinal prostheses can produce a useful spatial image has proven more difficult. One study on the 16-electrode Argus I showed that 3 subjects were able to find and discriminate objects, determine the orientation of a capital L, and differentiate the direction of motion in a 4-alternative forced-choice task; however, for many tasks, multi-electrode stimulation was only slightly more effective than single-channel stimulation.9 Studies on both epiretinal10 and subretinal11 arrays indicated that creating the percept of a shape through direct, concurrent stimulation of patterns of electrodes was possible but only for a small number of subjects.
Camera image or photodiode-based stimulation has proven to be more successful in providing spatially structured percepts to a few blind subjects. A study of 3 subjects with a subretinal photodiode array found that 1 subject was able to detect the orientation of grid patterns and a Landolt C optotype, identify large letters, and read short words.12 Another investigation on a single Argus I epiretinal prosthesis subject demonstrated spatial vision up to the resolution limit of the 4 × 4 array.7
To our knowledge, the current clinical trial of the Argus II is the first study on a large number of subjects with a device designed for therapeutic use. Interim results from the trial indicated that the Argus II system allowed most subjects to locate objects, more than 50% of subjects to identify the direction of motion of a bar, and about a quarter of subjects to identify the orientation of gratings.13 The clinical trial has resulted in the Argus II receiving CE Mark; as a result, it is now available commercially in the European Economic Area. The finding reported here—that subjects can perform the direction of motion task only with correct spatial mapping and not with scrambled mapping—demonstrates for the first time that electrical stimulation of the retina can be used to produce useful spatial vision in a large number of blind patients.
Acknowledgments
Funding/Support: This study was funded by grant EY012893 from the National Institutes of Health (National Eye Institute's Research/Development of Artificial Retinas for the Blind) to Dr Greenberg (principal investigator).
Footnotes
Author Contributions: Dr McMahon had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Additional Contributions: The sponsor of this study, Second Sight Medical Products Inc, participated in the design and conduct of the study; in the collection, analysis, and interpretation of the data; and in the preparation, review, and approval of the manuscript. Data were collected at each clinical trial site under the supervision of independent site investigators, whose financial interests were limited to compensation for study costs provided to their institutions.
Conflict of Interest Disclosures: Drs Dorn, Caspi, and Greenberg are employed by Second Sight Medical Products Inc, and Drs Ahuja and McMahon were employees while this study was being conducted. Dr McMahon holds stock in the company.
Online-Only Material: The eAppendix is available at http://www.jamaophth.com.
Trial Registration: clinicaltrials.gov Identifier: NCT00407602
REFERENCES
- 1.Zrenner E, Stett A, Weiss S, et al. Can subretinal microphotodiodes successfully replace degenerated photoreceptors? Vision Res. 1999;39(15):2555–2567. doi: 10.1016/s0042-6989(98)00312-5. [DOI] [PubMed] [Google Scholar]
- 2.Rizzo JF, III, Wyatt J, Humayun M, et al. Retinal prosthesis: an encouraging first decade with major challenges ahead. Ophthalmology. 2001;108(1):13–14. doi: 10.1016/s0161-6420(00)00430-9. [DOI] [PubMed] [Google Scholar]
- 3.Humayun MS, de Juan E, Jr, Dagnelie G, Greenberg RJ, Propst RH, Phillips DH. Visual perception elicited by electrical stimulation of retina in blind humans. Arch Ophthalmol. 1996;114(1):40–46. doi: 10.1001/archopht.1996.01100130038006. [DOI] [PubMed] [Google Scholar]
- 4.Stone JL, Barlow WE, Humayun MS, de Juan E, Jr, Milam AH. Morphometric analysis of macular photoreceptors and ganglion cells in retinas with retinitis pigmentosa. Arch Ophthalmol. 1992;110(11):1634–1639. doi: 10.1001/archopht.1992.01080230134038. [DOI] [PubMed] [Google Scholar]
- 5.Klein M, Birch DG. Psychophysical assessment of low visual function in patients with retinal degenerative diseases (RDDs) with the Diagnosys full-field stimulus threshold (D-FST). Doc Ophthalmol. 2009;119(3):217–224. doi: 10.1007/s10633-009-9204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roessler G, Laube T, Brockmann C, et al. Implantation and explantation of a wireless epiretinal retina implant device: observations during the EPIRET3 prospective clinical trial. Invest Ophthalmol Vis Sci. 2009;50(6):3003–3008. doi: 10.1167/iovs.08-2752. [DOI] [PubMed] [Google Scholar]
- 7.Caspi A, Dorn JD, McClure KH, Humayun MS, Greenberg RJ, McMahon MJ. Feasibility study of a retinal prosthesis: spatial vision with a 16-electrode implant. Arch Ophthalmol. 2009;127(4):398–401. doi: 10.1001/archophthalmol.2009.20. [DOI] [PubMed] [Google Scholar]
- 8.Besch D, Sachs H, Szurman P, et al. Extraocular surgery for implantation of an active subretinal visual prosthesis with external connections: feasibility and outcome in seven patients. Br J Ophthalmol. 2008;92(10):1361–1368. doi: 10.1136/bjo.2007.131961. [DOI] [PubMed] [Google Scholar]
- 9.Yanai D, Weiland JD, Mahadevappa M, Greenberg RJ, Fine I, Humayun MS. Visual performance using a retinal prosthesis in three subjects with retinitis pigmentosa. Am J Ophthalmol. 2007;143(5):820–827. doi: 10.1016/j.ajo.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 10.Dorn JD, Ahuja AK, Arsiero M, et al. The Argu II Retinal Prosthesis provides complex form vision for a subject blinded by retinitis pigmentosa.. Paper presented at: Association for Research in Vision and Ophthalmology 2010; Ft Lauderdale, Florida. May 4, 2010. [Google Scholar]
- 11.Wilke R, Gabel VP, Sachs H, et al. Spatial resolution and perception of patterns mediated by a subretinal 16-electrode array in patients blinded by hereditary retinal dystrophies. Invest Ophthalmol Vis Sci. 2011;52(8):5995–6003. doi: 10.1167/iovs.10-6946. [DOI] [PubMed] [Google Scholar]
- 12.Zrenner E, Bartz-Schmidt KU, Benev H, et al. Subretinal electronic chips allow blind patients to read letters and combine them to words. Proc Biol Sci. 2011;278(1711):1489–1497. doi: 10.1098/rspb.2010.1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Humayun MS, Dorn JD, da Cruz L, et al. Interim results from the international trial of Second Sight's visual prosthesis. Ophthalmology. 2012;119(4):779–788. doi: 10.1016/j.ophtha.2011.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]