Abstract
Purpose
To compare long-term postoperative outcomes when performing an adjustment to achieve a desired immediate postoperative alignment versus simply tying off at the desired immediate postoperative alignment when using adjustable sutures for strabismus surgery.
Methods
We retrospectively identified 89 consecutive patients who underwent a reoperation for horizontal strabismus using adjustable sutures and also had a 6-week and 1-year outcome examination. In each case, the intent of the surgeon was to tie off and only to adjust if the patient was not within the intended immediate postoperative range. Postoperative success was predefined based on angle of misalignment and diplopia at distance and near.
Results
Of the 89 patients, 53 (60%) were adjusted and 36 (40%) were tied off. Success rates were similar between patients who were simply tied off immediately after surgery and those who were adjusted. At 6 weeks, the success rate was 64% for the nonadjusted group versus 81% for the adjusted group (P = 0.09; difference of 17%; 95% CI, −2% to 36%). At 1 year, the success rate was 67% for the nonadjusted group versus 77% for the adjusted group (P = 0.3; difference of 11%; 95% CI, −8% to 30%).
Conclusions
Performing an adjustment to obtain a desired immediate postoperative alignment did not yield inferior long-term outcomes to those obtained by tying off to obtain that initial alignment. If patients were who were outside the desired immediate postoperative range had not been not adjusted, it is possible that their long-term outcomes would have been worse, therefore, overall, an adjustable approach may be superior to a nonadjustable approach.
The potential advantages of adjustable suture strabismus surgery have been debated since the technique was popularized by Jampolsky1 in the 1970s. The underlying premise in adjustable suture strabismus surgery is that controlling the immediate postoperative alignment can determine the long-term outcome. Previous studies of adjustable sutures are comparative case series; there have been no adequately powered randomized controlled trials. Some retrospective studies indicate superiority of adjustable sutures compared to fixed sutures,2–4 whereas others suggest the opposite or are neutral.5–7 In the present study, we adopted an alternative methodology, comparing outcomes in a cohort of patients undergoing adjustable suture surgery, some of whom were simply tied off at the time of adjustment and some of whom were adjusted. This comparison allows evaluation of whether or not adjustment per se is inferior to simply tying the suture without adjustment. Since the aim of adjustment is to achieve an alignment that corresponds to a target range, we predicted that there would be no difference between success rates in patients who were adjusted and those that were tied-off.
Subjects and Methods
Mayo Clinic Institutional Review Board approval was obtained for this study. All procedures and data collection were conducted in a manner compliant with the Health Insurance Portability and Accountability Act (HIPAA).
To study a uniform patient cohort in whom adjustable sutures are commonly used by many surgeons, we identified patients who underwent surgery for horizontal strabismus following any previous strabismus surgery (for example in childhood). All surgeries performed by the same surgeon (JMH) from January 2001 to December 2010 were retrospectively reviewed. Only patients who had surgery on horizontal rectus muscles and who had both 6-week and 1-year follow-up examinations were included, in order to assess both short- and long-term outcomes. For the few patients who had more than one reoperation, only the first reoperation was included. Patients with vertical transposition of the horizontal rectus muscles were excluded.
Classification of Patients
Patients were broadly classified into one of four strabismus types on the basis of preoperative examination (esodeviation or exodeviation and with or without probable potential for bifoveal fusion): (1) esodeviations with fusion potential, (2) esodeviations without fusion potential, (3) exodeviations with fusion potential, (4) exodeviations without fusion potential. These categories reflect the different surgical target angles in the surgical plan (Table 1). The presence of fusion potential was assessed based on documentation in the medical record. History of early-onset childhood strabismus was assumed to indicate no bifoveal fusion potential. A sensory fusion response to prism in space with motor amplitudes or fusion on the synoptophore was assumed to indicate potential for bifoveal fusion.
Table 1.
Target angles defined depending on patient’s strabismus typea
| Esodeviations | Exodeviations | |||
|---|---|---|---|---|
| Fusion potential | No fusion potential | Fusion potential | No fusion potential | |
| Distanceb | 0 PD to 6 PD XT | 2 PD to 8 PD ET | 2 PD to 8 PD ET | 4 PD to 14 PD ET |
| Nearc | 0 PD to12 PD XT | 4 PD XT to 8 PD ET | 10 PD XT to 8 PD ET | 4 PD XT to 14 PD ET |
ET, esotropia; PD, prism diopters; XT, exotropia.
Rare exceptions to target angles were made for patients with internuclear ophthalmoplegia, convergence insufficiency, and third nerve palsies, where the target angle was a greater ET (n = 7), when a patient had an atypical ET or XT drift after previous surgery (n = 4), and when appearance of the strabismus overrode measurements in nonfusing patients (n = 2).
Distance target ranges were observed when Krimsky measurements were used to optimize appearance for patients with abnormal angle kappa or when visual acuity precluded prism testing.,.
The distance target range was prioritized; the near target range became important in cases where the near XT exceeded the target range.
To enable appropriate assessment of outcome, patients were also classified according to preoperative presence and type of diplopia as diplopic, nondiplopic, or atypical diplopic, using previously published criteria.8 This classification system allows for differential application of diplopia criteria depending on preoperative diplopia status, using Table 2 for diplopic and non-diplopic patients but allowing persistent diplopia postoperatively in patients with previous childhood strabismus and loss of suppression (atypical diplopia), where diplopia is less likely to be addressed by surgery.
Table 2.
Criteria used to define postoperative clinical outcomes as success, partial success, or failure postoperatively in patients undergoing strabismus surgery
| Success (All criteria must be met) |
Partial successa (All criteria must be met) |
Failurea (If any one criterion met) |
|
|---|---|---|---|
| Angle of deviationb | <10 PD distance straight ahead and near | ≤15 PD distance straight ahead and near (without prism) | >15 PD distance straight ahead or near (without prism) |
| Diplopia/visual confusionc | None or rare distance straight ahead and reading | None, rare, or sometimes distance straight ahead and reading | Always or often distance straight ahead and reading |
| Prism | Not allowed | Allowed | N/A |
| Bangerter foil/occlusion | Not allowed | Not allowed | Allowed |
N/A, not applicable; PD, prism diopters.
For classification as success or partial success, all listed criteria had to be met, for classification as failure only one criterion had to be met. If the criteria for more than one outcome group was met, the patient was allocated to the group with the better outcome.
Measurements used by order of preference: simultaneous prism cover test, prism and alternate cover test, or Krimsky. If abnormal angle kappa was present, Krimsky was used as the angle of deviation to assess outcome.
Diplopia criteria were not used in patients with atypical diplopia who presented with infantile strabismus and diplopia, where elimination of diplopia cannot be a primary goal (12 of 89 patients).
Surgery and Adjustment
Surgery was performed on the horizontal muscles only using recession, resection, and/or advancement techniques, with at least one muscle on adjustable sutures. For the majority of patients adjustable sutures were 6-0 polyglactin 910, but in a few cases of very large recession, 6-0 nonabsorbable polyester sutures were used. The adjustment was performed under topical anesthesia on the day of the surgery in all but one case, in which adjustment took place on the following day. In every case, the intent of the surgeon was to tie off and only to adjust if the patient was not within the intended immediate postoperative range, which differed depending on the patient’s classification at the preoperative examination (Table 1). Target angles were based on prism and alternate cover tests. In rare cases, exceptions to the target angle were made for patients with internuclear ophthalmoplegia, convergence insufficiency, and third nerve palsies (n = 7) where the target angle was a greater esotropia, when a patient had an atypical esotropia or exotropia drift after previous surgery (n = 4), and when appearance of the strabismus overrode measurements in nonfusing patients (n = 2).
Classification of 6-week and 1-year Outcomes
Surgical outcome at the 6-week (window 21 days to 150 days, actual range 31 to 138 days, median 51 days) and 1-year (window 151 days to 730 days, actual range 167 days to 710 days, median 369.5 days) follow-up visits was defined using angle of deviation and diplopia criteria previously described8 (Table 2). Angle of deviation data were taken from the simultaneous prism cover test at distance (3 m) and near (1/3 m), where available. If simultaneous prism cover test data were not available, prism and alternate cover test data were used. If visual acuity was too poor for an accurate cover test, or if an abnormal angle kappa was present, Krimsky measurements were used. Frequency of diplopia in distance straight ahead gaze and reading gaze was judged based on medical history (73%) or assessed using a diplopia questionnaire (27%).9 At both the 6-week and 1-year outcome visits, patients were classified as either success, partial success, or failure by applying predetermined angle and diplopia criteria (Table 2).
The proportion of patients classified as “success” was calculated overall and for each predefined strabismus type (Table 3) at both 6 weeks and 1 year postoperatively. Success rates were compared between patients who were adjusted and those who were not, overall and for each strabismus type, using the Fisher exact test.
Table 3.
Classification of strabismic patients based on diplopia at the preoperative examination
| Esodeviations | Exodeviations | ||||
|---|---|---|---|---|---|
| Fusion potential | No fusion potential | Fusion potential | No fusion potential | Total | |
| Diplopic | 18 | 2a | 13 | 0 | 33 |
| Nondiplopic | 0 | 11 | 2 | 31 | 44 |
| Atypical diplopic | N/A | 6 | N/A | 6 | 12 |
| Total | 18 | 19 | 15 | 37 | 89 |
One patient with visual confusion was grouped with the diplopic patients since the goal of surgery was to eliminate the symptoms of visual confusion
Results
A total of 89 patients who underwent surgery for a horizontal deviation after previous surgery were included. Median patient age was 42 years (range, 12–83 years); 60 (67%) were female, and 81 (91%) self-reported their race as white. Median visual acuity was 20/20 (range, 20/15–20/40) in the better eye and 20/25 (range, 20/15 to counting fingers) in the worse eye. Alignment before surgery ranged from an exotropia of 55Δ to an esotropia of 60Δ at distance using the prism and alternate cover test. Small vertical deviations were allowed but were only included if the vertical deviation was not addressed as part of the surgical plan because either it did not need to be corrected to attain fusion or because it was not noticeable to the nonfusing patient. Diagnoses included consecutive, recurrent, and residual esotropia and exotropia, cranial nerve palsies, divergence insufficiency, intermittent exotropia, convergence insufficiency (CI), sensory esotropia, Duane syndrome, decompensated accommodative esotropia, dissociated horizontal deviations, internuclear ophthalmoplegia (INO), and Graves’ eye disease. The number of patients in each of the three diplopia categories and in each of the four strabismus type categories is presented in Table 3.
Overall, of the 89 patients, 53 (60%) were adjusted and 36 (40%) were tied off. At both the 6-week and 1-year visits, there was a numerically higher success rate in the patients that were adjusted compared with those tied off, although differences did not reach statistical significance (81% vs 64%, P = 0.09 at 6 weeks [difference of 17%; 95% CI, −2% to 36%] and 77% vs 67%, P = 0.3 at 1 year [difference of 11%; 95% CI, −8% to 30%]).
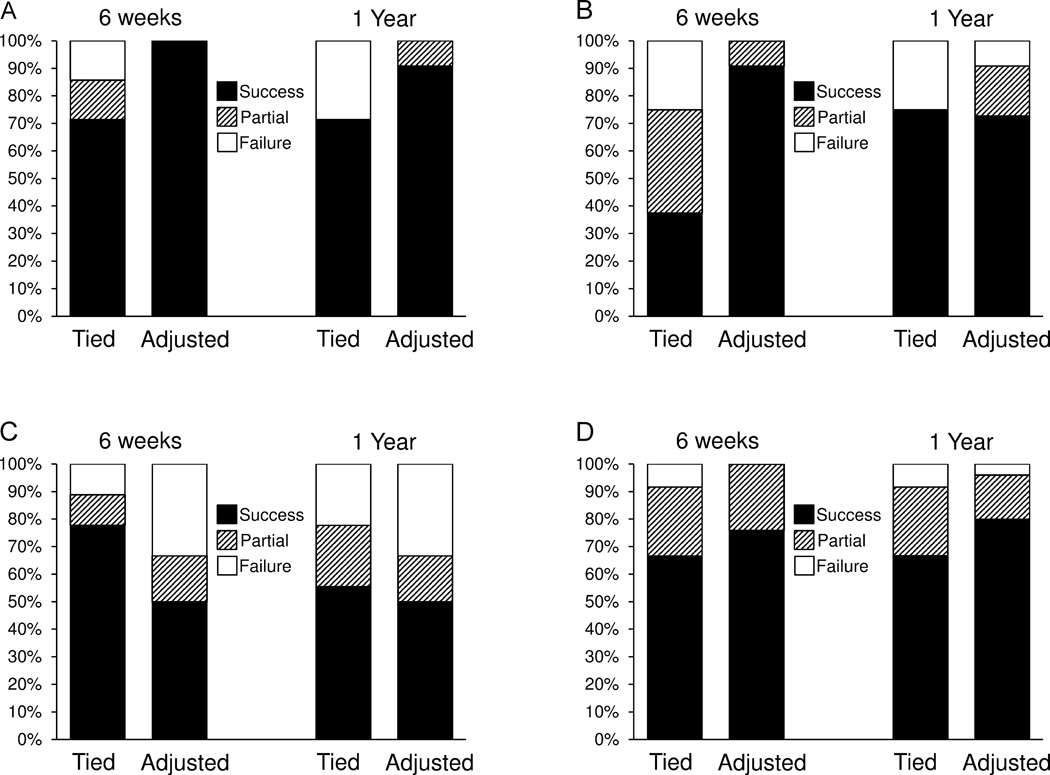
Esodeviations with Fusion Potential
A total of 11 esotropic patients (61%) with probable bifoveal fusion were adjusted, and 7 (39%) were tied off. At 6 weeks and 1 year postoperatively, there was a numerically higher success rate in the patients who were adjusted compared with those tied off, although differences did not reach statistical significance (6 weeks, 100% vs 71%, P = 0.1 [difference of 29%; 95% CI, −5% to 62%]; 1 year, 91% vs 71%, P = 0.5 [difference of 20%; 95% CI, −18% to 57%]; Figure 1A).
FIG. 1.
Surgical outcomes (success, partial success, or failure) divided by type in tied-off and adjusted patients at 6-week and 1-year postoperatively. A, Esodeviations: fusion potential. B, Esodeviations: no fusion potential. C, Exodeviations: fusion potential. D, Exodeviations: no fusion potential).
Esodeviations without Fusion Potential
A total of 11 esotropic patients (58%) without bifoveal fusion were adjusted, and 8 (42%) were tied off. At 6 weeks postoperatively, there was a higher success rate in the patients who were adjusted compared with those tied off (91% vs 38%, P = 0.04 [difference of 53%; 95% CI, 16% to 91%]). At 1 year postoperatively, there was a comparable success rate in patients who were adjusted compared with those tied off (73% vs 75%, P = 1.0 [difference of −2%; 95% CI, −42% to 38%]; Figure1B).
Exodeviations with Fusion Potential
A total of 6 exotropic patients (40%) with probable bifoveal fusion were adjusted, and 9 (60%) were tied off. At 6 weeks postoperatively, there was a numerically lower success rate in the patients who were adjusted compared with those tied off (50% vs 78%, P = 0.3 [difference of −28%; 95% CI, −76% to 21%]) although differences did not reach statistical significance. At 1 year postoperatively, success rates were comparable for patients who were adjusted compared with those who were tied off (50% vs 56%, P = 1.0 [difference of −6%; 95% CI, −57% to 46%], Figure 1C).
Exodeviations without Fusion Potential
A total of 25 exotropic patients (68%) without bifoveal fusion were adjusted, and 12 (32%) were tied off. At 6 weeks and 1 year postoperatively, there was a numerically higher success rate in the patients who were adjusted compared with those tied off (6 weeks, 76% vs 67%, P = 0.7 [difference of 9%; 95% CI, −22% to 41%]; 1 year, 80% vs 67%, P = 0.4 [difference of 13%; 95% CI, −18% to 44%]; Figure 1D), although differences did not reach statistical significance.
Target Angle
The target angle (Table 1) was achieved for both distance and near measurements in 78 of the 89 patients (88%) and not achieved at distance, near, or both in 11 (12%) patients (3 in the tied-off group and 8 in the adjusted group; Table 4). Among these 11 patients, only 1 did not achieve the target angle at either distance or near (in the adjusted group).
Table 4.
Achievement of target angle at the time of adjustment in tied-off and adjusted patients, divided by type (based on the target angles given in Table 1).
| Esodeviations | Exodeviations | Total | ||||
|---|---|---|---|---|---|---|
| Fusion potential |
No fusion potential |
Fusion potential |
No fusion potential |
|||
| Tied-off | Achieved distance and near | 7 | 5 | 9 | 12 | 33 |
| Not achieved distance and/or near | 0 | 3 | 0 | 0 | 3 | |
| Adjusted | Achieved distance and near | 10 | 9 | 5 | 21 | 45 |
| Not achieved distance and/or near | 1 | 2 | 1 | 4 | 8 | |
Discussion
In this study evaluating outcomes in patients undergoing adjustable suture strabismus surgery for horizontal deviations in context of previous surgery, the overall success rate in those who were adjusted was not worse than in those who were not adjusted, whether assessed at 6 weeks or 1 year post surgery. The immediate postoperative target angle was the same for both tied off and adjusted patients; therefore, we did not expect to find that suture adjustment yielded better outcomes. As we predicted, our strategy of using adjustable sutures to achieve the predetermined target range resulted in equally successful outcomes in patients whose adjustable sutures were adjusted and whose adjustable sutures were tied off.
To our knowledge, no previous studies compare outcomes in patients undergoing adjustable suture strabismus surgery between those who were tied-off and those who were adjusted. In other studies of patients undergoing adjustable suture surgery the proportion requiring adjustment varies from 29%3 to 82%.2 The adjustment rate of 60% in our study is well within this range . The adjustment rate will depend on width of the target range, with narrow target ranges expected to have a higher rate of adjustment.
When interpreting our findings, there is an underlying assumption that adjusting alignment to a desired immediate postoperative target angle was helpful in achieving successful outcomes. We speculate that the outcomes of the adjusted patients would have been worse if they had not been adjusted, because the pre-adjustment angles were not within the desired range. It is possible that the outcomes of adjusted patients would have been the same even if their immediate postoperative alignment was outside of the desired range. Nevertheless, Mireskandari and colleagues recently presented optimum immediate postoperative target angles (for esotropic patients 4Δ exotropia to 4Δ esotropia, and for exotropic patients 0Δ to 8Δ esotropia), and concluded that patients in whom the target angle was achieved had significantly higher success rates (Mireskandari K, Cotesta M, Schofield J, Stephens D, Kraft SP. Achieving postoperative target range increases strabismus surgery success in adults. J AAPOS 2012;16:e23 [Abstract 085]). However, the patients in whom the target angle was achieved and the patients in whom it was not achieved may have differed by other important ways. Few studies specify the postadjustment target angles they are aiming to achieve. Weston and colleagues,10 after reviewing the postoperative drift of 201 patients undergoing adjustable suture surgery, suggested adjusting esotropic patients to orthotropia and exotropic patients to 5Δ-7Δ of esotropia. Del Monte and Archer11 described target ranges to achieve following adjustment, dividing patients according to their diagnosis and fusion potential. Their target ranges are narrower and within those used in the present study , except for fusing exotropia for which they allowed 2 more prism diopters of esotropia. Further work is needed to validate commonly used target ranges.
A randomized controlled trial comparing adjustable and fixed sutures has not yet been completed because there are several challenges. Depending on where surgeons train, some never use adjustable sutures, some use them occasionally, and some perform nearly all their surgeries using adjustable sutures. As a result, it may be difficult for surgeons to maintain true equipoise. In addition, specific target angles to be achieved immediately postoperatively would need to be agreed upon, and outcomes would need to be assessed by masked certified orthoptists or strabismologists.
There are some limitations to our study. Some patients did not return for a 1-year postoperative examination and therefore could not be included in our analysis, introducing potential bias, as the patients coming back at 1 year postoperatively might have been more likely to have a recurrence of their condition. We only analyzed a cohort of horizontal reoperations in the present study in order to study a homogeneous population and also because it represented a population on whom adjustable surgery is commonly performed. Therefore results may not be generalizable to other populations. Although only horizontal reoperations were included, diagnoses of the population studied were heterogeneous, and it is possible that outcomes were affected by the patient’s individual diagnosis and previous history.
Patients who underwent adjustable suture strabismus surgery and who were adjusted had outcomes that were at least as good as patients who underwent adjustable suture strabismus surgery and were simply tied off. We speculate that success would almost certainly have been worse without adjustable sutures for the patients who needed an adjustment to achieve their target angle. Overall, the strategy of using adjustable sutures may result in superior outcomes, but the question still awaits a randomized clinical trial.
Literature Search
PubMed was searched using the following terms: adjustable suture strabismus surgery and randomized clinical trials.
Acknowledgments
Financial support: National Institutes of Health Grant EY018810 (JMH), Research to Prevent Blindness, New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, Minnesota.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented as a poster at the 38th Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus, San Antonio, Texas, March 24–28, 2012.
References
- 1.Jampolsky A. Current techniques of adjustable strabismus surgery. Am J Ophthalmol. 1979;88:406–418. doi: 10.1016/0002-9394(79)90641-x. [DOI] [PubMed] [Google Scholar]
- 2.Zhang MS, Hutchinson AK, Drack AV, Cleveland J, Lambert SR. Improved ocular alignment with adjustable sutures in adults undergoing strabismus surgery. Ophthalmology. 2012;119:396–402. doi: 10.1016/j.ophtha.2011.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mireskandari K, Cotesta M, Schofield J, Kraft SP. Utility of Adjustable Sutures in Primary Strabismus Surgery and Reoperations. Ophthalmology. 2012;119:629–633. doi: 10.1016/j.ophtha.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 4.Tripathi A, Haslett R, Marsh IB. Strabismus surgery: Adjustable sutures—good for all? Eye. 2003;17:739–742. doi: 10.1038/sj.eye.6700465. [DOI] [PubMed] [Google Scholar]
- 5.Bishop F, Doran RM. Adjustable and non-adjustable strabismus surgery: A retrospective case-matched study. Strabismus. 2004;12:3–11. doi: 10.1076/stra.12.1.3.29010. [DOI] [PubMed] [Google Scholar]
- 6.Park YC, Chun BY, Kwon JY. Comparison of the stability of postoperative alignment in sensory exotropia: Adjustable versus non-adjustable surgery. Korean J Ophthalmol. 2009;23:277–280. doi: 10.3341/kjo.2009.23.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sundaram V, Haridas A. Adjustable versus non-adjustable sutures for strabismus. Cochrane Database Syst Rev. 2005:CD004240. doi: 10.1002/14651858.CD004240.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Hatt SR, Leske DA, Liebermann L, Holmes JM. Comparing outcome criteria performance in adult strabismus surgery. Ophthalmology. 2012;119:1930–1936. doi: 10.1016/j.ophtha.2012.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holmes JM, Liebermann L, Hatt SR, Smith SJ, Leske DA. Quantifying diplopia with a questionnaire. Ophthalmology. 2013 doi: 10.1016/j.ophtha.2012.12.032. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weston B, Enzenauer RW, Kraft SP, Gayowsky GR. Stability of the postoperative alignment in adjustable-suture strabismus surgery. J Pediatr Ophthalmol Strabismus. 1991;28:206–211. doi: 10.3928/0191-3913-19910701-05. [DOI] [PubMed] [Google Scholar]
- 11.Del Monte MA. Adjustable Suture Strabismus Techniques. In: Del Monte MA, Archer SM, editors. Atlas of Pediatric Ophthalmology and Strabismus Surgery. New York: Churchill Livingstone; 1993. [Google Scholar]