Abstract
We review the literature conjoining acupuncture, migraine, and cerebral hemodynamics. To do so, we searched PubMed in March 2013 for studies investigating cerebral hemodynamics with functional magnetic resonance imaging (fMRI), near-infrared spectroscopy (NIRS), transcranial Doppler (TCD) ultrasound, and other tools in migraineurs, acupuncture recipients, and migraineurs receiving acupuncture. Our search identified 1321 distinct articles – acupuncture (n = 463), migraine (n = 866), and both (n = 8). Only three (n = 3) satisfied our inclusion criteria. Based on these three, we found the following: (1) Acupuncture may positively influence not just dynamic, but also static cerebral autoregulation during the interictal phase, depending on the intervals between sessions of acupuncture as dose units. (2) TCD can detect pretreatment differences between responders and non-responders to acupuncture, which may be predictive of clinical response. (3) “Point-through-point” needling (at angles connecting acupoints) may be clinically superior to standard acupuncture, thus needling angles may affect treatment effectiveness. None of the reviewed articles investigated patient responses during migraine attack. Although the 2009 Cochrane review affirmed acupuncture as effective prophylaxis for migraine, few studies investigated the cerebrovascular aspects – only analyzing arterial blood flow, but not microcirculation. Future research is warranted in monitoring brain tissue oxygenation to investigate acupuncture as both a preventive and abortive treatment for migraine, varying the type and dose interval and analyzing variations in clinical response.
Keywords: Acupuncture, Cerebral autoregulation, Cerebral hemodynamics, Migraine, Transcranial doppler sonography
INTRODUCTION
Migraine is a neurovascular disorder, often characterized by unilateral, throbbing, debilitating recurrent headache, which may be accompanied by visual aura.[1] Episodic migraine may evolve to a chronic condition. It occurs in more than 10% of the world's population, afflicting more women than men by a ratio 3:1, and inflicts significant personal and socioeconomic costs.[2] It was ranked eighth worldwide by the World Health Organization among the leading causes of disability in 2010.[3] Standard acute treatment of migraine to treat attacks revolves around pain relievers [e.g., nonprescription nonsteroidal anti-inflammatory drugs (NSAIDs) or nonprescription analgesics], ergotamines, or triptans. Standard preventive treatment entails drug therapy based on beta-blockers (e.g., propranolol, originally developed to treat high blood pressure), anti-seizure drugs (e.g., topiramate), or tricyclic antidepressants (e.g., amitriptyline), in combination with behavioral therapy or lifestyle adjustments. Alternative and complementary therapies range from natural treatments, such as riboflavin, magnesium, coenzyme Q10, and butterbur, to non-drug treatments, such as biofeedback and relaxation training.
Acupuncture, historically and theoretically grounded in Chinese medical theory, has recently been gaining acceptance in the West as a viable alternative or complementary treatment for migraine and other pain conditions.[4] The most current Cochrane review on acupuncture for migraine prophylaxis concluded in 2009 that acupuncture is at least as effective as the standard drug treatment for migraine and carries fewer side effects.[5] In addition, the treatment appears effective as prophylaxis for migraine patients suffering from medication overuse, notwithstanding the potential for reduced costs.[6,7]
Nonetheless, the mechanisms behind the treatment's effectiveness remain obscured. It is known that acupuncture modulates neuronal responses in the brain for healthy individuals, affecting many of the regions in the brain that are also affected by migraine. This suggests that acupuncture attenuates migraine, at least in part, through cerebrovascular mechanisms, which rely on brain topographic tools to unravel.[8,9,10,11,12]
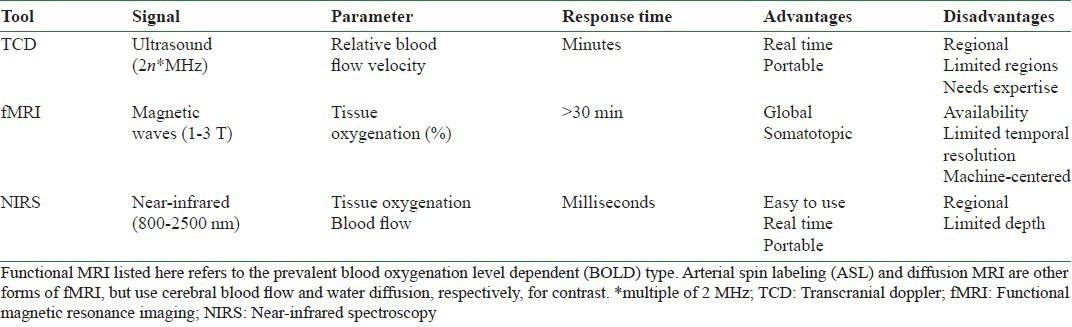
The tools that can investigate the blood flow dynamics (hemodynamics encompassing macro- and microcirculation, perfusion, and hemoglobin oximetry) of the brain, such as functional magnetic resonance imaging (fMRI), transcranial Doppler (TCD) ultrasound, and near-infrared spectroscopy (NIRS), as opposed to other aspects, like the electrophysiological, metabolic, or biochemical, are generally safer and more convenient than their counterparts [Table 1]. Such tools access the neuronal aspects of brain activity by observing the vascular system and present a two-pronged approach for investigating the dual nature of migraine, in contrast to inferring neuronal activity via, say, electrical signals by electroencephalography (EEG) or glucose metabolism observed by positron emission tomography (PET).
Table 1.
Primary hemodynamic brain mapping tools: A summary of the advantages and disadvantages of fMRI, NIRS, and TCD
Our aim is to review the cerebral hemodynamics (CH) involved in acupuncture and migraine headache, elucidated by modern brain imaging techniques.
MATERIALS AND METHODS
For our search, we identified articles that investigate migraine patients undergoing acupuncture treatment with at least one brain mapping tool, such as fMRI. Other aspects of the studies were left to vary. As a first step, we broadly searched the PubMed database to the limits of its coverage on 20 March 2013 for mention in title or abstract, or by MeSH Term when applicable, of acupuncture, migraine, or both acupuncture and migraine, with 1 of 12 terms for mapping modalities, to generate 36 separate queries of the database. (While it is sufficient to generate only the 24 separate queries involving either “acupuncture” or “migraine,” since querying “both” generates redundant articles, we nonetheless opted for the method described.) We used no additional sources (no contact with study authors to identify additional studies).
Search criteria for studies:
Involves migraine patients
Involves acupuncture treatment
Uses hemodynamic brain mapping tool (e.g., fMRI or TCD)
No restriction on comparisons, study design, or length of follow-up
No restriction on years considered (up to the limits of the database)
No restriction on language during the search
No restriction on publication status during the search.
Mapping modalities chosen:
fMRI
TCD ultrasound
NIRS
Single-photon emission computed tomography (SPECT)
Perfusion imaging (PI)
Arterial spin labeling (ASL).
In the search, we also included a term for CH to capture results not found using the above modalities.
Considered but excluded modalities:
EEG
Magnetoencephalography (MEG)
PET (can be used to obtain information on blood flow, but this feature is less frequently relied on and thus not included above)
Magnetic resonance spectroscopy (MRS)
Nuclear magnetic resonance (NMR)
Magnetic resonance imaging (MRI), including diffusion MRI (DMRI), but not fMRI, ASL, and MR perfusion
Angiography (gives primarily structural, not functional data)
Venography (gives primarily structural, not functional data).
Search results were collected and managed as references in a private database using EndNote© software. Our table also lists all but the last three excluded modalities [Table 2]. After identifying “hemodynamic” articles in the “both” category, we excluded reviews, study designs, study protocols, and any article not in English or Chinese. Our review is based on the remaining articles [Figure 1 and Table 3].
Table 2.
Search results: Numbers of articles found for each brain mapping tool
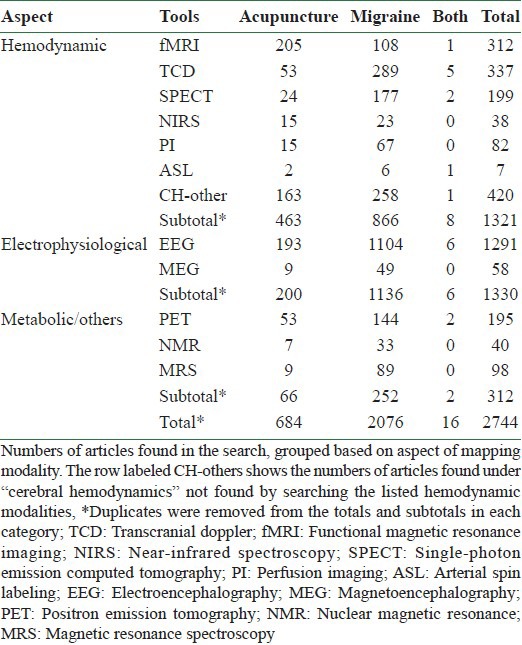
Figure 1.
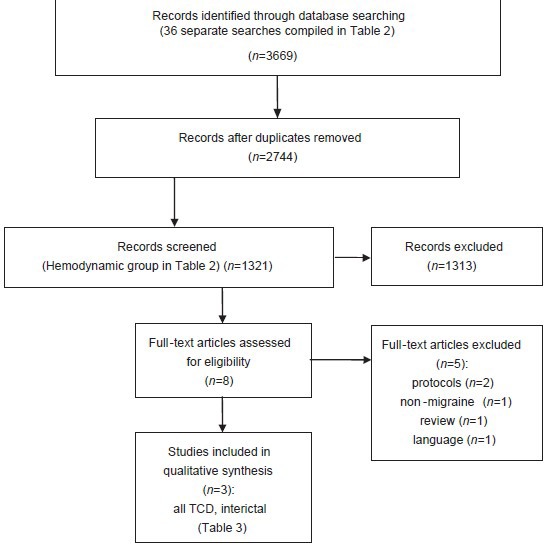
Summary of search methodology
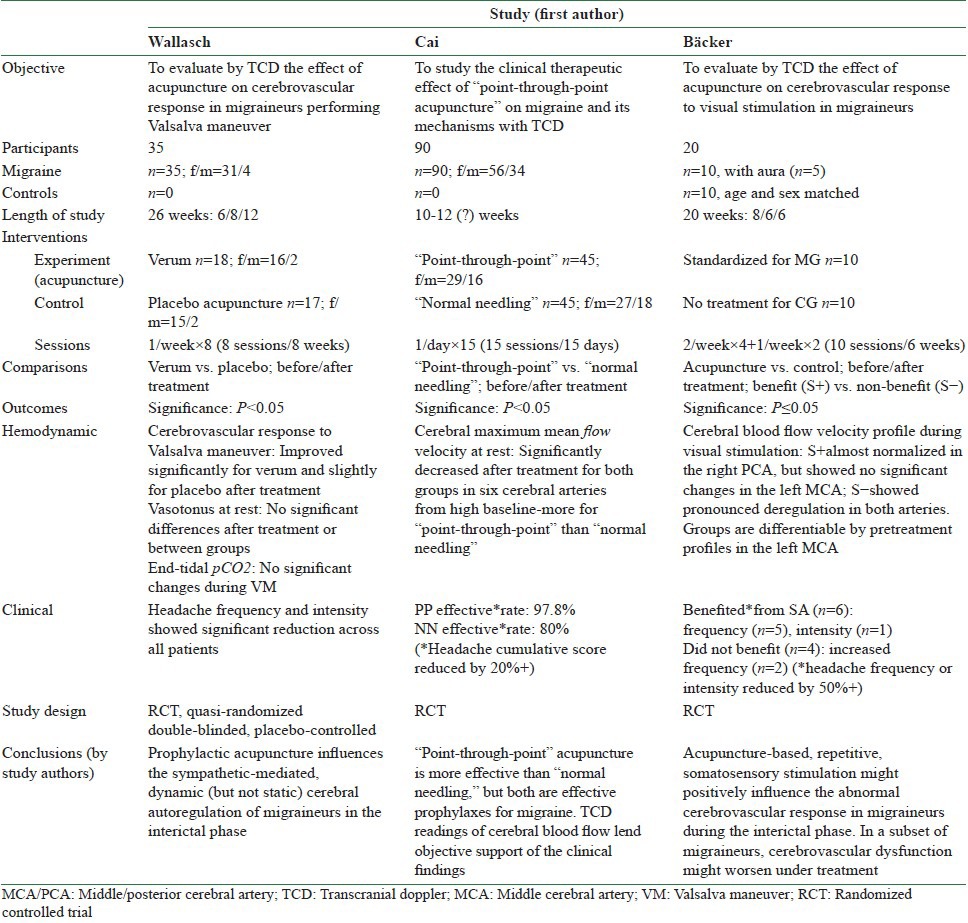
Table 3.
Included studies: A summary of the articles included for review
RESULTS
We conducted a broad search, identifying 1321 unique articles mentioning a hemodynamic brain mapping modality and acupuncture (n = 463), migraine (n = 866), or both (n = 8) [Figure 1 and Table 1]. After excluding review articles, study protocols, and a non-migraine article, only three articles of interest remained. Of the excluded articles, one is a summary of clinical findings for acupuncture and moxibustion at a hospital in Japan taking ASL readings of patients suffering from neurological diseases, some of whom are migraineurs.[13] This Japanese study, whose abstract only provided qualitative information, was excluded primarily for language reasons, being neither in English nor Chinese. The studies included for review vary in size, comparisons, experiment protocols (type of acupuncture treatment, treatment schedule, stimulation paradigm), but their common thread is the use of TCD to measure arterial blood flow in the brains of migraineurs in the interictal phase [Table 3].
Changes in cerebrovascular response to visual stimulation in migraineurs after acupuncture
The pilot study by Bäcker et al. employed healthy control subjects (n = 10) for comparison with migraine patients (n = 10) under acupuncture treatment to establish baseline cerebrovascular response patterns to visual stimulation (flashing light), but had no sham control treatment.[14] Patients had at least a 1-year history of migraine, based on the International Classification of Headache Disorders, 1st edition International Classification of Headache Disorders (ICHD-I) criteria ca. 1988, for diagnosis. A 6-week course (10 sessions) of acupuncture was applied twice weekly for the first 4 weeks, and then once weekly for 2 weeks. Needling was bilateral on the acupoints: Baihui (Du20), Fengchi (Gb20), Taiyang (ExHN5), Sizhukong (3B23), Waiguan (3B5), Taichong (LR3), and Zulinqi (Gb41). A standardized, non-uniform protocol was used for manual rotary stimulation of needles after insertion, varied by angle of rotation (Baihui, Sizhukong, and Taiyang received none). Needles were left in place for 30 min after the stimulation period. Post facto comparisons were also made between responders and non-responders to treatment. Clinical response was defined as a 50% or greater reduction in either headache frequency or headache intensity in the post-treatment period. Quantitative and qualitative changes in cerebral blood flow velocity were recorded through TCD, applied to the left middle cerebral artery (MCA) and the right posterior cerebral artery (PCA).
Most (n = 5) of those who benefited (n = 6) from acupuncture passed the threshold for reduction in headache frequency. Some (n = 2) of those who did not benefit (n = 4) showed increased headache frequency after treatment. Before treatment, cerebral blood flow in migraine patients showed an exaggerated response pattern (overshooting at the beginning of stimulation and a delayed return to the baseline after stimulation) compared with healthy controls. After treatment, the benefit group (n = 6) showed significant change approaching normalization in the right PCA, with no significant change in the left MCA, while the non-benefit group (n = 4) showed increased blood flow velocity during all phases in both arteries, presenting a response diverging further from the pattern for control subjects. In pretreatment data, blood flow in the left MCA of the benefit group showed habituation to stimulation, in significant contrast with the non-benefit group, which showed steady increase of blood flow velocity during stimulation.
Cerebrovascular response in migraineurs during acupuncture treatment
Wallasch's group divided migraine patients into treatment arms for verum acupuncture (n = 18) and a sham (placebo acupuncture) control treatment (n = 17).[15] Patients had at least a 2-year history of migraine, based on ICHD-II criteria ca. 2004, with a mean duration of disease (with standard deviation) of 16.8 (11.2) years for the verum group and 18.5 (10.9) years for the placebo group. They had no healthy control subjects. Treatment (8 sessions) was applied once a week over 8 weeks. Verum acupuncture was bilateral, with acupoints selected from channel points – Hegu (LI4), Zusanli (ST36), Waiguan (3B5), Zulinqi (Gb41), Houxi (SI3), and Shenmai (UB62) – and local points – Baihui (Du20), Fengchi (GB20), Taiyang (ExHN5), Sizhukong (3B23), Taichong (LV3), and Taixi (K3). Needles were rotated manually to induce de qi sensation. This procedure is comparable to the acupuncture in Backer's study. Sham differed from verum by the points chosen (theoretically not acupoints) and the depth of needling (shallow), with no manual rotation after insertion. Needle retention and session were identical to verum. The sham procedure was uniform for all patients and sessions.
Cerebrovascular response was recorded before and after treatment by TCD directed to both MCAs of patients performing a Valsalva maneuver. Clinical response was assessed by changes in hours of headache per month and days with migraine, but had no set definition save for significance of change. No analysis was made between treatment responders and treatment non-responders. To probe dynamic cerebral autoregulation, cerebrovascular response was quantified by two ratios – one, by maximum end-diastolic flow acceleration [cerebrovascular Valsalva ratio (CVR)], taking the steepest slope of the end-diastolic flow velocity curve in the time shortly after Valsalva maneuver (maximal dV/dt); and the other, by the ratio [centroperipheral Valsalva ratio (CPVR)] of maximal dV/dt over maximal dP/dt, the corresponding peripheral blood pressure acceleration, also the corresponding steepest slope in the peripheral blood pressure curve.[16] Static cerebral autoregulation was assessed through vasotonus at rest, indicated by three measures – systolic flow velocity, mean flow velocity, and pulsatility index. Pulsatility index was defined as the ratio of the difference of systolic and diastolic flow velocities over mean flow velocity.
Clinical response to treatment was significant in the verum group, but mixed in the sham treatment group, in that the verum group, but not the sham treatment group, showed significantly reduced headache hours per month, while reduction in migraine days reached significance in both groups, albeit more so in the verum group. Hemodynamically, the CVR and CPVR decreased significantly after treatment in the verum group, while in the placebo acupuncture group, the decrease in both ratios did not reach significance. Both groups were comparable before treatment. Also, vasotonus showed no significant differences in comparing between groups and before/after treatment over all parameters.
Therapeutic and hemodynamic effects of “point-through-point” acupuncture on migraine
The largest study of the three, by Cai et al., compared migraine patients undergoing “point-through-point” acupuncture (n = 45) with patients treated by “normal needling” (n = 45).[17] In “point-through-point” acupuncture, needles are angled at one point in the direction of another, usually connecting the two. The points connected were: Taiyang (ExNH5) to Shuaigu (GB8), Toulinqi (GB15) to Zhengying (GB17), Shangxing (Du23) to Baihui (Du20), Naokong (GB19) to Fengchi (GB20), and Hegu (LI4) to Houxi (SI3). Needles were inserted at a 30° angle, followed by manual rotation at 3.3 Hz for 1 min; they were retained for 30 min. “Normal needling” inserts the needles vertically as per convention, with point selected from: A Shi points, Hegu (LI4), Sanyinjiao (SP6), Geshu (BL17), Weizhong (BL54); de qi was induced, with needle retention for 30 min. Treatment (15 sessions) was applied once daily for 15 days. Although the ICHD-II was not cited by the authors, the expressed criteria for patient diagnosis are mostly in line with IHCD-II criteria for migraine (with or without aura). No restriction on length of headache history was imposed. The shortest migraine history for an included patient was 3 months and the longest was 7 years. Only patients suffering moderate to severe headache were included – this level of headache is generally strong enough to hinder a patient from working. No healthy control subjects were used. There was no sham acupuncture control treatment. No stimulation protocol was used to gauge cerebrovascular response. No comparisons between responders and non-responders to treatment were made. The primary clinical measure – also used as the basis for classifying headache as light, moderate, or severe – was the Headache Cumulative Score, an aggregate sum of four sub-values representing headache frequency, headache duration, impact on lifestyle, and number of secondary symptoms. These scores are not readily comparable to other studies. Clinical response was defined as a 20% or greater reduction in the Headache Cumulative Score. TCD was used to record the maximum mean flow velocities of blood flow in both pairs of anterior cerebral artery (ACA), MCA, and PCA for patients at rest.
All clinical measures showed significant decrease in both groups. Also, both groups showed comparable numbers before treatment, but after treatment, significantly lower values were observed in the “point-through-point” group. The superior efficacy of “point-through-point” acupuncture (97.8% effective rate) to standard acupuncture (80% effective rate) was also reflected by TCD findings. The “point-through-point” group showed dramatically reduced (P < 0.01) maximum mean blood flow velocities in the left ACA, PCA, and both MCAs, and significantly reduced (P < 0.05) maximum blood flow velocity in the right ACA and PCA. Compared with “normal needling,” the blood flow velocities in the “point-through-point” group were significantly lower in all cerebral arteries except the right ACA. Reduction in blood flow velocity in all pairs of cerebral arteries was also found to be significant in the “normal needling” group. The effective rate of acupuncture, disregarding type, was found to be significantly higher for moderate headache (95.2%) than for severe headache (63%).
DISCUSSION
Dynamic versus static cerebral autoregulation and frequency of acupuncture treatment
The key hemodynamic finding of the reports discussed above is that acupuncture positively influences the cerebrovascular dysfunction of migraineurs in the interictal phase, affecting dynamic cerebral autoregulation – a conclusion reached by Wallasch, as his group noted that acupuncture may positively modulate the cerebrovascular response of migraine patients performing a Valsalva maneuver.[15] Bäcker noted similar findings in his pilot study on patient's cerebrovascular response to visual (flashing light) stimulation.[14] Wallasch also observed no significant changes in baseline blood flow variability (vasotonus) for patients at rest and, thus, concluded that acupuncture does not impact static cerebral autoregulation.[15] By contrast, Cai found that acupuncture (both “point-through-point” and “normal needling”) significantly reduced the maximum mean blood flow velocities in the cerebral arteries of patients at rest.[17] This suggests that acupuncture may even alter static cerebral autoregulation, as well. As a caveat, maximum mean blood flow velocity may not be as indicative of static cerebral autoregulation as the vasotonus measures used by Wallasch.
The primary factors accounting for this difference seem to be the intervals between each treatment and the number of sessions, where one (Wallasch) administered treatment on a weekly basis for 8 weeks while another (Cai) administered daily treatment for 15 days [Table 3]. Therefore, reducing the interval between successive applications of acupuncture may lead to cumulative efficacy for migraine. However, Cai's “normal needling,” which relies on A Shi points, and Wallasch's “verum acupuncture,” which uses channel and local points, share little overlap in point selection. This leaves open the possibility of another strong factor. Nonetheless, both forms incorporate induction of de qi and are otherwise similar – bilateral application, manual rotation, needles in place for 30 min after insertion. Hence, considering the inconclusive effects of point specificity for migraine, it is likely the impact from differences in point selection is minor.[5] Here, “point-through-point” acupuncture is left out of the comparison with “verum,” even though some acupoints are shared. The “point-through-point” method differs in that the needles are inserted at an angle to connect acupoints and showed stronger results than “normal needling.” It bears mention that differences in patient populations may well be another important factor. For example, the migraine histories of patients recruited by Wallasch are generally much longer than of those recruited by Cai.
Predictive value of TCD for clinical response to acupuncture
Another important finding is that TCD may have predictive value for clinical response to acupuncture as a diagnostic tool. Bäcker found that the cerebrovascular response profiles to visual stimulation, taken before and after the treatment period, of patients who benefited from acupuncture differed from those of patients who did not benefit. Both groups shared in the mean comparable headache frequency and intensity before treatment. After treatment, cerebrovascular profiles of the benefit group became similar to those of healthy controls, whereas pretreatment differences (stronger response to stimulation and slower habituation) showed differences compared to healthy controls, matching the clinical effect.
In contrast, patients who did not benefit exhibited a more exaggerated cerebrovascular response post treatment, leading Bäcker to conclude that the cerebrovascular dysfunction of non-responders to treatment may actually worsen from acupuncture therapy. Post facto analysis of pretreatment data during visual stimulation also found sufficient difference between the benefit group and non-benefit group to suggest the potential use of TCD in predicting the efficacy of acupuncture prior to application, although the small sample size of the study precludes firm assertion.[14] Here, TCD was applied asymmetrically to two cerebral arteries (left MCA and right PCA). The effects of acupuncture on blood flow patterns in the other cerebral arteries of migraine patients facing stimulation, such as flashing light, are unknown at such detail. Another study (Cai) noted that clinical response to treatment inversely correlated with severity of headache, but did not present a corresponding hemodynamic analysis.[17] Backer's results do not seem to depend on migraine severity.
Neither Cai nor Wallasch provided analysis of non-responders to treatment, so it is unclear what effect non-standard acupuncture (e.g., point-through-point) or increased frequency of treatment may have on this subset of patients. It is also not clear if TCD can detect similar differentiating factors in the cerebrovascular response to Valsalva maneuver or other stressing stimuli. Additionally, TCD is limited in reading depth, requires expertise to administer, and thus cannot immediately monitor blood flow. Not only are there difficulties with TCD in capturing spontaneous changes, but the details of microcirculation, blood composition, and oxygenation also escape detection.
Variation in clinical effects from different needling methods
The final finding of note is that different needling methods may yield varying degrees of effectiveness, considering the more pronounced positive effects, observed both clinically and hemodynamically, of “point-through-point” acupuncture over “normal needling” techniques for treating migraine.[17] This suggests that the direction of needles during insertion may affect the effectiveness of an acupuncture treatment. This is not a new idea.[18] Unfortunately, differences in clinical measures prevent direct comparison with the standard acupuncture of Wallasch or Bäcker. But provided that point specificity has little correlation to the effectiveness of acupuncture treatment for migraine, “normal needling” may be comparable. Cai did not implement a sham acupuncture control, so placebo factors were unaccounted for. The sham treatment in the Wallasch study, applied weekly, was found to have a positive, but under-significant effect. It is unknown whether any positive effects might accrue from daily applied sham acupuncture. Further studies are required to confirm the clinical superiority of “point-through-point” acupuncture over standard acupuncture for migraine prophylaxis and to investigate needling angles as a significant parameter in acupuncture effectiveness.
Study limitations
The findings mentioned above need to be confirmed by additional studies. Our cross-study comparisons suffer from lack of uniform clinical and hemodynamic measures, potentially significant differences in patient populations (such as length of migraine histories and diagnostic criteria), variations in acupuncture treatment, and low statistical power from the relatively small numbers of study participants. Additionally, none of the reviewed studies investigated migraine during the ictal phase, i.e. none investigated either acupuncture as an abortive treatment or the effects of prophylactic acupuncture on the ictal state. Furthermore, primary hemodynamic data were restricted to blood flow velocities in the cerebral arteries within a limited time frame, such that high-resolution tissue-level details over large temporal and spatial windows were missed.
Recommendations for study design
Patient recruitment, diagnosis, and numbers should follow international randomized control trial standards. Analysis distinguishing positive from negative response to treatment within the treated populations may be able to identify possible predictors of clinical response or profiles of patients who should not receive acupuncture. Interventions for comparison should include at least one clearly documented form of acupuncture, standard drug therapy reflecting best current practice, and placebo controls including at least one clearly documented sham acupuncture and a placebo drug. A session of acupuncture can be viewed as a dose unit, where details of point selection, method of de qi induction, and needling methods (including angle of insertion), among others, are included in the description of a dose. Such perspective is justified considering the neural mechanisms identified with acupuncture.[19]
A variety of well-defined clinical and hemodynamic measures, based on earlier work and present priorities, should be used to facilitate any cross-study analyses down the road. Also, the use of TCD is generally limited to interictal studies, which may resort to a stressful stimulus protocol to simulate events during migraine attack. A technology, such as NIRS, which can monitor blood flow in real time and is easy to administer, can fill many of the gaps left open by TCD, such as reading of microcirculation and oxygenation changes at the tissue level. This type of continuous monitoring also provides a way to observe changes during the ictal phase of migraine, as well as offers an objective measure of acupuncture as a potential abortive treatment.
CONCLUSION
Acupuncture was found to positively influence cerebral autoregulation by varying degrees, during the interictal phase of migraine, depending on the dose intervals between sessions of acupuncture. The clinical effectiveness of an acupuncture treatment also depends on the needling technique, possibly more on needling angles and induction of de qi, than on point specificity. TCD was instrumental, but other tools, such as NIRS, should be considered to refine the findings. The scarcity of studies covered in this review indicates a need for further investigations into the cerebral hemodynamics of migraine and acupuncture. Such studies should ideally be medium to large scale, prospective, randomized, controlled, placebo controlled, and double blinded.
ACKNOWLEDGMENT
We would like to thank Lin-Chun Chiu for his efforts in gathering and organizing information for this article. The research is support by NTU grant: Aim For Top University Program 102R-7620.
REFERENCES
- 1.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders. Cephalalgia. (2nd ed) 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 2.WHO, Lifting the Burden. Atlas of headache disorders and resources in the world 2011. World Health Organization. 2011. [Last accessed on 2013 Sep 12]. p. 72. Available from: http://www.who.int/mental_health/management/atlas_headache_disorders/en/
- 3.The Global Burden of Disease: Generating Evidence, Guiding Policy. Seattle WA: 2013. Institute for Health Metrics and Evaluation. [Google Scholar]
- 4.Frass M, Strassl RP, Friehs H, Müllner M, Kundi M, Kaye AD. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: A systematic review. Ochsner J. 2012;12:45–56. [PMC free article] [PubMed] [Google Scholar]
- 5.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;1 doi: 10.1002/14651858.CD001218.pub2. CD001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang CP, Chang MH, Liu PE, Li TC, Hsieh CL, Hwang KL, et al. Acupuncture versus topiramate in chronic migraine prophylaxis: A randomized clinical trial. Cephalalgia. 2011;31:1510–21. doi: 10.1177/0333102411420585. [DOI] [PubMed] [Google Scholar]
- 7.Ambrósio EM, Bloor K, MacPherson H. Costs and consequences of acupuncture as a treatment for chronic pain: A systematic review of economic evaluations conducted alongside randomised controlled trials. Complement Ther Med. 2012;20:364–74. doi: 10.1016/j.ctim.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Bäcker M, Grossman P, Schneider J, Michalsen A, Knoblauch N, Tan L, et al. Acupuncture in migraine: Investigation of autonomic effects. Clin J Pain. 2008;24:106–15. doi: 10.1097/AJP.0b013e318159f95e. [DOI] [PubMed] [Google Scholar]
- 9.Chae Y, Chang DS, Lee SH, Jung WM, Lee IS, Jackson S, et al. Inserting needles into the body: A meta-analysis of brain activity associated with acupuncture needle stimulation. J Pain. 2013;14:215–22. doi: 10.1016/j.jpain.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Otti A, Noll-Hussong M. Acupuncture-induced pain relief and the human brain's default mode network-an extended view of central effects of acupuncture analgesia. Forsch Komplementärmed. 2012;19:197–201. doi: 10.1159/000341928. [DOI] [PubMed] [Google Scholar]
- 11.Huang W, Pach D, Napadow V, Park K, Long X, Neumann J, et al. Characterizing acupuncture stimuli using brain imaging with FMRI – a systematic review and meta-analysis of the literature. PLoS One. 2012;7:e32960. doi: 10.1371/journal.pone.0032960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hori E, Takamoto K, Urakawa S, Ono T, Nishijo H. Effects of acupuncture on the brain hemodynamics. Auton Neurosci. 2010;157:74–80. doi: 10.1016/j.autneu.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Yamaguchi S, Araki N. The practical use of acupuncture and moxibustion treatment cooperated with neurological practice. Rinsho Shinkeigaku. 2012;52:1287–9. doi: 10.5692/clinicalneurol.52.1287. [DOI] [PubMed] [Google Scholar]
- 14.Backer M, Hammes M, Sander D, Funke D, Deppe M, Tolle TR, et al. Changes of cerebrovascular response to visual stimulation in migraineurs after repetitive sessions of somatosensory stimulation (acupuncture): A pilot study. Headache. 2004;44:95–101. doi: 10.1111/j.1526-4610.2004.04017.x. [DOI] [PubMed] [Google Scholar]
- 15.Wallasch TM, Weinschuetz T, Mueller B, Kropp P. Cerebrovascular response in migraineurs during prophylactic treatment with acupuncture: A randomized controlled trial. J Altern Complement Med. 2012;18:777–83. doi: 10.1089/acm.2011.0308. [DOI] [PubMed] [Google Scholar]
- 16.Wallasch TM, Beckmann P, Kropp P. Cerebrovascular reactivity during the Valsalva maneuver in migraine, tension-type headache and medication overuse headache. Funct Neurol. 2011;26:223–7. [PMC free article] [PubMed] [Google Scholar]
- 17.Cai YY, Wang S. Therapeutic effect of point-through-point acupuncture on migraine and its effects on brain blood flow velocity. Zhongguo Zhen Jiu. 2006;26:177–9. [PubMed] [Google Scholar]
- 18.Fan GQ, Zhao Y, Fu ZH. Acupuncture analgesia and the direction, angle and depth of needle insertion. Zhongguo Zhen Jiu. 2010;30:965–8. [PubMed] [Google Scholar]
- 19.Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008;85:355–75. doi: 10.1016/j.pneurobio.2008.05.004. [DOI] [PubMed] [Google Scholar]


