Abstract
In this article we give a case report on a PTC patient with pancreatic metastasis. In this case, the patient was admitted to our hospital for recurrence of PTC and occupying pancreatic lesions. We considered that the pancreatic neoplasm may be pancreatic metastasis of PTC but there is no previous experience about therapeutic approaches to this type of metastases. After some discussion the distant metastasis within the pancreas was successfully removed by a laparotomy and postoperative histology confirmed the diagnosis. After that surgery, the patient recovered well and then received total thyroidectomy and cervical lymph node dissection for recurrent thyroid cancer. After recovery he was discharged from hospital without further treatment. Eventually, he died of acute myocardial infarction in January 2010. To conclude, it is widely believed that the surgical operation should be chosen more positively in the management of those patients without multiple organ metastases. Thus on one hand it can serve to make a definite diagnosis, and on the other hand it can help the body get rid of the bulk of the tumor burden to prolong survival time of the patients.
Keywords: Papillary thyroid carcinoma, pancreatic metastasis
Introduction
Papillary thyroid carcinomas (PTC) are the most common endocrine cancer. Around the world, they account for 60% of all thyroid cancer cases in adults and nearly 100% in children. In addition, they are more common in women between 30 to 45 years old [1]. The first manifestation of PTC is usually a thyroid nodule or a neck mass and the main route of metastasis is locoregional spread to the lymph nodes of the neck while distant metastases are rare. Age, tumor size, and certain histopathological types are associated with a high risk for recurrence and mortality, but distant metastases are probably the most important prognostic factor and usually occur in advanced stage of the disease, especially in lungs, bones, and thoracic lymph nodes [2]. Metastases of PTC to pancreas are extremely rare. Up to now, only 8 cases of metastatic PTC to the pancreas have been previously published [3]. The presence of pancreatic metastases is usually accompanied by widespread metastases to other organs, but in this report, we describe a patient with PTC and isolated pancreatic metastasis.
Patient
A 66-year-old male patient was admitted to our hospital in August 2009 because of multiple masses in his neck for 4 months. He had a PTC history and had received the operation of total removal of the left-sided thyroid with neoplasm in 1998 at the local hospital. From then on, three subsequent operations had been performed consecutively for the recurrence of PTC in the next 10 years. Physical examination on admission revealed several palpable masses on the right side of the neck that were smooth, not fixed, without tenderness, and the diameters varied from 0.5 cm to 4.0 cm in size. Furthermore, we found a neoplasm in the middle left abdomen which is smooth and fixed. The ultrasonography (US) and computed tomographic scan (CT) of the neck revealed a low hypoechoic nodule sized 2.1 cm × 0.9 cm in right thyroid and multiple lymph nodes, both of which are with rich blood flow signal near the right common carotid artery (Figure 1). Surprisingly, an enhanced CT scan showed a mass (6.2 cm × 5.8 cm) affecting the body and tail of the pancreas with clear border (Figure 2). Following that, a systemic PET-CT was performed and did not show other abnormalities. In August 2009, a distal pancreatectomy, splenectomy, and resection of part of the posterior gastric wall were performed. After the operation, the pathology revealed that the tumor resected from pancreas was a metastasis of papillary thyroid carcinoma. The patient had an uneventful recovery, and then received total thyroidectomy and cervical lymph node dissection for recurrent thyroid cancer. The specimen from pancreatic metastasis (Figure 3A) were histologically similar to the primary thyroid tumor (Figure 3B, the dashed arrow indicates the papillary thyroid carcinoma and the arrow indicates the normal pancreas tissue). Immunohistochemical studies showed positive Ki67 (Figure 3C, +12%), TG (Figure 3D), TTF-1 (Figure 3E), and CK19 (Figure 3F) staining in metastatic tumor cells, with negative staining of CgA(-), Syn(-), CEA(-) and CD56(-). Of them, the positive results of Ki67, TG and TTF-1 had special significance to the diagnosis of pancreatic metastasis of PTC. After surgery, the patient recovered well and was discharged from hospital without further treatment. Eventually, he died of acute myocardial infarction in January 2010.
Figure 1.
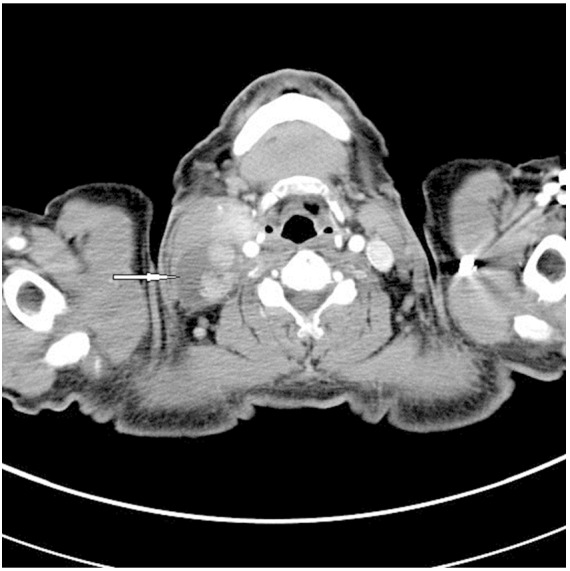
CT manifestation of PTC (white arrow).
Figure 2.
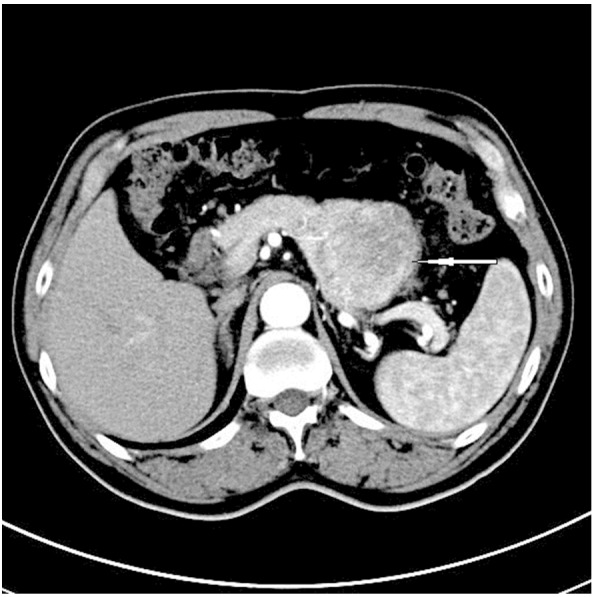
CT manifestation of solitary mass affecting the body and tail of the pancreas (white arrow).
Figure 3.
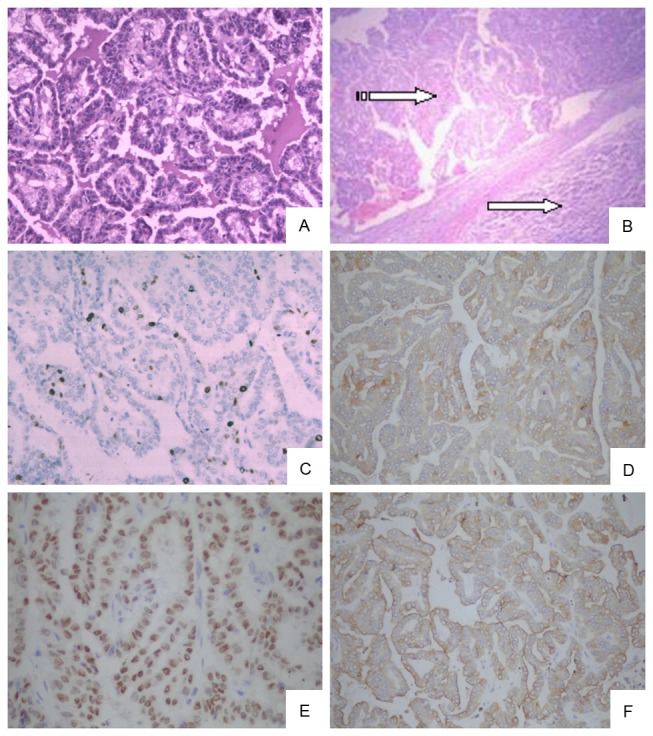
HE staining of PTC (A); pancreatic metastasis (B) (the dashed arrow indicates the papillary thyroid carcinoma and the arrow indicates the normal pancreas tissue); Immunohistochemical staining of pancreatic metastasis (C-Ki67, D-TG, E-TTF-1 and F-ck19).
Discussion
Pancreatic metastatic tumors (PM) usually occur at multiple sites and isolated pancreatic metastases are very rare. Only 3% of the patients with multiple metastases would have pancreatic metastases and metastatic carcinomas accounted for just 2% of the pancreatic tumors [4]. Most PM patients have similar clinical manifestations and radiographic signs to pancreas primary tumors, thus the preoperative misdiagnosis rate could reach 30%. The primary tumors are commonly from renal cancer, bronchiolar carcinoma, colorectal cancer, breast cancer, gastric cancer, and endometrial cancer [5]. It takes a long time generally for 36 to 90 months when primary tumors spread to the pancreas. PM can be limited or diffuse lesions and Minni concludes that 64.7% of PM were single lumps and 19.1% were multiple nodules, while 16.2% were diffuse lesions [6,7].
PTC is considered as a low-grade malignant tumor whose clinical symptoms are due to the presence of a thyroid nodule or the metastases in the cervical lymph nodes. Distant metastases are infrequent and usually occur in lungs, bones, and thoracic lymph nodes [2]. According to the previous reports, pancreatic metastatic tumor due to PTC is quite rare and it has been rarely reported that a single pancreatic metastatic lump was from PTC without any other organ metastasis [8]. It is very difficult to make differences between the primary and the secondary pancreatic tumor. In the case of this patient, we once considered for the patient with primary thyroid cancer and primary pancreatic tumor at the same time before the operation. According to the literature, CT examinations have many advantages in favor of the diagnosis of PTC such as 1) the pancreatic metastasis is often multiple; 2) the metastatic tumor is always a nodule with low density, especially by enhanced scan; 3) the invasive pancreatic vessels are quite rare in the pancreatic metastases. Neither are the bile duct and pancreatic duct dilation; 4) the pancreatic metastasis is usually accompanied by liver or splenic metastases [9]. PTC with pancreatic metastasis hints the advanced stage of disease and the prognosis is always very poor. According to a report by Hirota et al, the moderate living time is no more than 8.7 months for the patients with pancreatic metastases [10]. However, when the metastatic pancreatic nodule is the unique metastatic carcinoma, the resection of the nodule is able to increase the five-year survival rate to 31% [11]. So the surgical operation should be chosen more positively in the management of this kind of patients without multiple organs metastases. Thus on one hand it can make a definite diagnosis, and on the other hand it can help the body get rid of the bulk of the tumor burden for prolonging survival time of the patient [12].
Because the incidence of complications and mortality is higher after pancreatic resection, whether the PM surgery is beneficial to the prognosis of patients is still disputed, therefore, the proposed PM resection patients should receive careful evaluation. Preoperative consultation for multidisciplinary cooperation includes oncology, pancreas surgery, imaging and intervention, etc. Evidence-based medical research according to the results of resection of the PM reveals that the surgeries should be performed in the hospital which has perfected devices and implementation of mature technology [13]. Patient selection criteria are as follows: 1) the type of primary tumor has good prognosis; 2) the primary tumor is controllable in operation; 3) isolation of metastases; and 4) patients can tolerate pancreatectomy. Only when the primary tumor is under control was pancreatic metastases resection meaningful [4]. Whether pancreatic metastases resection and primary tumor resection can be taken in the same period remains questionable. Although in some cases it can be considered simultaneously, but to remove the primary tumor and metastatic tumor of pancreas surgery will at the same time double the risk. Staging surgery and perioperative with systemic comprehensive treatment in PM treatment is a better choice. Several studies have shown that pancreatic metastases resection shall adopt regular pancreatectomy while partial resection is meaningless.
Disclosure of conflict of interest
None.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics. CA Cancer J Clin. 2011 Mar-Apr;61:133–134. [Google Scholar]
- 2.Sugitani I, Fujimoto Y, Yamamoto N. Papillary thyroid carcinoma with distant metastases: survival predictors and the importance of local control. Surgery. 2008 Jan;143:35–42. doi: 10.1016/j.surg.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 3.Alzahrani AS, AlQaraawi A, Al Sohaibani F, Almanea H, Abalkhail H. Pancreatic metastasis arising from a BRAF(V600E)-positive papillary thyroid cancer: the role of endoscopic ultrasound-guided biopsy and response to sorafenib therapy. Thyroid. 2012 May;22:536–541. doi: 10.1089/thy.2011.0247. [DOI] [PubMed] [Google Scholar]
- 4.Reddy S, Wolfgang CL. The role of surgery in the management of isolated metastases to the pancreas. Lancet Oncol. 2009 Mar;10:287–293. doi: 10.1016/S1470-2045(09)70065-8. [DOI] [PubMed] [Google Scholar]
- 5.Adsay NV, Andea A, Basturk O, Kilinc N, Nassar H, Cheng JD. Secondary tumors of the pancreas: an analysis of a surgical and autopsy database and review of the literature. Virchows Arch. 2004 Jun;444:527–535. doi: 10.1007/s00428-004-0987-3. [DOI] [PubMed] [Google Scholar]
- 6.Crippa S, Angelini C, Mussi C, Bonardi C, Romano F, Sartori P, Uggeri F, Bovo G. Surgical treatment of metastatic tumors to the pancreas: a single center experience and review of the literature. World J Surg. 2006 Aug;30:1536–1542. doi: 10.1007/s00268-005-0464-4. [DOI] [PubMed] [Google Scholar]
- 7.Minni F, Casadei R, Perenze B, Greco VM, Marrano N, Margiotta A, Marrano D. Pancreatic metastases: observations of three cases and review of the literature. Pancreatology. 2004;4:509–520. doi: 10.1159/000080248. [DOI] [PubMed] [Google Scholar]
- 8.Al-Brahim N, Asa SL. Papillary thyroid carcinoma-an overview. Arch Pathol Lab Med. 2006 Jul;130:1057–1062. doi: 10.5858/2006-130-1057-PTCAO. [DOI] [PubMed] [Google Scholar]
- 9.Borschitz T, Eichhorn W, Fottner C, Hansen T, Schad A, Schadmand-Fischer S, Weber MM, Schreckenberger M, Lang H, Musholt TJ. Diagnosis and treatment of pancreatic metastases of a papillary thyroid carcinoma. Thyroid. 2010 Jan;20:93–98. doi: 10.1089/thy.2009.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hirota T, Tomida T, Iwasa M, Takahashi Km Kaneda M, Tamaki H. Solitary pancreatic metastasis occurring eight years after nephrectomy for renal cell carcinoma. A case report and surgical review. Int J Pancreatol. 1996 Apr;19:145–153. doi: 10.1007/BF02805229. [DOI] [PubMed] [Google Scholar]
- 11.Soyluk O, Selcukbiricik F, Erbil Y, Bozbora A, Kapran Y, Ozbey N. Prognostic factors in patients with papillary thyroid carcinoma. J Endocrinol Invest. 2008 Nov;31:1032–1037. doi: 10.1007/BF03345644. [DOI] [PubMed] [Google Scholar]
- 12.Meyer A, Behrend M. Is pancreatic resection justified for metastasis of papillary thyroid cancer? Anticancer Res. 2006 May-Jun;26:2269–2273. [PubMed] [Google Scholar]
- 13.McPhee JT, Hill JS, Whalen G, Zayaruzny M, Litwin DE, Sullivan ME, Anderson FA, Tseng JF. Perioperative mortality for pancreatectomy: a national perspective. Ann Surg. 2007 Aug;246:246–253. doi: 10.1097/01.sla.0000259993.17350.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]


