Abstract
This paper investigates the prevalence of incapacity in performing daily activities and the associations between household composition and availability of family members and receipt of care among older adults with functioning problems in Spain, England and the United States of America (USA). We examine how living arrangements, marital status, child availability, limitations in functioning ability, age and gender affect the probability of receiving formal care and informal care from household members and from others in three countries with different family structures, living arrangements and policies supporting care of the incapacitated. Data sources include the 2006 Survey of Health, Ageing and Retirement in Europe for Spain, the third wave of the English Longitudinal Study of Ageing (2006), and the eighth wave of the USA Health and Retirement Study (2006). Logistic and multinomial logistic regressions are used to estimate the probability of receiving care and the sources of care among persons age 50 and older. The percentage of people with functional limitations receiving care is higher in Spain. More care comes from outside the household in the USA and England than in Spain. The use of formal care among the incapacitated is lowest in the USA and highest in Spain.
Keywords: informal care, formal care, long-term care, Spain, England, USA, disability, SHARE, ELSA, HRS
Introduction
In recent decades, industrialised countries have experienced an increase in the average length of life, improved economic circumstances, a reduction in widowhood and a reduction in the number of children. These changes have affected the availability of family members and the resources of families and individuals to provide care (Doty 1986). While developed countries have generally shared similar economic, demographic and social trends, there are many differences across countries in the details of the familial, social, economic and policy context in which older people live which affect the sources of care available and how these are used by those with functioning problems (Himes 1992).
Our question is how the availability of family members affects informal care and formal care receipt for older persons with incapacities who live in three countries with different availability of family, different living arrangements and different policies toward providing care for the older incapacitated population. We investigate the effect of family composition and living arrangements on use of informal or formal care for adults aged 50+ in Spain, England and the United States of America (USA). Spain, as a southern European country, is characterised by more co-resident intergenerational living arrangements. England, a northern European country, is characterised by the presence of fewer family members in the household; and finally, in the USA older people have had more children but they have fewer residing in their households. We hypothesise that larger households, more intergenerational living arrangements and greater availability of children will result in more usage of informal care (Gans and Silverstein 2006); however, the effects of these variables will vary across countries with different policies. In countries with more generous policies, we expect to see more use of formal care. Cross-national analysis has the potential to contribute to a greater understanding in all countries of the links between demographic trends, cultural traditions and welfare policies, and the ways in which care for incapacitated adults is provided.
Background
The increasing size of the older population has generated concern among policy makers because of the related increase in demand for and cost of long-term care (Comas-Herrera et al. 2006; Palloni 2001). Spain and the United Kingdom (UK) are currently among the oldest European countries, with percentages of individuals age 65 and older of 16.6 per cent in Spain and 16.1 per cent in the UK (Statistical Office of the European Commission 2010); the USA is somewhat younger with 12.9 per cent of its population aged 65 and older (United States Bureau of the Census 2009). The proportion of the population that is older reflects past fertility as well as mortality. These countries have had different fertility histories with family sizes larger in the USA. Past fertility determines the number of children older people have to provide support in old age and is also associated with living arrangements in old age as older individuals with more children are less likely to live alone than those with fewer children (Wolf 1995).
Living arrangements are crucial for understanding whether an older person can receive support to age at home. Living arrangements are affected by marital and family status of older and younger people as well as economic and cultural conditions, and they vary among Spain, England and the USA. Higher survival rates among older persons have been accompanied by lower rates of widowhood (Elwert and Christakis 2008; Holden and Kuo 1996; Schaefer, Quesenberry and Wi 1995); however, past histories of divorce and separation also affect the likelihood that older persons will live with a spouse. The greater longevity of females, as well as lower remarriage rates after divorce, mean that women are likely to spend more years widowed and living alone (Guillén et al. 2006). Because women are more likely to be incapacitated (Crimmins, Kim and Solé-Auró 2011), their need for long-term care is greater while the availability of spouses to provide care is lower.
Culturally influenced norms relevant to family responsibilities and obligations are important in affecting living arrangements among older people (Crimmins and Ingegneri 1990; Glaser 1997). Co-residency of older people with children is more common in more traditional and familistic Southern European societies like Spain (Huber et al. 2009; Reher 1998; Silverstein et al. 2010). However, in almost all countries living arrangements of older people have changed over time. After a long-term trend from the 1950s through the 1990s toward increasing solitary living among older individuals in Europe and the USA, levels of independent living have now stabilised or even declined, depending on the country (Macunovich et al. 1995; Tomassini et al. 2004; Wolf 1995).
The availability of family members is related to differences in how informal care is provided across countries. In Nordic countries more assistance is provided to non-coresident elders, whereas more care is provided by co-residents in Southern Europe (Bonsang 2009). While care-giving is more gender balanced in the UK and the USA, female carers in Spain provide more than 80 per cent of care (Huber et al. 2009). Children have been shown to be the predominant carers in Spain and the UK; while partners in Spain appear to have reduced their care-giving role in recent years (Huber et al. 2009). The age group providing the largest share of informal care in Europe is those 40–65 years old, but in the USA more informal care is provided by older persons. These differences may represent different availability of carers or cultural differences in the view of appropriate roles for care-giving.
Determinants of use of formal and informal care among non-institutionalised elderly people have been investigated by numerous researchers (Branch et al. 1988; Litwin and Attias-Donfut 2009; Kemper 1992). Disability is a strong predictor of receipt of long-term care, both formal and informal. Informal care is also more likely to be received by older incapacitated people who live with someone (Huber et al. 2009). Whether informal care compensates, complements, or substitutes for formal care may differ across countries with different policies. Studies of home care in the USA have found that an increase in informal services was linked to a decrease in usage of formal services, suggesting that they were substitutes (Greene 1983; Van Houtven and Norton 2004). On the other hand, Bonsang (2009) and Bolin, Lindgren and Lundborg (2008), examining European countries, have concluded that informal care complements professional home and institutional care. Bonsang (2009) reports that the substitution of informal care for paid domestic help tends to disappear as the level of disability of older persons increases, and that informal care is a weak complement for nursing care. Bolin, Lindgren and Lundborg (2008) found that informal care behaves as a substitute for formal care in some circumstances but is a complement for hospital and doctor visits. Jiménez-Martín and Prieto (2012) provide evidence that informal and ‘inside home’ formal care can be complements and informal and ‘outside home’ formal care are substitutes in Spain (García, Prieto-Flores and Rosenberg 2008). Research in the UK showed that informal care-givers acted as a substitutes for formal care for simple tasks but as complements for more skilled and technological tasks (Mentzakis, McNamee and Ryan 2009).
The type of policies and programmes offered for support of the incapacitated also influence the use of informal and formal help (Broese van Groenou et al. 2006). In general, welfare systems are more generous in Europe than in the USA (Börsch-Supan 2007). There have been recent changes in programmes for home care of the incapacitated in both Spain and the UK, which have increased the availability of cash payments for care at home. Spain supplies cash benefits to family care-givers of severely incapacitated people in order to maintain them at home. The UK has also introduced attendant allowances which can be used to provide intensive care for people at home (Organisation for Economic Co-operation and Development (OECD) 2005). These allowances supplement or replace in-kind services. Their aim is to enhance care at home, namely by serving as ‘routed wages’ (Yeandle and Steill 2007). In the USA, publicly provided home care is limited. Formal care policies in the USA are regulated by a mixture of state and federal regulations creating great variability across the country and across socio-economic groups in the availability of care paid for by medical or social programmes. In the USA, home care, as well as institutional care, is often only paid for by Medicare immediately after a hospital stay. In addition many programmes are means-tested and not open to all incapacitated persons (Feder, Komisar and Niefeld 2000). In the last two decades there was growth in the availability of Medicare-supported home health services; however, recent attempts to control costs have resulted in a reduction in availability (Murtaugh et al. 2003).
This study focuses on the role of household and family composition in the provision of informal and formal care for incapacitated adults aged 50+ in Spain, England and the USA. We examine (a) whether there are differences in the three countries in the likelihood of receiving help among incapacitated individuals; (b) whether there are differences in the type of care received; (c) whether the provision of care is related to differences in household and family composition; and (d) whether these differences vary by age and functioning status. In our descriptive analysis we examine differences by age in receipt of care, source and type of care in order to gain insight into how these differences might change with ageing. In our model-based analysis we examine the effect of household composition, availability of spouse and children, and level of disability on the source and type of care within each country in order to better understand how the influence of these factors affects the overall pattern of international differences in sources and types of care used by the incapacitated older population.
Data
This analysis uses three datasets: the Survey of Health, Ageing and Retirement in Europe for Spain (SHARE, 2006), the English Longitudinal Study of Ageing (ELSA, 2006–07), and the Health and Retirement Study for the USA (HRS, 2006). SHARE, ELSA and HRS were designed to be comparable and have comparable measurement of use of informal and formal care, living arrangements, family circumstances, health, functioning, and socio-economic characteristics. Weights are used with each of the three cross-sectional datasets to provide estimates for the national non-institutionalised population. The analysis focuses on care received among those living in the community because the sampling designs do not include institutionalised individuals.
Spain: Survey of Health, Ageing and Retirement in Europe
The SHARE data in Spain come from release 2.3.1 of the second wave of the SHARE (2006) database which is co-ordinated at the Mannheim Research Institute for the Economics of Ageing (MEA). SHARE provides probability samples of the non-institutionalised population of each country’s population aged 50+, and their spouses. Each country conducted its own national survey using a common questionnaire translated into the appropriate language (for more details, see Börsch-Supan, Hank and Jürges 2005). Our analysis of the presence of difficulties with activities of daily living (ADL) and instrumental activities of daily living (IADL) includes information for 2,170 individuals aged 50+ living in Spain. This includes 997 males and 1,173 females. The average age of the sample is 66.1 years old (see Table 1).
Table 1.
Descriptive statistics of sample aged 50 +
| Explanatory variables | Spain |
England |
USA |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Males | Females | Total | Males | Females | Total | Males | Females | |
| Number of individuals | 2,170 | 997 | 1,173 | 9,121 | 4,096 | 5,025 | 17,986 | 7,474 | 10,512 |
| Mean age | 66.1 | 65.0 | 67.1 | 65.8 | 65.5 | 66.1 | 68.4 | 68.1 | 68.7 |
| At least one ADL difficulty (%) | 12.8 | 9.4 | 15.8 | 19.2 | 17.9 | 20.2 | 18.5 | 15.3 | 20.9 |
| At least one IADL difficulty (%) | 20.5 | 14.4 | 25.9 | 20.0 | 15.7 | 23.5 | 33.2 | 25.5 | 39.1 |
| Marital status (%): | |||||||||
| Married | 72.7 | 80.7 | 66.0 | 64.8 | 74.0 | 57.2 | 62.8 | 77.0 | 52.1 |
| Widowed | l6.3 | 5.0 | 25.9 | 17.5 | 9.4 | 24.1 | 20.7 | 8.9 | 29.6 |
| Separated/divorced | 2.3 | 2.9 | 1.8 | 11.9 | 10.0 | 13.4 | 13.2 | 10.8 | 15.1 |
| Never married | 8.7 | 11.4 | 6.3 | 5.9 | 6.6 | 5.3 | 3.3 | 3.4 | 3.2 |
| Household composition (%): | |||||||||
| Living alone | 17.3 | 13.5 | 20.6 | 26.3 | 19.0 | 32.3 | 23.0 | 14.7 | 29.3 |
| Live with a spouse/co-habitant | 70.7 | 78.8 | 63.8 | 67.4 | 77.1 | 59.5 | 65.1 | 79.6 | 54.0 |
| Child in hh | 45.2 | 42.7 | 47.1 | 21.1 | 22.5 | 19.9 | 14.0 | 13.2 | 14.6 |
| Child outside hh | 764 | 73.9 | 78.5 | 77.7 | 75.5 | 79.5 | 91.2 | 91.4 | 91.0 |
| Mean number of children | 2.3 | 2.1 | 2.4 | 2.2 | 2.2 | 2.2 | 3.2 | 3.2 | 3.2 |
Notes: USA: United States of America. hh: household. ADL: activity of daily living. IADL: instrumental activity of daily living.
Source: Survey of Health, Ageing and Retirement in Europe for Spain (SHARE, 2006), English Longitudinal Study of Ageing (ELSA, 2006-07), and the Health and Retirement Study for the USA (HRS, 2006). Weights are applied.
England: English Longitudinal Study of Ageing
ELSA is a longitudinal multifaceted survey of ageing among persons aged 50 and older in England. ELSA began by following all age-appropriate respondents to the Health Survey for England for the years 1998, 1999 and 2001 along with their spouses and partners. The original sample was a nationally representative sample of non-institutionalised adults living in England who were born before 28 February 1952. In Wave 3, a cohort of people born between 1 March 1953 and 29 February 1956 were added to the sample in order to make it representative of those 50 and over. This analysis uses data from the third wave of ELSA, completed in 2006-07. The sample used to estimate ADL and IADL difficulty is composed of 9,121 individuals, 44.9 per cent male and 55.1 per cent female. The average age of the sample is 65.8 years old (see Table 1).
The USA: Health and Retirement Study
The HRS is a nationally representative longitudinal study representing the USA population over age 50. Beginning in 1992, the HRS has enrolled a new birth cohort every six years in order to maintain representation of the over 50 USA population. This analysis uses data for 2006 when the sample is 52 and older, but we include spouses who are 50 and 51 years of age. The initial sample is composed of 17,986 individuals, 41.6 per cent male and 58.4 per cent female. The average age of the sample is 68.4 years old (see Table 1).
Measures and method
Measures
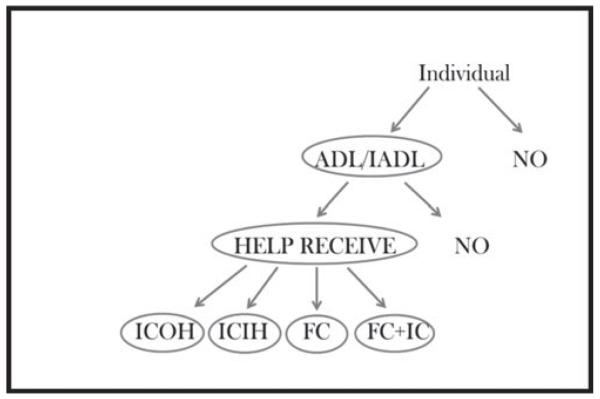
Figure 1 outlines how our analysis proceeds. We first examine how many people have ADL and IADL impairments in each country using the samples described above. Receipt of help is then examined among the sub-samples in each country who have difficulty performing at least one ADL or IADL task. The number of individuals in the sample for whom we examine receipt of help is 509 in |Spain, 2,372 in England and 7,008 in the USA. Finally, we consider the source of care among those who receive help; that is, among 384 persons in Spain, 1,600 English older persons and 2,756 respondents in the USA.
Figure 1.
Analysis stages.
Notes: ICOH: informal care outside the household. ICIH: informal care inside the household. FC: formal care. FC+IC: formal and informal care. ADL: activity of daily living. IADL: instrumental activity of daily living.
Having an ADL or IADL disability is defined similarly in the three countries as difficulty performing at least one task because of a physical, mental, emotional or memory problem. ADL tasks include bathing and showering, dressing, using the toilet, getting in and out of bed, walking across a room, and eating. IADL tasks include using a map, making phone calls, shopping, preparing meals, taking medications, doing work around the house, and managing money. The percentages having difficulty with an ADL or an IADL task are reported in Table 1.
Dependent variables
In all three countries, persons who report an ADL or IADL difficulty indicated whether they received help and from whom they received help for any of their disabilities. For ELSA and HRS, information on help received is explicitly provided by respondents immediately following the questions on ADL and IADL functioning for individuals with problems; for SHARE, questions on receipt of help for ADL and IADL activities are asked of all respondents. Help received for ADLs and IADLs is reported in response to questions as follows: ‘Thinking about the activities that you have problems with, does anyone ever help you with these activities?’ Two dichotomous variables are constructed indicating receiving help for either an ADL or IADL difficulty. Respondents, were then asked: ‘From whom do you receive assistance with personal care (e.g. bathing, dressing, using the toilet, getting in and out of bed, walking across a room, eating) or independent living functions (e.g. using a map, phone, shopping, food preparation, taking medications, work around the house, managing money)’. The kind of care received was coded as being from formal, informal sources or both, and the source of help received is classified as from inside or outside the household.
The kind of care and the source of care are used to divide recipients into four categories: i.e. only informal help from within the household, only informal help from outside the household, only formal help, or a combination of informal and formal help. Informal care is care provided to incapacitated persons for doing ADL or IADL, by family members or friends. It is not linked to a professional health-care system and it does not receive remuneration. Formal care is care provided by a public institution or entity, either profit-seeking or not-for-profit, or by a self-employed professional, either in the home or outside the home. Volunteers (without remuneration) who are part of an organisation are considered to be part of the formal sector (IMSERSO 2004).
Independent variables
Age is categorised as 50–64, 65–79, 80+. Gender is a binary variable, with men in the reference category. In the descriptive material we examine marital status using four categories: single, married, widowed and separated/divorced). In the regressions being married is a dichotomous variable (1=married, 0=not). We also indicate living arrangements by a dichotomous variable, living with a spouse or not. In the descriptive analysis we provide detail on average number of individuals per household. We also examine the number of surviving children at the time of the survey. In the regressions, we include indicators of whether there is a child living in the household of the older person and whether there is a child living outside the household. The expectation is that having children in and out of the household will be associated with a greater probability of receiving help.
Methods
We examine receipt of care among those who have ADL or IADL disability using a logistic regression model:
where Pr is the probability of getting help, α is the Y intercept, βi is the vector with regression coefficients, and Xi is a vector of explanatory variables. We then use a multinomial logit regression model, appropriate for responses that are categorical but unordered, to examine associations of the family and household variables with use of different types and sources of care. When fitting this model we consider the effect of selection into care receipt. The effect of independent variables on the relative likelihood of receiving ‘informal care from outside the household’, ‘informal care from inside the household’, ‘formal care’ or ‘a combination of both, formal and informal’ is determined. ‘Formal and informal care’ is the reference or omitted category. The multinomial logistic regression model is formulated as follows:
where βk is a k-vector of parameters and X is a vector of explanatory variables, and i is an individual, and the subscript j denotes the number of alternative categories and k denotes one category of the dependent variable.
Results
Descriptive information
Table 1 provides summary data on the total 50+ sample, incapacitated and not, for all variables for the three countries by gender. ADL difficulties are more common in the USA (18.5%) and England (19.2%) compared to Spain (12.8%); having at least one IADL difficulty is more common in the USA (33.2%), than Spain (20.5%) or England (20.0%). Women in the three countries have higher percentages with ADL and IADL difficulties than men.
More older persons are married in Spain (72.7%) than in England or the USA, where being separated or divorced is more common. Linked to marital status differences, fewer people were living alone in Spain (17.3%) than in England (26.3%) or the USA (23.0%) and more were living with a spouse or partner in Spain than in the other two countries (70.7% in Spain, 67.4% in England and 65.1% in the USA). Living with a child is much more frequent in Spain than in England or the USA (45.2% in Spain, 21.1% in England and 14.0% in the USA). But having a child who lives outside the household is higher in the USA (91.2%), than in Spain (76.4%) or England (77.7%). The mean number of children is similar in Spain and England, 2.3 and 2.2 children, respectively; while in the USA the number of children is higher, 3.2. These descriptive statistics reaffirm that patterns of living arrangements in Spain are characteristic of countries with strong familial culture – i.e. more married people, fewer people living alone, more children living in the household – as compared to the USA and England, where these patterns are not as common. They also confirm the greater overall availability of children to older persons in the USA.
The percentages of the total sample with some disability (either an ADL or IADL difficulty) range from the lowest 23.5 per cent in Spain, to 26.0 per cent in England, to the highest 40.0 per cent in the USA (Table 2). Among these incapacitated persons, the percentage receiving care is higher in Spain (75.4%) than in England (67.4%) or the USA (39.3%). This group receiving care is the group described in the rest of Table 2 for whom we now examine their demographic and household characteristics as well as the source and type of care received.
Table 2.
Percentage of total sample with activity of daily living (ADL) or instrumental activity of daily living (IADL) limitations and characteristics of persons aged 50 + with ADL and IADL limitations and those receiving care in Spain, England and the United States of America (USA)
| Variables | Spain |
England |
USA |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Males | Females | Total | Males | Females | Total | Males | Females | |
| N (%) of sample with at least one ADL or IADL difficulty |
509 (23.5) | 175 (17.6) | 334 (28.5) | 2,372 (26.0) | 928 (22.7) | 1,444 (28.8) | 7,008 (40.0) | 2,353 (31.5) | 4,655 (44.3) |
| N (%) of individuals with ADL or IADL difficulties receiving help |
384 (75.4) | 139 (79.4) | 245 (73.4) | 1,600 (67.4) | 588 (63.4) | 1,012 (70.1 ) | 2,756 (39.3) | 943 (40.1) | 1,813 (38.9) |
| Mean age | 75.4 | 74.1 | 76.1 | 72.0 | 71.8 | 72.1 | 73.4 | 73.6 | 73.3 |
| Mean number of individuals per dwelling |
2.28 | 2.51 | 2.16 | 1.86 | 2.04 | 1.77 | 2.34 | 2.33 | 2.34 |
| Married (%) | 57.4 | 82.1 | 45.1 | 52.8 | 70.8 | 42.6 | 49.9 | 71.7 | 37.7 |
| Household/family composition: | |||||||||
| Child in hh (%) | 40.4 | 35.6 | 42.4 | 16.1 | 15.3 | 16.6 | 21.1 | 14.9 | 24.4 |
| Child outside hh (%) | 82.2 | 84.6 | 81.0 | 82.0 | 83.6 | 81.1 | 89.0 | 89.5 | 88.8 |
| Mean number of children | 2.6 | 2.6 | 2.6 | 2.3 | 2.5 | 2.2 | 3.6 | 3.6 | 3.6 |
| Mean number of ADLs | 1.88 | 2.01 | 1.81 | 1.64 | 1.76 | 1.57 | 1.97 | 1.80 | 2.07 |
| Mean number of IADLs | 3.09 | 3.22 | 3.02 | 1.93 | 1.82 | 1.98 | 2.41 | 2.35 | 2.45 |
| Type and source of care (%): | |||||||||
| Informal care inside the hh | 63.7 | 71.0 | 60.1 | 55.0 | 69.8 | 47.1 | 63.9 | 76.1 | 57.1 |
| Informal care outside the hh: | 6.0 | 1.1 | 8.5 | 26.6 | 17.6 | 31.4 | 26.4 | 16.2 | 32.1 |
| Children | 73.9 | 57.7 | 79.0 | 59.9 | 57.4 | 60.7 | 59.0 | 47.8 | 62.1 |
| Siblings | 4.8 | 6.3 | 4.3 | 6.0 | 6.1 | 6.0 | 1.5 | 2.1 | 1.4 |
| Grandchildren | 1.7 | 0.0 | 2.3 | 11.2 | 9.6 | 11.7 | 39.3 | 35.8 | 40.2 |
| Relatives and friends | 26.5 | 39.0 | 22.5 | 50.7 | 45.2 | 52.3 | 46.0 | 50.8 | 44.6 |
| Formal care | 12.4 | 11.8 | 12.6 | 5.1 | 3.6 | 5.9 | 1.8 | 1.5 | 2.1 |
| Informal care and formal care | 17.9 | 16.0 | 18.8 | 13.3 | 9.0 | 15.6 | 7.9 | 6.3 | 8.7 |
Notes: SE: standard error. hh: household.
Source: See Table 1.
As expected, the incapacitated care recipients are an older subsample: average age of 75.4 in Spain, 72.0 in England and 73.4 in the USA. Within the incapacitated subgroup, the average number of individuals per dwelling is higher in Spain (2.28) and the USA (2.34) than in England (1.86). In all three countries, more than half of the males are married and less than half of the females are married. The percentage of the incapacitated living with a child in the household is considerably higher for Spain (40.4%) than England (16.1%) or the USA (21.1%), indicating that the incapacitated population in Spain is more likely to have multiple generations in their households. Having a child living outside the household is about the same in Spain and England, but slightly higher in the USA, where the mean number of children is the highest (3.6). In Spain and the USA, two-thirds of the incapacitated individuals who receive care, receive it from household members (63.7 and 63.9%, respectively); this percentage is lower for England (55.0%). Receipt of care from within the household is more likely for men than for women in all three countries. In Spain, 6 per cent of the incapacitated receive only informal help from outside the household and the providers are primarily children (73.9%) and then relatives and friends (26.5%). Little care is provided by siblings (4.8%) and grandchildren (1.7%). Help received from non-members of the household in England accounts for 26.6 per cent of care and is provided by children (59.9%), siblings (6.0%), grandchildren (11.2%), and relatives and friends (50.7%). In the USA, 26.4 per cent received informal care from outside the household and this is provided by children (59.0%), siblings (1.5%), grandchildren (39.3%), and relatives and friends (46.0%). The role of grandchildren appears to be greater in the USA than in either Spain or in England, and the role of friends and other relatives is greater in England and the USA than in Spain.
Among this group of incapacitated community dwellers, receipt of only formal care is most common in Spain (12.4%); it is lower in England (5.1%) and very low in the USA (1.8%). Finally, use of a combination of informal and formal care is higher in Spain (17.9%) when compared to England (13.3%) and the USA (7.9%). Overall among the incapacitated, the percentage of people who receive informal care is highest in the USA (90%) and lowest in Spain (70%); and the percentage receiving some formal care is highest in Spain (30%) and lowest in the USA (9%).
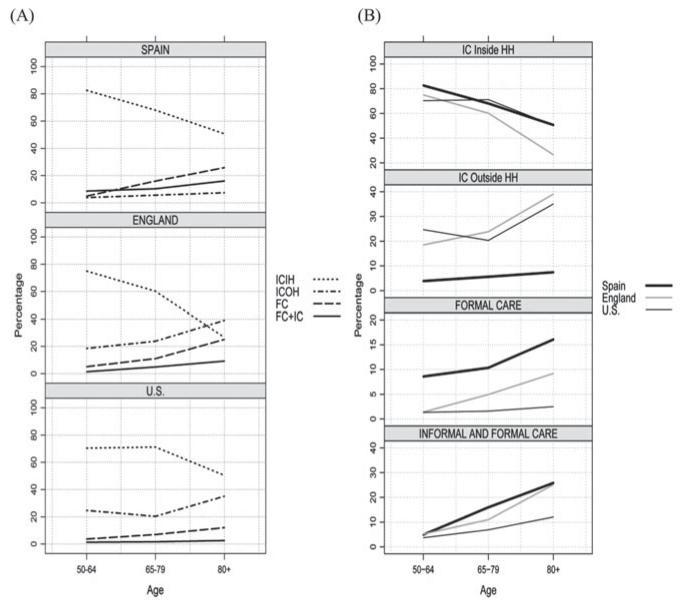
Use of care by age
To aid our understanding of changing care across the lifecycle, we present information on the type and source of care in two ways in Figure 2. Panel A shows how care type and source differ by age within each country for three ages (50–64, 65–79, 80+); Panel B shows how type and source of care by age differ across countries. Panel A shows that receiving only informal care from household members decreases with increasing age in all three countries but more sharply in Spain and England than in the USA. Panel B shows that the percentage receiving only informal care is higher for Spain in the first age group (83%) compared to England (75%) and the USA (70%). Among those 80 years of age and older, persons in Spain and the USA receive a higher percentage of care from household members (50.7 and 50.4%, respectively); in England this percentage drops markedly to 26.6 per cent.
Figure 2.
Distributions of care received by type and source of care by age in Spain, England and the USA, conditional on receiving help with at least one activity of daily living or instrumental activity of daily living.
Notes: ICIH: informal care inside the household (HH). ICOH: informal care outside the HH. FC: formal care. FC+IC: formal and informal care.
Source: See Table 1.
Panel A shows that receiving informal care from outside the household increases at older ages in all three countries. In England and the USA, this source of informal care is similar in importance to care from within the household for the oldest group; this is not true in Spain where care from inside the household remains the dominant source of care. Panel B shows that informal care received from non-household members is low in Spain at each age relative to the much higher levels in England and the USA. At higher ages, the loss of household member support in England and the USA appears to be supplemented by an increase in informal care from outside the household so that the percentage getting informal care from either inside or outside the household stays about the same. However, in Spain, the care received from outside the household is very flat across ages and the receipt of care from inside falls with age, resulting in fewer people getting only informal care at older ages.
Panel A shows that receiving only formal care increases with age in all three countries, but the increase is more pronounced in Spain where it is the second most important source of help received at the oldest age. In England and the USA this type of care remains the least prevalent category at each age. Panel B shows that use of only formal care is highest in Spain and increases markedly across age. Use of only formal care is moderate in England but increases markedly with age; in the USA, it is uniformly low across ages.
Finally, using a combination of informal and formal care is more prevalent in Spain and England and at higher ages. This combination of care accounts for about 20 per cent of care in Spain and England at the oldest age, but only about 8 per cent in the USA. At the oldest age, the use of any formal care is higher in Spain (about 25.8%) and England (25.1%) than the USA (12.1%).
Regression results
The results of logistic regressions examining receipt of help among the incapacitated in the three countries indicate that the association of socio-demographic and functioning indicators are differentially related to getting help across the three countries (Table 3). In Spain, only the number of IADL difficulties is related to a higher likelihood of getting care. In England, younger people are less likely to get care and women, married persons, those with more functioning problems and those with children in the household are more likely to receive care. In the USA, women are less likely than men to get care and those with children either in or out of the household are less likely to receive care. So in Spain, care receipt seems less related to demographic and living circumstances than in the other two countries.
Table 3.
Coefficients from logistic regressions on help received: Spain, England and the United States of America (USA)
| Variables | Spain (N = 509) |
England (N = 2,372) |
USA (N = 7,008) |
|||
|---|---|---|---|---|---|---|
| β | SE | β | SE | β | SE | |
| Age: | ||||||
| 50–64 | 0.14 | 0.3640 | −0.84✽✽✽ | 0.1660 | −0.33✽✽ | 0.1617 |
| 65–79 | 0.10 | 0.2936 | −0.39✽✽ | 0.1551 | −0.08 | 0.1425 |
| 80 + | – | – | – | – | – | – |
| Female | −0.31 | 0.2846 | 0.34✽✽✽ | 0.1188 | −0.23✽ | 0.1325 |
| Married | −0.07 | 0.2786 | 0.75✽✽✽ | 0.1248 | 0.45✽✽✽ | 0.1314 |
| Child in the hh | 0.21 | 0.2618 | 0.31✽ | 0.1658 | −0.37✽✽ | 0.1616 |
| Child outside hh | 0.01 | 0.2973 | 0.05 | 0.1486 | −1.65✽✽✽ | 0.4337 |
| Number of ADL difficulties |
0.08 | 0.0980 | 0.79✽✽✽ | 0.0710 | 0.12✽✽✽ | 0.0390 |
| Number of IADL difficulties |
0.39✽✽✽ | 0.0874 | 1.69✽✽✽ | 0.0945 | 1.38✽✽✽ | 0.0718 |
| Likelihood ratio test (chi-square) |
52.2362 | 871.2295 | 790.0319 | |||
Notes: SE: standard error. hh: household. ADL: activity of daily living. IADL: instrumental activity of daily living.
Source: See Table 1.
Significance levels:
p<0.1
p<0.05
p<0.01.
The results of the multinomial logit model examining the association of the type and source of care received for those with ADL and IADL difficulties who received help are shown in Table 4. The reference category in this analysis is those who receive both informal and formal care. Thus, the interpretation of all the coefficients on informal care from outside the household, informal care inside the household and formal care is relative to the use of a combination of formal plus informal care.
Table 4.
Coefficients from multinomial logistic regressions of type and source of care: Spain, England and the United States of America (USA)
| Variables | Spain (N=384) |
England (N= 1,600) |
USA (N=2,756) |
|||
|---|---|---|---|---|---|---|
| β | SE | β | SE | β | SE | |
| Informal care inside the household: |
||||||
| Age: | ||||||
| 50–64 | 1.41 ** | 0.708 | 2.20*** | 0.332 | 1.46*** | 0.325 |
| 65–79 | 0.53 | 0.382 | 1.30*** | 0.246 | 0.63*** | 0.210 |
| 80 + | – | – | – | – | – | – |
| Female | −0.32 | 0.410 | −0.64*** | 0.263 | −0.07 | 0.223 |
| Married | −0.01 | 0.405 | 3.06*** | 0.257 | 1.76*** | 0.226 |
| Child in the hh | 1.10*** | 0.389 | 2.78*** | 0.364 | 1.00*** | 0.259 |
| Child out hh | −1.11 ** | 0.479 | 0.46 | 0.292 | 0.26 | 0.482 |
| Number of ADLs | 0.08 | 0.106 | −0.19*** | 0.075 | −0.34*** | 0.052 |
| Number of IADLs | −0.35*** | 0.104 | −0.24*** | 0.079 | −0.28*** | 0.056 |
| Informal care outside the household: |
||||||
| Age: | ||||||
| 50–64 | 0.44 | 1.089 | 1.15*** | 0.333 | 1.31*** | 0.334 |
| 65–79 | 0.15 | 0.652 | 0.39* | 0.223 | 0.17 | 0.224 |
| 80 + | – | – | – | – | – | – |
| Female | 1.35 | 1.005 | −0.24 | 0.271 | 0.16 | 0.243 |
| Married | −0.75* | 0.689 | −1.46*** | 0.260 | −1.24*** | 0.261 |
| Child in the hh | 0.39 | 0.677 | −2.34*** | 0.586 | 0.40 | 0.266 |
| Child outside hh | 0.38 | 0.931 | 0.45* | 0.254 | 1.07** | 0.531 |
| Number of ADLs | −0.41 * | 0.285 | −0.42*** | 0.075 | −0.35*** | 0.055 |
| Number of IADLs | −0.69*** | 0.224 | −0.23*** | 0.083 | −0.25*** | 0.059 |
| Formal care: | ||||||
| Age: | ||||||
| 50-64 | −0.60 | 0.952 | −0.21 | 0.517 | 1.35** | 0.574 |
| 65-79 | −0.59 | 0.280 | 0.21 | 0.317 | 0.39 | 0.440 |
| 80 + | – | – | – | – | – | – |
| Female | 0.08 | 0.593 | −0.19 | 0.351 | −0.31 | 0.442 |
| Married | −0.13 | 0.563 | −0.69* | 0.381 | −1.30** | 0.553 |
| Child in hh | 0.16 | 0.552 | −1.09 | 0.780 | −0.47 | 0.694 |
| Child outside hh | −0.70 | 0.639 | −0.73*** | 0.325 | −0.66*** | 1.042 |
| Number of ADLs | 0.23 | 0.159 | −0.31*** | 0.129 | −0.47*** | 0.126 |
| Number of IADLs | −0.59*** | 0.149 | −0.38*** | 0.127 | −0.58*** | 0.150 |
| Likelihood ratio test (chi-square) |
393.4 | 913.7 | 1,486.8 | |||
Notes: SE: standard error. hh: household. ADL: activity of daily living. IADL: instrumental activity of daily living. “Formal and informal care” is the omitted category.
Source: See Table 1.
Significance levels:
p<0.1
p<0.05
p<0.01.
Informal care inside the household
Being married means one is significantly more likely to receive only informal care from inside the household in England and the USA, but not in Spain. This means that marriage does not protect the incapacitated in Spain from needing to combine informal and formal care. Having a child inside the household is linked to receiving more care from inside the household in all three countries. Having a child outside the household is linked to a lower likelihood of an incapacitated person receiving informal care from within the household in Spain relative to the likelihood of a combination of formal care and informal care.
Informal care from inside the household is more likely to be received by younger persons in all three countries relative to receiving care from a combination of sources. This is likely to be linked to the fact that older persons might require more technical care. Gender does not affect the receipt of this type of care, except in England where females are significantly less likely to receive only informal care inside the household. Having more ALDs or IADLs reduces significantly the likelihood of only receiving informal help from inside the household as compared to receiving both formal and informal help.
Informal care outside the household
In all three countries, being married is linked to being significantly less likely to be receiving informal care only from outside the household relative to the likelihood of receiving both formal and informal care. This indicates that married people who receive informal care from outside the household are more likely to supplement this care with formal care than to have only care from outside the household. Having a child inside the household is also linked to being significantly less likely to be receiving informal care from outside the household in England; an indication that a person in the household is linked to less receipt of formal care. Having a child outside the household is related to being more likely to be receiving informal care from outside the household in England and the USA, an indication that these children are providing care. This indicates that, in these countries, having a child outside the household reduces the likelihood of needing to supplement that care with formal care. This is not true in Spain.
In England and the USA, younger persons with impairments are significantly more likely to receive informal care from outside the household relative to receiving a combination of care. Gender does not significantly affect receipt of this type of care. Having more ADL or IADL difficulties is associated with less use of only informal care from outside the household as compared to receiving a combination of informal and formal care in each of the three countries, indicating an increasing need to use combined sources of care with more disability.
Formal care
Being married means one is significantly less likely to receive only formal care in England and the USA but there is no relationship between marriage and receiving only formal care in Spain. Having a child outside the household also reduces the likelihood of receiving only formal care in both the USA and England but not in Spain. Having a child in the household does not affect the likelihood of receiving only formal care relative to the combination of formal and informal in any country.
Finally, receiving only formal care relative to a combination of sources is more likely at younger ages in the USA. Gender has no effect on receiving formal help across these countries. Having more ADL or IADL difficulties is linked to a lower likelihood of using only formal care relative to a combination of sources of care.
Discussion
The percentage of the 50+ population receiving some form of help with ADL and IADL difficulties is similar across countries: 17.7 per cent in the USA, 17.5 per cent in England and 15.3 per cent in Spain. However, because there are more incapacitated people in the USA non-institutional population, our data show that the likelihood that an incapacitated person will receive care is much higher in Spain (75.4%) than in England (67.4%) or the USA (39.3%).
While care-giving is primarily provided by family members in all three countries, the sources and types of care are quite different across these three countries. In all these countries, people who live in the household are the most likely to provide care. In Spain, most of those who are getting informal care get it from inside the household. Because care provided from outside the household is higher in England and the USA, the overall provision of informal care is greater in England and the USA than in Spain. Children are the most important source of care from outside the household in all three countries, but grandchildren also play an important role in the USA, as do relatives and friends in both England and the USA (Banks et al. 2010), indicating that where living arrangements are less multigenerational, care-giving is provided from outside the household.
In spite of having similar household sizes among the incapacitated in Spain and the USA, formal care use is highest among the incapacitated in Spain and lowest in the USA where provision of formal care paid for by social programmes is weakest. Generous provision of formal care, as in Spain, appears to result in greater usage even when there are potential care-givers in the household. In Spain being married does not reduce the likelihood that one will receive formal care; nor does having a child outside the household appear to reduce the likelihood of formal care or increase the likelihood of getting informal care from within the household in Spain. The fact that being married in Spain is not linked to more care from inside the household may reflect a difference in gender roles in Spain from those in the USA and England; so that spousal care is not as likely to be provided from a man to a woman. The differences in the effect of children in Spain may indicate that living with a child has very different implications in Spain than in the other two countries. For instance, where the culture emphasises intergenerational residence, such residence may be linked to inheritance and may come with expectations for care from the co-resident child but not the non-resident child. In the USA, research has shown that when parents and children live together, it is often the child who has difficulties living independently who stays in the parental home; this would be less likely to be connected to inheritance and to expectations of care (Crimmins and Ingegneri 1990).
Clearly family care-givers have a very significant role in the three countries; but the extent of their role appears to depend on the policies toward providing care within each country. Our results imply that where formal care is more readily available, as in Spain and England, care-givers may be willing to relinquish or supplement their informal roles with formal care as disability increases. Spain is the country where formal care is used most extensively even though it is the country with the greatest availability of potential care-givers in the home. Our results are similar to others in indicating less care-giving between spouses in Spain than in other countries (Huber et al. 2009). It also appears that children outside the household have a reduced role in Spain relative to other countries. This all points to the complexity of factors determining long-term care including past fertility, living arrangements, cultural experiences and policies directed toward care.
Since the institutional population is not included in our analysis, our results apply only to the community-dwelling population and not the institutional population. Recent figures, however, indicate little difference in the likelihood of institutionalisation among these countries. Spain actually has the highest level of institutionalisation for the population 65 years and older at 5.8 per cent (EDAD 2008); for the UK and the USA this figure is 5.1 and 4.3 per cent, respectively (OECD 2005). Because all institutionalised persons are receiving formal care, we can still conclude that incapacitated people in Spain receive more formal care than in the USA and England.
There are some limitations to the present study that should be noted here. The smaller sample size of the Spanish sample could result in fewer significant relationships. Additionally, we could better understand the roles of children in each country if we had information on the specific reasons behind intergenerational living arrangements and the geographical distance separating respondents and non-resident children (Bonsang 2009; Charles and Sevak 2005; Donovan et al. 2011). Moreover, the link between reports of help received and ADL and IADL incapacity in SHARE is not as explicit as in ELSA and HRS. While we believe the effect of this difference on our results will be minimal, it is possible that people reported more help received in Spain without a direct link to the disability sequence. In addition, we were not able to incorporate income into the analysis because it was not collected in a comparable manner in the three surveys. However, we should note that adding controls for education levels in our regression models did not significantly change the results and education was not a significant predictor of type of care used except in England where higher education resulted in less use of informal care, both inside and outside the household.
The use of these three datasets allows us to better understand the complex ways in which care for the older population is provided in three different cultural, economic and policy milieus. Care receipt seems to be less related to socio-demographic links and living circumstances in Spain than in the other two countries, perhaps indicating a tendency in familistic countries for care-giving within families to be more integrated into the fabric of society and less influenced by either the needs of recipients or the characteristics of care-givers. However, the clear link between greater generosity of formal programmes and greater use in a country like Spain in spite of their familistic living arrangements indicates a willingness even in familistic societies to adopt formal care-giving if it is freely available.
Given the increasing life expectancy at older ages in the last few decades, and the growing number of older people with functioning problems (Lafortune and Balestat 2007), the demand for care-giving is increasing in most countries and this increase poses a growing challenge for families, social systems and the economic wellbeing of nations. The results of this analysis demonstrate the complexity of the factors determining the availability and use of care; and the need to consider the feasibility of policies within a given social and familial context.
Acknowledgements
This work was started while Aïda Solé-Auró was visiting the Academic Unit of Health Economics, Leeds Institute of Health Sciences, University of Leeds (Leeds, U.K.). Aïda Solé-Auró thanks Professor Claire Hulme and Professor Sandy Tubeuf for their help and for hosting her in their unit. Most of the work was completed while Aïda Solé-Auró was a postdoctoral fellow at the Center on Biodemography and Population Health at the University of Southern California. Financial help from the Spanish Ministry of Science and Innovation project, ECO2010-21787-C03-01, Beatriu de Pinós grant (2010–2012), and the National Institute on Aging of the United States (P30AG017265) are gratefully acknowledged. The SHARE data collection has been primarily funded by the European Commission through the 5th framework programme (project QLK6-CT-2001-00360 in the thematic programme Quality of Life). Further support by the European Commission through the 6th framework programme (projects SHARE-I3, RII-CT-2006-062193, as an Integrated Infrastructure Initiative, COMPARE, CIT5-CT-2005-028857, as a project in Priority 7, Citizens and Governance in a Knowledge Based Society, and SHARE-LIFE (CIT4-CT-2006-028812)) and through the 7th framework programme (SHARE-PREP (No211909) and SHARE-LEAP(No 227822)) is gratefully acknowledged. Substantial co-funding for add-ons such as the intensive training programme for SHARE interviewers came from the U.S. National Institute on Aging (U01 AG09740-13S2, P01 AG005842, P01 AG08291, P30 AG12815, R21 AG025169, Y1-AG-4553-01, IAG BSR06-11 and OGHA 04-064). Support for the HRS data collection was primarily provided by the national Institute on Aging (U01 AG009740).
References
- Banks J, Berkman L, Smith JP, Avendano M, Glymour M. Do cross-country variations in social integration and social interactions explain differences in life expectancy in industrialized countries? In: Crimmins EM, Preston SH, Cohen B, editors. International Differences in Mortality at Older Ages: Dimensions and Sources. National Academies Press; Washington DC: 2010. pp. 217–56. [PubMed] [Google Scholar]
- Bolin K, Lindgren B, Lundborg P. Informal and formal care among single-living elderly in Europe. Health Economics. 2008;17(3):393–409. doi: 10.1002/hec.1275. [DOI] [PubMed] [Google Scholar]
- Bonsang E. Does informal care from children to their elderly parents substitute for formal care in Europe? Journal of Health Economics. 2009;28(1):143–54. doi: 10.1016/j.jhealeco.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Börsch-Supan A. European Welfare State Regimes and Their Generosity Toward the Elderly. Levy Economics Institute; Annandale-on-Hudson, New York: 2007. [Google Scholar]
- Börsch-Supan A, Hank K, Jürges H. A new comprehensive and international view on ageing. European Journal of Ageing. 2005;2(4):245–53. doi: 10.1007/s10433-005-0014-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branch LG, Wetle TT, Scherr PA, Cook NR, Evans DA, Hebert LE, Masland EN, Keough ME, Taylor JO. A prospective study of incident comprehensive medical home care use among the elderly. American Journal of Public Health. 1988;78(3):255–9. doi: 10.2105/ajph.78.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broese van Groenou M, Glaser K, Tomassini C, Jacobs T. Socio-economic status differences in older people’s use of informal and formal help: a comparison of four European countries. Ageing & Society. 2006;26(5):745–66. [Google Scholar]
- Charles KK, Sevak P. Can family caregiving substitute for nursing home care? Journal of Health Economics. 2005;24(6):1174–90. doi: 10.1016/j.jhealeco.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Comas-Herrera A, Wittenberg R, Costa-Font J, Gori C, Di Maio A, Patxot C, Pickard L, Pozzi A, Rothgang H. Future long-term care expenditure in Germany, Spain, Italy and the United Kingdom. Ageing & Society. 2006;26(2):285–302. [Google Scholar]
- Crimmins EM, Ingegneri DG. Interaction and living arrangements of older parents and their children. Past trends, present determinants, future implications. Research on Aging. 1990;12(1):3–35. doi: 10.1177/0164027590121001. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, Solé-Auró A. Gender differences in health: results from SHARE, ELSA and HRS. European Journal of Public Health. 2011;21(1):81–91. doi: 10.1093/eurpub/ckq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan R, Williams A, Stajduhar K, Brazil K, Marshall D. The influence of culture on home-based family caregiving at end-of-life: a case study of Dutch reformed family care givers in Ontario, Canada. Social Science & Medicine. 2011;72(3):338–46. doi: 10.1016/j.socscimed.2010.10.010. [DOI] [PubMed] [Google Scholar]
- Doty P. Family care of the elderly: the role of public policy. The Milbank Quarterly. 1986;64(1):34–75. [PubMed] [Google Scholar]
- EDAD . Survey on Disability, Personal Autonomy and Dependency Situations. 2008. http://www.ine.es/jaxi/menu.do?type=pcaxis&path=/t15/p418&file=inebase&L=1 [Google Scholar]
- Elwert F, Christakis NA. The effect of widowhood on mortality by the causes of death of both spouses. American Journal of Public Health. 2008;98(11):2092–8. doi: 10.2105/AJPH.2007.114348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feder J, Komisar HL, Niefeld M. Long-term care in the United States: an overview. Health Affairs. 2000;19(3):40–56. doi: 10.1377/hlthaff.19.3.40. [DOI] [PubMed] [Google Scholar]
- Gans D, Silverstein M. Norms of filial responsibility for aging parents across time and generations. Journal of Marriage and Family. 2006;68(4):961–76. [Google Scholar]
- García JR, Prieto-Flores M-E, Rosenberg MW. Health services use by older people with disabilities in Spain: do formal and informal care matter? Ageing & Society. 2008;28(7):959–78. [Google Scholar]
- Glaser K. The living arrangements of elderly people. Reviews in Clinical Gerontology. 1997;7(1):63–72. doi: 10.1017/s0959259800003191. [DOI] [PubMed] [Google Scholar]
- Greene VL. Substitution between formally and informally provided care for the impaired elderly in the community. Medical Care. 1983;21(6):609–19. doi: 10.1097/00005650-198306000-00003. [DOI] [PubMed] [Google Scholar]
- Guillén M, Albarrán I, Alcañiz M, Ayuso M, Blay D, Monteverde M. Longevidad y dependencia en España: consecuencias sociales y económicas. Fundación BBVA; Madrid: 2006. [Google Scholar]
- Himes CL. Future caregivers: projected family structures of older persons. Journal of Gerontology. 1992;47(1):S17–26. doi: 10.1093/geronj/47.1.s17. [DOI] [PubMed] [Google Scholar]
- Holden KC, Kuo HHD. Complex marital histories and economic well-being: the continuing legacy of divorce and widowhood as the HRS cohort approaches retirement. The Gerontologist. 1996;36(3):383–90. doi: 10.1093/geront/36.3.383. [DOI] [PubMed] [Google Scholar]
- Huber M, Rodrigues R, Hoffmann F, Gasior K, Marin B. Facts and Figures on Long-term Care Europe and North America. European Centre for Social Welfare Policy and Research; Vienna: 2009. [Google Scholar]
- IMSERSO . Situación y evolución del apoyo informal a los mayores en España. Informe de resultados; Madrid: 2004. http://www.imsersomayores.csic.es/documentacion/biblioteca/registro.htm?id=51002. [Google Scholar]
- Jiménez-Martín S, Prieto C. The trade-off between formal and informal care in Spain. The European Journal of Health Economics. 2012;13(4):461–90. doi: 10.1007/s10198-011-0317-z. [DOI] [PubMed] [Google Scholar]
- Kemper P. The use of formal and informal home care by the disabled elderly. Health Services Research. 1992;27(4):421–51. [PMC free article] [PubMed] [Google Scholar]
- Lafortune G, Balestat G. Trends in Severe Disability Among Elderly People Assessing the Evidence in 12 OECD Countries and the Future Implications. Organisation for Economic Co-operation and Development; Paris: 2007. [Google Scholar]
- Litwin H, Attias-Donfut C. The inter-relationship between formal and informal care: a study in France and Israel. Ageing & Society. 2009;29(1):71–91. doi: 10.1017/S0144686X08007666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macunovich D, Easterlin R, Schaeffer C, Crimmins EM. Echoes of the baby boom and bust: recent and prospective changes in living alone among elderly widows in the United States. Demography. 1995;32(1):17–28. [PubMed] [Google Scholar]
- Mentzakis E, McNamee P, Ryan M. Who cares and how much: exploring the determinants of co-residential informal care. Review of Economics of the Household. 2009;7(3):283–303. [Google Scholar]
- Murtaugh CM, McCall N, Moore S, Meadow A. Trends in Medicare home health care use: 1997-2001. Health Affairs. 2003;22(5):146–56. doi: 10.1377/hlthaff.22.5.146. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development (OECD) Health at a Glance OECD Indicators. OECD; Paris: 2005. 2005. [Google Scholar]
- Palloni A, editor. Living Arrangements of Older Persons. Population Bulletin of the United Nations; New York: 2001. [Google Scholar]
- Reher DS. Family ties in western Europe: persistent contrasts. Population and Development Review. 1998;24(2):203. [Google Scholar]
- Schaefer C, Quesenberry CP, Wi S. Mortality following conjugal bereavement and the effects of a shared environment. American Journal of Epidemiology. 1995;141(12):1142–52. doi: 10.1093/oxfordjournals.aje.a117387. [DOI] [PubMed] [Google Scholar]
- Silverstein M, Gans D, Lowenstein A, Giarrusso R, Bengtson V. Older parent-child relationships in six developed nations: comparisons at the intersection of affection and conflict. Journal of Marriage and Family. 2010;72(4):1006–21. doi: 10.1111/j.1741-3737.2010.00745.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistical Office of the European Commission . Europe in Figures – Eurostat Yearbook 2010. European Commission; Luxembourg: 2010. [Google Scholar]
- Tomassini C, Glaser K, Wolf DA, Broese van Groenou MI, Grundy E. Living arrangements among older people: an overview of trends in Europe and the USA. Population Trends. 2004;115:24–34. [PubMed] [Google Scholar]
- United States Bureau of the Census . Census of Governments. [Accessed October 2011]. 2009. Available online at http://www.census.gov/govs/cog. [Google Scholar]
- Van Houtven CH, Norton EC. Informal care and health care use of older adults. Journal of Health Economics. 2004;23(6):1159–80. doi: 10.1016/j.jhealeco.2004.04.008. [DOI] [PubMed] [Google Scholar]
- Wolf DA. Changes in the living arrangements of older women: an international study. The Gerontologist. 1995;35(6):724–31. doi: 10.1093/geront/35.6.724. [DOI] [PubMed] [Google Scholar]
- Yeandle S, Steill B. Issues in the development of the direct payments scheme for older people in England. In: Ungerson C, Yeandle S, editors. Cash for Care in Developed Welfare States. Palgrave; Basingstoke, UK: 2007. pp. 104–36. [Google Scholar]