Abstract
The increased use of Chinese herbal products (CHPs) worldwide has raised the concern of herb–drug interactions. The aim of this study was to determine the prevalence and utilization patterns of concurrent use of conventional drugs and CHPs in Taiwan. The usage and frequency of services in the co-prescription of a CHP and a conventional drug were evaluated. Subjects were recruited from a simple random sample of 1,000,000 subjects from over 22 million beneficiaries of the National Health Insurance in 2007. The logistic regression method was employed to estimate the odds ratios (ORs) for the co-prescription of a CHP and a conventional drug (CH + D) and a conventional drug alone (D-alone). The prevalence of the CH + D was 14.1%. Females, regular salary earners, and elderly (65 years and above) were more likely to consume a CHP and a conventional drug concurrently. Painkillers, especially acetaminophen, and anti-cough medicines were the top two conventional drugs that were most frequently co-prescribed with a CHP. Anti-cough medication is the most common conventional drug co-prescribed with CHP, after painkillers. We recommend that safety issues be investigated in future research and integrating both healthcare technologies may be beneficial for the overall health and quality of life of patients.
Keywords: Chinese herbal product, Co-prescription, Conventional drug, Herb–drug interaction
INTRODUCTION
Even with modern medical advances, Chinese herbal products (CHPs), which have been used as traditional medicine in China, Japan, and Korea for over thousands of years, continue to be widely used for health maintenance, disease prevention, and even disease treatment.[1] Furthermore, in many developed countries, CHPs are becoming increasingly popular, and the world expenditure on CHPs is not only large but also growing rapidly.[1] Therefore, a CHP and a conventional drug are likely used concurrently. Recent studies have indicated that the majority of people do not tell their physicians about the co-utilization of conventional drugs and CHPs.[2,3,4] The concurrent use of conventional drugs and CHPs will increase the risk of potential herb–drug interactions occurring due to the interference in the pharmacokinetics of the first drug.[5,6,7,8,9,10] Cytochrome P450 (CYP450) enzymes are responsible for more than 50% of the metabolism of not only painkillers in our body but also of CHPs like Corydalis Rhizoma (延胡索 Yán Hú Suǒ) and Salviae Miltiorrhiza Radix (丹參 Dān Shēn).[11,12,13] The inhibition of CYP450 because of concurrent CHP use may lead to increased drug plasma level and toxicities. A study reported that concurrent use of conventional drugs and herbal products was found in 15% of patients and there were nearly 40% potential adverse herb–drug interactions among these patients.[14] However, few studies have been performed to survey the prevalence of co-utilization between conventional drugs and CHPs, and previous studies might introduce recall bias due to the nature of self-reporting surveys.[15,16]
Traditional Chinese Medicine (TCM) as a unique traditional therapy for various ailments has also been used in Taiwan for over hundreds of years, and its popularity remains unabated despite the modernization of medical care in Taiwan. In addition, one distinguishing feature of the national healthcare system is the co-existence of the modern conventional medicine and TCM (including acupuncture, chiropractic, and CHP), which has been regularly reimbursed by the National Health Insurance (NHI) in Taiwan since 1995.[17,18,19,20] Also, people in Taiwan are free to visit conventional medicine clinics or TCM clinics. Thus, the NHI research database provides an ideal platform for a pharmacoepidemiological study of this field. This study aimed to explore the demographics and utilization patterns of how frequent is the concurrent use of conventional drugs and CHP on a nationwide level in real practice. We believe that this study would provide evidence-based information for formulating appropriate management strategies of drug safety and integrative medicine.
MATERIALS AND METHODS
Data resources
This study was commenced after obtaining approval from the review board of the Committee on Chinese Medicine and Pharmacy, Department of Health, Taiwan. It was designed as a cross-sectional analysis of a random sample of 1,000,000 subjects out of 22 million beneficiaries of the NHI of Taiwan to determine the national prevalence of co-prescription of CHP and conventional drugs. All data were obtained from the National Health Insurance Research Database (NHIRD), which included all the reimbursement data of the NHI transformed and maintained by the National Health Research Institutes of Taiwan.[21] The identification numbers of all individuals in the NHI database were encrypted to protect the privacy of the individuals. For research purposes, the NHIRD had selected a random sample of 1 million subjects from the 22 million insured population, which contained their medical record files, including medical care facilities and specialties, drugs and/or management for treatment, patient's gender and date of birth, date of visiting, transferred identification number, and three major diagnoses coded in the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) format.[22] Both TCM doctors and conventional doctors must follow the standard diagnoses of using the ICD-9-CM coding system when claiming reimbursement.
Study sample
As all the prescribed conventional drugs are covered under the NHI of Taiwan, no drug could be dispensed at a pharmacy without a doctor's prescription. To construct a fixed cohort, we included the patients who were prescribed conventional drugs from the random sample of 1 million individuals. TCM is one of the oldest healing systems in the world and has been followed in Taiwan for over hundreds of years. Its practice includes CHPs, acupuncture, and traumatology manipulative therapies; these are reimbursed by the NHI of Taiwan. For the purpose of studying combined prescriptions of a CHP and a conventional drug in the present study, we downloaded the claim forms for reimbursed CHPs from the website of the Bureau of NHI. The corresponding herbal information about a specific mixture or name was then obtained from the Committee on Chinese Medicine and Pharmacy (CCMP) website, including the names of each herb and the herbal formulae, the proportions of each constituent, the date and period of approval as drug, code and name of manufacturer given by CCMP. For simplicity, all CHPs with the same CCMP standard formulae are classified under the same categories, regardless of the slight variations among products of different pharmaceutical companies.[23] The variables of a co-prescription of a CHP and a conventional drug for analyses were defined based on the CHP and the conventional drug that were prescribed to one individual on the same day. Figure 1 illustrates the prevalence of the co-prescription of a CHP and a conventional drug in the study cohort from 1997 to 2007. This prevalence seems to have stabilized around 1998, although it does demonstrate a slight increase since 2003. We, therefore, selected 2007, the most up-to-date year, to simplify our analysis. The final fixed cohort consisted of 859,102 users of conventional medicines. Among them, we further categorized the types of preparation used as follows: 738,373 were prescribed a conventional drug alone (D-alone) and 120,729 were co-prescribed a CHP with a conventional drug (CH + D).
Figure 1.
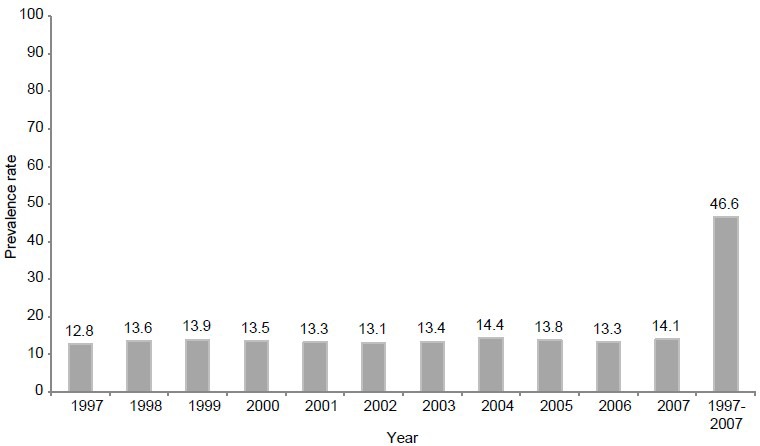
Prevalence of co-prescriptions of Chinese herbal products and conventional drugs among the cohort of users of conventional medicine at the outpatient departments, 1997-2007
Study variables
To understand the key independent variables affecting the utilization of a co-prescribed CHP and conventional drug among users of conventional medicines, we selected the demographic factors according to previous studies.[19] In addition to gender, age of the subjects was categorized into nine groups: 0-4, 5-14, 15-24, 25-34, 35-44, 45-54, 55-64, 65-74, and 75 years or older. Registry for regions was also used to determine the major predictors of the co-prescription group. We split the monthly income into three levels: 0, NT$ 1-9999 and ≥ NT$ 10,000 (1 US$ =29 NT$).
Statistical analysis
Data analysis was undertaken using descriptive statistics, including the prescription rates of either D-alone or CH + D stratified by patient's age and gender, the population distribution, the frequencies of the disease categories prescribed with D-alone and CH + D, and the most frequently prescribed herbs. We also carried out statistical analysis of the database to compare the characteristics between CH + D and D-alone groups. The logistic regression method was used to estimate the odds ratios (ORs) for CH + D and D-alone groups. A significance level of α =0.05 was selected. The most common indications or diagnoses for CH + D group were evaluated. The classification of primary indications was according to the ICD-9-CM. We considered the first diagnosis as the major diagnosis in the outpatient clinic, which was coded in ICD-9 in the NHIRD and then grouped into broader disease categories. For example, ICD-9 codes of 460-519 were classified as diseases of the respiratory system; codes 780-799 were grouped as symptoms, signs, and ill-defined conditions; and codes 520-579 were classified as diseases of the digestive system. The statistical software SAS 9.13 was used for data management and analyses.
RESULTS
The outpatient claims database for 2007 contained information on 859,102 users of conventional medicines with 10,309,191 prescriptions. During the prescription period of conventional medicine, 14.1% (120,729) of the users also received 402,570 prescriptions of CHP on the same day at least once, given by the TCM doctors, of whom 94.3% had worked at local TCM clinics. Approximately 95% of the prescriptions for the concurrent use of a conventional drug and a CHP were for a period of no more than 8 days. Details on the demographic distribution of concurrent use of CH + D and D-alone are provided in Table 1, which shows that the mean age of the CH + D population was slightly higher than that of the D-alone population.
Table 1.
Demographic characteristics of patients who co-prescribed Chinese herbal products and conventional drugs (CH + D) or conventional drug alone (D-alone) from the 1 million random sample of the National Health Insurance Research Database, 2007
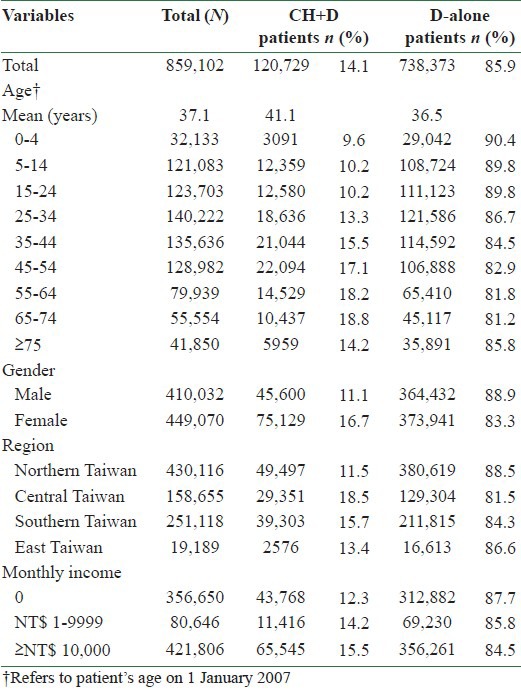
Adjusted OR and 95% confidence intervals (95% CIs) resulting from the logistic regression model are presented in Table 2. After adjusting for other factors, the OR of female patients (CH + D: OR 1.60; D-alone: OR 1.16) was higher than that of males (OR 1.00) to be a concurrent user. Compared with the 25-34 years age group (OR 1.00), the OR of the CH + D increased with age to a peak in the 65-74 years age group (OR 1.49), whereas the ORs of D-alone group became relatively high only in the over 55 years age groups (≥ 75 years age group: OR 6.48). Unlike the behavior of the children's usage of a conventional drug, the OR of children using a combination of a CHP and a conventional drug was less than that of 25-34 years age group (OR 1.00).
Table 2.
Adjusted odds ratios and 95% confidence intervals for the characteristics associated with the utilization of co-prescribed Chinese herbal products and conventional drugs (CH+D) and conventional drug alone (D-alone) in Taiwan, 2007
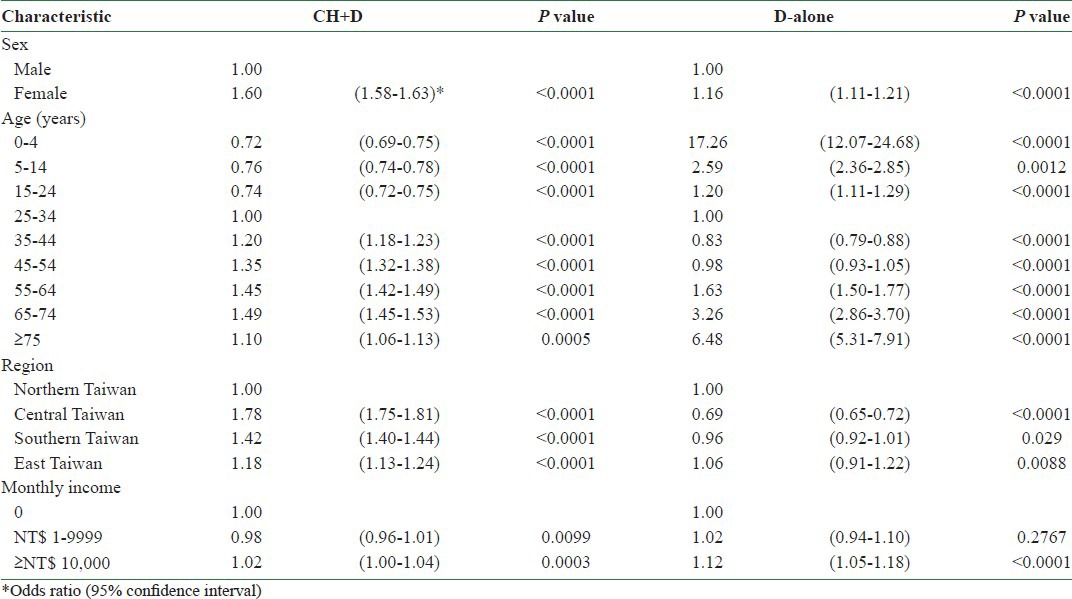
As compared to patients living in Northern Taiwan (OR 1.00), the ORs of CH + D for patients living in Central, Southern, and Eastern Taiwan were 1.78, 1.42, and 1.18, respectively, whereas those of D-alone for patients living in Central, Southern, and Eastern Taiwan were 0.69, 0.96, and 1.06, respectively. As expected, the ORs of patients with monthly income in excess of NT$ 10,000 (CH + D: OR 1.02; D-alone: OR 1.12) were more likely to combine CHPs and conventional drugs than those with no income (OR 1.00).
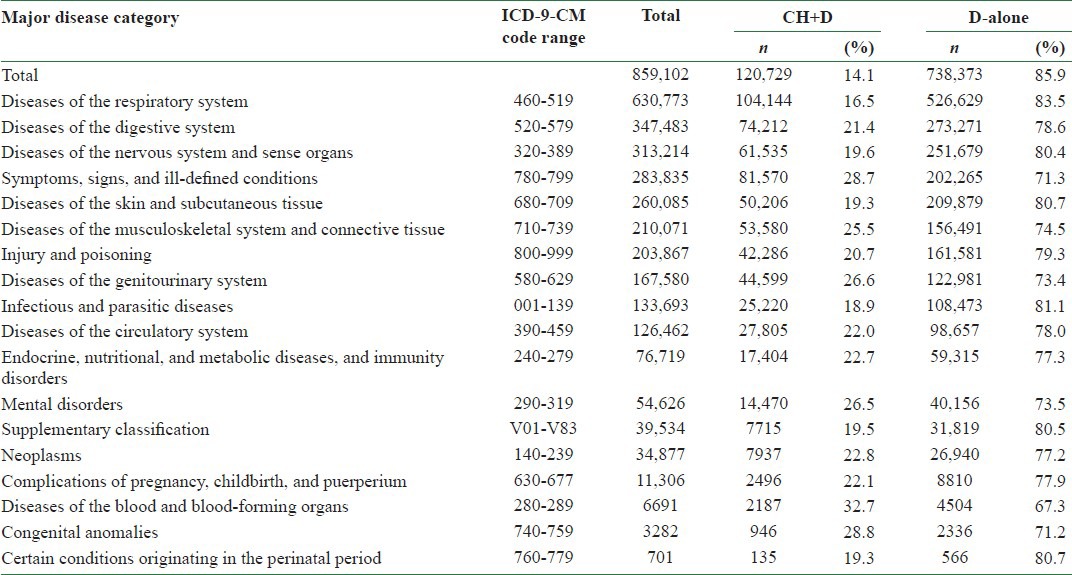
On analysis of the percentage distribution of 859,102 users of conventional medicines, we found the diseases of the respiratory system (630,773) were the most frequent major disease category, followed by diseases of the digestive system (347,483) and diseases of the nervous system and sense organs (313,214) [Table 3]. As for the prevalence rate of either concurrent use of conventional medicine and CHP or use of D-alone with respect to the major disease categories, compared with the patients suffering from diseases of the respiratory system (OR 1.00), patients with diseases of the blood and blood-forming organs were associated with a 2.46-fold (95% CI 2.33-2.59), patients with congenital anomalies had 2.05-fold (95% CI 1.90-2.21), and patients with diseases of the symptoms, signs, and ill-defined conditions had 2.04-fold (95% CI 2.02-2.06) increase in the use of a CHP and a conventional drug.
Table 3.
Subjects’ and frequency distribution of the co-prescribed Chinese herbal medicine and conventional drugs (CH+D) and conventional medicine alone (D-alone) at outpatient visits stratified by major disease categories (according to ICD codes) in Taiwan, 2007
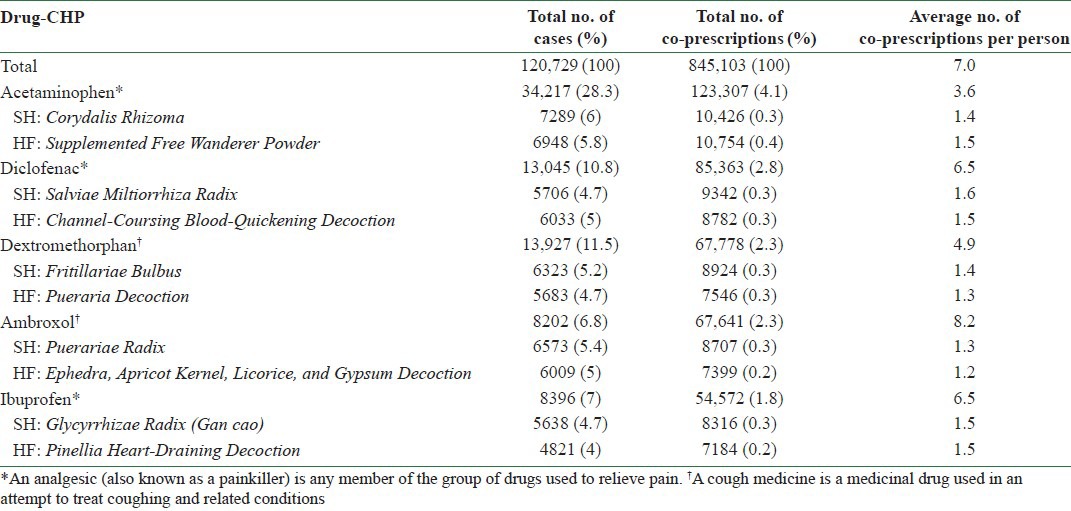
As Table 4 shows, acetaminophen, dextromethorphan, diclofenac, ibuprofen, and ambroxol were the top five most frequently combined prescribed conventional drugs with CHPs. Details on the most frequently prescribed herbs are also provided in Table 4, which shows that Corydalis Rhizoma (延胡索 Yán Hú Suǒ) was the most frequently prescribed herb, followed by Fritillariae Bulbus (貝母 bèi mǔ) and Salviae Miltiorrhiza Radix (丹參 Dān Shēn). Supplemented Free Wanderer Powder (加味逍遙散 Jiā Wèi Xiāo Yáo Sǎn) was the most frequently prescribed formula, followed by Pueraria Decoction (葛根湯 Gé Gēn Tang) and Channel-Coursing Blood-Quickening Decoction (舒筋活血湯 Shū Jīn Huó Xuè Tang).
Table 4.
Top five co-prescribed Chinese herbal products and conventional drugs, by case and co-prescription frequency, 2007
DISCUSSION
High prevalence of co-prescription
This survey provides evidence that the co-prescription of a CHP and a conventional drug has a relatively high prevalence (14.1%) in Taiwan. To the best of our knowledge, this study is the first of its kind using a random national-level sample to document the use of CHP concomitant with prescription medicines. It is interesting to note how simultaneously conventional medicine was used among TCM users when the expenses of the conventional medicine and CHPs are both reimbursed by the NHI system in Taiwan.[17,18,19,20] This system allowed all beneficiaries choosing either conventional medicine or TCM freely to relieve their discomfort and/or diseases, resulting in a high insured rate of 99% of the Taiwanese population who have joined the NHI program.[17,21] Therefore, the estimated prevalence rate presented here is close to the true concomitant use of CHP and conventional drug in Taiwan. Moreover, unlike recall bias, which can be introduced by self-reporting surveys,[15,16] all patients in the present study who suffered from some degree of discomfort or a disease were prescribed CHP by licensed TCM doctors and conventional drugs by doctors of conventional medicine. The computerized reimbursement database of the NHI stores longitudinal data of the beneficiaries of both Western and Chinese medicines, thus providing an optimal platform for determining the utilization pattern of CHPs and conventional drugs concurrently. These data provide important information on Taiwan's experience for policy makers of other countries who seriously consider the recommendations of integrating traditional medicine into the national health system by the World Health Organization.[1]
The present study indicates that more than one of every ten patients receiving conventional drugs that were prescribed by their doctors still sought for TCM and received CHP prescription on the same day in 2007. Furthermore, the present data also show that more than 94% of the patients who simultaneously used both a conventional drug and a CHP received the drug and CHP from different locations. This finding indicates that most doctors of conventional medicine do not know from patient charts what herbs their patients consume and for what reasons their patients want to add Chinese herbs to their regular conventional medicine, which may result in a potential herb-drug interaction and lead to an unpredictable efficacy.[5,6,7,8,9,10] We actually knew very little about herbs and their potential for interaction with drugs; therefore, these incidents could be only the tip of the iceberg. Healthcare providers and public health and policy analysts should give greater attention to this particular healthcare seeking behavior and should assess the potential long-term impact on health outcomes among this population.
Characteristics of concurrent users
The present study found that frequent TCM users such as females and individuals with a regular salary income[18,19,20,24,25,26,27,28,29,30,31,32,33] were more likely to consume CHPs and conventional drugs concurrently than males and those in the low-income group. As compared to patients living in Northern Taiwan, patients living in Central, Southern, or Eastern Taiwan were more likely to be a concurrent user. Possibly, Taiwan's earliest settlers who had come from mainland China introduced TCM into the southern part of Taiwan, which became the major health care of Southern Taiwan in the early 17th century. The present data also show that the co-administration peaked over 64 years of age, followed by the 55-64 and 45-54 years age groups, which was in contrast to the distribution of the D-alone group. Among the elderly users of conventional medicine, approximately one out of five, at some day during the study period in Taiwan, consumed herbs concurrently intending to relieve their discomfort from an upper respiratory infection or hypertension or from diseases of symptoms, signs, and ill-defined conditions. A previous study has proposed that the public and physicians require more education concerning the inappropriate use of conventional drugs by the elderly in Taiwan.[34,35,36] The results of the present study suggest that without setting up an integrative system to fully communicate between systems of TCM and conventional medicine, the add-on prescriptions of TCM might further produce complications among the elderly population. Further studies are warranted to provide information for the safe use of TCM interventions in conjunction with conventional medicine among the elderly.[37,38]
In contrast to the utilization pattern of the D-alone group, the present data show that diseases of the blood and blood-forming organs (ICD-9 codes 280-289), congenital anomalies (ICD-9 codes 740-759), and diseases of the symptoms, signs, and ill-defined conditions (ICD-9 codes 780-799) were the top three categories of patients with a high proportion that consumed a CHP and a conventional drug on the same day in Taiwan.[39] Ancient Chinese medicine theory encourages women taking Chinese herbal medicine to build up their blood supply in order to reserve strength for each menstruation cycle because women expect a significant amount of blood to be lost during that.[40,41] The anemia-related fatigue, dizziness, and palpitations might be the major reasons that lead to the patient's behavior of seeking TCM and receiving prescriptions of conventional drugs and CHPs concurrently. Similar to the diseases of the symptoms, signs, and ill-defined conditions, congenital anomalies often present physical problems not easily resolved, which tend to increase patient's and family's anxiety, leading to concurrent use of conventional drugs and complementary treatments. To avoid herb–drug interaction, we recommend the establishment of integrative approach between conventional medicine and TCM in the future, beginning with the above three major categories of diagnosis.
The most common concurrent drugs and CHPs
Table 4 shows that pain killers and cough medicines were among the most frequent drugs co-prescribed with CHPs. Over one-fourth of the CH + D group had taken acetaminophen. Among these concurrent users, Corydalis Rhizoma was the most common Chinese single herb that, according to the documentation of ancient Chinese medicine book, can relieve pain in any part of the body resulting from Qi stagnation and blood stasis. In addition, a previous clinical trial indicated that Supplemented Free Wanderer Powder (加味逍遙散 Jiā Wèi Xiāo Yáo Sǎn), which was the most commonly prescribed Chinese formula in acetaminophen users, might be an alternative choice for relief of somatic symptoms in postmenopausal women. Similarly, Fritillariae Bulbus (貝母 Bèi Mǔ) or Pueraria Decoction (葛根湯 Gé Gēn Tang) and Puerariae Radix (葛根 Gé Gēn) or Ephedra, Apricot Kernel, Licorice, and Gypsum Decoction (麻杏甘石湯 Má Xìng Gān Shí Tāng) were often prescribed for treating cough and reducing sputum retention by TCM doctors. Therefore, the concerns regarding herb–drug interactions cannot be overlooked; thus, further study on the safety and efficacy of such concurrent use of conventional drugs and CHPs is warranted.[42]
Limitations
Our study has three limitations. First, NHI only reimburses CHPs; decoction is not reimbursed and, therefore, not included and cannot be generalized as to its usage. Second, this study did not include Chinese herbal remedies purchased directly from the pharmacies of TCM, nor did it include health food containing herbs. Thus, the frequency of concurrent use of conventional medicine and CHP might have been underestimated. However, because the NHI system has a comprehensive coverage and the copayment for prescriptions is universally NT$ 50 (new Taiwan) (approximately equal to US$ 1.5), which is generally less than the cost of herbs sold in Taiwan's markets, the likelihood that the subjects purchased many other herbs outside of the NHI database is not high.
CONCLUSION
In summary, under the co-existence of the conventional medicine system and Chinese medicine system, this study found that concurrent use of the drugs and CHP was high in Taiwan. Acetaminophen was the most frequently prescribed painkiller to be used in combination with CHP. The present data provide up-to-date information for all physicians and TCM practitioners concerning the safety of co-administration of pain killers and CHPs. Thus, we recommend that to optimize the health care of our patients under limited resources, policy makers should implement their plans to allow integration of two separate healthcare systems. Additionally, we recommend that countries that plan to integrate traditional medicine into the modern healthcare system should set strategies to minimize the potential drug–herb interactions at the very early beginning of the development of integrative medicine.
ACKNOWLEDGMENTS
This research was conducted at the Institute of Traditional Medicine at the School of Medicine, National Yang-Ming University, and Taipei. We would like to express our sincere gratitude for the partial support provided for this project in the form of grants by the Committee on Chinese Medicine and Pharmacy (CCMP100-RD-033) and the National Health Research Institutes (NHRI-EX96-9204PP). We also thank Drs Chang-Hsing Lee, Yao-Shau Yang, and Chien-Tung Wu for the helpful comments provided on the theory and practice of Chinese medicine.
REFERENCES
- 1.World Health Organization. The regional strategy for traditional medicine in the Western Pacific. (2011-2020) [Last accessed on 2013 Oct 02]. Available from: http://www.wpro.who.int/publications/PUB_9789290615590/en/
- 2.Eisenberg DM, Kessler RC, Van Rompay MI, Kaptchuk TJ, Wilkey SA, Appel S, et al. Perceptions about complementary therapies relative to conventional therapies among adults who use both: Results from a national survey. Ann Intern Med. 2001;135:344–51. doi: 10.7326/0003-4819-135-5-200109040-00011. [DOI] [PubMed] [Google Scholar]
- 3.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the United States, 1990-1997: Results of a follow-up national survey. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 4.Casey M, Adams J, Sibbritt D. An examination of the clinical practices and perceptions of professional herbalists providing patient care concurrently with conventional medical practice in Australia. Complement Ther Med. 2008;16:228–32. doi: 10.1016/j.ctim.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Fugh-Berman A. Herb-drug interactions. Lancet. 2000;355:134–8. doi: 10.1016/S0140-6736(99)06457-0. [DOI] [PubMed] [Google Scholar]
- 6.Miller LG. Herbal medicinals: Selected clinical considerations focusing on known or potential drug-herb interactions. Arch Intern Med. 1998;158:2200–11. doi: 10.1001/archinte.158.20.2200. [DOI] [PubMed] [Google Scholar]
- 7.Izzo AA, Ernst E. Interactions between herbal medicines and prescribed drugs: An updated systematic review. Drugs. 2009;69:1777–98. doi: 10.2165/11317010-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Zhou S, Huang M, Xu A, Yang H, Duan W, Paxton JW. Prediction of herb–drug metabolic interactions: A simulation study. Phytother Res. 2005;19:464–71. doi: 10.1002/ptr.1559. [DOI] [PubMed] [Google Scholar]
- 9.Li CG, Yang L, Zhou S-F. Interaction between Chinese herbal medicines and drugs. Aust J Acupunct Chin Med. 2007;2:17–24. [Google Scholar]
- 10.Hu Z, Yang X, Ho PC, Chan SY, Heng PW, Chan E, et al. Herb-drug interactions: A literature review. Drugs. 2005;65:1239–82. doi: 10.2165/00003495-200565090-00005. [DOI] [PubMed] [Google Scholar]
- 11.Forrest J, Clements JA, Prescott LF. Clinical Pharmacokinetics of Paracetamol-Springer. Clinical Pharmacokinet. 1982;7:93–107. doi: 10.2165/00003088-198207020-00001. [DOI] [PubMed] [Google Scholar]
- 12.Verbeeck RK, Blackburn JL, Loewen GR. Clinical pharmacokinetics of non-steroidal anti-inflammatory drugs. Clin Pharmacokinet. 1983;8:297–331. doi: 10.2165/00003088-198308040-00003. [DOI] [PubMed] [Google Scholar]
- 13.Zhou L, Zuo Z, Chow MS. Danshen: An overview of its chemistry, pharmacology, pharmacokinetics, and clinical use. J Clin Pharmacol. 2005;45:1345–59. doi: 10.1177/0091270005282630. [DOI] [PubMed] [Google Scholar]
- 14.Bush TM, Rayburn KS, Holloway SW, Sanchez-Yamamoto DS, Allen BL, Lam T, et al. Adverse interactions between herbal and dietary substances and prescription medications: A clinical survey. Altern Ther Health Med. 2007;13:30–5. [PubMed] [Google Scholar]
- 15.Ng TP, Tan CH, Kua EH. Singapore Chinese Longitudinal Aging Study. The use of Chinese herbal medicines and their correlates in Chinese older adults: The Singapore Chinese Longitudinal Aging Study. Age Ageing. 2004;33:135–42. doi: 10.1093/ageing/afh016. [DOI] [PubMed] [Google Scholar]
- 16.Loh CH. Use of traditional Chinese medicine in Singapore children: Perceptions of parents and paediatricians. Singapore Med J. 2009;50:1162–8. [PubMed] [Google Scholar]
- 17.Lee YC, Huang YT, Tsai YW, Huang SM, Kuo KN, McKee M, et al. The impact of universal National Health Insurance on population health: The experience of Taiwan. BMC Health Serv Res. 2010;10:225. doi: 10.1186/1472-6963-10-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen FP, Chen TJ, Kung YY, Chen YC, Chou LF, Chen FJ, et al. Use frequency of traditional Chinese medicine in Taiwan. BMC Health Serv Res. 2007;7:26. doi: 10.1186/1472-6963-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang LC, Huang N, Chou YJ, Lee CH, Kao FY, Huang YT. Utilization patterns of Chinese medicine and Western medicine under the National Health Insurance Program in Taiwan, a population-based study from 1997 to 2003. BMC Health Serv Res. 2008;8:170. doi: 10.1186/1472-6963-8-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hsieh SC, Lai JN, Lee CF, Hu FC, Tseng WL, Wang JD. The prescribing of Chinese herbal products in Taiwan: A cross-sectional analysis of the national health insurance reimbursement database. Pharmacoepidemiol Drug Saf. 2008;17:609–19. doi: 10.1002/pds.1611. [DOI] [PubMed] [Google Scholar]
- 21.National Health Research Institutes. National Health Insurance Research database. [Last accessed on 2013 Oct 02]. Available from: http://nhird.nhri.org.tw/date_01.html .
- 22.Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision (ICD-9) 1979. [Last cited in 2009 Oct 21]. Available from: http://www.cdc.gov/nchs/icd/icd9.htm .
- 23.Department of Chinese Medicine and Pharmacy (previous name: Committee on Chinese Medicine and Pharmacy), Ministry of Health and Welfare, Taiwan. [Last accessed on 2013 Oct 02]. http://http://www.mohw.gov.tw/CHT/DOCMAP/query_liense.aspx?mode=1 .
- 24.Chen LC, Wang BR, Chou YC, Tien JH. Drug utilization pattern of Chinese herbal medicines in a general hospital in Taiwan. Pharmacoepidemiol Drug Saf. 2005;14:651–7. doi: 10.1002/pds.1087. [DOI] [PubMed] [Google Scholar]
- 25.Lim M, Sadarangani P, Chan H, Heng J. Complementary and alternative medicine use in multiracial Singapore. Compl Therap Med. 2005;13:16–24. doi: 10.1016/j.ctim.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Cassidy CM. Chinese medicine users in the United States part I: Utilization, satisfaction, medical plurality. J Altern Complement Med. 1998;4:17–27. doi: 10.1089/acm.1998.4.1-17. [DOI] [PubMed] [Google Scholar]
- 27.Kang J, Lee C, Chen C. Factors related to the choice of clinic between Chinese traditional medicine and Western medicine. J Formos Med Assoc. 1994;93:S49–55. [PubMed] [Google Scholar]
- 28.Chi C, Lee J, Lai J, Chen S. Utilization of Chinese medicine in Taiwan. Altern Ther Health Med. 1997;3:40–53. [PubMed] [Google Scholar]
- 29.Chou P. Factors related to utilization of traditional Chinese medicine in Taiwan. Zhonghua Yi Xue Za Zhi (Taipei) 2001;64:191–202. [PubMed] [Google Scholar]
- 30.Wolsko PM, Eisenberg DM, Davis RB, Ettner SL, Phillips RS. Insurance coverage, medical conditions, and visits to alternative medicine providers: Results of a National survey. Archives of Internal Medicine. JAMA. 2002;162:281–7. doi: 10.1001/archinte.162.3.281. [DOI] [PubMed] [Google Scholar]
- 31.Ma GX. Between two worlds: The use of traditional and Western health services by Chinese immigrants. J Commun Health. 1999;24:421–37. doi: 10.1023/a:1018742505785. [DOI] [PubMed] [Google Scholar]
- 32.Druss B. Association between use of unconventional therapies and conventional medical services. JAMA. 1999;287:651–6. doi: 10.1001/jama.282.7.651. [DOI] [PubMed] [Google Scholar]
- 33.Cleary-Guida MB, Okvat HA, Oz MC, Ting W. A regional survey of health insurance coverage for complementary and alternative medicine: Current status and future ramifications. J Altern Complement Med. 2001;7:269–73. doi: 10.1089/107555301300328142. [DOI] [PubMed] [Google Scholar]
- 34.Ma H, Lum C, Dai L. Potentially inappropriate medication in elderly patients in outpatient clinics. Asian J Gerontol Geriatr. 2008;3:27–33. [Google Scholar]
- 35.Lin HY, Liao CC, Cheng SH, Wang PC, Hsueh YS. Association of potentially inappropriate medication use with adverse outcomes in ambulatory elderly patients with chronic diseases. Drugs Aging. 2008;25:49–59. doi: 10.2165/00002512-200825010-00006. [DOI] [PubMed] [Google Scholar]
- 36.Chen YC, Hwang SJ, Lai HY, Chen TJ, Lin MH, Chen LK, et al. Potentially inappropriate medication for emergency department visits by elderly patients in Taiwan. Pharmacoepidemiol Drug Saf. 2009;18:53–61. doi: 10.1002/pds.1684. [DOI] [PubMed] [Google Scholar]
- 37.Williams CM. Using medications appropriately in older adults. Am Fam Physician. 2002;66:1917–25. [PubMed] [Google Scholar]
- 38.Dergal JM, Gold JL, Laxer DA, Lee MS, Binns MA, Lanctôt KL, et al. Potential interactions between herbal medicines and conventional drug therapies used by older adults attending a memory clinic. Drugs Aging. 2002;19:879–86. doi: 10.2165/00002512-200219110-00005. [DOI] [PubMed] [Google Scholar]
- 39.Roy MJ, Koslowe PA, Kroenke K, Magruder C. Signs, symptoms, and ill-defined conditions in Persian Gulf War veterans: Findings from the Comprehensive Clinical Evaluation Program. Psychosom Med. 1998;60:663–8. doi: 10.1097/00006842-199811000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Yeh LL, Liu JY, Liu YS, Lin KS, Tsai TF, Wang LH. Anemia-related hemogram, uterine artery pulsatility index, and blood pressure for the effects of Four-Agents-Decoction (Si Wu Tang) in the treatment of primary dysmenorrhea. J Altern Complement Med. 2009;15:531–8. doi: 10.1089/acm.2008.0208. [DOI] [PubMed] [Google Scholar]
- 41.Yeh LL, Liu JY, Lin KS, Liu YS, Chiou JM, Liang KY, et al. A randomised placebo-controlled trial of a traditional Chinese herbal formula in the treatment of primary dysmenorrhoea. PLoS One. 2007;2:e719. doi: 10.1371/journal.pone.0000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Delgoda R, Younger N, Barrett C, Braithwaite J, Davis D. The prevalence of herbs use in conjunction with conventional medicines in Jamaica. Complement Ther Med. 2010;18:13–20. doi: 10.1016/j.ctim.2010.01.002. [DOI] [PubMed] [Google Scholar]


