Abstract
Objective
To examine whether primary care team cohesion changes the association between using an integrated outpatient-inpatient electronic health record (EHR) and clinician-rated care coordination across delivery sites.
Study Design
Self-administered surveys of primary care clinicians in a large integrated delivery system, collected in 2005 (N = 565), 2006 (N = 678), and 2008 (N = 626) during the staggered implementation of an integrated EHR (2005–2010), including validated questions on team cohesion. Using multivariable regression, we examined the combined effect of EHR use and team cohesion on three dimensions of care coordination across delivery sites: access to timely and complete information, treatment agreement, and responsibility agreement.
Principal Findings
Among clinicians working in teams with higher cohesion, EHR use was associated with significant improvements in reported access to timely and complete information (53.5 percent with EHR vs. 37.6 percent without integrated-EHR), agreement on treatment goals (64.3 percent vs. 50.6 percent), and agreement on responsibilities (63.9 percent vs. 55.2 percent, all p < .05). We found no statistically significant association between use of the integrated-EHR and reported care coordination in less cohesive teams.
Conclusion
The association between EHR use and reported care coordination varied by level of team cohesion. EHRs may not improve care coordination in less cohesive teams.
Keywords: Electronic health records, care coordination, primary care, teams, team cohesion
A growing number of Americans are living with chronic medical conditions and often require medical care that bridges multiple delivery sites, such as hospitals and primary care clinics (Partnership for Solutions 2004; Bodenheimer, Chen, and Bennett 2009; Schoen et al. 2009; Anderson 2010; Thorpe, Ogden, and Galactionova 2010). Effective coordination is necessary to ensure high-quality care for these patients. In part to promote greater care coordination, the American Recovery and Reinvestment Act (ARRA) of 2009 allocated $27 billion to encourage adoption and meaningful use of electronic health records (EHRs) in the United States (Blumenthal 2010b; Blumenthal and Tavenner 2010). Communication of clinical information for coordination of care across delivery sites is an explicit requirement for “meaningful use” payments under ARRA (Blumenthal 2010a). Other health care innovations such as bundled payments, accountable care organizations, and patient centered medical homes aim to improve care quality in part through facilitating care coordination and a greater reliance on team-based care (Rittenhouse and Shortell 2009; Blumenthal and Tavenner 2010; Shortell, Casalino, and Fisher 2010). Given the ongoing reforms targeting the organization and financing of health care, and sizable federal investment in EHRs, it is important to understand how the organizational environment can influence the EHR effect on various outcomes, including care coordination.
The shared use of an EHR across hospitals, specialist and primary care practices, and other provider organizations offers great potential to improve coordination by enabling access to comprehensive, current patient information each time a patient is seen by clinicians. EHRs also provide tools to monitor a patient’s health status and intervene promptly when necessary. However, effective use of the information and tools made available by an EHR requires active communication and teamwork between clinicians. In other words, having the basic infrastructure of an integrated delivery system or shared EHR may be insufficient to improve the delivery of care if clinicians do not make full use of the information or fail to use it when working with other clinicians. There is limited research on the effects of EHR use on care coordination (Graetz et al. 2009; O’Malley et al. 2009) and no evidence on how organizational factors may change this effect.
For this study, we focus on the coordination of care across delivery sites, such as when patients leave hospitals and re-enter primary care. These transitions represent a timely area of policy and clinical interest, during which prior studies have found high rates of errors (Coleman et al. 2006). We examined the combined effect of an integrated outpatient–inpatient certified EHR and team cohesion on clinician ratings of care coordination across delivery sites in a prepaid IDS. We used survey data from primary care clinicians collected in three different years (2005, 2006, and 2008), during the staggered implementation of a commercially available, integrated EHR system (2005–2010). We hypothesized that the use of the integrated EHR would result in improvements in all reported measures of care coordination and that the magnitude of the association would be greater for clinicians working in primary care teams with higher cohesion.
Methods
Study Setting
This study was conducted at Kaiser Permanente Northern California, a large, prepaid IDS providing comprehensive medical care for over 3 million members. The system receives bundled prospective payment for all medical care. Over 1,000 primary care clinicians work in the Internal Medicine and Family Medicine departments and are grouped into 110 primary care teams, across 18 Medical Centers.
Primary Care Teams
Adult primary care teams were created in 1998 as part of an effort to redesign primary care using multidisciplinary teams, which include different types of care providers in addition to physicians, such as nurse practitioners, behavioral medicine specialists, physical therapists, health educators, and pharmacists. On average, primary care teams had 10 clinicians (physicians and nurse practitioners) and 5 nonclinician team members, and ranged from 3 to 25 total members per team.
Health Information Technology
In 2005, the IDS began a 5-year staggered implementation of a commercially available, integrated outpatient-inpatient certified-EHR system. The system was rolled out in two phases: staggered across outpatient clinics (2005–2008) followed by inpatient hospitals 1–2 years later (2007–2010). Once implemented, use of the EHR system was mandatory, meaning it replaced the paper-based medical record and ordering systems. Although the sequence of the EHR implementation was not random, it was not based on the ability of medical centers to implement the EHR or chronic disease care quality, and it did not correspond with any other organizational changes (Reed et al. 2012).
The EHR is an EpicCare-based integrated system that increases the amount of information available at the point-of-care, presenting clinical information in an electronic medical record, and provides comprehensive computer-based provider order entry for labs and prescriptions, sophisticated decision-support tools, and secure messaging between providers and with patients. This system has been certified by the Certification Commission for Health Information Technology as a complete EHR, thereby providing its users with the capabilities necessary to meet the goals of the “Meaningful Use” criteria for federal incentive payments. All primary care clinicians received equivalent classroom-style training on the basics of how to use the EHR and ongoing technical support.
Prior to the EHR implementation, clinicians had access to a limited number of Health IT applications. Importantly, use of these applications was voluntary and sporadic, as paper-based medical charts were still in use (Bardach et al. 2009).
Integrated EHR
We defined each primary care clinician’s integrated EHR status at the date he or she completed the survey. Clinicians working in facilities which had implemented both the inpatient and outpatient EHR components were defined as having an integrated EHR.
Survey Collection
In 2005, 2006, and 2008, we mailed a self-administered questionnaire to all adult primary care clinicians working in the IDS, including physicians, nurse practitioners, and physician’s assistants. Each clinician received a letter introducing the study, the survey, and a prepaid return envelope. Respondents who completed the survey received a small gift card. Nonrespondents were resent reminder letters and surveys; up to four follow-up mailings were sent during each year of survey collection.
The target population included 1,175 clinicians in 2005; 1,103 clinicians in 2006; and 1,030 clinicians in 2008. Overall, 565 primary care clinicians responded in 2005, 678 in 2006, and 626 in 2008 (48, 62, and 61 percent response rates, respectively).
Care Coordination
Using a five-point scale, we asked clinicians the following questions about coordination when care is transferred across delivery sites: “How often does each of the following occur when care is transferred across delivery sites (e.g., from the hospital to the outpatient team)?”
“All relevant medical information is available.”
“The information transfer is timely, i.e., available when it is needed.”
“All clinicians agree on the treatment goals and plans.”
“All clinicians agree on roles and responsibilities of each party.”
The response categories were as follows: never, rarely, sometimes, usually, and always. Questions on care coordination were developed by expert scientific advisors specifically for this study. After we developed these questions, the Stanford-UCSF Evidence-based Practice Center published a comprehensive report on care coordination, which supported the same key elements: access to information, agreement on goals and responsibilities, and agreement on a purpose or goal (McDonald et al. 2007).
We combined responses to the questions asking if “all relevant medical information is available” and “information transfer is timely” to simplify the presentation. We reasoned that for information to be useful when coordinating care, it must be both complete and timely. Also, responses to these two survey questions were highly correlated (0.8). “Access to complete and timely information” was coded as one if the respondent reported “always” or “usually” to both questions; otherwise it was coded as zero.
We created two dichotomous variables: “agreement on treatment goals and plans” and “agreement on roles and responsibilities”; each was coded as 1 if the clinician responded that the relevant agreement “always” or “usually” occurred; otherwise it was coded as a 0. The number of missing values was small (<5 percent) and not correlated with EHR status; therefore, missing responses were dropped from the analyses.
Team Cohesion
Team cohesion questions were developed using published validated instruments (Ohman-Strickland et al. 2007). Using a five-point Likert agreement response scale, we asked each clinician the following questions:
“When there is conflict on this team, the people involved usually talk it out and resolve the problem successfully.”
“Our team members have constructive work relationships.”
“There is often tension among people on this team.” (reverse scored)
“The team members operate as a real team.”
We calculated the average response over the four items and aggregated them across all members from the same primary care team. The overall measure demonstrated high internal consistency with a Cronbach alpha coefficient of reliability of 0.83. For simplicity in presentation, we categorized team cohesion scores into quartiles and created a binary indicator variable classifying each team as having lower or higher cohesion, with the lowest quartile of scores representing lower cohesion teams. We chose to categorize teams by the lowest quartile cohesion because the average cohesion score in this IDS setting was higher than those previously reported in other settings (Ohman-Strickland et al. 2007). Sensitivity analyses using other thresholds and constructions of team cohesion yielded comparable findings.
Open-Ended Questions
We also asked clinicians open-ended questions on barriers to care coordination across delivery sites and to describe how they learned to use the EHR. While we did not formally analyze these questions, they provided key quotes to help illustrate the plausibility of our findings (Table 3).
Table 3.
Key Quotes from Clinician Survey Responses
| Barriers to Care Coordination |
| “The question is not if the information is available but if we have time to access it or can find it.” |
| “There is so much information and repetition in the system. It’s easy to miss the important points.” |
| “Handoffs continue to be a problem. Communication is still needed, not just relying on [the EHR] messages. Info is generally available but sometimes hard to access—that is, it is, “buried” and not easily found.” |
| EHR training |
| “I learned the most from colleagues; it’s helpful when we all meet to share knowledge.” |
| “[I learned to use EHRs] mostly by practicing, trying to solve problems, talking to other people, and a lot of trial and error.” |
| “Colleagues taught me more [on how to use EHRs] than formal presentations.” |
Covariates
Our survey collected several respondent characteristics, including race/ethnicity, gender, tenure, and job title. We supplemented survey responses with information from the IDS’s automated database, including age, gender, race/ethnicity, and job title.
Analytic Approach
We used generalized linear latent and mixed models logistic regression with random intercepts for clinician and hospital (Rabe-Hesketh, Skrondal, and Pickles 2004), with an interaction term for integrated outpatient–inpatient EHR status and team cohesion to allow for potentially different EHR effects by team cohesion. We included clinician characteristics as covariates (e.g., age, gender, race/ethnicity, and job title) and a year indicator variable to control for time trends that may have affected coordination but were unrelated to the EHR implementation.
To calculate the estimated EHR effect for clinicians working in teams with higher versus lower cohesion, we used results from our logistic regression models to compute the marginal adjusted percent of respondents reporting each outcome by fitting the models as if all respondents worked in teams with (1) no integrated EHR and lower team cohesion; (2) integrated EHR and lower team cohesion; (3) no integrated EHR and higher team cohesion; and (4) integrated EHR and higher team cohesion.
Team cohesion was created to be a team-level variable, including responses of multiple clinicians per team, whereas coordination was designed as an individual clinician-level variable. As a sensitivity analysis to test the stability of the team cohesion measure, we ran all models excluding teams with fewer than four respondents (N = 51) and models where the response of the individual clinician was excluded from their primary care team cohesion score and attained comparable results. All analyses were implemented using Stata 10 (StataCorp LP, College Station, TX, USA).
Results
Table 1 shows the characteristics of respondents and nonrespondents by study year. In 2005, none of the respondents had access to the integrated EHR; by 2006, 6.3 percent were using the EHR, and in 2008, 52.2 percent were using the integrated EHR. We compared respondents and nonrespondents on several characteristics, and in 2005 and 2006, women were more likely to respond than men, nurse practitioners more than physicians, and in 2008, younger clinicians more likely than older clinicians (p < .05).
Table 1.
Respondent Characteristics by Survey Year (%)
| 2005 | 2006 | 2008 | ||||
|---|---|---|---|---|---|---|
| Respondents (N = 565) | Nonrespondents (N = 610) | Respondents (N = 678) | Nonrespondents (N = 424) | Respondents (N = 626) | Nonrespondents (N = 404) | |
| Gender | ||||||
| Male | 45.3 | 56.9 | 46.0 | 52.4 | 48.3 | 51.7 |
| Female | 54.7* | 43.1 | 54.0* | 47.6 | 51.7 | 48.3 |
| Race/ethnicity | ||||||
| Nonwhite | 51.0 | 53 | 56.9 | 55.4 | 60.6 | 65.1 |
| White | 49.0 | 47 | 43.1 | 44.6 | 39.4 | 34.9 |
| Job title | ||||||
| Nurse practitioners | 15.8* | 6.7 | 11.7* | 6.6 | 5.6 | 4.5 |
| Physicians | 84.3 | 93.3 | 88.4 | 93.4 | 94.4 | 95.5 |
| Age | ||||||
| 25–39 | 36.0 | 35.1 | 38.1 | 30.3 | 39.5* | 29.5 |
| 40–49 | 32.5 | 32.2 | 32.0 | 35 | 33.8 | 37.9 |
| 50–59 | 27.0 | 25.9 | 23.9 | 26.7 | 21.8 | 25.7 |
| 60+ | 4.6 | 6.7 | 6.1 | 8 | 5.0 | 6.9 |
| No integrated EHR | 100.0 | 100 | 93.7 | 95.3 | 52.2 | 56.7 |
| Integrated EHR | 0.0 | 0 | 6.3 | 4.7 | 7.8 | 43.3 |
Note.
A total of 262 clinicians completed the survey in all three waves of data collection (2005, 2006, and 2008), 609 completed at least two surveys, and 1,207 completed at least one survey. Clinicians who worked in facilities where both the inpatient and outpatient EHR components were implemented were defined as having an integrated EHR.
p < .05 compared respondent and nonrespondent characteristics each year and represents groups that were more likely to respond.
Table 2 shows characteristics of the primary care teams. In 2005, teams had an average of 11 primary care clinicians per team, and that number decreased to less than 10 in 2008. On average, respondents reported working in the same primary care team for over 5 years. Overall, 46.6 percent of teams changed cohesion category over the study period, but these changes were not statistically associated with use of the integrated EHR.
Table 2.
Team Characteristics (Mean, Standard Deviation)
| 2005 | 2006 | 2008 | |
|---|---|---|---|
| N | 105 | 106 | 104 |
| Primary care clinicians per team | 11.14 (3.78) | 10.4 (3.86) | 9.86 (5.92) |
| Respondents per team | 5.39 (2.32) | 6.40 (2.71) | 6.01 (4.24) |
| Reported team tenure (years) | 5.62 (4.53) | 5.54 (4.79) | 6.39 (4.75) |
| Team cohesion | |||
| Lower (bottom quartile) | 3.30 (0.35) | 3.23 (0.35) | 3.18 (0.42) |
| Higher (2nd–4th quartiles) | 3.87 (0.27) | 3.87 (0.23) | 3.83 (0.19) |
Note. We calculated team cohesion scores by averaging responses over the four team cohesion survey items and aggregating them across members from the same primary care team. We categorized team cohesion scores into quartiles and created a binary indicator variable for teams in the lowest quartile. Possible team cohesion scores ranged from 1 to 5, with 5 representing the highest level of cohesion.
From our multivariate analyses, we found that the association between use of the integrated EHR and access to timely and complete information and clinician agreement on the patient’s treatment plan was statistically different for clinicians working in teams with higher versus lower cohesion (p < .05), but not for clinician agreement on each other’s roles and responsibilities. Figure 1 shows the adjusted percent of respondents who reported each care coordination outcome by primary care team cohesion and integrated outpatient–inpatient EHR status.
Figure 1.
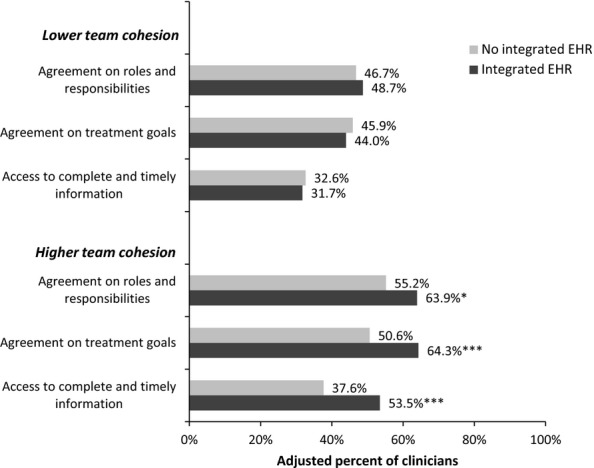
Adjusted Clinician Reported Care Coordination by Availability of Integrated Outpatient–Inpatient Electronic Health Record (EHR) and Team CohesionNote. We computed the marginal adjusted percent of respondents who reported each outcome by fitting the logistic regression models as if all respondents had (1) no integrated EHR and lower team cohesion; (2) integrated EHR and lower team cohesion; (3) no integrated EHR and higher team cohesion; and (4) integrated EHR and higher team cohesion. Clinicians who worked in facilities where both the inpatient and outpatient EHR components were implemented were defined as having an integrated EHR. *p < .05, **p < .01, ***p < .001. p-value compared integrated EHR to no integrated EHR by team cohesion category.
The change in reported access to complete and timely clinical information was substantially greater with use of the integrated EHR for clinicians working in higher cohesion teams (53.5 percent with EHR vs. 37.6 percent no-EHR, p < .001) compared with those in lower cohesion teams (31.7 percent with EHR vs. 32.6 percent no-EHR). Likewise, the change in reported clinician agreement on treatment goals and plans was greater with access to an integrated EHR for clinicians in higher cohesion teams (64.3 percent with EHR vs. 50.6 percent no-EHR, p < .001) compared with those in lower cohesion teams (44.0 percent with EHR vs. 45.9 percent no-EHR). Similarly, the change in clinician agreement on roles and responsibilities was greater with access to an integrated EHR for higher cohesion teams (63.9 percent with vs. 55.2 percent no-EHR, p < .05) compared with clinicians working in lower cohesion teams (48.7 percent with vs. 46.7 percent non-EHR).
After adjustments, we also found that physicians were significantly more likely to report each coordination outcome compared with nurse practitioners or physician assistants (p < .05, see appendix). Older clinicians were more likely to report greater access to complete and timely information and less likely to report agreement on the treatment plan (p < .05). The full results of the multivariate analysis are included in the appendix.
Discussion
EHR use has the potential to improve clinical care delivery; however, the literature documenting achievement of this potential has been sparse and mixed (Linder et al. 2007; Friedberg et al. 2009; Cebul et al. 2011; Holroyd-Leduc et al. 2011; Romano and Stafford 2011; Reed et al. 2012). There is documented variability in the success of US clinical practices implementing EHRs, with some implementations being met with resistance and a few resulting in noted failures (Poon et al. 2006). Given the complexity of the implementation and care delivery processes for individual and groups of clinicians, there is surprisingly little known about how the organization of clinicians might influence the effect of EHR use on care coordination. We found that integrated EHR use was associated with greater care coordination among clinicians working in primary care teams with higher cohesion but not for those working in teams with lower cohesion.
One of the principal functions of an EHR is to provide current and comprehensive patient health information to all of a patient’s health care clinicians at the point of care. Therefore, we were surprised to find that clinicians working in lower cohesion teams did not experience statistically significant improvements in the reported measures of care coordination with use of the integrated EHR. One potential explanation is that the additional information creates new processing challenges. More information and “places” within the EHR to store information engender new obstacles. It is possible that clinicians working in less cohesive teams struggled to navigate the EHR (e.g., less shared learning) or had fewer systematically agreed-upon approaches to document and retrieve information.
EHR use can lead to a number of unintended consequences, such as clinicians entering critical data in miscellaneous sections of the EHR, making it difficult for others to retrieve, and the EHR eliminating the need for frequent informal interactions, which previously provided redundant checks that helped prevent errors (Harrison, Koppel, and Bar-Lev 2007). This possibility is consistent with clinician responses (Table 3) to open-ended questions on barriers to care coordination (Bostrom and Heinen 1977; Harrison, Koppel, and Bar-Lev 2007).
In addition, team cohesion may promote greater informal learning, which is reinforced through ongoing communication and the strength of relationships (Robey, Boudreau, and Rose 2000). Although all clinicians received equivalent formal classroom-style training on the EHR, this training focused on basic tasks such as documenting and ordering. There was little training on how to use the wealth of information available through the EHR or how to work better with other clinicians. Thus, informal learning through one’s professional network and team represents an important mechanism through which cohesion could mediate the EHR effects. Members working in teams with higher cohesion may have been more comfortable experimenting with the EHR and willing to share best practices with each other. This could quicken the learning process, ensuring that clinicians are able to maximize the potential benefits of the EHR while also avoiding undesirable consequences. In response to open-ended questions on EHR training, clinicians reported learning more from colleagues than formal training (Table 3). This is consistent with the literature on organizational learning indicating the critical role of the team environment in the adoption and learning of new technology (Edmondson, Bohmer, and Pisano 2001; Edmondson et al. 2003).
Our study has a number of limitations. The study focused on primary care providers in a single IDS, using a specific EHR system. In other settings, the effect of EHR use and team cohesion on care coordination may differ. While the care coordination and team cohesion measures were based on self-reported data, audit trails did not provide adequate measures of care coordination and team cohesion. Furthermore, team relationships can only be captured through self-reported data and have been associated with improvements in care quality (Shortell et al. 2004). We had a relatively high level of response and multiple respondents per each team. We collected ratings of team cohesion and of care coordination at the same point in time for each respondent, which could raise two related concerns: (1) response bias (e.g., some respondents tend to give uniformly high or low ratings) and (2) the direction of the relationship. In the analysis, however, the cohesion measure is a team-level variable consisting of multiple clinicians per team.
Using sensitivity analyses excluded the individual clinician’s rating of team cohesion from the primary care team’s cohesion score, we attained comparable results. Since the inpatient EHR implementation occurred 1–2 years following the outpatient EHR implementation, some of the EHR effects could be attributable to improvements in use of the outpatient EHR system over time. Still, because we focused on care coordination across delivery sites, it is unlikely that use of the outpatient EHR alone had much impact. Preliminary analysis confirmed that use of the outpatient EHR alone was not statistically associated with care coordination across delivery sites. Lastly, because this was an observational study, our findings represent an association and not a causal effect.
In short, we found that the association of an integrated outpatient–inpatient EHR on reported care coordination varied by primary care team cohesion. Future studies should examine how changes in coordination impact patient outcomes. While EHRs have the potential to improve care quality, they are not panaceas and their impact may be limited if deficiencies of the work environment, such as team cohesion, are not addressed. Our findings suggest that EHRs may not improve care coordination across delivery sites if teams are not working well together.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported by grants from the Agency for Healthcare Research and Quality (1R36HS021082-01 and R01DK085070) and the National Institute of Diabetes and Digestive and Kidney Diseases (R01HS015280). The content, findings, and conclusions of this article are the sole responsibility of the authors; the sponsors were not involved in any way in the determination of the content of this article. The authors have no conflict of interest.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional Supporting Information may be found in the online version of this article at the publisher’s web-site:
Author Matrix.
Logistic Regression of Clinician Reported Coordination Measures for Care Transferred across Delivery Sites with Random Intercepts for Clinician and Medical Center (full model results).
References
- Anderson GF. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation; 2010. [Google Scholar]
- Bardach NS, Huang J, Brand R, Hsu J. Evolving Health Information Technology and the Timely Availability of Visit Diagnoses from Ambulatory Visits: A Natural Experiment in an Integrated Delivery System. BMC Medical Informatics and Decision Making. 2009;9(1):35. doi: 10.1186/1472-6947-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal D. Guiding the Health Information Technology Agenda. Interviewed by David J. Brailer. Health Affairs. 2010a;29(4):586–95. doi: 10.1377/hlthaff.2010.0274. [DOI] [PubMed] [Google Scholar]
- Blumenthal D. Launching HITECH. New England Journal of Medicine. 2010b;362(5):382–5. doi: 10.1056/NEJMp0912825. [DOI] [PubMed] [Google Scholar]
- Blumenthal D, Tavenner M. The ‘Meaningful Use’ Regulation for Electronic Health Records. New England Journal of Medicine. 2010;6:501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Chen E, Bennett HD. Confronting the Growing Burden of Chronic Disease: Can the U.S. Health Care Workforce Do the Job? Health Affairs. 2009;28(1):64–74. doi: 10.1377/hlthaff.28.1.64. [DOI] [PubMed] [Google Scholar]
- Bostrom RP, Heinen JS. MIS Problems and Failures: A Socio-Technical Perspective, Part II: The Application of Socio-Technical Theory. MIS Quarterly. 1977;1(4):11–28. [Google Scholar]
- Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic Health Records and Quality of Diabetes Care. New England Journal of Medicine. 2011;365:825–83. doi: 10.1056/NEJMsa1102519. [DOI] [PubMed] [Google Scholar]
- Coleman EA, Parry C, Chalmers S, Min S-J. The Care Transitions Intervention: Results of a Randomized Controlled Trial. Archives of Internal Medicine. 2006;166(17):1822. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- Edmondson AC, Bohmer RM, Pisano GP. Disrupted Routines: Team Learning and New Technology Implementation in Hospitals. Administrative Science Quarterly. 2001;46(4):685–716. [Google Scholar]
- Edmondson AC, Winslow AB, Bohmer RMJ, Pisano GP. Learning How and Learning What: Effects of Tacit and Codified Knowledge on Performance Improvement Following Technology Adoption. Decision Sciences. 2003;34(2):197–224. [Google Scholar]
- Friedberg MW, Coltin KL, Gelb Safran D, Dresser M, Zaslavsky AM, Schneider EC. Associations between Structural Capabilities of Primary Care Practices and Performance on Selected Quality Measures. Annals of Internal Medicine. 2009;151(7):456–63. doi: 10.7326/0003-4819-151-7-200910060-00006. [DOI] [PubMed] [Google Scholar]
- Graetz I, Reed M, Rundall T, Bellows J, Brand R, Hsu J. Care Coordination and Electronic Health Records: Connecting Clinicians. AMIA Annual Symposium Proceedings. 2009;2009:208–12. [PMC free article] [PubMed] [Google Scholar]
- Harrison MI, Koppel R, Bar-Lev S. Unintended Consequences of Information Technologies in Health Care—An Interactive Sociotechnical Analysis. Journal of the American Medical Informatics Association. 2007;14(5):542–9. doi: 10.1197/jamia.M2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holroyd-Leduc JM, Lorenzetti D, Straus SE, Sykes L, Quan H. The Impact of the Electronic Medical Record on Structure, Process, and Outcomes within Primary Care: A Systematic Review of the Evidence. Journal of the American Medical Informatics Association. 2011;18(6):732–7. doi: 10.1136/amiajnl-2010-000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linder JA, Ma J, Bates DW, Middleton B, Stafford RS. Electronic Health Record Use and the Quality of Ambulatory Care in the United States. Archives of Internal Medicine. 2007;167(13):1400–5. doi: 10.1001/archinte.167.13.1400. [DOI] [PubMed] [Google Scholar]
- McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft S, McKinnon M, Paguntalan H, Owens DK. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. Rockville, MD: Agency for Healthcare Research and Quality; 2007. [PubMed] [Google Scholar]
- Ohman-Strickland PA, John OA, Nutting PA, Perry DW, Scott-Cawiezell J, Hahn K, Gibel M, Crabtree BF. Measuring Organizational Attributes of Primary Care Practices: Development of a New Instrument. Health Services Research. 2007;42(3 Pt 1):1257–73. doi: 10.1111/j.1475-6773.2006.00644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley AS, Tynan A, Cohen GR, Kemper N, Davis MM. Coordination of Care by Primary Care Practices: Strategies, Lessons and Implications. Research Briefs. 2009;12:1–16. [PubMed] [Google Scholar]
- Partnership for Solutions. Chronic Conditions: Making the Case for Ongoing Care. Baltimore, MD: Johns Hopkins University Press; 2004. pp. 1–68. [Google Scholar]
- Poon EG, Jha AK, Christino M, Honour MM, Fernandopulle R, Middleton B, Newhouse J, Leape L, Bates DW, Blumenthal D, Kaushal R. Assessing the Level of Healthcare Information Technology Adoption in the United States: A Snapshot. BMC Medical Informatics and Decision Making. 2006;6:1. doi: 10.1186/1472-6947-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A, Pickles A. Berkeley: University of California; 2004. pp. 1–140. GLLAMM Manual Division of Biostatistics Working Paper Series. Working Paper No. 160. [Google Scholar]
- Reed M, Huang J, Graetz I, Brand R, Hsu J, Fireman B, Jaffe M. Outpatient Electronic Health Records and the Clinical Care and Outcomes of Patients with Diabetes Mellitus. Annals of Internal Medicine. 2012;157(7):482–9. doi: 10.7326/0003-4819-157-7-201210020-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rittenhouse DR, Shortell SM. The Patient-Centered Medical Home. Journal of the American Medical Association. 2009;301(19):2038–40. doi: 10.1001/jama.2009.691. [DOI] [PubMed] [Google Scholar]
- Robey D, Boudreau MC, Rose GM. Information Technology and Organizational Learning: A Review and Assessment of Research. Accounting, Management and Information Technologies. 2000;10(2):125–55. [Google Scholar]
- Romano MJ, Stafford RS. Electronic Health Records and Clinical Decision Support Systems: Impact on National Ambulatory Care Quality. Archives of Internal Medicine. 2011;171(10):897–903. doi: 10.1001/archinternmed.2010.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoen C, Osborn R, How SK, Doty MM, Peugh J. In Chronic Condition: Experiences of Patients with Complex Health Care Needs, in Eight Countries, 2008. Health Affairs. 2009;28(1):w1–16. doi: 10.1377/hlthaff.28.1.w1. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Casalino LP, Fisher ES. How the Center for Medicare and Medicaid Innovation Should Test Accountable Care Organizations. Health Affairs (Millwood) 2010;29(7):1293–8. doi: 10.1377/hlthaff.2010.0453. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Marsteller JA, Lin M, Pearson ML, Wu S-Y, Mendel P, Cretin S, Rosen M. The Role of Perceived Team Effectiveness in Improving Chronic Illness Care. Medical Care. 2004;42(11):1040–8. doi: 10.1097/00005650-200411000-00002. [DOI] [PubMed] [Google Scholar]
- Thorpe KE, Ogden LL, Galactionova K. Chronic Conditions Account for Rise in Medicare Spending from 1987 to 2006. Health Affairs. 2010;29(4):718–24. doi: 10.1377/hlthaff.2009.0474. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Matrix.
Logistic Regression of Clinician Reported Coordination Measures for Care Transferred across Delivery Sites with Random Intercepts for Clinician and Medical Center (full model results).


