Abstract
Objective
Assess the Regional Extension Center (REC) program’s progress toward its goal of supporting over 100,000 providers in small, rural, and underserved practices to achieve meaningful use (MU) of an electronic health record (EHR).
Data Sources/Study Setting
Data collected January 2010 through June 2013 via monitoring and evaluation of the 4-year REC program.
Study Design
Descriptive study of 62 REC programs.
Data Collection/Extraction Methods
Primary data collected from RECs were merged with nine other datasets, and descriptive statistics of progress by practice setting and penetration of targeted providers were calculated.
Principal Findings
RECs recruited almost 134,000 primary care providers (PCPs), or 44 percent of the nation’s PCPs; 86 percent of these were using an EHR with advanced functionality and almost half (48 percent) have demonstrated MU. Eighty-three percent of Federally Qualified Health Centers and 78 percent of the nation’s Critical Access Hospitals were participating with an REC.
Conclusions
RECs have made substantial progress in assisting PCPs with adoption and MU of EHRs. This infrastructure supports small practices, community health centers, and rural and public hospitals to use technology for care delivery transformation and improvement.
Keywords: Health information technology, electronic health records, meaningful use, practice transformation, primary care providers
Health information technology (health IT) is foundational to the pursuit of the three-part aim of achieving better care, better health, and reducing costs (Berwick, Nolan, and Whittington 2008; Buntin, Jain, and Blumenthal 2010). Despite the potential benefits of health IT, adoption of electronic health records (EHRs) has been slow (Blumenthal 2010). In 2008, only 8 percent of hospitals (Jha et al. 2010) and 13 percent of physicians practicing in ambulatory settings had adopted at least a basic EHR (DesRoches et al. 2008). Small practices and critical access hospitals (CAHs) historically have lower rates of EHR adoption (Mostashari, Tripathi, and Kendall 2009), raising concerns of a “digital divide” in access to health IT among rural and underserved populations.
The Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 spurred the adoption of health IT by offering financial incentives and technical assistance for the adoption and meaningful use (MU) of EHRs as well as the exchange of health information (Blumenthal 2010). HITECH appropriated $2 billion to Office of the National Coordinator (ONC) for health IT, and the Secretary of Health and Human Services delegated authority to ONC to establish the health IT Regional Extension Center (REC) program. The $720 million REC program was designed to provide assistance and information on best practices to accelerate efforts to adopt and optimize the use of EHR technology to improve the quality and value of the health care delivery system. The fundamental goal of the REC program was to assist at least 100,000 providers with the technical and organizational barriers encountered during health IT implementation and optimization (Blumenthal 2011a). Main implementation tasks included needs assessment, product selection, and assistance with the project management involved in installing an EHR system (Maxson et al. 2010). Two prior extension programs that supported EHR adoption in ambulatory care demonstrated that practice needs vary widely, particularly with regards to optimizing health IT for quality improvement (Mostashari, Tripathi, and Kendall 2009), and there may be a need for extensive outreach (Samantaray et al. 2011) and sustained technical assistance, practice facilitation, and practice coaching, particularly in small under-resourced physician practices (Ryan et al. 2013).
Many practices lack the resources to manage the business and practice changes needed to improve care by optimizing health IT (Crabtree et al. 2011), so practices that had already adopted EHRs were also eligible for REC assistance with optimization. Practice coaching aims to “train the trainer” and help practices and CAHs build adaptive reserve (Nutting et al. 2009) and capacity for learning and change management, to reduce practice disruption and fatigue (Nutting et al. 2011; Grumbach, Bainbridge, and Bodenheimer 2012). Practice facilitation and coaching help providers improve care (Nagykaldi, Mold, and Aspy 2005) and implement evidence-based guidelines (Baskerville, Liddy, and Hogg 2012).
This article describes the REC program’s success in reaching the 100,000 targeted providers in the first 3 years of the program, as well as the progress of REC-participating providers in adopting and meaningfully using EHRs.
Regional Extension Center (REC) Program
The REC program was funded first to assist priority providers that serve underserved populations to prevent a widening of the digital divide, then to serve as a national infrastructure to disseminate best practices throughout the health care system (Maxson et al. 2010; Blumenthal 2011a). Priority REC providers include those in small practices, community health centers, and rural and public hospitals (HITECH 2009).
In 2010, ONC awarded 62 cooperative agreements to 60 local organizations to support the adoption of EHRs and demonstration of MU, with additional supplemental awards to further assist rural and CAHs (see Appendix SA2A for program launch details). A diverse group of existing and some newly formed not-for-profit organizations with expertise in EHR adoption received REC funding, including health IT research and consulting organizations, universities, quality improvement organizations, and health center controlled networks. RECs were awarded support largely on the size of the provider population they sought to support, ranging from 525 to 6,000 providers and monetary awards averaging $11.6 million, ranging from $4.5 to $29.9 million. Building on the lessons from previous extension services in agriculture (Birkhaeuser, Evenson, and Feder 1991; Umali-Deininger, Umali, and Schwartz 1994) and manufacturing (Oldsman 1996; Hallacher 2005), flexibility was built into the REC program. REC grantees were allowed to leverage existing provider networks by subcontracting and partnering with other organizations such as state and local medical societies, independent provider associations (IPAs), and hospital referral networks. The main activities undertaken by RECs were tailored to address barriers and local market conditions of targeted providers in three domains: technical, organizational, and economic (Blumenthal 2011a).
Regional Extension Center grantees were supported by four main knowledge management and business intelligence (BI) tools. The Health Information Technology Research Center (HITRC) online learning portal provided access to tools and resources for REC staff, supporting rapid-cycle spread of innovative approaches to challenges faced by RECs and enrolled providers. The Learning Management System (LMS) provided online training to REC staff on key issues such as vendor selection, workflow redesign, and project management. The online Customer Relationship Management (CRM) tool enabled RECs to track provider progress on programmatic milestones. Finally, the National Learning Consortium (NLC) facilitated communities of practice among REC grantees, to disseminate best practices and support discussions about optimizing the use of health IT.
Methods
Primary Data Collection
Administrative data from the REC program’s Customer Relationship Management (CRM) database were merged with nine other data sources to construct the analytic file used in this study. To receive reimbursement from ONC, RECs were required to submit data to the CRM on demographics and practice characteristics of enrolled providers, in addition to progress on three major milestones: enrollment with the REC program, implementation of an EHR (“go live”), and demonstration of MU (ONC 2013). Enrollment counts included only active providers and facilities, excluding those that had disenrolled.1
As of July 2013, there were over 1,200 CRM users and more than 1.7 million data elements across all 62 RECs. The train-the-trainer model was used to support CRM end users, with two CRM Leads designated at each REC attending regular webinars and in-person meetings. ONC’s BI team conducted regular validation activities to detect data outliers and inconsistencies, requesting further clarification from RECs where necessary. In response to evolving REC operational needs, a Change Advisory Board comprised of five REC leads and three ONC staff processed requests for CRM improvements, and tested new functionalities before introducing system-wide changes. The CRM also contained optional capabilities used by some RECs, including project management, provider outreach management, and the ability to track specific challenges practices are facing as they work towards achieving MU. This ability to track challenges faced by REC-enrolled providers in primary, secondary, and tertiary categories was added in response to REC grantees’ requests for tools to identify and track barriers related to health IT adoption and MU.
Secondary Data Sources
Nine additional datasets were used in this study: four from the Centers for Medicare and Medicaid Services (CMS), three from the Health Resources and Services Administration (HRSA), one from The Flex Monitoring Team university consortium, and a dataset collected by SK&A Information Services (details available in Appendix SA2D). Additional data sources were merged with the CRM to add information on urban/rural characteristics, whether the area was medically underserved, provider and practice characteristics, and whether providers were participating in EHR Incentive Programs and delivery system transformation programs. The 2011 and 2012 Area Resource File (ARF) datasets were used to designate providers as urban or rural, based on practice zip code (HRSA Bureau of Health Professions, 2011 and 2012). Locations were coded as rural if the Core Based Statistical Area was designated as Micropolitan or Small Rural and as urban if the area type was Metropolitan. HRSA designates areas as Primary Care Health Professional Shortage Areas (HPSAs) if there are more than 3,500 patients per primary care physician, and for this study county-level designations were used; HPSA designations listed in the ARF are current as of 2010 (HRSA Bureau of Health Professions, 2011 and 2012).
When enrolling new practices, RECs assigned practice setting based on definitions specified in the REC program funding opportunity announcement. ONC reimbursement was only available for providers in settings defined as a priority within the announcement. These are provided in Appendix SA2B. ONC performed an additional level of matching to further identify practice settings as Federally Qualified Health Centers (FQHCs), using a list downloaded from the HRSA data warehouse (methods described in Heisey-Grove et al. 2013). The CMS Certified Hospital List (March, 2013) and a national CAH database maintained by The Flex Monitoring Team were used to identify CAHs and the Flex list was used as the universe of CAHs (Flex Monitoring Team 2012; method described in Heisey-Grove et al. 2012). RECs also provided assistance to small rural hospitals. ONC used HRSA’s Small Hospital Improvement Program list to identify rural hospitals with 50 beds or less.
The other data sources used in this study indicate whether the provider or facility participated in relevant CMS programs. Medicare and Medicaid CMS EHR Incentive Program attestation and payment data (current as of June 31, 2013) were used, as well as data from the Center for Medicare and Medicaid Innovation on participation in two initiatives: the Comprehensive Primary Care Initiative and the Medicare FQHC Advanced Primary Care Practice Demonstration (current as of August and September 2011 respectively; U.S. Department of Health and Human Services 2013b).
Analysis
Descriptive statistics were calculated in the aggregate as well as stratified by state, REC, urban/rural location, location in an HPSA, provider type, and practice setting. Penetration rates were calculated using REC enrollment data against the universe of providers and facilities from SK&A, the CMS Certified Hospital List for CAHs, and lists of small rural hospitals and FQHCs from HRSA. Analysis was executed with SAS, version 9.3 (SAS, Cary, NC, United States).
Results
As of June 2013, the REC program has exceeded its target of enrolling and assisting more than 100,000 primary care providers with adopting EHRs. RECs have enrolled a total of 133,922 PCPs across nearly 30,000 practices with enrollment ramping up in the third quarter of 2010 and continuing to increase steeply through 2011 (Figure 1). Around 80 percent of REC-enrolled PCPs (115,729 providers) had an EHR installed and were routinely using the technology. While some providers had an EHR installed before REC assistance commenced, almost all required system upgrades or requested a full EHR replacement to implement Certified EHR Technology (CEHRT) to reach MU. RECs support provider’s adoption of Certified EHR Technology and richer functionality of MU, including clinical quality reporting, e-prescribing and medication reconciliation to improve patient care and successfully demonstrate the MU stage 1 criteria. As of June 2013, almost 50 percent of all REC-PCPs had demonstrated MU of certified EHR technology. This proportion is expected to grow as the REC program pivots in the latter half of the program from the initial focus on outreach, enrollment, and EHR implementation to assisting providers with MU and using health IT for clinical transformation.
Figure 1.
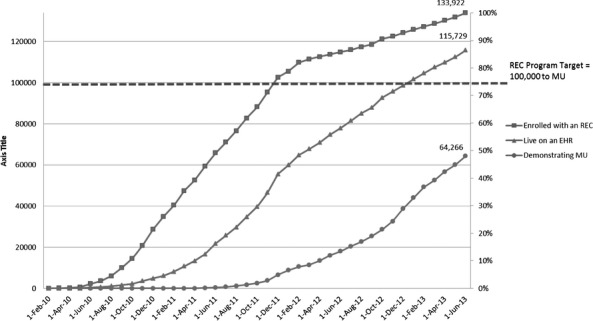
Cumulative Number and Proportion of REC Primary Care Providers Enrolled, Live on an EHR, and Demonstrating Meaningful Use over Time Source: Customer Relationship Management (CRM) Tool, maintained by Health and Human Services, Office of the National Coordinator for Health IT, data as of July 10, 2013.
Table 1 examines REC penetration by practice characteristics and practice setting. Nearly half of the nation’s 300,000 total PCPs were enrolled with an REC (44 percent), including 52 percent of rural PCPs (24,215 providers). Penetration into FQHC organizations and CAHs was even higher. Four in five FQHC and FQHC Look-Alikes had at least one provider enrolled with an REC (954 organizations, 83 percent). Over a thousand of the nation’s 1,327 CAHs were enrolled with an REC (78 percent). RECs were also involved in the national Center for Medicare and Medicaid Innovation practice transformation and delivery system redesign efforts, with 265 Comprehensive Primary Care Initiative sites (53 percent) participating with an REC. In addition, 409 of the Medicare FQHC Advanced Primary Care Practice Demonstration Programs were participating with an REC (82 percent).
Table 1.
Proportion of REC Providers and Practices in Key Demographic Categories and Practice Settings
| Providers | No. of Providers Enrolled with an REC* | Total No. of Providers Nationwide † | Proportion of Providers Enrolled with an REC (%) |
|---|---|---|---|
| Rural primary care providers‡ | 24,215 | 47,000 | 52 |
| Total primary care providers§ | 131,967 | 302,362 | 44 |
| Organizations | No. of Organizations Enrolled with an REC1 | Total No. of Organizations Nationwide | Proportion of Organizations Enrolled with an REC (%) |
|---|---|---|---|
| Federally qualified health center¶ | |||
| Look-alike grantees | 954 | 1,147 | 83 |
| Critical access hospitals∥ | 1,033 | 1,327 | 78 |
| Sites | No. of Sites Enrolled with an REC1 | Total No. of Sites Nationwide | Proportion of Sites Enrolled with an REC (%) |
|---|---|---|---|
| Comprehensive primary care initiative sites** | 265 | 503 | 53 |
| Advanced primary care initiative sites†† | 409 | 500 | 82 |
Note.
US Department of Health and Human Services, Office of the National Coordinator for Health Information Technology. Customer Relationship Management database, July 10, 2013.
SK&A Office-based Providers Database, SK&A Information Services 2011, Irvine, CA.
Rural areas defined using the Core Based Statistical Area Micropolitan and Small Rural designations in US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions2011. Area Resource File, 2011–2012. Rockville, MD. Primary Care Provider count includes physicians, NPs, and PAs. Community health aide practitioners and nurse midwives were excluded from the numerator because these counts are not available in the SK&A database.
Primary Care Provider count includes physicians, NPs, and PAs.
Federally Qualified Health Center (FQHC) universe and matching of FQHC grantees against REC-enrolled practices defined using the US Department of Health and Human Services, Health Resources and Services Administration2011. Data Warehouse. Rockville, MD.
Critical Access Hospital (CAH) denominator and matching of CAHs against REC-enrolled practices defined using the US Department of Health and Human Services, Centers for Medicare and Medicaid Services2013a. CMS Certified Hospital List. Baltimore, MD.
Comprehensive Primary Care Initiative (CPC) denominator and matching of CPC sites against REC-enrolled practices defined using the US Department of Health and Human Services, Centers for Medicare and Medicaid Services, Center for Medicare and Medicaid Innovation2011a. List of Comprehensive Primary Care Initiative sites, August 2011. Baltimore, MD.
Advanced Primary Care Initiative (APC) denominator and matching of APC sites against REC-enrolled practices defined using the US Department of Health and Human Services, Centers for Medicare and Medicaid Services, Center for Medicare and Medicaid Innovation2011b. List of FQHC Advanced Primary Care Practice Demonstration sites, November, 2011. Baltimore, MD.
The progress of REC-enrolled providers toward EHR adoption and MU varied across locations, practice settings, and provider types (Table 2). The progress of urban and rural PCPs appeared similar, with 86 percent and 87 percent live with an EHR, respectively, and 48 percent and 47 percent demonstrating MU. Primary care physicians in HPSAs were making slower progress, with 82 percent using EHR technology and 39 percent demonstrating MU.
Table 2.
Number of Primary Care Providers Enrolled by RECs and Proportion Live on an EHR and Demonstrating Meaningful Use, by Area Type, Practice Setting, and Provider Type*
| Area Type† | No. of Primary Care Providers Enrolled | Proportion Live on an EHR (%) | Proportion Demonstrating MU (%) |
|---|---|---|---|
| Urban | 109,109 | 86 | 48 |
| Rural | 24,522 | 87 | 47 |
| Primary care health professional shortage area (HPSA) | 3,202 | 82 | 39 |
| Practice Setting | No. of Primary Care Providers Enrolled | Proportion Live on an EHR (%) | Proportion Demonstrating MU (%) |
|---|---|---|---|
| Small primary care practice | 48,765 | 84 | 52 |
| Public hospital outpatient dept. or other underserved | 38,029 | 86 | 45 |
| Practice consortium | 20,183 | 90 | 58 |
| Federally Qualified Health Center‡ | 16,911 | 92 | 38 |
| Small Rural Hospital, Rural Health Clinic, or Critical Access Hospital§¶ | 10,034 | 82 | 37 |
| Total | 133,922 | 86 | 48 |
| Provider Type | No. of Primary Care Providers Enrolled | Proportion Live on an EHR (%) | Proportion Demonstrating MU (%) |
|---|---|---|---|
| Physician | 101,584 | 86 | 52 |
| Nurse practitioner | 20,437 | 86 | 35 |
| Physician assistant | 9,553 | 89 | 37 |
| Certified nurse midwife | 1,955 | 86 | 33 |
| Community health aide practitioner (Indian Health Service) | 393 | 97 | 0 |
| Total | 133,922 | 86 | 48 |
Note.
US Department of Health and Human Services, Office of the National Coordinator for Health Information Technology. Customer Relationship Management database, July 10, 2013.
Area types defined using the US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions. Area Resource File, 2011–2012. Rockville, MD.
Federally Qualified Health Center grantees matched against REC-enrolled practices using the US Department of Health and Human Services, Health Resources and Services Administration. Data Warehouse. Rockville, MD.
Critical Access Hospitals matched against REC-enrolled practices defined using the US Department of Health and Human Services, Centers for Medicare and Medicaid Services. CMS Certified Hospital List. Baltimore, MD.
Rural Hospitals matched against REC-enrolled practices defined using the US Department of Health and Human Services, Health Resources and Services Administration, Office of Rural Health Policy2012. Small Rural Hospital Improvement Program list, 2012. Rockville, MD. Formerly available at: http://www.hrsa.gov/ruralhealth/about/hospitalstate/index.html.
Almost 49,000 primary care providers in small practices were enrolled with an REC, and 84 percent were live with an EHR. An additional 20,183 PCPs in practice consortiums were participating, and 90 percent were using an EHR. Robust progress to MU was seen among providers in small primary care practices and practice consortiums; 52 and 58 percent had demonstrated MU, respectively. Over 90 percent of FQHC providers participating with an REC were live with an EHR (92 percent), and 38 percent had attained MU. Over 80 percent of REC-enrolled providers in other underserved settings were live with an EHR, including rural health clinics, CAHs and small rural hospitals, and public hospital outpatient departments. RECs were working with over 80 percent of FQHCs (Heisey-Grove et al. 2013) and 1,164 CAHs and rural hospitals (73 percent of all CAHs and 41 percent of all small rural hospitals; Heisey-Grove et al. 2012).
Of the PCPs supported by RECs, 101,584 were physicians, 20,437 were nurse practitioners, 9,553 were physician assistants, and 1,955 were certified nurse midwives. The proportion of providers live with an EHR ranged from 86 to 89 percent. Over half of REC-enrolled primary care physicians had attained MU (52 percent), while the proportion for nonphysician providers ranged from 33 percent for certified nurse midwives to 37 percent for physician assistants. Nearly 10,000 specialists from 38 different specialties were also enrolled in their local REC (data not shown).
Electronic health record adoption among REC-enrolled providers varied by state (Figure 2). EHR adoption rates exceeded 70 percent in 50 states and the District of Columbia. In 24 states and American Samoa, EHR adoption rates were 90 percent or above. See Appendix SA2C for adoption and MU milestones by state, as well as milestone achievement by each REC.
Figure 2.
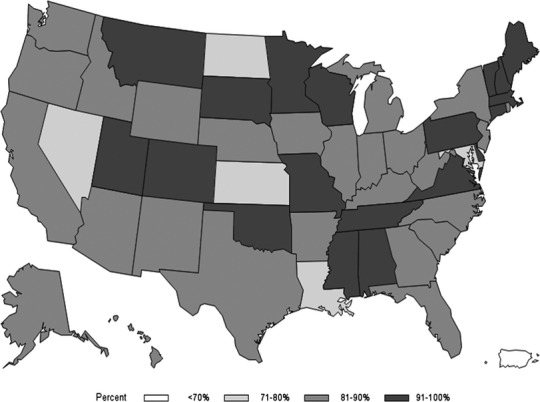
Proportion of REC-enrolled Primary Care Providers Live on an EHR Source: US Department of Health and Human Services, Office of the National Coordinator for Health Information Technology. Customer Relationship Management database, July 10, 2013.
Discussion
The REC program has made significant progress toward the HITECH goals of assisting primary care providers with the adoption and MU of EHRs. These findings indicate strong penetration of the REC program in outreach and enrollment, particularly among providers in rural and underserved settings (Samuel et al. 2013). Most REC-participating providers have adopted EHRs and nearly half have demonstrated MU. A recent study found providers working with RECs were 2.3 times more likely to have received incentive funds through Centers for Medicare and Medicaid Services’ EHR incentive program (U.S. Government Accountability Office 2012).
In meeting the REC program’s initial outreach and EHR adoption goals, significant challenges with changing local markets, diffusion of innovative practices, and coordination with partners were identified. In addressing these challenges, the REC program has relied on three foundational strategies: (1) responsiveness to the marketplace using adaptive BI, (2) developing infrastructure for rapid cycle improvement and diffusion of innovative practices and lessons from early adopters, and (3) partnerships and collaboration. Lessons learned from these strategies can inform policy interventions and future extension center and health care transformation initiatives in the United States and abroad.
Using BI Tools to Be Responsive to Local Markets
Regional Extension Centers used data collection via BI tools for situational awareness of local markets. BI allows RECs to develop targeted, locally relevant solutions to provider challenges, smoothing the transition to MU. Commonly reported challenges to MU included incorporating the Clinical Summary into practice workflow; EHR template issues; provider resistance; making accommodations for non-English speakers; and additional printing and mailing expenses. BI tools create a systematic way to track and respond to challenges faced by these diverse providers. Through this process, providers reported the Clinical Summary requirement to be one of the most challenging MU measures, impacting providers across all practice settings. Using BI, resources and tools were tested, revised, and disseminated among all RECs, then made publically available on HealthIT.gov. As new challenges emerge, systematic data collection and analytics help preempt large-scale issues with timely interventions, adaptable to local organizational and cultural needs. This aggregation of issues and dissemination of resources using BI can increase the adaptive reserves of individual practices and REC staff supporting their efforts (Nutting et al. 2009).
Infrastructure for Diffusion of Innovative Practices Using Knowledge Management and Learning Collaboration
RECs utilized real-time performance monitoring and multimodal situational awareness to guide and inform the program, as well as support the diffusion process. Communities of practice utilize common processes and can develop customized CRM reports to bring on-the-ground experience from individual RECs to share success areas, identify barriers, and develop solutions. These efforts aggregate and inform individual interactions in provider offices, and similarly are instructive to REC and ONC leadership of technical assistance gaps and opportunities to improve interventions.
Partnership and Collaboration
To effect large and wide-scale implementation of EHRs among PCPs, RECs have relied on federal partners to coordinate efforts across stakeholders instead of intervening separately across multiple agencies to achieve collective impact (Kramer and Kania 2011). For example, the REC program has worked with partners to align existing federal, state, and local resources and programs with a special focus on rural providers. Within the U.S. Department of Agriculture, ONC has mobilized resources to connect rural health care providers with capital loan programs to support their acquisition of health IT. In partnership with the Departments of Labor and Education, rural health IT job search and training services are being expanded. In support of the Federal Communications Commission’s efforts to expand rural health care provider access to robust broadband, ONC has facilitated RECs’ understanding of and participation in the Federal Communications Commission’s Healthcare Connect Fund.
Continuing to Support Health Care Transformation
Building on lessons learned with MU of EHRs, RECs are positioned to assist providers with new care delivery and payment reform programs; many of which include MU measures as program milestones or requirements. RECs enable accountable care by helping providers electronically measure and report on evidence-based clinical quality measures for improved quality at the point of care. RECs also assist providers with participating in health information exchange for improved and coordinated care, safer transitions of care, population health management, and interfacing with public health infrastructure such as immunization registries. RECs help providers communicate with patients and families using technology, such as patient portals, for informed and inclusive decision making. Providers also utilize REC assistance to make the clinical and workflow changes necessary for medical home recognition.
RECs are supporting PCPs, specialists, and state governments with new care delivery and payment reform programs such as Accountable Care Organizations (ACO), the Million Hearts program, and Patient Centered Medical Home initiatives. For example, one East Coast ACO partnered with its local REC to receive additional technical support with data analytics, which required matching over 1,000 providers to beneficiaries and extracting quality data from the EHRs and paper-based charts. The REC then conducted in-office analytical review of both the EHR and paper-based records. Once reviewed and analyzed, the abstracted quality data were entered into Medicare’s group quality reporting system, which generated real-time analysis that was necessary for quality improvement, generating a report card, and educating physicians in the ACO.
This study has several limitations. Data were self-reported and may be biased from inconsistency with reporting, missing data, and data entry error. Date ranges of available data sources varied. In addition, errors could have occurred during the process of identifying FQHC, CAH, and small rural hospitals in the CRM. However, the two-step validation process for determining these practice settings minimizes the potential for this type of error. While these findings suggest REC assistance contributed to higher EHR adoption, this study was not designed to disentangle the impact of the program on EHR adoption and MU from the contributions of other factors, such as EHR Incentive Programs.
Conclusion
The REC program is making substantial progress in enrolling providers and supporting EHR adoption and MU among providers that historically have had lower rates of EHR adoption. Evidence indicates the REC program is the largest coordinated effort to build a national infrastructure capable of integrating and improving health care through supporting providers in technology adoption, change management, and clinical improvement. With hands-on practice facilitation and coaching, RECs are addressing key practice-level challenges through timely response to the marketplace, infrastructure for rapid-cycle improvement and diffusion, and collaboration with local partners. As change agents, RECs are responding to providers’ needs with outreach, education, technical assistance, and practice coaching. RECs are focused on supporting all providers, especially small practices, community health centers, and rural and public hospitals with not only health IT adoption, but technology for care delivery transformation and improvement.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: All authors are with the Office of the National Coordinator for Health IT, which established and supports the Regional Extension Center program.
Disclosures: None.
Disclaimers: None.
Notes
In addition to the nearly 134,000 PCPs currently enrolled with RECs, an additional 23,000 providers were at one time enrolled in the program and are no longer participating for reasons such as retirement or transitioning to a practice not enrolled with the REC.
Supporting Information
Additional Supporting Information may be found in the online version of this article at the publisher’s web-site:
Author Matrix.
Technical Details about the Regional Extension Center Program Launch.
References
- Baskerville NB, Liddy C, Hogg W. Systematic Review and Meta-Analysis of Practice Facilitation within Primary Care Settings. Annals Family Medicine. 2012;10(1):63–74. doi: 10.1370/afm.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick DM, Nolan TW, Whittington J. The Triple Aim: Care, Health, and Cost. Health Affairs. 2008;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- Birkhaeuser D, Evenson RE, Feder G. The Economic Impact of Agricultural Extension: A Review. Economic Development and Cultural Change. 1991;39(3):607–50. [Google Scholar]
- Blumenthal D. Launching HITECH. New England Journal of Medicine. 2010;362(5):382–5. doi: 10.1056/NEJMp0912825. [DOI] [PubMed] [Google Scholar]
- Blumenthal D. Wiring the Health System—Origins and Provisions of a New Federal Program. New England Journal of Medicine. 2011a;365(24):2323–9. doi: 10.1056/NEJMsr1110507. [DOI] [PubMed] [Google Scholar]
- Buntin MB, Jain SH, Blumenthal D. Health Information Technology: Laying the Infrastructure for National Health Reform. Health Affairs. 2010;29(6):1214–9. doi: 10.1377/hlthaff.2010.0503. [DOI] [PubMed] [Google Scholar]
- Crabtree BF, Nutting PA, Miller WL, McDaniel RR, Stange KC, Jaen CR, Stewart E. Primary Care Practice Transformation Is Hard Work: Insights from a 15-year Developmental Program of Research. Medical Care. 2011;49:S28. doi: 10.1097/MLR.0b013e3181cad65c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, Jha A, Kaushal R, Levy DE, Rosenbaum S, Shields AE, Blumenthal D. Electronic Health Records in Ambulatory Care—A National Survey of Physicians. New England Journal of Medicine. 2008;359(1):50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- Flex Monitoring Team. 2012. National CAH Database ” [accessed on June 30, 2012]. Available at http://www.flexmonitoring.org/cahlistRA.cgi.
- Grumbach K, Bainbridge E, Bodenheimer T. Facilitating Improvement in Primary Care: The Promise of Practice Coaching. Issue brief (Commonwealth Fund) 2012;15:1. [PubMed] [Google Scholar]
- Hallacher PM. Why Policy Issue Networks Matter: The Advanced Technology Program and the Manufacturing Extension Partnership. Lanham, MD: Rowman & Littlefield Pub Incorporated; 2005. [Google Scholar]
- Heisey-Grove D, Hufstader M, Hollin I, Samy L, Shanks K. Progress towards the Meaningful Use of Electronic Health Records among Critical Access and Small Rural Hospitals Working with Regional Extension Centers. Washington, DC: Office of the National Coordinator for Health Information Technology; 2012. ONC Data Brief, no. 5. [Google Scholar]
- Heisey-Grove D, Hawkins K, Jones E, Shanks K, Lynch K. 2013. Supporting Health Information Technology Adoption in Federally Qualified Health Centers [accessed on May 24, 2013]. ONC Data Brief No. 8. Available at http://www.healthit.gov/sites/default/files/rec-fqhc_data_brief_final.pdf.
- HITECH Act. 2009. HITECH Act was enacted as title XIII of division A and title IV of division B of the Recovery Act. Pub. L. No. 111-5, div. A, tit. XIII, 123 Stat. 115, 226-279 and div. B, tit. IV, 123 Stat. 115, 467-496.
- Jha A, ResRoches C, Kralovec P, Joshi M. A Progress Report of Electronic Health Records in US Hospitals. Health Affairs. 2010;29(10):1951–7. doi: 10.1377/hlthaff.2010.0502. [DOI] [PubMed] [Google Scholar]
- Kramer M, Kania J. Collective Impact. Stanford Social Innovation Review. 2011;57:36–41. [Google Scholar]
- Maxson E, Jain S, Kendall M, Mostashari F, Blumenthal D. The Regional Extension Center Program: Helping Physicians Meaningfully Use Health Information Technology. Annals of Internal Medicine. 2010;153(10):666. doi: 10.7326/0003-4819-153-10-201011160-00011. [DOI] [PubMed] [Google Scholar]
- Mostashari F, Tripathi M, Kendall M. A Tale of Two Large Community Electronic Health Record Extension Projects. Health Affairs. 2009;28(2):345–56. doi: 10.1377/hlthaff.28.2.345. [DOI] [PubMed] [Google Scholar]
- Nagykaldi Z, Mold JW, Aspy CB. Practice Facilitators: A Review of the Literature. Family Medicine—Kansas City. 2005;37(8):581. [PubMed] [Google Scholar]
- Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial Lessons from the First National Demonstration Project on Practice Transformation to a Patient-Centered Medical Home. Annals of Family Medicine. 2009;7(3):254–60. doi: 10.1370/afm.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutting P, Crabtree B, Miller W, Stange K, Stewart E, Jaen C. Transforming Physician Practices to Patient-Centered Medical Homes: Lessons from the National Demonstration Project. Health Affairs. 2011;30(3):439–45. doi: 10.1377/hlthaff.2010.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldsman E. Does Manufacturing Extension Matter? An Evaluation of the Industrial Technology Extension Services in New York. Research Policy. 1996;25:215–32. [Google Scholar]
- Phillips R, Kaufman A, Mold J, Grumbach K, Vetter-Smith M, Berry A, Teevan Burke B. The Primary Care Extension Program: A Catalyst for Change. Annals of Internal Medicine. 2013;11(2):173–8. doi: 10.1370/afm.1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers E. Diffusion of Innovations. Glencoe: Free Press; 1962. ISBN 0-612-62843-4. [Google Scholar]
- Ryan AM, Bishop T, Shih S, Casalino LP. Small Physician Practices in New York Needed Sustained Help to Realize Gains in Quality from Use of Electronic Health Records. Health Affairs. 2013;32(1):53–62. doi: 10.1377/hlthaff.2012.0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samantaray R, Njoku V, Brunner J, Raghaven V, Kendall M, Shih S. Promoting Electronic Health Record Adoption among Small Independent Primary Care Practices. American Journal of Managed Care. 2011;17(5):353–8. [PubMed] [Google Scholar]
- Samuel C, King J, Adetosoye F, Samy L, Furukawa M. Engaging Providers in Underserved Areas to Adopt Electronic Health Records. American Journal of Managed Care. 2013;19(3):229–34. [PubMed] [Google Scholar]
- SAS Institute Inc. Cary, NC: SAS Institute Inc; 2012. SAS (release 9.3) Statistical Software. [Google Scholar]
- SK&A Information Services. SK&A Office-Based Providers Database. Irvine, CA: 2011. [Google Scholar]
- Umali-Deininger D, Umali DL, Schwartz LA. Public and Private Agricultural Extension: Beyond Traditional Frontiers. Washington, DC: World Bank; 1994. (Vol. 236). [Google Scholar]
- US Department of Health and Human Services, Centers for Medicare and Medicaid Services. Baltimore, MD: 2013a. CMS Certified Hospital List from CASPER certificate and survey system, March 2013. [Google Scholar]
- US Department of Health and Human Services, Centers for Medicare and Medicaid Services. Baltimore, MD: 2013b. EHR Incentive Program Registration and Payment Data, June 2013. [Google Scholar]
- US Department of Health and Human Services, Centers for Medicare and Medicaid Services, Center for Medicare and Medicaid Innovation. Baltimore, MD: 2011a. List of Comprehensive Primary Care Initiative sites, August 2011 [accessed on June 30, 2013]. Available at https://data.cms.gov/dataset/CPC-Initiative-Participating-Primary-Care-Practice/mw5h-fu5i? [Google Scholar]
- US Department of Health and Human Services, Centers for Medicare and Medicaid Services, Center for Medicare and Medicaid Innovation. Baltimore, MD: 2011b. List of FQHC Advanced Primary Care Practice Demonstration sites, November 2011 [accessed June 30, 2013]. Available at http://innovation.cms.gov/initiatives/fqhcs/#collapse-tableDetails. [Google Scholar]
- US Department of Health and Human Services, Health Resources and Services Administration. Rockville, MD: 2011. Data Warehouse, August 2011 [accessed on June 30, 2013]. Available at http://datawarehouse.hrsa.gov/Download_HCC_LookALikes.aspx. [Google Scholar]
- US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions. Rockville, MD: 2011. –2012. Area Resource File [accessed on June 30, 2013]. Available at http://arf.hrsa.gov/ [Google Scholar]
- US Department of Health and Human Services, Health Resources and Services Administration, Office of Rural Health Policy. Rockville, MD: 2012. Small Rural Hospital Improvement Program List [accessed on June 30, 2013]. Available at http://www.hrsa.gov/ruralhealth/about/hospitalstate/index.html. [Google Scholar]
- US Department of Health and Human Services, Office of the National Coordinator for Health Information Technology. Customer Relationship Management Database [accessed on July 10, 2013] [Google Scholar]
- US Department of Health and Human Services, Office of the National Coordinator for Health Information Technology. Funding Opportunity Announcement. Recovery Act: Health Information Technology. Extension Program: Regional Centers. Funding Opportunity Number EP-HIT-09-003 [accessed on November 25, 2009]. Available at http://www.grants.gov/web/grants/search-grants.html?keywords=EP-HIT-09-003 [see the webpage section “Opportunity Status: archived”] [Google Scholar]
- U.S. Government Accountability Office. 2012. Number and Characteristics of Providers Awarded Medicare Incentive Payments for 2011 (Publication No. GAO-12-778R) [accessed on June 30, 2013]. Available at http://www.gao.gov/assets/600/593078.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Matrix.
Technical Details about the Regional Extension Center Program Launch.


