Abstract
Objectives
Research suggests that the strength of the relationship between body image and emotional distress decreases with age. Past research has focused on expected aging-related body changes, and has not yet examined unexpected body changes (e.g. breast cancer surgery). The present post-hoc study assessed relationships between age, body image, and emotional distress in women facing breast cancer surgery.
Methods
Older (≥65 years, n=40) and younger (<65 years, n=40) women were matched on race/ethnicity, marital status, and surgery type. Within one week prior to surgery, participants completed measures of demographics, aspects of body image, and emotional distress (general and surgery-specific).
Results
Results indicated that: (1) body image did not differ by age (p > .999); (2) older women reported less pre-surgical emotional distress than younger women (p’s < .01); and, (3) age moderated the relationship between body image and emotional distress (p’s < .06).
Significance of Results
The results suggest that younger women, particularly those with poor body image, are at an increased risk for pre-surgical emotional distress. These women may benefit from pre-surgical interventions designed to improve body image or to reduce pre-surgical emotional distress.
Keywords: Breast cancer, surgery, body image, emotional distress
Introduction
Research has examined the relationship between a woman’s body image and emotional distress over the lifespan. The results have found that: (1) body image remains relatively stable over the course of a lifetime (Tiggemann, 2004); and, (2) poor body image is associated with emotional distress (Cash et al., 2004; Paxton et al., 2006). In addition, initial evidence suggests an interaction between body image and age in predicting some aspects of emotional distress (i.e., self-esteem) (Webster & Tiggemann, 2003; Tiggemann, 2004).
This research has focused almost exclusively on expected body changes associated with aging. However, women of all ages can be faced with unexpected body changes. One of the most common, yet often unexpected threats to a woman’s body is breast cancer. An estimated 1 in 8 women will be diagnosed with breast cancer, and the vast majority of these women will undergo body altering surgical treatment (American Cancer Society, 2011). Not surprisingly, women often endure heightened emotional distress before breast cancer surgery (e.g. Schnur et al., 2008). It is unknown, however, how a woman’s age and her body image jointly contribute to her experience of emotional distress prior to breast cancer surgery.
The current study conducted secondary data analyses to: (1) compare body image between older and younger women facing breast cancer surgery; (2) compare pre-surgical emotional distress between older and younger women; and, (3) examine whether age moderates the relationship between body image and pre-surgery emotional distress.
Materials and methods
Participants
The data for this study was collected as part of a larger study investigating predictors of breast cancer surgery outcomes. Participants (n=80) for this secondary data analysis were women scheduled for breast cancer surgery. Forty of the patients were aged 65 and over, and the other forty were aged 64 and under. The decision to divide the groups at age 65 is consistent with the National Institute of Aging and US Census Bureau report 65+ in the United States (He et al., 2005). The mean age was 47.8 (SD = 10.7) for the younger group and 71.9 (SD = 6.0) for the older group. These 2 groups were matched on marital status, race/ethnicity, and surgery type (mastectomy, lumpectomy, excisional breast biopsy). These matching factors were chosen because they have previously been found to be associated with body image [marital status (King, et al., 2000); race/ethnicity (Wildes et al., 2001); and surgery type (Collins et al., 2011)]. Eligibility criteria included: age 18 years or older, English speaking, and scheduled for breast cancer surgery. Exclusion criteria included: current uncontrolled mental illness. The 2 age groups did not differ significantly in terms of body mass index (p > .90). See table 1 for demographic and medical information.
Table 1.
Participant demographics and medical information
| Demographics/Medical Information | N (%) |
|---|---|
| Surgery type | |
| Excisional biopsy | 28 (35%) |
| Lumpectomy | 24 (30%) |
| Mastectomy | 28 (35%) |
| Race/Ethnicity | |
| White, non-Hispanic | 68 (85%) |
| White, Hispanic | 4 (5%) |
| Black, non-Hispanic | 4 (5%) |
| Other | 4 (5%) |
| Marital Status | |
| Never married | 14 (17.5%) |
| Currently married | 46 (57.5%) |
| Separated | 2 (2.5%) |
| Divorced | 6 (7.5%) |
| Widowed | 12 (15%) |
Measures
Demographic/medical information was assessed via self-report questionnaire and medical chart review. Aspects of body image were assessed using items from the Additional Concerns section of the Functional Assessment of Cancer Therapy – Breast scale (FACT-B, version 4). Participants were asked to rate how true 2 statements had been for them since their surgery was scheduled. The items read: “I feel sexually attractive,” and “I am able to feel like a woman” (Brady et al., 1997). These 2 items have been used in other body image and breast cancer research (Arora et al., 2001). Items were rated on a 5-point Likert scale (0=Not at all; 4=Very much). The correlation between the 2 items was .44 (p < .001).
Two measures of general emotional distress were used. The first was the Short Version –Profile of Mood States (SV-POMS). The SV-POMS is a 37-item self-report measure which assessed level of mood disturbance over the past week (Shacham, 1983). Previous research has found the SV-POMS to have good internal consistency and validity with breast cancer patients (DiLorenzo et al., 1999). In the current sample, Cronbach’s alpha was .95. The second general emotional distress measure was a Visual Analog Scale (VAS) item (0–100 mm) that asked: “Right now, how emotionally upset do you feel?” The scale was anchored by “not at all upset” and “as upset as I could be.” Visual analog scales have previously been used with breast cancer surgery patients (e.g. Schnur et. al, 2008).
Surgery-specific distress was measured using the Impact of Events Scale – Intrusion subscale (IES-Intrusion) (Horowitz et al., 1979). The 7-item subscale asked the frequency of surgery-specific intrusion symptoms over the last month. Items were rated on a 4-point Likert scale, ranging from “not at all” to “often”. The IES has previously been used with breast cancer surgery patients (Tjemsland et al., 1997; Schnur et al., 2008). In the current sample, Cronbach’s alpha was .90.
Procedure
Patients scheduled for breast cancer surgery were referred to the study by their surgeon. Consenting participants completed the demographics questionnaire at home 5 days before surgery. On the day of surgery (prior to surgery) all participants completed the FACT-B body image items, the SV-POMS, the IES-Intrusion scale, and the VAS emotional upset item.
Results
Aim 1 analyses (see Table 2) revealed that older adults did not differ significantly from younger adults in terms of body image (p > .999) prior to surgery. Aim 2 analyses revealed that older adults did however report significantly lower levels of both general distress (SV-POMS, p < .001; VAS, p <.001) and surgery-specific distress (IES-Intrusion, p < .01) than younger adults. Aim 3 results indicated that the relationship between body image and pre-surgery emotional distress differed by age group. Using a regression approach, body image, age (<65 or ≥65), and an interaction term (Body Image x Age) were entered as predictors of surgery-specific distress (IES-Intrusion) and of general distress (VAS, SV-POMS) separately. The regression to predict IES-Intrusion revealed that both body image (F (1, 76) = 4.67, p < .05) and age group (F (1, 76) = 12.72, p < .01) uniquely predicted surgery-specific distress, as did the interaction term (F (1, 76) = 7.30, p < .01) (Total model R2 = .20). The regression to predict VAS distress revealed that both body image (F (1, 76) = 13.40, p < .01) and age group (F (1, 76) = 13.22, p < .01) uniquely predicted general distress, as did the interaction term (F (1, 76) = 6.09, p < .05) (Total model R2 = .29). The regression analysis to predict SV-POMS distress revealed that both body image (F (1, 76) = 10.33, p < .01) and age group (F (1, 76) = 11.62, p < .01) uniquely predicted general distress, and the interaction term approached significance (F (1, 76) = 3.59, p =.06) (Total model R2 =.31). To better understand the interactions, we plotted the effects for each of the dependent variables (see Figure 1). For younger women, poor body image was related to increased general and surgery-specific pre-surgery distress. For older women, distress and body image were not significantly related.
Table 2.
Mean body image and emotional distress scores by age group
| Older Adults (≥ 65 years) (n = 40) Mean (SD) |
Younger Adults (< 65 years) (n = 40) Mean (SD) |
F | df | p | d | 95% CI | |
|---|---|---|---|---|---|---|---|
| Body Image score | 5.13 (2.17) | 5.13 (1.81) | 0.00 | (1,78) | 0.999 | 0 | −0.44, 0.44 |
| SV-POMS total mood disturbance score (general distress) | 0.31 (.51) | 0.89 (.69) | 18.83 | (1,78) | <0.001 | 0.96 | 0.49, 1.42 |
| Visual Analog Scale score (general distress) | 29.08 (27.31) | 53.48 (35.72) | 11.78 | (1,78) | 0.001 | 0.77 | 0.31, 1.22 |
| IES – Intrusion score (surgery-specific distress) | 8.98 (8.34) | 14.83 (10.31) | 7.78 | (1,78) | 0.007 | 0.62 | 0.18, 1.07 |
Note: SV-POMS = Short Version - Profile of Mood States, IES = Impact of Events Scale. Higher body image scores indicate more positive body image.
Figure 1.
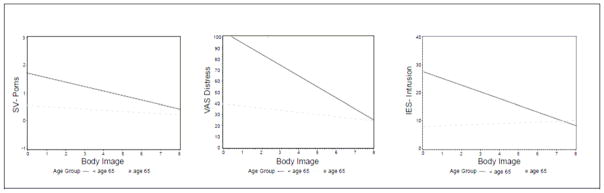
Age by body image interactions in predicting general (SV-POMS and VAS Distress) and surgery-specific (IES-Intrusion) distress.
Discussion
This study yielded 3 primary findings. First, older and younger women had equivalent levels of body image prior to breast cancer surgery. This is consistent with the general body image literature, which has demonstrated that body image tends to remain stable throughout the lifespan (Tiggemann, 2004). Second, relative to older women, younger women had significantly greater levels of pre-surgical emotional distress. This is consistent with the larger breast cancer literature which has found that younger women with breast cancer experience greater levels of emotional distress, when compared to their older counterparts (Mosher & Danoff-Burg, 2005). Third, younger women with poor body image experience heightened emotional distress in the face of breast cancer surgery, while older women, and younger women with better body image, seem to approach breast cancer surgery with less emotional distress. Although a similar interaction effect has been found in the general body image literature (Tiggemann, 2004), the present study is the first to examine this relationship in women facing immediate, potentially disfiguring changes to their bodies.
There are limitations to the present study that should be considered when interpreting the results. First, the body image measure that was used focused on 2 specific areas of body image (i.e., perceptions of sexual attractiveness and femininity) rather than measuring body image as a multi-dimensional construct. Future research should replicate this study with a more comprehensive body image measure. Second, the current study exclusively focused on women undergoing breast cancer surgery. Future research should examine the unique interactions between body image, age, and emotional distress with regard to other body-altering cancer treatments (e.g. chemotherapy).
Conclusions
Overall, this study can inform clinical care of women facing breast cancer surgery. The results of the present study suggest that younger women, particularly those with poor body image, are at an increased risk for pre-surgical emotional distress. These women may benefit from pre-surgical interventions designed to improve body image (e.g. cognitive behavioral therapy) (Rosen et al., 1989) or to reduce pre-surgical emotional distress (Montgomery et al., 2007). Drawing from our assessment items, interventions that target perceptions of femininity and sexual attractiveness may be particularly therapeutic.
Acknowledgments
Preparation of this manuscript was supported by the National Cancer Institute (K07CA131473; R25CA129094; R25CA081137; R03CA159530). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
References
- American Cancer Society. Breast cancer facts & figures 2011–2012. Atlanta: American Cancer Society, Inc; 2011. [Google Scholar]
- Arora NK, Gustafson DH, Hawkins RP, McTavish F, Cella DF, Pingree S, Mahvi DM. Impact of surgery and chemotherapy on the quality of life of younger women with breast carcinoma: A prospective study. Cancer. 2001;92(5):1288–1298. doi: 10.1002/1097-0142(20010901)92:5<1288::aid-cncr1450>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, Shiomoto G. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 1997;15(3):974–986. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- Cash TF, Theriault J, Annis NM. Body image in an interpersonal context: Adult attachment, fear of intimacy, and social anxiety. Journal of Social and Clinical Psychology. 2004;23(1):89–103. [Google Scholar]
- Collins KK, Liu Y, Schootman M, Aft R, Yan Y, Dean G, Jeffe DB. Effects of breast cancer surgery and surgical side effects on body image over time. Breast Cancer Research and Treatment. 2011;126(1):167–176. doi: 10.1007/s10549-010-1077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiLorenzo TA, Bovbjerg DH, Montgomery GH, Valdimarsdottir H, Jacobsen PB. The application of a shortened version of the Profile of Mood States in a sample of breast cancer chemotherapy patients. British Journal of Health Psychology. 1999;4:315–325. [Google Scholar]
- He W, Sengupta M, Velkoff VA, DeBarros KA. 65+ in the United States: 2005. U.S. Department of Health and Human Services & U.S. Department of Commerce; 2005. [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- King MT, Kenny P, Shiell A, Hall J, Boyages J. Quality of life months and one year after first treatment for early stage breast cancer: Influence of treatment and patient characteristics. Quality of Life Research. 2000;9(7):789–800. doi: 10.1023/a:1008936830764. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Bovbjerg DH, Schnur JB, David D, Goldfarb A, Weltz CR, Silverstein JH. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. Journal of the National Cancer Institute. 2007;99(17):1304–1312. doi: 10.1093/jnci/djm106. [DOI] [PubMed] [Google Scholar]
- Mosher CE, Danoff-Burg S. A review of age differences in psychological adjustment to breast cancer. Journal of Psychosocial Oncology. 2005;23(2–3):101–114. doi: 10.1300/j077v23n02_07. [DOI] [PubMed] [Google Scholar]
- Paxton SJ, Neumark-Sztainer D, Hannan PJ, Eisenberg ME. Body dissatisfaction prospectively predicts depressive mood and low self-esteem in adolescent girls and boys. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2006;35(4):539–549. doi: 10.1207/s15374424jccp3504_5. [DOI] [PubMed] [Google Scholar]
- Rosen JC, Saltzberg E, Srebnik D. Cognitive behavior therapy for negative body image. Behavior Therapy. 1989;20:393–404. [Google Scholar]
- Schnur JB, Montgomery GH, Hallquist MN, Goldfarb AB, Silverstein JH, Weltz CR, Bovbjerg DH. Anticipatory psychological distress in women scheduled for diagnostic and curative breast cancer surgery. International Journal of Behavioral Medicine. 2008;15(1):21–28. doi: 10.1007/BF03003070. [DOI] [PubMed] [Google Scholar]
- Shacham S. A shortened version of the Profile of Mood States. Journal of Personality Assessment. 1983;47(3):305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- Tiggemann M. Body image across the adult life span: Stability and change. Body Image. 2004;1(1):29–41. doi: 10.1016/S1740-1445(03)00002-0. [DOI] [PubMed] [Google Scholar]
- Tjemsland L, Soreide JA, Matre R, Malt UF. Pre-operative [correction of properative] psychological variables predict immunological status in patients with operable breast cancer. Psycho-Oncology. 1997;6(4):311–320. doi: 10.1002/(SICI)1099-1611(199712)6:4<311::AID-PON285>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- Webster J, Tiggemann M. The relationship between women’s body satisfaction and self-image across the life span: The role of cognitive control. The Journal of Genetic Psychology. 2003;164(2):241–252. doi: 10.1080/00221320309597980. [DOI] [PubMed] [Google Scholar]
- Wildes JE, Emery RE, Simons AD. The roles of ethnicity and culture in the development of eating disturbance and body dissatisfaction: A meta-analytic review. Clinical Psychology Review. 2001;21(4):521–551. doi: 10.1016/s0272-7358(99)00071-9. [DOI] [PubMed] [Google Scholar]


