Abstract
We investigated the impact of light exposure history on light sensitivity in humans, as assessed by the magnitude of the suppression of melatonin secretion by nocturnal light. The hypothesis was that following a week of increased daytime bright-light exposure, subjects would become less sensitive to light, and that after a week of restriction to dimmer light they would become more sensitive. During the bright week, subjects (n = 12) obtained 4.3 ± 0.4 hr of bright light per day (by going outside and using light boxes indoors). During the dim week, they wore dark goggles (about 2% light transmission) when outside during daylight and spent 1.4 ± 0.9 hr per day outside. Saliva samples were obtained every 30 min for 7 hr in dim light (<15 lux) on two consecutive nights (baseline and test night) at the end of each week. On the test night, 500 lux was presented for 3 hr in the middle of the collection period to suppress melatonin. There was significantly more suppression after the dim week compared with after the bright week (to 53 versus 41% of the baseline night values, P < 0.05). However, there were large individual differences, and the difference between the bright and dim weeks was most pronounced in seven of the 12 subjects. Possible reasons for these individual differences are discussed, including the possibility that 1 wk was not long enough to change light sensitivity in some subjects. In conclusion, this study suggests that the circadian system’s sensitivity to light can be affected by a recent change in light history.
Keywords: circadian rhythms, human, light, light sensitivity, melatonin, melatonin suppression
Introduction
The circadian rhythm of nocturnal melatonin secretion from the pineal gland is generated by the suprachiasmatic nuclei. This secretion can be suppressed by ocular light exposure [1], which reaches the pineal via the circadian visual pathway [2, 3]. There is a dose–response relationship between light intensity and melatonin suppression, with higher light intensities producing more melatonin suppression [4–8]. Light intensities greater than or equal to about 2500 lux produce maximal suppression to near daytime values [1, 5, 7, 8], and as little as 100 lux has been shown to produce measurable suppression [9].
There are marked individual differences in the magnitude of melatonin suppression to a given light intensity [10, 11], which may reflect individual differences in light sensitivity. One melatonin suppression study found that women were more sensitive to light than men [12]. A methodological factor that might cause individual differences in melatonin suppression is differences in the circadian time of the nocturnal test light [13]. Therefore, it is better to include a baseline night in dim light, so that the changes in melatonin during the light exposure can be compared with what would occur naturally, e.g. a decrease in melatonin levels during the falling phase of melatonin secretion.
Light exposure history may also affect light sensitivity. More melatonin suppression was found in laboratory-raised squirrels than in wild-captured squirrels [14], which could be because of differences in previous light exposure. People are exposed to much less bright light in the winter [15–18], which could lead to an increase in light sensitivity. In a few humans studied in Antarctica [19], there was greater light sensitivity, as measured with melatonin suppression, during the winter than during the summer. In the winter, when the sun does not rise, maximum light intensity was around 500 lux, whereas in the summer, when the sun does not set, light intensity was as high as 100,000 lux.
The purpose of this study was to determine if short-term changes in light history can affect light sensitivity in humans. We created two different light conditions, a brighter light week and a dimmer light week, and used melatonin suppression as a measure of light sensitivity. A baseline and a melatonin-suppression night were included after each light history week. To our knowledge, this represents the first study of the effect of a rapid (1 wk) change of light history on light sensitivity in humans.
Materials and methods
Subjects
A total of 12 healthy subjects, six females, six males, mean age ± S.D., 25.5 ± 6.4 yr, completed the study. None of the subjects were taking prescription medications (except oral contraceptives for one woman), working night shifts, or had traveled through more than two time zones 1 month preceding the experiment. Subjects read and signed informed consent forms and were paid for their participation.
Design
The protocol was a counter-balanced crossover design, composed of a dim week and a bright week, lasting a total of 14 consecutive days. Seven subjects completed the bright week first and five subjects completed the dim week first. Eleven subjects completed the experiment in the summer (June–August), six in 1998 and five in 1999, and one subject participated in October 1998. Clock times are reported in Central Standard Time (CST).
Sleep schedule
Subjects had to adhere to a sleep schedule of 0:00–8:00 (subjects C08, C09, C10, C11, C13, C14 and C19) or 23:30– 7:30 (subjects C21, C25, C26, C27 and C28) depending on their usual schedules. They were allowed to go to bed and wake up 1 hr earlier than the planned schedule. To monitor compliance with the sleep schedule, subjects wore a wrist activity monitor (Ambulatory Monitoring, Ardsley, NY, USA, first seven subjects; Actiwatch 64, Mini Mitter Co. Inc., Bend, OR, USA, last five subjects) on the non-dominant wrist throughout the study. Subjects also filled out daily sleep logs and called the lab voice mail at bedtime and wake up time. Caffeine was not permitted during the 6 hr before the latest allowed bedtime.
Dim- and bright-week conditions
During the dim week, subjects were instructed to minimize their outdoor light exposure and to wear dark welders’ goggles (#5 lens = about 2% transmission; Uvex Cricket frames, first seven subjects, Uvex Flashback frames, last five subjects; Uvex Safety Inc., Smithfield, RI, USA) when outside during the daytime. These goggles resemble ordinary sunglasses, but have top and side shields and adjust in two different ways to fit the face. At the beginning of the dim week, we darkened subjects’ bedrooms by covering windows with black plastic and using black photography tape to seal any light cracks. We also surveyed each subject’s apartment with a light meter to ensure that the ambient light level was less than 200 lux. If necessary, we covered more windows with black plastic.
During the bright week, subjects were instructed to get at least 4 hr of bright light each day by going outside and/or using light boxes that we provided. Light boxes (Sun Ray 58 × 39 × 8 cm, 4 Octron Curvalume fluorescent lamps, Sun Box Co.) were set up in the subject’s home and/or work place, at the subject’s convenience. The light boxes (usually three) were set up so that the subject would receive between 5000–7000 lux of light at eye level when working, reading or watching TV. Subjects were not allowed to use the light boxes in the 3 hr before their latest allowed bedtime, to prevent a possible phase delay of their circadian rhythms. When outside, sunglasses were not permitted. Subjects’ personal sunglasses were kept in the laboratory for the duration of the experiment.
Throughout the study, light exposure was monitored continuously with a photosensor worn on the chest (like a medallion) and connected to a monitor in a fanny pack (AMS-1000, Consumer Sensory Products, Palo Alto, CA, USA or Mini-Logger, Mini Mitter Co. Inc.). After 1 day into the experiment and then every 2 days, subjects came to the laboratory and their light data were downloaded for inspection in their presence. Throughout the study, subjects had to maintain a daily light log to indicate when they were outside or using light boxes during the bright week, and when they were outside and if they were wearing their dark goggles during the dim week. Light logs were compared with the printed light graphs, derived from the photosensor, to ensure that subjects were getting the required amount of bright light and that they were sitting close enough to the light boxes in order to receive the required intensity. The logs were also checked to see if they wore their dark goggles when outside during the dim week.
Baseline and test (melatonin suppression) nights
On the sixth and seventh nights of each week, baseline and test nights, respectively, subjects were admitted to the lab, and saliva samples were collected in dim light (<15 lux) every 30 min for 7 hr starting at the time corresponding to their earliest allowed bedtime (23:00 or 22:30). On the test nights, 500 lux was presented for 3 hr in the middle of the 7-hr collection period (from 1:00 to 4:00 or from 00:30 to 3:30, depending on the sleep schedule). Melatonin levels from the test night were compared with those obtained in the previous night (baseline) to assess melatonin suppression.
Two tall light boxes provided the 500-lux light exposure, one on each side of a 120-cm tall bookshelf. A 25-in. TV was on top of the bookcase. Recliners faced the TV such that the subjects could comfortably watch TV in the reclined position. Each light box had a diffuser screen (25 cm wide × 121 cm high) and contained four, 120-cm fluorescent tubes arranged vertically. To produce an even ambient illumination, the light boxes were placed in short floor stands that tilted them slightly up towards the ceiling (about 15± relative to the vertical plane). The distance from the subjects’ eyes to the light boxes averaged about 270 cm. Subjects were required to watch movies during the 3-hr light exposure so that their gaze was directed towards the light boxes, but not directly at them. However, every half hour, subjects were required to stare directly at the light boxes for 2 min. Light exposure was measured with a light meter (TL-1, Minolta Corp., Ramsey, NJ, USA) every 20 min at the subject’s forehead and small adjustments were made, if necessary, to maintain the level of light exposure at 500 ± 10 lux.
Subjects were permitted up to two alcoholic beverages a day, but had to refrain from alcohol 48 hr prior to each lab night. At the beginning of each lab night, subjects were breath-analyzed. During the lab nights, to minimize posture changes (which may affect melatonin levels), a wheel chair was used to transport subjects to a nearby washroom. Subjects wore dark welders’ goggles (Uvex Cricket frames, #7 lens = about 0.35% light transmission) during these trips so that light intensity was not greater than the very dim light of the lab. Subjects were permitted to drink beverages that did not contain caffeine, but not 10 min before each sample. Food was not permitted.
Saliva samples were collected using Salivettes (Sarstedt, Newton, NC, USA). Tubes were immediately centrifuged after collection and placed in a freezer. Radioimmunoassay (RIA) analyses were performed by DiagnosTech (Osceola, WI, USA). All samples from a given subject were analyzed in the same assay. The maximum intra-assay variability and inter-assay variability were 12.1 and 13.2%, respectively. The lower limit of detection of the assay was at least 1.5 pg/mL throughout the study.
Statistical analysis
Melatonin suppression was quantified by comparing the average melatonin level in the last 2 hr of light exposure during the test night (test post) to the average level obtained during the corresponding time during the baseline night (baseline post). The suppression score was equal to [(baseline post − test post)/(baseline post)] × 100. This formula yields a positive percentage for decreased melatonin secretion due to light. Suppression scores were calculated for after the bright week and for after the dim week for each subject. To assess the effect of sex on melatonin suppression, we performed a 2 × 2 analysis of variance (ANOVA) with the following factors: sex (male versus female) and light history (dim versus bright week).
In addition to calculating suppression scores for the dim and bright weeks, we also calculated the difference between these suppression scores for each subject. These three measures of melatonin suppression were correlated with average daily light exposure durations calculated from the daily light logs: time spent outside during the bright light week, time spent in front of the light boxes, total time in bright light during the bright week (outside + light boxes), time spent outside during the dim week and the difference between total time in bright light during the bright week and the time spent outside during the dim week. We will report two-tailed P-values.
Results
Table 1 shows the melatonin suppression scores after the bright week and after the dim week. There was more suppression after the dim week compared with after the bright week (53 vs. 41%), and this difference was statistically significant (P < 0.05, paired t-test). The last column in Table 1 shows that there was more suppression after the dim week (a positive number) in nine of the 12 subjects. The ANOVA showed that there was no effect of sex on melatonin suppression [F(1,10) = 0.13, P > 0.05]. However, the effect of light history was significant [F(1,10) = 5.22, P < 0.05], corroborating our analysis using a t-test.
Table 1.
Melatonin levels and amount of suppression to 3 hr of 500-lux light presented during the test night at the end of the bright light week and at the end of the dim light week
| Subject | Bright week
|
Dim week
|
Difference between suppression scoresd | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline night
|
Test night
|
Suppression scorec (%) | Baseline night
|
Test night
|
Suppression scorec (%) | ||||||
| Prea | Postb | Prea | Postb | Prea | Postb | Prea | Postb | ||||
| C08e | 3.3 | 6.9 | 3.5 | 3.4 | 50.7 | 1.4 | 7.3 | 2.3 | 2.1 | 71.2 | 20.5 |
| C09 | 3.1 | 4.9 | 3.7 | 2.2 | 55.1 | 3.2 | 4.9 | 3.2 | 1.1 | 77.6 | 22.5 |
| C10e | 9.4 | 7.7 | 6.9 | 3.8 | 50.6 | 9.6 | 8.0 | 8.6 | 2.0 | 75.0 | 24.4 |
| C11 | 10.4 | 16.6 | 5.5 | 4.3 | 74.1 | 8.1 | 11.7 | 6.1 | 3.6 | 69.2 | −4.9 |
| C13e | 12.9 | 10.8 | 14.8 | 8.7 | 19.4 | 8.2 | 12.0 | 11.0 | 7.0 | 41.7 | 22.3 |
| C14 | 9.2 | 11.2 | 6.9 | 4.7 | 58.0 | 6.9 | 16.8 | 8.1 | 10.8 | 35.7 | −22.3 |
| C19 | 16.6 | 15.6 | 12.7 | 18.4 | −17.9 | 8.9 | 15.2 | 7.9 | 19.2 | −26.3 | −8.4 |
| C21 | 11.0 | 20.3 | 6.7 | 11.9 | 41.4 | 1.6 | 21.5 | 2.9 | 11.5 | 46.5 | 5.1 |
| C25e | 8.5 | 14.7 | 6.0 | 10.0 | 32.0 | 4.0 | 7.7 | 4.9 | 3.7 | 51.9 | 19.9 |
| C26 | 2.3 | 6.6 | 3.5 | 4.6 | 30.3 | 3.0 | 6.7 | 4.4 | 2.0 | 70.1 | 39.8 |
| C27 | 19.7 | 17.3 | 19.9 | 13.2 | 23.7 | 16.2 | 18.9 | 19.5 | 13.2 | 30.2 | 6.5 |
| C28e | 6.6 | 7.3 | 5.6 | 1.8 | 75.3 | 5.0 | 5.0 | 3.6 | 0.5 | 90.0 | 14.7 |
| Mean | 9.4 | 11.7 | 8.0 | 7.3 | 41.1 | 6.3 | 11.3 | 6.9 | 6.4 | 52.7* | 11.7 |
| S.D. | 5.3 | 5.1 | 5.1 | 5.2 | 25.9 | 4.2 | 5.6 | 4.8 | 6.0 | 31.1 | 17.2 |
P < 0.05 compared with bright week by paired t-test.
Mean pg/mL for 2 hr before light exposure time.
Mean pg/mL for last 2 hr of light exposure time.
[(baseline post − test post)/(baseline post)] × 100; larger percentage indicates more suppression by test light.
Dim week suppression score − bright week suppression score; positive difference indicates more suppression after dim week.
Dim week first.
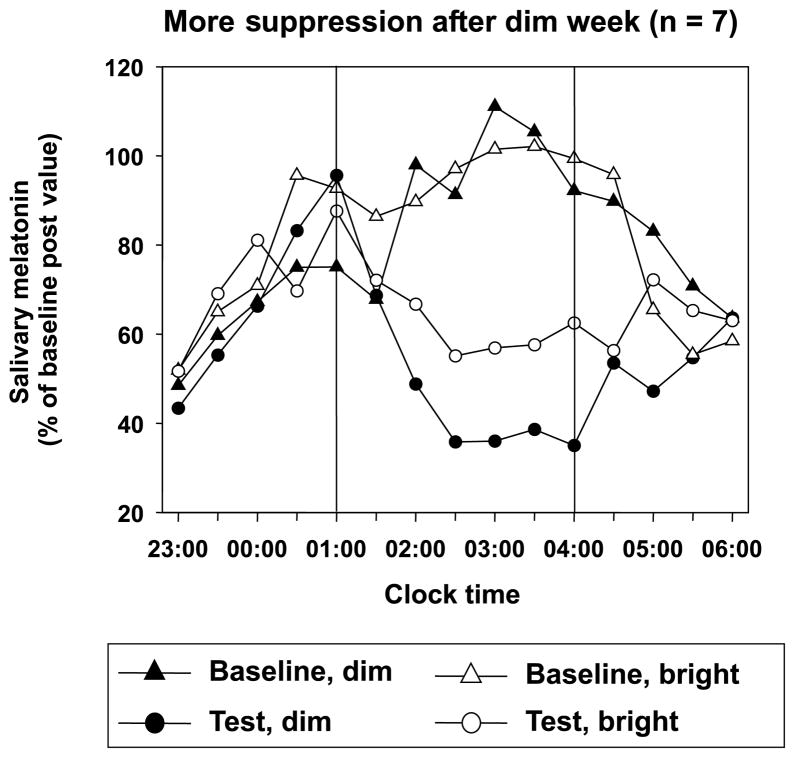
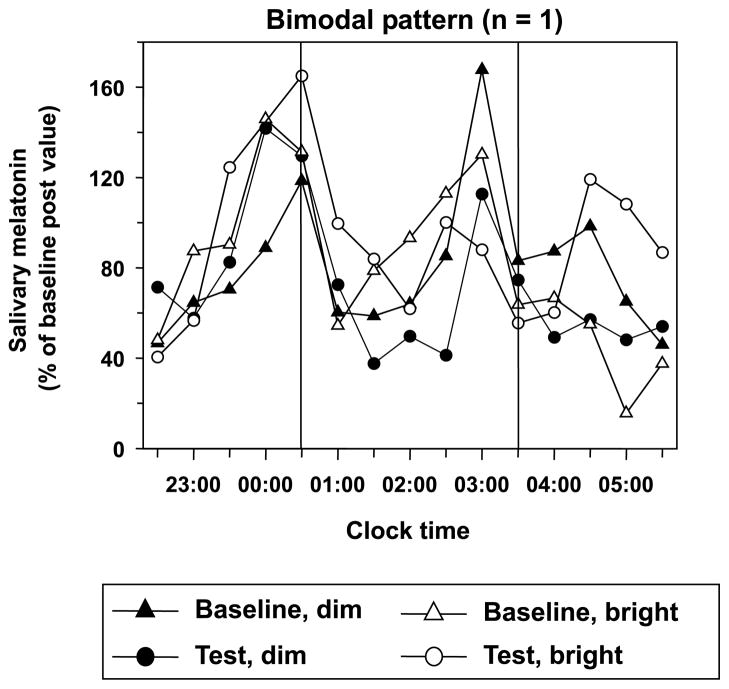
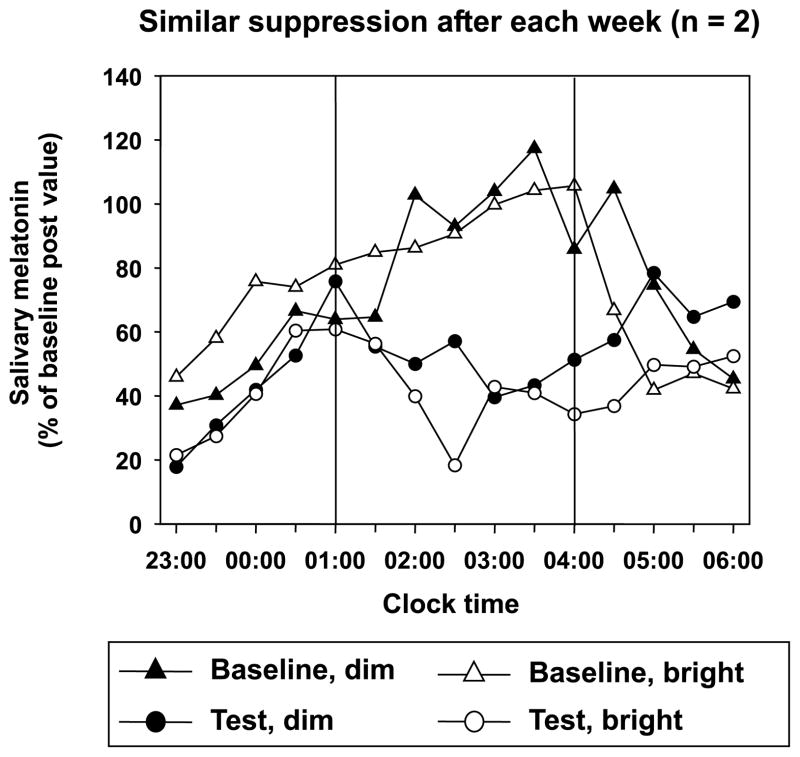
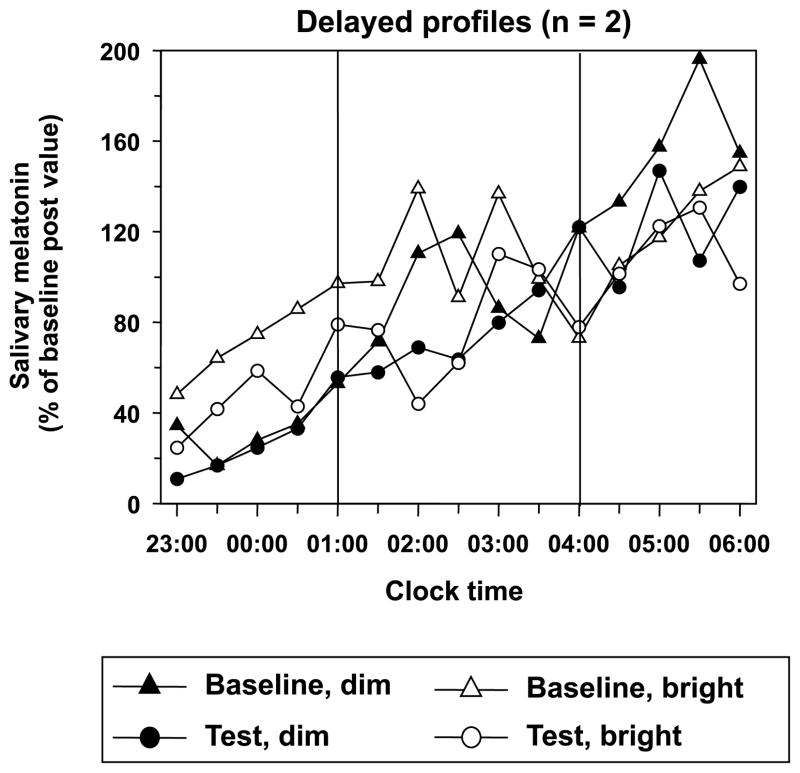
There were four types of melatonin secretion profiles and patterns of melatonin suppression as shown in Figs 1–4. The seven subjects in Fig. 1 had typical profiles of nocturnal melatonin secretion during the baseline nights (triangles). Melatonin increased rapidly for the first 2 hr, reached maximal levels within the next 3 hr, and then decreased rapidly during the last 2 hr of the 7-hr recording period. The 3-hr light exposure of 500 lux on the test nights occurred when melatonin reached its highest level. There was more suppression after the dim week compared with after the bright week (closed versus open circles). During the 3-hr light exposure, melatonin levels decreased rapidly, reaching a plateau within the first 1.5 hr, and then gradually rose after lights off. The two subjects in Fig. 2 had typical profiles during baseline, but the amount of melatonin suppression was similar after the dim and bright weeks. Figs 3 and 4 show profiles of melatonin in which suppression could not easily be observed graphically. The two subjects in Fig. 3 showed an increase of melatonin levels throughout the recording period. We interpret this to be the beginning of the nocturnal profile of relatively phase-delayed subjects. The subject in Fig. 4 had a bimodal profile with two peaks split by a substantial decrease of melatonin during both the baseline and test nights.
Fig. 1.
Melatonin profiles from seven subjects who showed more melatonin suppression after the dim week than after the bright week (subjects C08, C09, C10, C13, C25, C26 and C28). Vertical lines indicate the period of 500-lux light exposure on the test nights. At all other times the light intensity was <15 lux. Profiles were averaged so that the 3 hr of light exposure were aligned. The clock times shown are for subjects who had the light exposure from 1:00 to 4:00. The others had the light from 0:30 to 3:30. Before group averaging, each profile was converted into percentages of its respective baseline post-value. The baseline post-value was the average melatonin level of the last four samples collected in the 3-hr interval during the baseline night, e.g. 2:30, 3:00, 3:30 and 4:00.
Fig. 4.
Melatonin profiles from subject C27 who had a bimodal pattern. For more details see Fig. 1.
Fig. 2.
Melatonin profiles from two subjects who showed similar suppression after the dim week compared with after the bright week (subjects C11 and C14). For more details see Fig. 1.
Fig. 3.
Melatonin profiles from two subjects who had delayed profiles (subjects C19 and C21). For more details see Fig. 1.
Analysis of daily light logs showed that subjects reported spending 4.3 ± 0.4 hr per day (mean ± S.D.) in bright light during the bright week (range 3.8–4.9 hr). On average, about half the time was spent outside and half was spent in front of the light boxes, although this varied greatly among individuals. Subjects reported spending 1.4 ± 0.9 hr per day outside during the dim week (range 0.2–3.5 hr).
There was only one significant (P < 0.05) correlation in our small sample (n = 12) between melatonin suppression and light exposure duration from light logs. This was the correlation (r = 0.70, P = 0.012) between the time spent in bright light during the bright week (outside + light boxes) and the difference in melatonin suppression scores (last column of Table 1). This indicates that the more bright light subjects received during the bright week, the greater their melatonin suppression after the dim week compared with after the bright week. There was also a large negative correlation between time spent outside during the bright week and the suppression score after the bright week (r = −0.51, P = 0.087). This means that more exposure to outside light resulted in less melatonin suppression (less sensitivity to the 500-lux test light). If a subject spent more of his or her 4-hr bright light requirement in front of the light boxes, then he or she spent less time outside. Thus, there was a positive correlation between time spent in front of the light boxes and suppression after the bright week (r = 0.57, P = 0.060).
We were unable to analyze the photosensor data because of technical difficulties.
Discussion
In this study, we observed significantly more melatonin suppression after a week of exposure to relatively dim light compared with after a week of exposure to long durations (about 4 hr per day) of brighter light, suggesting greater light sensitivity after the dim week when compared with the bright week. Although the difference in melatonin suppression between the light history conditions was statistically significant, it was most pronounced in seven subjects (Fig. 1), and was small or in the opposite direction in the other five subjects (Figs 2–4). Some of the factors that may have masked the effect in these five subjects include: (1) non-optimal circadian timing of test light; (2) duration of light history conditions (1 wk) too short; and (3) not enough bright light during the bright week or too much light during the dim week.
First, the 3-hr test light may have occurred too early on the profile for two subjects (Fig. 3) or in between the peaks of a bimodal profile (Fig. 4) making it difficult to demonstrate a difference between bright and dim weeks using our methods. Second, it is possible that only 1 wk of each condition was not long enough to produce changes in light sensitivity in some individuals. There could be genetic differences among individuals in light sensitivity and in the ability to adjust to changes in lighting conditions. In rats, the structure of the retina gradually changes to ensure that a constant number of photons is absorbed each day, a process called photostasis [20]. For example, rats kept in dim light will develop retinas with greater photon-catching ability than those exposed to more intense light (see Ref. [21] for review). If such a process also occurs in humans, then perhaps more than a week is necessary for such changes to fully develop.
Third, there may not have been enough bright light during the bright week, or too much light during the dim week, to produce differences in light sensitivity in some subjects. The correlations between the duration of bright light exposure during the bright light week and melatonin suppression support this possibility. Perhaps if our subjects had spent more of their 4-hr bright light requirement outside, it would have decreased their light sensitivity even more. However, even though our subjects were studied primarily during the summer, most told us that the most difficult part of the study was finding the time for the 4 hr of bright light per day. Studies of light exposure in healthy young adults in North American cities (Montreal, Canada; Rochester, MN, USA) found that outdoor light exposure in the summer was approximately 2.5 hr per day [16, 17]. According to a Chicago study of SAD subjects while remitted in summer, and who typically enjoy outdoors summer activities, the average time outside per day was only 3.0 hr [15]. Although our subjects spent less time outdoors during the dim week (compared with the bright week) and wore dark welders’ goggles, they could still have been exposed to relatively bright light. Subjects were run during the summer when outdoor light intensity can reach 100,000 lux or more. Given 100,000 lux, the 2% transmission lenses would permit 2000 lux to reach the eye, which is more intense than ordinary room light (usually <500 lux), and thus not even considered dim in current terminology. Finally, we could not be absolutely sure that subjects always wore their dark glasses when outside. Perhaps more reliable differences in light sensitivity would be produced in a study that compared subjects who were kept indoors for days or weeks in ordinary room light with subjects who were outside for long periods in sunlight.
In agreement with other studies [8, 22, 23], we did not find a sex difference in the amount of melatonin suppression. However, in one study [12] there was greater suppression in females than in males. A preliminary report indicated more suppression in females when compared with the males when evaluated in the fall and the winter, but not in the summer or spring [24]. It is possible that the results of both these studies could be explained by light history, which was not assessed in these studies. If males spent more time outdoors they could have become less sensitive to light. Light history might also explain conflicting reports regarding melatonin suppression in patients with affective disorders. Some studies found greater suppression than in controls [25–28], but others found the opposite or no difference between patients and controls [29–32]. Our study shows that it is important to monitor or control the light exposure history of subjects, including whether they wear sunglasses, because ordinary sunglasses can block as much as about 90% of the light intensity.
In conclusion, this study was the first to show that light sensitivity in humans, as assessed by melatonin suppression to nocturnal light, may be changed by manipulating light exposure history in the previous week. However, our sample size was small, and there were large individual differences. More research is necessary to confirm and extend these results. There should also be investigations of light sensitivity of the circadian clock as measured by phase shifts following a particular light history.
Acknowledgments
The authors thank Mathias S. Fleck for assistance with data collection, the volunteers for their participation, John Taylor for building the light box stands, and Helen Burgess, PhD, for her comments on the paper. Supported by NIH grants R01 NS23421 and R01 NS35695 to C.I.E.
References
- 1.Lewy AJ, Wehr TA, Goodwin FK, et al. Light suppresses melatonin secretion in humans. Science. 1980;210:1267–1269. doi: 10.1126/science.7434030. [DOI] [PubMed] [Google Scholar]
- 2.Klein DC, Moore RY, Reppert SM. The Mind’s Clock. Oxford University Press; Oxford: 1991. Suprachiasmatic Nucleus. [Google Scholar]
- 3.Morin LP. The circadian visual system. Brain Res Rev. 1994;67:102–127. doi: 10.1016/0165-0173(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 4.Brainard GC, Lewy AJ, Menaker M, et al. Dose–response relationship between light irradiance and the suppression of plasma melatonin in human volunteers. Brain Res. 1988;454:212–218. doi: 10.1016/0006-8993(88)90820-7. [DOI] [PubMed] [Google Scholar]
- 5.McIntyre IM, Norman TR, Burrows GD, et al. Human melatonin suppression by light is intensity dependent. J Pineal Res. 1989;6:149–156. doi: 10.1111/j.1600-079x.1989.tb00412.x. [DOI] [PubMed] [Google Scholar]
- 6.McIntyre IM, Norman TR, Burrows GD, et al. Quantal melatonin suppression by exposure to low intensity light in man. Life Sci. 1989;45:327–332. doi: 10.1016/0024-3205(89)90142-2. [DOI] [PubMed] [Google Scholar]
- 7.Aoki H, Yamada N, Ozeki Y, et al. Minimum light intensity required to suppress nocturnal melatonin concentration in human saliva. Neurosci Lett. 1998;252:91–94. doi: 10.1016/s0304-3940(98)00548-5. [DOI] [PubMed] [Google Scholar]
- 8.Nathan PJ, Wyndham EL, Burrows GD, et al. The effects of gender on the melatonin suppression by light: a dose response relationship. J Neural Transm. 2000;107:271–279. doi: 10.1007/s007020050022. [DOI] [PubMed] [Google Scholar]
- 9.Brainard GC, Rollag MD, Hanifin JP. Photic regulation of melatonin in humans: ocular and neural signal transduction. J Biol Rhythms. 1997;12:537–546. doi: 10.1177/074873049701200608. [DOI] [PubMed] [Google Scholar]
- 10.Bojkowski CJ, Aldhous ME, English J, et al. Suppression of nocturnal plasma melatonin and 6-sulphatoxymelatonin by bright and dim light in man. Horm Metab Res. 1987;19:437–440. doi: 10.1055/s-2007-1011846. [DOI] [PubMed] [Google Scholar]
- 11.Laakso ML, Porkka-Heiskanen T, Stenberg D, et al. Interindividual differences in the responses of serum and salivary melatonin to light. In: Fraschini F, Reiter RJ, editors. Role of Melatonin and Pineal Peptides in Neuroimmunomodulation. Plenum Press; New York: 1991. pp. 307–311. [Google Scholar]
- 12.Monteleone P, Esposito G, LaRocca A, et al. Does bright light suppress nocturnal melatonin secretion more in women than men? J Neural Transm. 1995;102:75–80. doi: 10.1007/BF01276567. [DOI] [PubMed] [Google Scholar]
- 13.Nathan PJ, Burrows GD, Norman TR. The test re-test reliability of the melatonin suppression by white light. Biol Rhythm Res. 1999;30:467–475. [Google Scholar]
- 14.Reiter RJ, Steinlechner S, Richardson BA, et al. Differential response of pineal melatonin levels to light at night in laboratory-raised and wild-captured 13-lined ground squirrels. Life Sci. 1983;32:2625–2629. doi: 10.1016/0024-3205(83)90353-3. [DOI] [PubMed] [Google Scholar]
- 15.Eastman CI. Natural summer and winter sunlight exposure patterns in seasonal affective disorder. Physiol Behav. 1990;48:611–616. doi: 10.1016/0031-9384(90)90199-e. [DOI] [PubMed] [Google Scholar]
- 16.Cole RJ, Kripke DF, Wisbey J, et al. Seasonal variation in human illumination exposure at two different latitudes. J Biol Rhythms. 1995;10:324–334. doi: 10.1177/074873049501000406. [DOI] [PubMed] [Google Scholar]
- 17.Hebert M, Dumont M, Paquet J. Seasonal and diurnal patterns of human illumination under natural conditions. Chronobiol Int. 1998;15:59–70. doi: 10.3109/07420529808998670. [DOI] [PubMed] [Google Scholar]
- 18.Guillemette J, Hebert M, Paquet J, et al. Natural bright light exposure in the summer and winter in subjects with and without complaints of seasonal mood variations. Biol Psychiatry. 1998;44:622–628. doi: 10.1016/s0006-3223(97)00543-x. [DOI] [PubMed] [Google Scholar]
- 19.Owen J, Arendt J. Melatonin suppression in human subjects by bright and dim light in Antarctica: time and season-dependent effects. Neurosci Lett. 1992;137:181–184. doi: 10.1016/0304-3940(92)90399-r. [DOI] [PubMed] [Google Scholar]
- 20.Penn JS, Williams TP. Photostasis: regulation of daily photon- catch by rat retinas in response to various cyclic illuminances. Exp Eye Res. 1986;43:915–928. doi: 10.1016/0014-4835(86)90070-9. [DOI] [PubMed] [Google Scholar]
- 21.Boulos Z, Terman M. Photostasis: implications for pineal, circadian and visual photosensitivity. In: Williams TP, Thistle AB, editors. Photostasis and Related Phenomena. Plenum Press; New York: 1998. pp. 153–170. [Google Scholar]
- 22.Boyce P, Kennaway DJ. Effects of light on melatonin production. Biol Psychiatry. 1987;22:473–478. doi: 10.1016/0006-3223(87)90169-7. [DOI] [PubMed] [Google Scholar]
- 23.Nathan PJ, Burrows GD, Norman TR. The effect of dim light on suppression of nocturnal melatonin in healthy women and men. J Neural Transm. 1997;104:643–648. doi: 10.1007/BF01291882. [DOI] [PubMed] [Google Scholar]
- 24.Lewy AJ, Cutler NL, Hughes RJ, et al. Women are more sensitive than men to 500 lux light suppression of melatonin (LSM) in fall and winter. Sleep Res. 1997;26:731. [Google Scholar]
- 25.Lewy AJ, Wehr TA, Goodwin FK, et al. Manic-depressive patients may be supersensitive to light. Lancet. 1981;14:384. doi: 10.1016/s0140-6736(81)91697-4. [DOI] [PubMed] [Google Scholar]
- 26.Lewy AJ, Nurnberger JI, Wehr TA, et al. Supersensitivity to light: possible trait marker for manic-depressive illness. Am J Psychiatry. 1985;142:725–727. doi: 10.1176/ajp.142.6.725. [DOI] [PubMed] [Google Scholar]
- 27.Thompson C, Stinson D, Smith A. Seasonal affective disorder and season-dependent abnormalities of melatonin suppression by light. Lancet. 1990;336:703–706. doi: 10.1016/0140-6736(90)92202-s. [DOI] [PubMed] [Google Scholar]
- 28.Nathan PJ, Burrows GD, Norman TR. Melatonin sensitivity to dim white light in affective disorders. Neuropsychopharmacology. 1999;21:408–413. doi: 10.1016/S0893-133X(99)00018-4. [DOI] [PubMed] [Google Scholar]
- 29.Cummings MA, Berga SL, Cummings KL, et al. Light suppression of melatonin in unipolar depressed patients. Psychiatry Res. 1989;27:351–355. doi: 10.1016/0165-1781(89)90149-2. [DOI] [PubMed] [Google Scholar]
- 30.Lam RW, Berkowitz AL, Berga SL, et al. Melatonin suppression in bipolar and unipolar mood disorders. Psychiatry Res. 1990;33:129–134. doi: 10.1016/0165-1781(90)90066-e. [DOI] [PubMed] [Google Scholar]
- 31.Murphy DGM, Murphy DM, Abbas M, et al. Seasonal affective disorder – response to light as measured by electroencephalogram, melatonin suppression, and cerebral blood flow. Br J Psychiatry. 1993;163:327–331. doi: 10.1192/bjp.163.3.327. [DOI] [PubMed] [Google Scholar]
- 32.Nurnberger JI, Adkins S, Lahiri DK, et al. Melatonin suppression by light in euthymic bipolar and unipolar patients. Arch Gen Psychiatry. 2000;57:572–579. doi: 10.1001/archpsyc.57.6.572. [DOI] [PubMed] [Google Scholar]