Abstract
Particle size dictates where aerosolized pathogens deposit in the respiratory tract, thereafter the pathogens potential to cause disease is influenced by tissue tropism, clearance kinetics and the host immunological response. This interplay brings pathogens into contact with a range of tissues spanning the respiratory tract and associated anatomical structures. In animal models, differential deposition within the respiratory tract influences infection kinetics for numerous select agents. Greater numbers of pathogens are required to infect the upper (URT) compared with the lower respiratory tract (LRT), and in comparison the URT infections are protracted with reduced mortality. Pathogenesis in the URT is characterized by infection of the URT lymphoid tissues, cervical lymphadenopathy and septicemia, closely resembling reported human infections of the URT. The olfactory, gastrointestinal, and ophthalmic systems are also infected in a pathogen-dependent manner. The relevant literature is reviewed with respect to particle size and infection of the URT in animal models and humans.
Keywords: particle size, aerosols, upper respiratory tract, infection, pneumonia
Introduction: The Ubiquitous Nature of Bioaerosols
Bioaerosols are defined as a collection of particles suspended on a column of air derived from or incorporating material of biological origin. Individual particles within the bioaerosol can vary markedly in aerodynamic diameter from submicron (e.g., viruses) to many millimeters (e.g., pet dander). Importantly, bioaerosols can affect human health due to the presence of pathogens or allergens. The sources of bioaerosols containing pathogens are varied and individual aerosol particles may vary widely from submicron to several millimeters dependent on the method of aerosol generation and attachment to larger particulates, for example skin cells (Table 1); although only those <100 μm are within the inhalable range for humans, it should be noted that the initial particles will rapidly evaporate depending on the humidity of the local environment.4,33,34 The final inhaled particle size is dependent on a number of factors including the solid organic content of the initial particle (including pathogens) and location of an individual to the aerosol source. It is evident that even pollen grains that represent comparatively larger bioaerosols can travel large distances in conducive meteorological conditions.15,35 Airborne dissemination whether outdoors or indoors is influenced by a number of inter-relating factors that impact on air mass movement, turbulence, and thermal convection including meteorology, vehicle/human activity, and ventilation that may far outweigh the terminal velocity of particles that are generally calculated in very still air.4,34 This review will concentrate on aerosols containing pathogens and the inter-relationship between factors governing particle size, deposition site, clearance, and inhalational infection.
Table 1. Sources of bioaerosol.
| Bioaerosol source | Mechanisms | Particle size distributiona,b | Reference(s) |
| Healthcare | Surgical or dental procedures | Up to 50 µme | 1 and 2 |
| Hospital air | <2 µm (22%), 2 to 6 µm (30%), >5 µm (48%) | 3 | |
| Mechanical ventilators, bed making, and resuspension on dust or skin squamae | 0.3 to >5 µm | 4 and 5 | |
| Water industry | Cooling towers | <5 up to >100 µm (bimodal peaks at <5 µm and 20–40 µm) | 6 |
| Wastewater irrigation sites | 1.0 to 5.9 µm | 7 | |
| Agricultural/forestry industries | Grain harvesting, food processing, dust, and/or feces from animal housing and farming activities | 0.9 to 18.9 µm 0.5 to >5 µm (increase in 2 to >5 µm range) |
8 and 9 |
| Insecticidal crop spraying | 4.6 to 39 µmd | 10 and 11 | |
| 12.3 to 37.1 µmc | 12 | ||
| 15 to 45 µmc | 13 | ||
| 60 to 100 µm (kromecote card); 5.3 to 7.3 µm (Anderson cascade impactor) | 14 | ||
| Genetic dispersion | Pollen grains: 10 to 100 µme | 15 | |
| Fungal spores: 1 to 50 µme | 16 | ||
| Postal and shopping industry | Mail sorting and opening | 0.3 to >5 µm; 19.6-fold increase in particles >5 µm | 17 |
| Mist machine | “between 40 and 70 µm” | 18 | |
| Leisure activities | Marine activities, e.g., surfing | 24 to 44 µm, median 34 µm | 19 |
| Whirlpools | <1 to 15 µm dependent on turbulence | 20 | |
| Human activity | Breathing | <0.8 to 2 µm | 21 |
| Speaking | 16 to 125 µm | 22 and 23 | |
| <0.8 to 7 µm | 21 | ||
| Shouting | 0.5 to 10 µm (mean = 1.0 µm) | 24 | |
| Coughing | 0.62 to 15.9 µm | 21, 22, and 25–27 | |
| 40 to 125 µm | 23 and 28 | ||
| Sneezing | 7 to 125 µm | 28 and 29 | |
| Vuvuzela playing | 0.5 to >10 µm (mean = 1.3 µm) | 24 | |
| Showering | Hot water (5.2 to 7.5 µm) | 30 | |
| Cold water (2.5 to 3.1 µm) | |||
| Miscellaneous | Pulp waste water treatment plant | 2.4 to 3.5 µm (median); 99.9% of particles were below 15 µm | 31 |
| Building tower (sweeping dust containing pigeon feces) | 1.1 to 11.0 µm | 32 |
a Aerodynamic diameter; bdistributions should be viewed with caution as often experiments used samplers with cut off limits less than 15 µm and therefore were preferentially selective for particles smaller than this size; cspray-dried Bacillus thuringiensis produced at different homogenization speeds; dnon-biological aerosols for vector control; eprocedure- or species-dependent.
Aerosol Transmission: Relation to Mechanism of Generation
The mechanism of generation influences the particle size of the resultant bioaerosol (Table 1), and these may be biotic (e.g., sneeze or pollen), or abiotic where the aerosol is produced by a non-living system (e.g., water cooling towers). Irrespective, all aerosols will be generated with an initial mass median aerodynamic diameter (MMAD) that will decrease with increased distance from the source due to evaporation and settling dependent on environmental parameters such as relative humidity and turbulence.
All mechanisms of human oro-nasal activity such as breathing, talking, laughing, coughing and sneezing produce particles within the inhalable range for humans of <1 to >100 μm (Table 1). Significant variation occurs between studies regarding number of particles expelled, size range of the particles and the number of pathogens incorporated within the particles, attributable to differences in methodology and human factors where standardization is difficult.21,26,28,36,37,39 Comparatively, coughing and sneezing produce greater quantities of particles28,36,37 that travel further due to the velocity of expulsion from the nose or mouth.40 The majority of these particles reside in the inhalable fraction for humans (i.e., <100 μm) at 78.6–96.0% and 98.9% for coughing and sneezing respectively; while of this inhalable fraction, 7.1–46.7% and 18.8% produced by coughing and sneezing were less than 4 μm, evaporating to droplet nuclei and deposit in the bronchoalveolar region of the lung.28,36,37
The situation in relation to deposition is more complex due to evaporation. Atmospheric relative humidity (RH) and temperature are generally lower than that of the body. Once the particles are in the atmosphere evaporation occurs at rates according to their original size and composition of the particle to reach equilibrium with atmospheric conditions. Hence, the aerosol produced is dynamic, changing with distance from the initial point of generation. Particles produced from sneezing and coughing will contain varying amounts of saliva and mucus comprising inorganic and organic ions plus glycoproteins.33,38 Many aerosol transmission modeling studies are based on assumptions e.g., settling velocities and/or evaporation parameters of pure water droplets within a vacuum and droplet distributions from healthy volunteers.21,22 It is probable that irrespective of composition due to the small droplet sizes originating from a cough or sneeze that evaporation will be rapid unless the presence of solutes greatly retards evaporation, for example, a 5 µm water droplet will evaporate within 0.8 s in 97% RH.21 However, extrapolating to natural situations where the droplet composition will be very different and turbulence will exert a large effect on how rapidly particles deposit requires care. Indeed, one recent study demonstrated that infected individuals generated larger aerosol particles than healthy counterparts.41 This could be attributable to differences in mucus (composition, quantity, and viscosity) produced during infection affecting evaporation and the location of the infection.33,42 The closer an individual is situated to an aerosol source then the greater the likelihood of large particles being inhaled prior to complete evaporation.
Similar principles can be extrapolated to any aerosol present in Table 1, simply the mechanism of generation, the solute type and concentrations (organic and inorganic) plus the surrounding environment will differ and therefore the processes of evaporation and dissemination will accordingly vary. Irrespective of whether aerosol particles are generated by abiotic or biotic processes (e.g., Table 1), inhalation of particles into the warm humid respiratory tract will prompt rehydration and affect deposition due to particle growth.43 It is evident that there is significant potential for URT deposition depending on how close an individual is to the source.
Initial Site of Deposition and Infection is Dependent on Particle Size
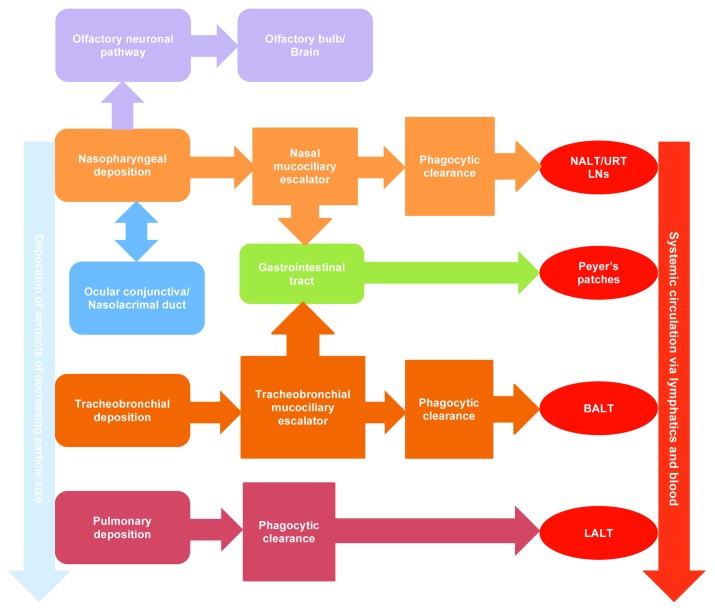
The respiratory tract is complex, comprising a collection of specialized organs, tissues, and cells ranging from the nares to the alveoli.44 These tissues convey a range of physiological functions connected to breathing (i.e., air conditioning, air conductance, and gaseous exchange) and defense against foreign particulates (i.e., immune function and mucociliary or phagocytic clearance). After exposure to a bioaerosol containing pathogens, the initial site of deposition where infection may ensue is likely to be the respiratory epithelium. However, due to the interconnecting anatomical features and clearance mechanisms within the mammalian body, the ocular conjunctiva, olfactory epithelium, or URT immunological tissues may represent further sites where infection could initiate after inhalational exposure to a pathogenic aerosol (Table 2; Fig. 1). Various viruses with dual tropism for both ocular and respiratory tissues utilize the nasolacrimal duct to produce URT infection (e.g., influenza virus, respiratory syncytial virus, and adenovirus).45 Depending on clearance mechanisms and the sensitivity of the pathogen to stomach acidity, gastrointestinal (GI) tissues may represent a further portal. The enteric Norwalk-like virus has been demonstrated to be transmitted by aerosol, presumably via droplets produced during diarrhea and vomiting.46,47 Similarly, aerosol dissemination of Clostridium difficile spores has been observed in hospital wards48; however this has not been conclusively linked to infection via inhalation.
Table 2. Tissues that may represent the primary site of deposition, clearance and infection during exposure to a bioaerosol.
| Anatomical region | Tissue(s) | Function | Epithelium |
|---|---|---|---|
| Nasopharyngeal/Oropharyngeal | Nares to nasopharynx | Inhalation, filtration, and mucociliary clearance of foreign particles; warming/humidification of air | Ciliated |
| Paranasal sinuses | Humidification of air; mucociliary clearance of foreign particles | Ciliated | |
| Olfactory epithelium | Detection of odors | Sensory | |
| Mouth to oropharynx | Mastication and ingestion; inhalation | Non-ciliated | |
| Tonsils, adenoidsa | Defense against inhaled/ingested pathogens; URT mucosal immunity | Lymphoepithelial | |
| Tracheobronchial | Larynx | Sound generation; mucociliary clearance | Ciliated/non-cilated |
| Trachea | Air conduction; mucociliary clearance | Ciliated | |
| Bronchi to bronchioles | Air conduction and particulate filtration; mucociliary clearance | Ciliated | |
| Pulmonary | Respiratory bronchioles to alveoli | Air conduction; gaseous exchange; pulmonary clearance and immunity | Non-ciliated |
| Ocular | Ocular conjunctiva | Lubrication of ocular region | Non-ciliated |
| Nasolacrimal duct | Drainage of excess tear fluid | Non-ciliated | |
| Gastrointestinal | Esophageal, stomach and intestinal epithelium | Digestion and absorption of ingested material, including inhaled particles trapped in the mucociliary escalator | Non-ciliated |
| Peyer patches | Defense against ingested pathogens | Lymphoepithelial |
a Nasal-associated lymphoid tissue (NALT) represents the rodent equivalent.
Figure 1. Schematic of the interplay between deposition sites and clearance mechanisms in the respiratory tract. BALT, bronchial-associated lymphoid tissue; LALT, lung-associated lymphoid tissue; LNs, lymph nodes; NALT, nasal-associated lymphoid tissue.
The aerodynamic diameter of inhaled particles determine where within the respiratory tract pathogens incorporated within the particles deposit and interact with host tissues. A number of mechanisms determine deposition of particles within the respiratory tract including inertial impaction, Brownian diffusion, gravitational sedimentation, and electrostatic effects.44 Small particles (<1–3 μm) diffuse deep into the lung tissue, depositing in the alveoli by a number of mechanisms including diffusion, sedimentation, and electrostatic effects. In contrast, larger particles (>8 μm) impact further up the respiratory airways due to greater inertion, depositing in a size-dependent manner from the nasal passages to the larger bronchioles. This relationship is extant across mammalian species albeit differences in respiratory anatomy and physiology dictate the penetration of a particular particle size into the respiratory tract.49-54 The size and body shape of the species determines the morphometry of the nasal cavity and respiratory airways influencing the size of the particles that may deposit in corresponding anatomical regions.51,55 Even within species, variables including age, body weight, breathing mode (oro-nasal/nasal), sex, strain (or ethnicity), activity (e.g., sleeping, exercise), and disease state (e.g., asthma, pneumonia, emphysema, and chronic obstructive pulmonary disorder) influence biometry or affect respiratory physiology and hence deposition profiles.49,56,57 The propensity of humans to revert to oro-nasal breathing during exertion significantly increases the size of particles that may be inhaled into the respiratory tract due to the comparative size of the oral cavity and bypassing the filtration of the nasal cavity.49 Differences in deposition can then affect clearance mechanisms and rates and ultimately infection kinetics for an inhaled pathogen (Fig. 1).
Clearance Mechanisms in the Respiratory Tract
Clearance kinetics are fundamental to determining the dose of deposited pathogens within the respiratory tract and ultimately systemically. A schematic of the interplay between deposition site, clearance mechanisms and pathogen dissemination from the respiratory tract is illustrated in Figure 1. The nose effectively filters foreign particles that enter the nasal cavity in a manner dependent on particle size and air flow rate with filtration efficiency decreasing with particle size.49 Once deposited, the speed of nasal clearance depends on the deposition location in the nasopharynx. In healthy humans, clearance from the ciliated anterior region is much more rapid than the non-ciliated poster region, ranging from 1.3 to 12.6 mm min−1.58 These rates are comparable to reported tracheal and bronchial mucociliary rates that range from 0.8 to 12.4 mm min−1.59,60 Similarities exist in animal models however clearance rates are generally more rapid due to the decreased distances required to reach the larynx.61
Both the nasal and tracheobronchial escalators comprise mucus that entraps deposited particulates and via the cumulative action of the cilia remove deposited material to the GI tract. Mucus composition is highly variable comprising glycoproteins (mucins), proteins, proteoglycans, and lipids. The quantities of these components present at any particular time govern the viscoelasticity, adhesiveness, and wettability of the mucus and can influence the size of particles emitted by coughing or sneezing.41,42,62 The diversity of oligosaccharide chains present on respiratory mucins and proteoglycans adds complexity providing a mechanism for microbial interaction and clearance.63 Factors such as underlying disease both infectious and non-infectious (e.g., cystic fibrosis, smoking, and diabetes) reduce mucociliary clearance rates,58,59,62,64 hence increasing residence time for deposited pathogens within the respiratory tract.
The pulmonary region is non-ciliated and clearance of foreign particulates is conducted by resident alveolar macrophages that phagocytose particles and transport to the local lung associated lymph nodes and play an important role in pulmonary immunity.65-67 Across species, numbers of alveolar macrophages increase in response to deposited foreign particles, however interspecies variability exists with respect to the rate of chemotaxis and phagocytosis.68
Pathogenesis as a Function of Particle Size in Animal Models
Lung and URT lymphoid tissue infections
No studies exist investigating the effects of particle size on respiratory infection in humans. However, comparative studies in animal models have been conducted using experimental systems that can differentially deposit pathogens in the LRT and URT within small or large particle aerosols.69-77 The general theme running through studies investigating the effects of aerosol particle size on infectivity is that greater numbers of pathogens need to deposit in the URT to produce lethal infection compared with the LRT (Tables 3 and 4). This is likely a function of the mucociliary escalators present in the nasal cavity and tracheobronchial regions clearing material to the gastrointestinal tract. An increased time to death was observed in animals that inhaled large particles that in time-course studies could be related to differences in pathogenesis between infections initiating in the LRT and URT.69-77
Table 3. Influence of aerosol particle size on the respiratory lethal dose values for respiratory pathogens.
| Particle size (μm) | Bacillus anthracis (cfu) | Yersinia pestis (cfu) | Francisella tularensis (cfu) | Brucella suis (cfu) | Burkholderia pseudomallei (cfu) | Coxiella burnetii (cfu) | VEEV (pfu) | EEEVa (pfu) | Ricinb (μg kg−1) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Animal species | Guinea pig | Mouse (A/Jola) | Guinea pig | Mouse (Balb/c) | Guinea pig | Rhesus macaque | Guinea pig | Mouse (Balb/c) | Guinea pig | Guinea pig | Guinea pig | Mouse (Balb/c) | Mouse (Balb/c) |
| 1.0–3.0 | 0.23–3.4 × 105 | 2.43 × 103 | 0.3–1.0 × 105 | 6.01 × 102 | 2.5 | 14–17.3 | ANNEX A 1.3–1.9 × 102 | 4.0–5.0 | 1.9 × 106 | 20 | 0.52–1.1 × 104 | 4.6–6.2 × 102 | 12.2 |
| 4.0–6.5 | 2.21 × 105 | ND | ND | ND | 6.5 × 103 | 2.4 × 102 | ND | ND | 5.27 × 107 | 1.9 × 104 | ND | ND | ND |
| 8.5–13.0 | 0.7–5.7 × 106 | 7.65 × 103 | 0.7–2.1 × 105 | 2.95 × 103 | 1.95 × 104 | 5.5–8.72 × 102 | ANNEX B 0.88–1.6 × 106 | 12.0 | > 2.4 × 109 | 2.8 × 105 | 3.0 × 104 | 2.9 × 105 | No lethality |
| 20.0–25.0 | ND | ND | ND | ND | ND | 3.75–4.45 × 103 | ND | ND | ND | ND | ND | ND | ND |
| Method 1–3 μm | COLL | COLL | COLL | COLL | NK | Atomizer | COLL | NK | NK | NK | COLL | COLL | COLL |
| Method >4 μm | STAG | FFAG | STAG | FFAG | NK | STAG | STAG | NK | NK | NK | STAG | STAG | STAG |
| References | 70 and 73 | 76 | 71 | 75 | 73 | 69 and 73 | 72 | 77 | 73 | 73 | 74 | 74 | 78 |
cfu, colony forming unit; COLL, Collison nebulizer; EEEV, eastern equine encephalitis virus; FFAG, flow-focusing aerosol generator; ND, not determined; NK, not known; pfu, plaque forming unit; STAG, spinning top aerosol generator; VEEV, Venezuelan Equine Encephalitis virus. a, values represent LD50 values from two virus strains (ArgM and NJ1959); b, no lethality using 45 µg kg−1
Table 4. Effect of aerosol particle size and deposition site on infection kinetics and pathology for selected pathogens in animal models of infection.
| Pathogen | Yersinia pestis (murine) | Bacillus anthracis (murine) | Burkholderia pseudomallei (murine) | Francisella tularensis (Rhesus macaque) | ||||
|---|---|---|---|---|---|---|---|---|
| Particle size | 1 | 12 | 1 | 12 | 1 | 12 | 1 | 12 |
| Deposition site | Lungs | Nasal mucosa | Lungs | Nasal mucosa | Lungs | Nasal mucosa | Lungs | Nasal mucosa |
| MLD (cfu) | 6.01 × 102 | 2.95 × 103 | 2.43 × 103 | 7.65 × 103 | 4 | 12 | 17 | 8.72 × 102 |
| MTTD (h) | 72 ± 0 | 90 ± 11.5 | 101.6 ± 10.4 | 161.0 ± 16.1 | 73.8 ± 11.3 | 174.7 ± 14.9 | 138.9 ± 8.8 | 224.5 ± 9.6 |
| Mortalitya (%) | 100 | 80 | 78 | 56 | 100 | 90 | 100 | 83 |
| Pathogenesis | 1° pneumonia | Nasal ulceration | BALT infection | Nasal ulceration | 1° pneumonia | Nasal ulceration | 1° pneumonia | Nasal ulceration |
| Splenitis | NALT infection | Mediastinal LN | NALT infection | Splenitis | NALT infection | Splenitis | Tonsillitis | |
| Septicemia | Cervical adenitis | Splenitis | Cervical adenitis | Septicemia | Cervical adenitis | Septicemia | Cervical adenitis | |
| Splenitis | Septicemia | Splenitis | Splenitis | Splenitis | ||||
| Septicemia | Septicemia | Septicemia | ||||||
| Primary gastritis | ||||||||
| 2° pneumonia | Peyer patches | Olfactory neuritis | Conjunctivitis | |||||
| Mesenteric LN | Brain abscess | |||||||
The inhalation of pathogens within small particle aerosols results in the typical disease profile associated with deposition in the alveolar region across all the rodent and NHP models used. Bacterial pathogens such as Francisella tularensis, Burkholderia pseudomallei, Brucella suis, and Yersinia pestis proliferate within the alveolar spaces or alveolar macrophages causing an influx of neutrophils that contribute to a massive cytokine storm resulting in edema and pneumonic consolidation characteristic of primary pneumonia. Eventually tissue destruction leads to dissemination to visceral organs, septic shock and death.69-72,75,76,79-82 B. pseudomallei is further characterized by the formation of abscesses throughout infected tissues and the potential to relapse after completion of antimicrobial therapy.77 B. anthracis endospores are phagocytosed by alveolar macrophages and dendritic cells and trafficked to lung-associated lymph nodes where they germinate and replicate destroying the lymph node before eventually disseminating via the bloodstream resulting in septicemic shock and toxemia.76,83
Deposition of these pathogens within the nasal cavity produces a different disease profile with some similarities across the different bacterial pathogens. Degradation and ulceration of the nasal epithelium precedes infection of the URT lymphoid tissues such as the nasal-associated lymphoid tissue (NALT) and tonsils. Eventually cervical lymphadenitis is observed prior to dissemination to other tissues and septic shock.69-72,75-77 NALT is the rodent equivalent of the Waldemeyer rings in primates comprising the adenoids and tonsils. Lung infection is often observed despite primary deposition in the URT. There are two reasons for this, first a limitation of the aerosol device that produces a polydisperse aerosol comprising some 1–3 µm particles in addition to the larger aerosol particle sizes. These will deposit in the alveoli producing dual infection of the LRT and URT in organisms such as B. pseudomallei that have a very low infectious dose of a few bacteria.77 Second, secondary pneumonia may occur very late in infection in mice that inhaled Y. pestis aerosolized within 12 µm particles resulting from hematogenous spread from the bloodstream into the alveolar spaces presumably after bacteraemic spread from the URT lymphoid tissues.71,75
Gastrointestinal, olfactory, and conjunctival infections from inhalational deposition
Intriguingly, differences in pathogenesis were observed between the bacterial pathogens upon deposition in the URT. In mice that inhaled 12 µm particles containing B. anthracis endospores GI pathology was observed with primary gastritis (17%), and activation and degeneration of GI lymphoid tissues such as the Peyer patches (72%) and mesenteric lymph nodes (67%).76 This pathology was not observed in other species, and is perhaps related to a combined effect of mucociliary clearance of the endospores to the stomach and the hardiness of endospores to the harsh acidic environment of the stomach. Bacteria such as Y. pestis, F. tularensis, and B. pseudomallei that do not produce GI pathology after URT deposition are much more sensitive to low acidity.84-86 Mice that inhaled B. pseudomallei within 12 µm particles demonstrated tropism toward the olfactory epithelium with sequential infection and resultant inflammatory responses within the olfactory neurone and olfactory bulb (100%) culminating in brain abscessation (33%).77 Similar observations were observed in an intranasal infection model.87 Ocular infection characterized by severe conjunctivitis associated with “purulent discharge from the nose and eyes” was observed in 16% of rhesus macaques that inhaled F. tularensis within 12–24 µm particles. In contrast, inhalation of 1–8 µm particles did not produce this pathology.69
In contrast, for the encephalitic alphaviruses, the demarcation between LRT and URT infection is much less marked demonstrating the difficulties in employing rigid health-related demarcations to particle size penetration into the respiratory tract. Mice challenged with 1–3 µm particle aerosols containing VEE virus or after intranasal deposition demonstrated neuroinvasion via trans-synaptic spread through the olfactory or trigeminal neuronal pathway to the brain. The terminal stages of infection were characterized by multifocal necrotising encephalitis.88-92 Intranasal deposition resulted in the presence of higher viral titers in the nasal mucosa, NALT, and cervical lymph nodes.90,93 Similarly, intranasal challenge in the Guinea pig resulted in targeted infection of the olfactory bulb prior to viremia.93 Similar pathogenesis has been observed in the Rhesus macaque, however, the virus localized in the olfactory bulb apparently not progressing to the brain.94,95 In eastern equine encephalitis virus (EEEV) the olfactory neuronal pathway is important for inhalational but not parenteral routes of infection in rodent models.74,92 Utilization of the olfactory neurone to cross the cribriform plate into the central nervous system has also been observed in URT infection models for Nipah virus, Japanese encephalitis virus, Hendra virus, herpes simplex virus, influenza virus (H5N1 subtype), Borna virus, Balamuthia mandrillaris, Naegleria fowleri, B. pseudomallei, Streptococcus pneumoniae, Listeria monocytogenes, and Neisseria meningitidis.77,87,96-105 Interestingly, recently differential phagocytosis of Escherichia coli and Burkholderia thailandensis was observed in vitro by olfactory sheathing and Schwann cells perhaps representing a mechanism for colonization, infection, or clearance.155
These studies demonstrate that deposition site can profoundly influence infection kinetics and pathogenesis within inhalational animal models. Depending on the initial site of deposition and clearance kinetics, aerosolized pathogens may come into contact with a range of tissues and organs through which infection may occur: nasal mucosa, nasal and URT lymphoid tissues, olfactory epithelium, bronchoalveolar epithelium, gastrointestinal tract, and ocular conjunctiva.
Can CDC Select Agents Cause Infection of the URT in Humans?
In the United States, possession and transfer of biothreat agents is regulated under the Select Agent Program (SAP) administered by the Centers for Disease Control and Prevention (CDC). The pathogens and toxins controlled by the SAP are commonly referred to as select agents and represent a potential severe threat to the health and agriculture sectors. This review specifically deals with those select agents that are harmful to humans.
It is difficult to extrapolate animal studies to humans directly because time-course data are not available in humans and therefore the intricacies of pathogenesis cannot be related to respiratory tract deposition. The reported pathology in human cases of inhalational infections is generally from terminal cases or during treatment regimens where the infection is already at a progressed stage and it is difficult to be certain where the infection initiated. It is further complicated by the high mortality, often approaching 90%, for the LRT infections caused by these pathogens.
However, cases of human infections caused by select agents occur that originate in the URT and demonstrate similar pathology to that described in inhalational animal infection models of the URT. Patients present with febrile illness, tonsillitis, pharyngitis, and cervical lymphadenitis prior to septicemia (Table 5). These presentations are generally termed pharyngeal or oro-pharyngeal infections and are predominantly associated with consumption of contaminated meats or water for Y. pestis,106-110 B. anthracis,111-118 and F. tularensis.119-123 B. pseudomallei presents as a pharyngocervical infection predominantly in children, however there are adult cases.124-129
Table 5. Upper respiratory tract symptoms in bacterial select agents.
| Symptoms | Percentage of patients with symptom (%) | |||||
|---|---|---|---|---|---|---|
| Plaguea (Pharyngeal) | Tularemia (Oropharyngeal) | Anthrax (Nasopharynx) | Anthrax (Oropharyngeal) | Anthrax (Laryngeal) | Melioidosis (Pharyngocervical) | |
| Fever | 92 | 96 | 83 | 97 | 50 | 60 |
| Tonsillitis | 75 | - | - | 63 | - | 15 |
| Pharyngitis | 92 | 81 | 33 | 72 | - | 30 |
| Nasal/sinus complaints | - | - | 83 | 3 | 0 | 10 |
| Malaise/fatigue | 92 | 54 | 33 | - | 25 | - |
| Headache | 92 | 62 | 17 | 6 | 0 | - |
| Cervical/submandibular lymphadenitis | 83 | 92 | 50 | 100 | - | 85 |
| Arthralgia/myalgia | 83 | 35 | - | - | - | 5 |
| Abdominal pain | 50 | - | 17 | 25 | - | |
| Vomiting/nausea | 50 | - | 0 | 3 | 25 | 5 |
| Cough | 42 | - | 0 | 6 | 0 | 5 |
| Dysphagia | 17 | - | 17 | - | 0 | - |
| Diarrhea | 17 | - | - | 3 | - | - |
| Hemoptysis/dyspnea | 8 | - | 17 | 39 | 75 | - |
| Anorexia | - | 46 | 17 | - | - | - |
| Depression | - | 50 | 17 | - | 0 | - |
| Concentration | - | 42 | - | - | - | - |
| Sleep disturbance | - | 46 | - | - | - | - |
| Mortality | 40% | < 10% | 50% | 40% | 50% | < 10% |
| Treatable | + | + | + | + | + | + |
Two respiratory forms of plague have been observed from outbreaks of bubonic and pneumonic plague, one that results in primary pneumonia and a second that results in tonsillitis and cervical lymphadenopathy in the absence of pneumonia.130-133 Flexner131 and Crowell130 respectively stated that “of all the buccal structures, the tonsils seem to be most frequently the one attacked” and “tonsils have formed the portal of entrance for the bacilli and that the involvement of the cervical glands occurs secondarily through the lymph stream”. Meyer133 further implied that “perhaps only the larger particles can lodge in the URT and give rise to tonsillar or septicemic plague”. The described URT pathology closely resembles that observed in NHPs, Guinea pigs, and mice (Table 4).71,75,133 Interestingly, Guinea pigs suffering from pneumonic plague demonstrated 17% cross-infection to healthy control animals during cross-infection studies. The cross-infected animals all suffered from the URT infection.75 It was implied that this may be a contributory factor toward the cessation of pneumonic plague outbreaks because the URT form is less infectious and has reduced mortality rates.133 It is noteworthy that for B. anthracis,117,134 B. melitensis,135 B. mallei,136,137 and Coxiella burnetii138 there are also bona fide cases of inhalational infections that lack LRT involvement and present with the aforementioned pathology indicative of primary infection via the URT. Furthermore, in humans, VEE, WEE, and EEE viruses can infect via the inhalational route and cause neurological sequelae similar to that observed in animal models.139 However it is not known in humans whether the olfactory neurone plays a role in the pathogenesis of these viruses or B. pseudomallei.
These cases demonstrate that in humans these pathogens can produce infection via the URT and although mortality is reduced compared with the respective LRT infections, the rates are not insignificant if untreated (Table 5). Similar to the LRT infection, the URT infections caused by select agents are treatable by intervention with antimicrobial therapy, and prognosis is good if promptly administered. Furthermore, the window of opportunity is longer compared with the LRT infection due to the protracted course of infection. However, misdiagnosis is problematic resulting in incorrect treatment regimens because symptoms resemble common URT diseases. For example, similar URT pathogenesis characterized by adenotonsillar disease, pharyngitis and /or cervical adenitis has been observed for a range of common pathogens including respiratory viruses, measles virus, Staphylococcus aureus, Hemophilus influenzae, Streptococcus pyogenes, Streptococcus pneumoniae, and Mycobacterium spp.140-146
Gastrointestinal anthrax, different from the oropharyngeal form, is known to occur in humans due to consumption of contaminated meats with mortality rates reaching 29% if untreated. It presents typically as a febrile illness with severe abdominal pain, mesenteric lymphadenopathy, hemorrhagic ascites, hematemesis, and diarrhea.115 Complications can include hemorrhagic gastritis.147 Interestingly, a recent case of GI anthrax occurred after exposure to endospores aerosolized during drumming, the inference being that the deposited endospores were cleared from the respiratory tract to the GI tract.148 This supports observations in mice where infection of the GI tract occurred in mice that inhaled 12 µm particles containing B. anthracis endospores with pathology similar to that described for humans.76
Conjunctivitis was observed in NHPs exposed to 12–24 µm particles containing F. tularensis.69 In humans, F. tularensis can cause a rare presentation known as oculoglandular syndrome characterized by conjunctivitis, ulceration and preauricular lymphadenitis,149 although this appears to be a result of direct contact with fomites or vector-borne rather than airborne transmission.
Conclusions
It is difficult to predict the particle size that an individual may inhale from a bioaerosol because any source comprises a particle distribution (Table 1) that changes with time and distance due to the local climate (e.g., meteorology, turbulent activity, ventilation, etc.) and removal from the air column. As such, from the view-point of inhalational infections the respiratory tract should be considered as a continuum with deposition occurring throughout and the probability of infection dependent on the interplay between respiratory physiology, regional dose, clearance kinetics, host-pathogen colonisation mechanisms and immunological response. Therefore, a range of tissues that have perhaps not been thought of as routes of inhalational challenge are brought into consideration including the URT lymphoid tissues, olfactory system, GI tract and potentially the ophthalmic system.
The site of deposition after an inhalational event can affect disease kinetics and pathogenesis, however, the deposition of respiratory pathogens in the lungs will generally result in the more rapid aggressive infection with higher mortality rates. However, evidence exists in both animal models and humans for a number of select agents for URT infections involving the URT lymphoid tissues as the initial foci followed by dissemination via the cervical lymph nodes and bacteremic spread. In addition to LRT presentations, other presentations have been observed in a pathogen specific manner including neurological infection via the olfactory system, GI tract infection, and conjunctivitis.
Increased understanding of the pathogenesis and immunology of infections resulting from inhalation and resultant clearance will aid in the development of vaccine candidates and antimicrobial regimens. Research into host-pathogen interactions and the immunology of URT infections is still in its infancy compared with LRT and systemic infections.67,80,150 However, recent years have seen an increased understanding of host-pathogen and pathogen-pathogen interactions throughout the URT and the function of immunological tissues.151-153 In humans it is unknown whether the olfactory system is utilized as a direct pathway from the URT to the brain. However, it remains a potential route and only recently has the immune response within the olfactory system been researched for viruses154 and the picture is even less clear for bacteria.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgments
The author recognizes the contribution of Ministry of Defense funding for aspects of work covered by this review. © Crown copyright 2013. Published with the permission of the Defence Science and Technology Laboratory on behalf of the Controller of HMSO.
Footnotes
Previously published online: www.landesbioscience.com/journals/virulence/article/27172
References
- 1.Jewett DL, Heinsohn P, Bennett C, Rosen A, Neuilly C. Blood-containing aerosols generated by surgical techniques: a possible infectious hazard. Am Ind Hyg Assoc J. 1992;53:228–31. doi: 10.1080/15298669291359564. [DOI] [PubMed] [Google Scholar]
- 2.Szymańska J. Dental bioaerosol as an occupational hazard in a dentist’s workplace. Ann Agric Environ Med. 2007;14:203–7. [PubMed] [Google Scholar]
- 3.Greene VW, Vesley D, Bond RG, Michaelsen GS. Microbiological contamination of hospital air. I. Quantitative studies. Appl Microbiol. 1962;10:561–6. doi: 10.1128/am.10.6.561-566.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang JW, Li Y, Eames I, Chan PKS, Ridgway GL. Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. J Hosp Infect. 2006;64:100–14. doi: 10.1016/j.jhin.2006.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts K, Hathway A, Fletcher LA, Beggs CB, Elliott MW, Sleigh PA. Bioaerosol production on a respiratory ward. Indoor Built Environ. 2006;15:35–40. doi: 10.1177/1420326X06062562. [DOI] [Google Scholar]
- 6.Rothman T, Ledbetter JO. Droplet size of cooling tower fog. Environ Lett. 1975;10:191–203. doi: 10.1080/00139307509435821. [DOI] [PubMed] [Google Scholar]
- 7.Bausum HT, Schaub SA, Kenyon KF, Small MJ. Comparison of coliphage and bacterial aerosols at a wastewater spray irrigation site. Appl Environ Microbiol. 1982;43:28–38. doi: 10.1128/aem.43.1.28-38.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee S-A, Adhikari A, Grinshpun SA, McKay R, Shukla R, Reponen T. Personal exposure to airborne dust and microorganisms in agricultural environments. J Occup Environ Hyg. 2006;3:118–30. doi: 10.1080/15459620500524607. [DOI] [PubMed] [Google Scholar]
- 9.Olsen KN, Lund M, Skov J, Christensen LS, Hoorfar J. Detection of Campylobacter bacteria in air samples for continuous real-time monitoring of Campylobacter colonization in broiler flocks. Appl Environ Microbiol. 2009;75:2074–8. doi: 10.1128/AEM.02182-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rathburn CB, Jr., Dukes JC. A comparison of the mortality of caged adult mosquitoes to the size, number and volume of ULV spray droplets sampled in an open and a vegetated area. J Am Mosq Control Assoc. 1989;5:173–5. [PubMed] [Google Scholar]
- 11.Mount GA. A critical review of ultralow-volume aerosols of insecticide applied with vehicle-mounted generators for adult mosquito control. J Am Mosq Control Assoc. 1998;14:305–34. [PubMed] [Google Scholar]
- 12.Kim JS, Je YH. Milling effect on the control efficacy of spray-dried Bacillus thuringiensis technical powder against diamondback moths. Pest Manag Sci. 2012;68:321–3. doi: 10.1002/ps.2330. [DOI] [PubMed] [Google Scholar]
- 13.Rosas-García NM. Laboratory and field tests of spray-dried and granular formulations of a Bacillus thuringiensis strain with insecticidal activity against the sugarcane borer. Pest Manag Sci. 2006;62:855–61. doi: 10.1002/ps.1245. [DOI] [PubMed] [Google Scholar]
- 14.Teschke K, Chow Y, Bartlett K, Ross A, van Netten C. Spatial and temporal distribution of airborne Bacillus thuringiensis var. kurstaki during an aerial spray program for gypsy moth eradication. Environ Health Perspect. 2001;109:47–54. doi: 10.1289/ehp.0110947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiGiovanni F, Kevan PG. Factors affecting pollen dynamics and its importance to pollen contamination: a review. Can J Res. 1991;21:1155–70. doi: 10.1139/x91-163. [DOI] [Google Scholar]
- 16.Brown JKM, Hovmøller MS. Aerial dispersal of pathogens on the global and continental scales and its impact on plant disease. Science. 2002;297:537–41. doi: 10.1126/science.1072678. [DOI] [PubMed] [Google Scholar]
- 17.Brandl H, Bachofen R, Bischoff M. Generation of bioaerosols during manual mail unpacking and sorting. J Appl Microbiol. 2005;99:1099–107. doi: 10.1111/j.1365-2672.2005.02700.x. [DOI] [PubMed] [Google Scholar]
- 18.Barrabeig I, Rovira A, Garcia M, Oliva JM, Vilamala A, Ferrer MD, Sabrià M, Domínguez A. Outbreak of Legionnaires’ disease associated with a supermarket mist machine. Epidemiol Infect. 2010;138:1823–8. doi: 10.1017/S0950268810000841. [DOI] [PubMed] [Google Scholar]
- 19.Baylor ER, Peters V, Baylor MB. Water-to-air transfer of virus. Science. 1977;197:763–4. doi: 10.1126/science.329413. [DOI] [PubMed] [Google Scholar]
- 20.Baron PA, Willeke K. Respirable droplets from whirlpools: measurements of size distribution and estimation of disease potential. Environ Res. 1986;39:8–18. doi: 10.1016/S0013-9351(86)80003-2. [DOI] [PubMed] [Google Scholar]
- 21.Morawska L, Johnson GR, Ristovski ZD, Hargreaves M, Mengersen K, Corbett S, et al. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. Aero Sci. 2009;40:256–69. doi: 10.1016/j.jaerosci.2008.11.002. [DOI] [Google Scholar]
- 22.Chao CYH, Wan MP, Morawska L, Johnson GR, Ritovski ZD, Hargreaves M, et al. Characterization of expiration air jets and droplet size distributions immediately at the mouth opening. Aerosol Sci. 2009;40:122–33. doi: 10.1016/j.jaerosci.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xie X, Li Y, Sun H, Liu L. Exhaled droplets due to talking and coughing. J R Soc Interface. 2009;6(Suppl 6):S703–14. doi: 10.1098/rsif.2009.0388.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lai KM, Bottomley C, McNerney R. Propagation of respiratory aerosols by the vuvuzela. PLoS One. 2011;6:e20086. doi: 10.1371/journal.pone.0020086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang S, Lee GWM, Chen C-M, Wu C-C, Yu K-P. The size and concentration of droplets generated by coughing in human subjects. J Aerosol Med. 2007;20:484–94. doi: 10.1089/jam.2007.0610. [DOI] [PubMed] [Google Scholar]
- 26.Fennelly KP, Martyny JW, Fulton KE, Orme IM, Cave DM, Heifets LB. Cough-generated aerosols of Mycobacterium tuberculosis: a new method to study infectiousness. Am J Respir Crit Care Med. 2004;169:604–9. doi: 10.1164/rccm.200308-1101OC. [DOI] [PubMed] [Google Scholar]
- 27.Lindsley WG, Blachere FM, Thewlis RE, Vishnu A, Davis KA, Cao G, Palmer JE, Clark KE, Fisher MA, Khakoo R, et al. Measurements of airborne influenza virus in aerosol particles from human coughs. PLoS One. 2010;5:e15100. doi: 10.1371/journal.pone.0015100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duguid JP. The numbers and the sites of origin of the droplets expelled during expiratory activities. Edinb Med J. 1945;52:385–401. [PMC free article] [PubMed] [Google Scholar]
- 29.Jennison MW. Atomizing of mouth and nose secretions into the air as revealed by high-speed photography. Aerobiol. 1942;17:106–28. [Google Scholar]
- 30.Zhou Y, Benson JM, Irvin C, Irshad H, Cheng Y-S. Particle size distribution and inhalation dose of shower water under selected operating conditions. Inhal Toxicol. 2007;19:333–42. doi: 10.1080/08958370601144241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blatny JM, Fossum H, Ho J, Tutkun M, Skogan G, Andreassen O, Fykse EM, Waagen V, Reif BA. Dispersion of Legionella-containing aerosols from a biological treatment plant, Norway. Front Biosci (Elite Ed) 2011;3:1300–9. doi: 10.2741/e333. [DOI] [PubMed] [Google Scholar]
- 32.Ruiz A, Bulmer GS. Particle size of airborn Cryptococcus neoformans in a tower. Appl Environ Microbiol. 1981;41:1225–9. doi: 10.1128/aem.41.5.1225-1229.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gralton J, Tovey E, McLaws M-L, Rawlinson WD. The role of particle size in aerosolised pathogen transmission: a review. J Infect. 2011;62:1–13. doi: 10.1016/j.jinf.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fernstrom A, Goldblatt M. Aerobiology and its role in the transmission of infectious diseases. J Pathog. 2013;2013:493960. doi: 10.1155/2013/493960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams CG. Long-distance pine pollen still germinates after meso-scale dispersal. Am J Bot. 2010;97:846–55. doi: 10.3732/ajb.0900255. [DOI] [PubMed] [Google Scholar]
- 36.Loudon RG, Roberts RM. Droplet expulsion from the respiratory tract. Am Rev Respir Dis. 1967;95:435–42. doi: 10.1164/arrd.1967.95.3.435. [DOI] [PubMed] [Google Scholar]
- 37.Loudon RG, Roberts RM. Relation between the airborne diameters of respiratory droplets and the diameter of the stains left after recovery. Nature. 1967;213:95–6. doi: 10.1038/213095a0. [DOI] [Google Scholar]
- 38.Nicas M, Nazaroff WW, Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J Occup Environ Hyg. 2005;2:143–54. doi: 10.1080/15459620590918466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Papineni RS, Rosenthal FS. The size distribution of droplets in the exhaled breath of healthy human subjects. J Aerosol Med. 1997;10:105–16. doi: 10.1089/jam.1997.10.105. [DOI] [PubMed] [Google Scholar]
- 40.Zhou B, Zhang Z, Li X. Numerical study of the transport of droplets or particles generated by respiratory system indoors. Build Environ. 2005;40:1032–9. doi: 10.1016/j.buildenv.2004.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hersen G, Moularat S, Robine E, Ghin E, Corbet S, Vabret A. Impact of health on particle size of exhaled respiratory aerosols: case-control study. Clean. 2008;36:572–7. doi: 10.1002/clen.200700189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Girod S, Zahm J-M, Plotkowski C, Beck G, Puchelle E. Role of the physiochemical properties of mucus in the protection of the respiratory epithelium. Eur Respir J. 1992;5:477–87. [PubMed] [Google Scholar]
- 43.Finlay WH, Stapleton KW, Chan HK, Zuberbuhler P, Gonda I. Regional deposition of inhaled hygroscopic aerosols: in vivo SPECT compared with mathematical modeling. J Appl Physiol (1985) 1996;81:374–83. doi: 10.1152/jappl.1996.81.1.374. [DOI] [PubMed] [Google Scholar]
- 44.Wang C-S. Inhaled Particles. Interface Sci Tech. 2005;5:1–187. [Google Scholar]
- 45.Belser JA, Rota PA, Tumpey TM. Ocular tropism of respiratory viruses. Microbiol Mol Biol Rev. 2013;77:144–56. doi: 10.1128/MMBR.00058-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Caul EO. Small round structured viruses: airborne transmission and hospital control. Lancet. 1994;343:1240–2. doi: 10.1016/S0140-6736(94)92146-6. [DOI] [PubMed] [Google Scholar]
- 47.Marks PJ, Vipond IB, Carlisle D, Deakin D, Fey RE, Caul EO. Evidence for airborne transmission of Norwalk-like virus (NLV) in a hotel restaurant. Epidemiol Infect. 2000;124:481–7. doi: 10.1017/S0950268899003805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roberts K, Smith CF, Snelling AM, Kerr KG, Banfield KR, Sleigh PA, Beggs CB. Aerial dissemination of Clostridium difficile spores. BMC Infect Dis. 2008;8:7. doi: 10.1186/1471-2334-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.ICRP. Annals of the ICRP – Human respiratory tract model for radiological protection. In. Smith H, (ed), New York. Pergamon. 1994. [Google Scholar]
- 50.Heyder J, Gebhart J, Rudolf G, Schiller CF, Stahlhofen W. Deposition of particles in the human respiratory tract in the size range 0.005-15 µm. J Aerosol Sci. 1986;5:811–25. doi: 10.1016/0021-8502(86)90035-2. [DOI] [Google Scholar]
- 51.Raabe OG, Al-Bayati MA, Teague SV, Rasolt A. Regional deposition of inhaled monodisperse coarse and fine aerosol particles in small laboratory animals. Ann Occup Hyg. 1988;3:53–63. doi: 10.1093/annhyg/32.inhaled_particles_VI.53. [DOI] [Google Scholar]
- 52.Schlesinger RB. Comparative deposition of inhaled aerosols in experimental animals and humans: a review. J Toxicol Environ Health. 1985;15:197–214. doi: 10.1080/15287398509530647. [DOI] [PubMed] [Google Scholar]
- 53.Ménache MG, Miller FJ, Raabe OG. Particle inhalability curves for humans and small laboratory animals. Ann Occup Hyg. 1995;39:317–28. [PubMed] [Google Scholar]
- 54.Kuehl PJ, Anderson TL, Candelaria G, Gershman B, Harlin K, Hesterman JY, Holmes T, Hoppin J, Lackas C, Norenberg JP, et al. Regional particle size dependent deposition of inhaled aerosols in rats and mice. Inhal Toxicol. 2012;24:27–35. doi: 10.3109/08958378.2011.632787. [DOI] [PubMed] [Google Scholar]
- 55.Schreider JP, Raabe OG. Anatomy of the nasal-pharyngeal airway of experimental animals. Anat Rec. 1981;200:195–205. doi: 10.1002/ar.1092000208. [DOI] [PubMed] [Google Scholar]
- 56.Oldham MJ, Phalen RF. Dosimetry implications of upper tracheobronchial airway anatomy in two mouse varieties. Anat Rec. 2002;268:59–65. doi: 10.1002/ar.10134. [DOI] [PubMed] [Google Scholar]
- 57.Schulz H, Johner C, Eder G, Ziesenis A, Reitmeier P, Heyder J, Balling R. Respiratory mechanics in mice: strain and sex specific differences. Acta Physiol Scand. 2002;174:367–75. doi: 10.1046/j.1365-201x.2002.00955.x. [DOI] [PubMed] [Google Scholar]
- 58.Puchelle E, Aug F, Zahm JM, Bertrand A. Comparison of nasal and bronchial mucociliary clearance in young non-smokers. Clin Sci (Lond) 1982;62:13–6. doi: 10.1042/cs0620013. [DOI] [PubMed] [Google Scholar]
- 59.Yeates DB, Aspin N, Levison H, Jones MT, Bryan AC. Mucociliary tracheal transport rates in man. J Appl Physiol. 1975;39:487–95. doi: 10.1152/jappl.1975.39.3.487. [DOI] [PubMed] [Google Scholar]
- 60.Foster WM, Langenback E, Bergofsky EH. Measurement of tracheal and bronchial mucus velocities in man: relation to lung clearance. J Appl Physiol Respir Environ Exerc Physiol. 1980;48:965–71. doi: 10.1152/jappl.1980.48.6.965. [DOI] [PubMed] [Google Scholar]
- 61.Lippmann M, Schlesinger RB. Interspecies comparisons of particle deposition and mucociliary clearance in tracheobronchial airways. J Toxicol Environ Health. 1984;13:441–69. doi: 10.1080/15287398409530509. [DOI] [PubMed] [Google Scholar]
- 62.Beule AG. Physiology and pathophysiology of respiratory mucosa of the nose and the paranasal sinuses. GMS Current Topics in Otorhinology –. Head Neck Surg. 2010;9:1–24. doi: 10.3205/cto000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lamblin G, Aubert JP, Perini JM, Klein A, Porchet N, Degand P, Roussel P. Human respiratory mucins. Eur Respir J. 1992;5:247–56. [PubMed] [Google Scholar]
- 64.Regnis JA, Robinson M, Bailey DL, Cook P, Hooper P, Chan H-K, Gonda I, Bautovich G, Bye PT. Mucociliary clearance in patients with cystic fibrosis and in normal subjects. Am J Respir Crit Care Med. 1994;150:66–71. doi: 10.1164/ajrccm.150.1.8025774. [DOI] [PubMed] [Google Scholar]
- 65.Sherman MP, Ganz T. Host defense in pulmonary alveoli. Annu Rev Physiol. 1992;54:331–50. doi: 10.1146/annurev.ph.54.030192.001555. [DOI] [PubMed] [Google Scholar]
- 66.Yoshida M, Whitsett JA. Interactions between pulmonary surfactant and alveolar macrophages in the pathogenesis of lung disease. Cell Mol Biol (Noisy-le-grand) 2004;50 Online Pub:OL639–48. [PubMed] [Google Scholar]
- 67.Eddens T, Kolls JK. Host defenses against bacterial lower respiratory tract infection. Curr Opin Immunol. 2012;24:424–30. doi: 10.1016/j.coi.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Warheit DB, Hartsky MA. Role of alveolar macrophage chemotaxis and phagocytosis in pulmonary clearance responses to inhaled particles: comparisons among rodent species. Microsc Res Tech. 1993;26:412–22. doi: 10.1002/jemt.1070260509. [DOI] [PubMed] [Google Scholar]
- 69.Day WC, Berendt RF. Experimental tularemia in Macaca mulatta: relationship of aerosol particle size to the infectivity of airborne Pasteurella tularensis. Infect Immun. 1972;5:77–82. doi: 10.1128/iai.5.1.77-82.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Druett HA, Henderson DW, Packman LP, Peacock S. Studies on respiratory infection. I. The influence of particle size on respiratory infection with anthrax spores. J Hyg (Lond) 1953;51:359–71. doi: 10.1017/S0022172400015795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Druett HA, Robinson JM, Henderson DW, Packman L, Peacock S. Studies on respiratory infection. II. The influence of aerosol particle size on infection of the guinea-pig with Pasteurella pestis. J Hyg (Lond) 1956;54:37–48. doi: 10.1017/S0022172400044284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Druett HA, Henderson DW, Peacock S. Studies on respiratory infection. III. Experiments with Brucella suis. J Hyg (Lond) 1956;54:49–57. doi: 10.1017/S0022172400044296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fothergill LD. Biological warfare – Nature and consequences. Tex Med. 1964;60:8–14. [PubMed] [Google Scholar]
- 74.Roy CJ, Reed DS, Wilhelmsen CL, Hartings J, Norris S, Steele KE. Pathogenesis of aerosolized Eastern Equine Encephalitis virus infection in guinea pigs. Virol J. 2009;6:170–83. doi: 10.1186/1743-422X-6-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Thomas RJ, Webber D, Collinge A, Stagg AJ, Bailey SC, Nunez A, Gates A, Jayasekera PN, Taylor RR, Eley S, et al. Different pathologies but equal levels of responsiveness to the recombinant F1 and V antigen vaccine and ciprofloxacin in a murine model of plague caused by small- and large-particle aerosols. Infect Immun. 2009;77:1315–23. doi: 10.1128/IAI.01473-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Thomas RJ, Davies C, Nunez A, Hibbs S, Flick-Smith H, Eastaugh L, Smither S, Gates A, Oyston P, Atkins T, et al. Influence of particle size on the pathology and efficacy of vaccination in a murine model of inhalational anthrax. J Med Microbiol. 2010;59:1415–27. doi: 10.1099/jmm.0.024117-0. [DOI] [PubMed] [Google Scholar]
- 77.Thomas RJ, Davies C, Nunez A, Hibbs S, Eastaugh L, Harding S, et al. Particle-size dependent effects in the Balb/c murine model of inhalational melioidosis. Front Cell Infect Microbiol. 2012;2:1–12. doi: 10.3389/fcimb.2012.00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Roy CJ, Hale M, Hartings JM, Pitt L, Duniho S. Impact of inhalation exposure modality and particle size on the respiratory deposition of ricin in BALB/c mice. Inhal Toxicol. 2003;15:619–38. doi: 10.1080/08958370390205092. [DOI] [PubMed] [Google Scholar]
- 79.Agar SL, Sha J, Foltz SM, Erova TE, Walberg KG, Parham TE, Baze WB, Suarez G, Peterson JW, Chopra AK. Characterization of a mouse model of plague after aerosolization of Yersinia pestis CO92. Microbiology. 2008;154:1939–48. doi: 10.1099/mic.0.2008/017335-0. [DOI] [PubMed] [Google Scholar]
- 80.Weiner ZP, Glomski IJ. Updating perspectives on the initiation of Bacillus anthracis growth and dissemination through its host. Infect Immun. 2012;80:1626–33. doi: 10.1128/IAI.06061-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.West TE, Myers ND, Liggitt HD, Skerrett SJ. Murine pulmonary infection and inflammation induced by inhalation of Burkholderia pseudomallei. Int J Exp Pathol. 2012;93:421–8. doi: 10.1111/j.1365-2613.2012.00842.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Henning LN, Miller SM, Pak DH, Lindsay A, Fisher DA, Barnewall RE, Briscoe CM, Anderson MS, Warren RL. Pathophysiology of the rhesus macaque model for inhalational brucellosis. Infect Immun. 2012;80:298–310. doi: 10.1128/IAI.05878-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Twenhafel NA. Pathology of inhalational anthrax animal models. Vet Pathol. 2010;47:819–30. doi: 10.1177/0300985810378112. [DOI] [PubMed] [Google Scholar]
- 84.Butler T, Fu YS, Furman L, Almeida C, Almeida A. Experimental Yersinia pestis infection in rodents after intragastric inoculation and ingestion of bacteria. Infect Immun. 1982;36:1160–7. doi: 10.1128/iai.36.3.1160-1167.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.KuoLee R, Zhao X, Austin J, Harris G, Conlan JW, Chen W. Mouse model of oral infection with virulent type A Francisella tularensis. Infect Immun. 2007;75:1651–60. doi: 10.1128/IAI.01834-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.West TE, Myers ND, Limmathurotsakul D, Liggitt HD, Chantratita N, Peacock SJ, Skerrett SJ. Pathogenicity of high-dose enteral inoculation of Burkholderia pseudomallei to mice. Am J Trop Med Hyg. 2010;83:1066–9. doi: 10.4269/ajtmh.2010.10-0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Owen SJ, Batzloff M, Chehrehasa F, Meedeniya A, Casart Y, Logue CA, Hirst RG, Peak IR, Mackay-Sim A, Beacham IR. Nasal-associated lymphoid tissue and olfactory epithelium as portals of entry for Burkholderia pseudomallei in murine melioidosis. J Infect Dis. 2009;199:1761–70. doi: 10.1086/599210. [DOI] [PubMed] [Google Scholar]
- 88.Charles PC, Walters E, Margolis F, Johnston RE. Mechanism of neuroinvasion of Venezuelan equine encephalitis virus in the mouse. Virology. 1995;208:662–71. doi: 10.1006/viro.1995.1197. [DOI] [PubMed] [Google Scholar]
- 89.Ryzhikov AB, Ryabchikova EI, Sergeev AN, Tkacheva NV. Spread of Venezuelan equine encephalitis virus in mice olfactory tract. Arch Virol. 1995;140:2243–54. doi: 10.1007/BF01323243. [DOI] [PubMed] [Google Scholar]
- 90.Vogel P, Abplanalp D, Kell W, Ibrahim MS, Downs MB, Pratt WD, Davis KJ. Venezuelan equine encephalitis in BALB/c mice: kinetic analysis of central nervous system infection following aerosol or subcutaneous inoculation. Arch Pathol Lab Med. 1996;120:164–72. [PubMed] [Google Scholar]
- 91.Steele KE, Davis KJ, Stephan K, Kell W, Vogel P, Hart MK. Comparative neurovirulence and tissue tropism of wild-type and attenuated strains of Venezuelan equine encephalitis virus administered by aerosol in C3H/HeN and BALB/c mice. Vet Pathol. 1998;35:386–97. doi: 10.1177/030098589803500508. [DOI] [PubMed] [Google Scholar]
- 92.Steele KE, Twenhafel NA. REVIEW PAPER: pathology of animal models of alphavirus encephalitis. Vet Pathol. 2010;47:790–805. doi: 10.1177/0300985810372508. [DOI] [PubMed] [Google Scholar]
- 93.Danes L, Rychterová V, Kliment V, Hrusková J. Penetration of Venezuelan equine encephalomyelitis virus into the brain of guinea pigs and rabbits after intranasal infection. Acta Virol. 1973;17:138–46. [PubMed] [Google Scholar]
- 94.Danes L, Kufner J, Hrusková J, Rychterová V. The role of the olfactory route on infection of the respiratory tract with Venezuelan equine encephalomyelitis virus in normal and operated Macaca rhesus monkeys. I. Results of virological examination. Acta Virol. 1973;17:50–6. [PubMed] [Google Scholar]
- 95.Danes L, Rychterová V, Kufner J, Hrusková J. The role of the olfactory route on infection of the respiratory tract with Venezuelan equine encephalomyelitis virus in normal and operated Macaca rhesus monkeys. II. Results of histological examination. Acta Virol. 1973;17:57–60. [PubMed] [Google Scholar]
- 96.Jarolim KL, McCosh JK, Howard MJ, John DT. A light microscopy study of the migration of Naegleria fowleri from the nasal submucosa to the central nervous system during the early stage of primary amebic meningoencephalitis in mice. J Parasitol. 2000;86:50–5. doi: 10.1645/0022-3395(2000)086[0050:ALMSOT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 97.Jin Y, Dons L, Kristensson K, Rottenberg ME. Neural route of cerebral Listeria monocytogenes murine infection: role of immune response mechanisms in controlling bacterial neuroinvasion. Infect Immun. 2001;69:1093–100. doi: 10.1128/IAI.69.2.1093-1100.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kiderlen AF, Laube U. Balamuthia mandrillaris, an opportunistic agent of granulomatous amebic encephalitis, infects the brain via the olfactory nerve pathway. Parasitol Res. 2004;94:49–52. doi: 10.1007/s00436-004-1163-z. [DOI] [PubMed] [Google Scholar]
- 99.van Ginkel FW, McGhee JR, Watt JM, Campos-Torres A, Parish LA, Briles DE. Pneumococcal carriage results in ganglioside-mediated olfactory tissue infection. Proc Natl Acad Sci U S A. 2003;100:14363–7. doi: 10.1073/pnas.2235844100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yamada M, Nakamura K, Yoshii M, Kaku Y, Narita M. Brain lesions induced by experimental intranasal infection of Japanese encephalitis virus in piglets. J Comp Pathol. 2009;141:156–62. doi: 10.1016/j.jcpa.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 101.Mori I, Nishiyama Y, Yokochi T, Kimura Y. Olfactory transmission of neurotropic viruses. J Neurovirol. 2005;11:129–37. doi: 10.1080/13550280590922793. [DOI] [PubMed] [Google Scholar]
- 102.Sjölinder H, Jonsson A-B. Olfactory nerve--a novel invasion route of Neisseria meningitidis to reach the meninges. PLoS One. 2010;5:e14034. doi: 10.1371/journal.pone.0014034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dups J, Middleton D, Yamada M, Monaghan P, Long F, Robinson R, Marsh GA, Wang LF. A new model for Hendra virus encephalitis in the mouse. PLoS One. 2012;7:e40308. doi: 10.1371/journal.pone.0040308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Munster VJ, Prescott JB, Bushmaker T, Long D, Rosenke R, Thomas T, Scott D, Fischer ER, Feldmann H, de Wit E. Rapid Nipah virus entry into the central nervous system of hamsters via the olfactory route. Sci Rep. 2012;2:736. doi: 10.1038/srep00736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Schrauwen EJ, Herfst S, Leijten LM, van Run P, Bestebroer TM, Linster M, et al. The multibasic cleavage site in H5N1 virus is critical for systemic spread along the olfactory and hematogenous routes in ferrets. J Virol. 2012;86:3795–808. doi: 10.1128/JVI.06828-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Marshall JD, Jr., Quy DV, Gibson FL. Asymptomatic pharyngeal plague infection in Vietnam. Am J Trop Med Hyg. 1967;16:175–7. doi: 10.4269/ajtmh.1967.16.175. [DOI] [PubMed] [Google Scholar]
- 107.Conrad FG, LeCocq FR, Krain R. A recent epidemic of plague in Vietnam. Arch Intern Med. 1968;122:193–8. doi: 10.1001/archinte.1968.00300080001001. [DOI] [PubMed] [Google Scholar]
- 108.Arbaji A, Kharabsheh S, Al-Azab S, Al-Kayed M, Amr ZS, Abu Baker M, Chu MC. A 12-case outbreak of pharyngeal plague following the consumption of camel meat, in north-eastern Jordan. Ann Trop Med Parasitol. 2005;99:789–93. doi: 10.1179/136485905X65161. [DOI] [PubMed] [Google Scholar]
- 109.Bin Saeed AA, Al-Hamdan NA, Fontaine RE. Plague from eating raw camel liver. Emerg Infect Dis. 2005;11:1456–7. doi: 10.3201/eid1109.050081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Leslie T, Whitehouse CA, Yingst S, Baldwin C, Kakar F, Mofleh J, Hami AS, Mustafa L, Omar F, Ayazi E, et al. Outbreak of gastroenteritis caused by Yersinia pestis in Afghanistan. Epidemiol Infect. 2011;139:728–35. doi: 10.1017/S0950268810001792. [DOI] [PubMed] [Google Scholar]
- 111.Sirisanthana T, Navachareon N, Tharavichitkul P, Sirisanthana V, Brown AE. Outbreak of oral-oropharyngeal anthrax: an unusual manifestation of human infection with Bacillus anthracis. Am J Trop Med Hyg. 1984;33:144–50. doi: 10.4269/ajtmh.1984.33.144. [DOI] [PubMed] [Google Scholar]
- 112.Doğanay M, Almaç A, Hanağasi R. Primary throat anthrax. A report of six cases. Scand J Infect Dis. 1986;18:415–9. doi: 10.3109/00365548609032357. [DOI] [PubMed] [Google Scholar]
- 113.Navacharoen N, Sirisanthana T, Navacharoen W, Ruckphaopunt K. Oropharyngeal anthrax. J Laryngol Otol. 1985;99:1293–5. doi: 10.1017/S002221510009856X. [DOI] [PubMed] [Google Scholar]
- 114.Sirisanthana T, Brown AE. Anthrax of the gastrointestinal tract. Emerg Infect Dis. 2002;8:649–51. doi: 10.3201/eid0807.020062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Beatty ME, Ashford DA, Griffin PM, Tauxe RV, Sobel J. Gastrointestinal anthrax: review of the literature. Arch Intern Med. 2003;163:2527–31. doi: 10.1001/archinte.163.20.2527. [DOI] [PubMed] [Google Scholar]
- 116.Babamahmoodi F, Aghabarari F, Arjmand A, Ashrafi GH. Three rare cases of anthrax arising from the same source. J Infect. 2006;53:175–9. doi: 10.1016/j.jinf.2005.12.018. [DOI] [PubMed] [Google Scholar]
- 117.Holty JE, Kim RY, Bravata DM. Anthrax: a systematic review of atypical presentations. Ann Emerg Med. 2006;48:200–11. doi: 10.1016/j.annemergmed.2005.11.035. [DOI] [PubMed] [Google Scholar]
- 118.Ozdemir H, Demirdag K, Ozturk T, Kocakoc E. Anthrax of the gastrointestinal tract and oropharynx: CT findings. Emerg Radiol. 2010;17:161–4. doi: 10.1007/s10140-009-0821-y. [DOI] [PubMed] [Google Scholar]
- 119.Arikan OK, Koç C, Bozdoğan O. Tularemia presenting as tonsillopharyngitis and cervical lymphadenitis: a case report and review of the literature. Eur Arch Otorhinolaryngol. 2003;260:298–300. doi: 10.1007/s00405-002-0565-8. [DOI] [PubMed] [Google Scholar]
- 120.Kandemir B, Erayman I, Bitirgen M, Aribas ET, Guler S. Tularemia presenting with tonsillopharyngitis and cervical lymphadenitis: report of two cases. Scand J Infect Dis. 2007;39:620–2. doi: 10.1080/00365540601105814. [DOI] [PubMed] [Google Scholar]
- 121.Chitadze N, Kuchuloria T, Clark DV, Tsertsvadze E, Chokheli M, Tsertsvadze N, Trapaidze N, Lane A, Bakanidze L, Tsanava S, et al. Water-borne outbreak of oropharyngeal and glandular tularemia in Georgia: investigation and follow-up. Infection. 2009;37:514–21. doi: 10.1007/s15010-009-8193-5. [DOI] [PubMed] [Google Scholar]
- 122.Dlugaiczyk J, Harrer T, Zwerina J, Traxdorf M, Schwarz S, Splettstoesser W, Geissdörfer W, Schoerner C. Oropharyngeal tularemia--a differential diagnosis of tonsillopharyngitis and cervical lymphadenitis. Wien Klin Wochenschr. 2010;122:110–4. doi: 10.1007/s00508-009-1274-8. [DOI] [PubMed] [Google Scholar]
- 123.Uyar M, Cengiz B, Unlü M, Celebi B, Kılıç S, Eryılmaz A. [Evaluation of the oropharyngeal tularemia cases admitted to our hospital from the provinces of Central Anatolia] Mikrobiyol Bul. 2011;45:58–66. [PubMed] [Google Scholar]
- 124.Pongrithsukda V, Simakachorn N, Pimda J. Childhood melioidosis in northeastern Thailand. Southeast Asian J Trop Med Public Health. 1988;19:309–16. [PubMed] [Google Scholar]
- 125.Lumbiganon P, Viengnondha S. Clinical manifestations of melioidosis in children. Pediatr Infect Dis J. 1995;14:136–40. doi: 10.1097/00006454-199502000-00010. [DOI] [PubMed] [Google Scholar]
- 126.Tan NG, Sethi DS. An unusual case of sorethroat: nasopharyngeal melioidosis. Singapore Med J. 1997;38:223–5. [PubMed] [Google Scholar]
- 127.Lim WK, Gurdeep GS, Norain K. Melioidosis of the head and neck. Med J Malaysia. 2001;56:471–7. [PubMed] [Google Scholar]
- 128.How H-S, Ng K-H, Yeo H-B, Tee H-P, Shah A. Pediatric melioidosis in Pahang, Malaysia. J Microbiol Immunol Infect. 2005;38:314–9. [PubMed] [Google Scholar]
- 129.Brent AJ, Matthews PC, Dance DA, Pitt TL, Handy R. Misdiagnosing melioidosis. Emerg Infect Dis. 2007;13:349–51. doi: 10.3201/eid1302.061290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Crowell BC. Pathologic anatomy of bubonic plague. Philipp J Sci. 1915;10B:249–308. [Google Scholar]
- 131.Flexner S. The pathology of bubonic plague. Am J Med Sci. 1901;122:396–416. [Google Scholar]
- 132.Wu L-T, Chun WH, Pollitzer R. Clinical observations upon the second Manchurian plague epidemic, 1920-1921. Nat Med J China. 1922;8:225–55. [Google Scholar]
- 133.Meyer KF. Pneumonic plague. Bacteriol Rev. 1961;25:249–61. doi: 10.1128/br.25.3.249-261.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Krauss F. Anthrax appearing primarily in the nose. Arch Otolaryngol. 1943;37:238–41. doi: 10.1001/archotol.1943.00670030247008. [DOI] [Google Scholar]
- 135.Zachou K, Papamichalis PA, Dalekos GN. Severe pharyngitis in stockbreeders: an unusual presentation of brucellosis. Occup Med (Lond) 2008;58:305–7. doi: 10.1093/occmed/kqn020. [DOI] [PubMed] [Google Scholar]
- 136.Howe C, Miller WR. Human glanders; report of six cases. Ann Intern Med. 1947;26:93–115. doi: 10.7326/0003-4819-26-1-93. [DOI] [PubMed] [Google Scholar]
- 137.Gregory BC, Waag DM. Glanders. In. Lenhart MK, Lounsbury DE, Martin JW, ed(s). Medical Aspects of Biological Warfare. New York. Borden Institute. 2007:121-46. [Google Scholar]
- 138.Pappas G, Giannoutsos C, Christou L, Tsianos E. Coxiella burnetii: an unusual ENT pathogen. Am J Otolaryngol. 2004;25:263–5. doi: 10.1016/j.amjoto.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 139.Steele KE, Reed DS, Glass PJ, Hart MK, Ludwig GV, Pratt WD, et al. Alphavirus encephalitides. In: Lenhart, MK, Lounsbury, DE, Martin, JW, ed(s). Medical Aspects of Biological Warfare. New York. Borden Institute. 2007:241-70. [Google Scholar]
- 140.Lau SK, Kwan S, Lee J, Wei WI. Source of tubercle bacilli in cervical lymph nodes: a prospective study. J Laryngol Otol. 1991;105:558–61. doi: 10.1017/S0022215100116603. [DOI] [PubMed] [Google Scholar]
- 141.Al-Serhani AM. Mycobacterial infection of the head and neck: presentation and diagnosis. Laryngoscope. 2001;111:2012–6. doi: 10.1097/00005537-200111000-00027. [DOI] [PubMed] [Google Scholar]
- 142.Brook I. Current management of upper respiratory tract and head and neck infections. Eur Arch Otorhinolaryngol. 2009;266:315–23. doi: 10.1007/s00405-008-0849-8. [DOI] [PubMed] [Google Scholar]
- 143.Zautner AE. Adenotonsillar disease. Recent Pat Inflamm Allergy Drug Discov. 2012;6:121–9. doi: 10.2174/187221312800166877. [DOI] [PubMed] [Google Scholar]
- 144.Proenca-Modena JL, Pereira Valera FC, Jacob MG, Buzatto GP, Saturno TH, Lopes L, Souza JM, Escremim Paula F, Silva ML, Carenzi LR, et al. High rates of detection of respiratory viruses in tonsillar tissues from children with chronic adenotonsillar disease. PLoS One. 2012;7:e42136. doi: 10.1371/journal.pone.0042136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ludlow M, de Vries RD, Lemon K, McQuaid S, Millar E, van Amerongen G, Yüksel S, Verburgh RJ, Osterhaus AD, de Swart RL, et al. Infection of lymphoid tissues in the macaque upper respiratory tract contributes to the emergence of transmissible measles virus. J Gen Virol. 2013;94:1933–44. doi: 10.1099/vir.0.054650-0. [DOI] [PubMed] [Google Scholar]
- 146.Munck K, Mandpe AH. Mycobacterial infections of the head and neck. Otolaryngol Clin North Am. 2003;36:569–76. doi: 10.1016/S0030-6665(03)00032-X. [DOI] [PubMed] [Google Scholar]
- 147.Dutz W, Saidi F, Kohout E. Gastric anthrax with massive ascites. Gut. 1970;11:352–4. doi: 10.1136/gut.11.4.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mayo L, Dionne-Odom J, Talbot EA, Adamski C, Bean C, Daly ER, et al. Centers for Disease Control and Prevention (CDC) Gastrointestinal anthrax after an animal-hide drumming event - New Hampshire and Massachusetts, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:872–7. [PubMed] [Google Scholar]
- 149.Halperin SA, Gast T, Ferrieri P. Oculoglandular syndrome caused by Francisella tularensis. Clin Pediatr (Phila) 1985;24:520–2. doi: 10.1177/000992288502400909. [DOI] [PubMed] [Google Scholar]
- 150.Li B, Yang R. Interaction between Yersinia pestis and the host immune system. Infect Immun. 2008;76:1804–11. doi: 10.1128/IAI.01517-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Brandtzaeg P. Immune functions of nasopharyngeal lymphoid tissue. Adv Otorhinolaryngol. 2011;72:20–4. doi: 10.1159/000324588. [DOI] [PubMed] [Google Scholar]
- 152.Bosch AA, Biesbroek G, Trzcinski K, Sanders EAM, Bogaert D. Viral and bacterial interactions in the upper respiratory tract. PLoS Pathog. 2013;9:e1003057. doi: 10.1371/journal.ppat.1003057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mina MJ, Klugman KP. Pathogen replication, host inflammation, and disease in the upper respiratory tract. Infect Immun. 2013;81:625–8. doi: 10.1128/IAI.01460-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kalinke U, Bechmann I, Detje CN. Host strategies against virus entry via the olfactory system. Virulence. 2011;2:367–70. doi: 10.4161/viru.2.4.16138. [DOI] [PubMed] [Google Scholar]
- 155.Panni P, Ferguson IA, Beacham I, Mackay-Sim A, Ekberg JAK, St John JA. Phagocytosis of bacteria by olfactory ensheathing cells and Schwann cells. Neurosci Lett. 2013;539:65–70. doi: 10.1016/j.neulet.2013.01.052. [DOI] [PubMed] [Google Scholar]