Abstract
Background
Hospital readmission rates within 30 days following acute myocardial infarction (AMI) are a national performance metric. Prior data suggest that early physician follow-up after heart failure hospitalizations can reduce readmissions; whether these results can be extended to AMI is unclear.
Methods and Results
We analyzed data from the CRUSADE Registry linked with Medicare claims from 2003–2006 for 25,872 non–ST-segment elevation myocardial infarction (NSTEMI) patients ≥65 years old discharged home from 228 hospitals with >25 patients and full revascularization capabilities. After adjusting for patient, treatment, and hospital characteristics, we examined the relationship between hospital-level physician follow-up within 7 days of discharge and 30-day all-cause readmission using logistic regression. The median hospital-level percentage of patients receiving early physician follow-up was 23.3% (IQR 17.1%–29.1%). Among 24,165 patients with Medicare fee-for-service eligibility 30 days after discharge, 18.5% of patients were readmitted within 30 days of index hospitalization. Unadjusted and adjusted rates of 30-day readmission did not differ among quartiles of hospital-level early physician follow-up. Similarly, each 5% increase in hospital early follow-up was associated with an insignificant change in risk for readmission (adjusted OR 0.99; 95% CI 0.97, 1.02; p=0.60). Sensitivity analyses extended these null findings to 30-day cardiovascular readmissions, high-risk subgroups, and early cardiology follow-up.
Conclusions
While rates of early physician follow-up after AMI varied among U.S. hospitals, hospitals with higher early follow-up rates did not have lower 30-day readmission rates. Targeting strategies other than early physician follow-up may be necessary to reduce readmission rates in this population.
Keywords: early physician follow-up, acute myocardial infarction, non–ST-segment elevation myocardial infarction
Acute myocardial infarction (AMI) is a common cause of hospital admissions in the United States (U.S.). In 2008, AMI represented the sixth most expensive condition billed to the Centers for Medicare & Medicaid Services (CMS).1 Recent data estimate that the median national 30-day risk-standardized readmission rate for AMI is 19.9%.2 In an effort to improve hospital-based outcomes through quality improvement, CMS began publicly reporting 30-day risk-standardized readmission rates for patients admitted with AMI, heart failure, and pneumonia in 2009. Subsequent passage of the Patient Protection and Affordable Care Act in 2010 gave CMS the ability to reduce reimbursement to hospitals with excessive 30-day readmission rates for these conditions.3
While there are limited proven means of reducing readmissions following AMI, considerable focus has been placed on the topic of care transitions. Outpatient physician follow-up within 7 days of discharge has been associated with reduced 30-day readmissions after heart failure hospitalization.4 Whether early physician follow-up can reduce readmissions following non–ST-segment myocardial infarction (NSTEMI) is unknown. Therefore, we sought to: (1) characterize hospital variation in early physician follow-up after admission for NSTEMI; and (2) examine the relationship between early physician follow-up rates and patient outcomes using data from the Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines (CRUSADE) Registry linked with longitudinal Medicare data.
Methods
Setting
Clinical data were from CRUSADE, a national initiative aimed at improving adherence to guideline-based therapies for high-risk NSTEMI patients. Complete CRUSADE details have been previously published.5,6 Briefly, CRUSADE enrolled patients from 2001–2006 with high-risk acute coronary syndrome (ACS) features and ischemic rest symptoms within 24 hours before presentation. Patient characteristics, in-hospital treatments and outcomes, and discharge therapies were collected in a de-identified fashion. Longitudinal readmission and mortality outcomes were identified from administrative CMS data using inpatient and denominator files, respectively. Outpatient provider claims for services covered under Medicare Part B were examined using carrier files and Healthcare Common Procedure Coding System (HCPCS) codes. This study was approved by the Duke University Health System Institutional Review Board.
Patients
We included CRUSADE patients ≥65 years old with linked and matching CMS data from 2003–2006; this timeframe was chosen due to the use of a revised case report form that collected more clinical variables. The process for linking patient data using probabilistic matching based on indirect identifiers (e.g., age, date of service, and gender) has been previously described.7 Through this methodology, 72.5% of CRUSADE patients ≥65 years old were successfully linked with CMS records. We excluded patients presenting with ST-segment-elevation myocardial infarction (STEMI)—a population that was not enrolled consistently throughout CRUSADE and that makes up a small minority of the patient population; patients for whom data was collected using the less comprehensive first version of the case report form; patients who died in-hospital; and patients with non-matching CRUSADE and CMS records. Patients transferred to acute care facilities or discharged to a skilled nursing facility or hospice were also excluded, as were patients with first physician follow-up the same day as discharge. We included only the first admission for patients with multiple hospitalizations captured in CRUSADE, and we excluded hospitals without full-revascularization capabilities and low-volume centers (<25 patients).
Definitions and Outcomes
Early follow-up was defined as any physician outpatient evaluation and management visit (HCPCS codes 992.xx–994.xx) within 7 days after discharge from the index hospitalization. Emergency department visits were not considered early follow-up. Patients who died or were readmitted prior to receiving physician follow-up within 7 days after discharge were classified as having missing early follow-up status and were excluded when determining hospital-level early physician follow-up. Transfers to or from another hospital and rehabilitation admissions were not counted as readmissions. Our primary outcome was all-cause readmission within 30 days after discharge from index hospitalization. Secondary outcomes included 30-day all-cause mortality and the composite endpoint of readmission and mortality.
Statistical Analysis
Rates of early follow-up were calculated for patients without missing follow-up status and reported at the hospital-level for the overall study population, as well as by quartiles of hospital early follow-up. We examined baseline patient and in-hospital variables according to quartile of hospital-level early follow-up. Comparisons across quartiles were made for non-missing values (~1% missing). Categorical variables were summarized as frequencies and percentages, and continuous variables were presented as medians with interquartile ranges. Pearson chi-square and Kruskal-Wallis tests were used for comparisons among categorical and continuous variables, respectively. A significance level of 0.05 and two-sided tests were used for all analyses. Analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC).
We reported the unadjusted cumulative incidence for 30-day readmission, mortality, and composite readmission/mortality. Evaluations of readmission outcomes excluded patients ineligible for Medicare fee-for-service within 30 days after discharge from index hospitalization (n=1707), as readmissions for these patients could not be identified. In general, sicker patients with greater comorbidities are seen in follow-up sooner post-discharge than less sick patients, but are also at higher risk of readmission. Consequently, severity of illness may confound evaluations of physician follow-up and outcomes. This may be especially relevant for analyses conducted at the patient-level, as there may be dramatic differences in illness severity when comparing individual patients with one another. However, these differences may be reduced when making aggregate comparisons at the hospital-level and across multiple sites, as each hospital has a distribution of disease severity. Therefore, to reduce confounding, we chose to perform our analyses at the hospital-level and also adjusted for patient-level characteristics. We used logistic generalized estimating equations with exchangeable working correlation matrix to examine relationships between hospital-level rates of early physician follow-up and outcomes. This strategy has been used before to demonstrate the association of early physician follow-up and risk for readmission following heart failure hospitalization.4
When modeling readmission outcomes, missing continuous covariates were imputed to the median non-missing value, and missing categorical covariates were imputed to the value of the most frequent group. Rates of missingness were ≤2.2% for all variables, with the exception of hematocrit, creatinine, and troponin, which ranged from 2.4%–4.1%. Non-linear continuous covariates were fitted using splines. Hospital early follow-up was examined as a categorical variable for pairwise comparisons between the 2nd–4th quartiles and the 1st quartile of hospital follow-up. Hospital-level early follow-up was also considered a continuous variable. Odds ratios (ORs) for hospital early follow-up were reported per 5% increase in physician follow-up. Three adjustment models were constructed based on: (1) patient characteristics; (2) the addition of hospital features to the first model; and (3) the addition of treatment features to the second model. Covariates for adjustment in Model 1 included demographic variables (age, sex, race, weight); medical history (current/recent smoker, hypertension, diabetes, dyslipidemia, peripheral artery disease, prior percutaneous coronary intervention [PCI], prior coronary artery bypass graft [CABG] surgery, family history of coronary artery disease; prior myocardial infarction [MI], congestive heart failure [CHF], and stroke); and in-hospital characteristics (transfer-in status, presentation heart rate, systolic blood pressure, and electrocardiogram findings, signs of CHF, baseline hematocrit, troponin, and creatinine, and length of stay [LOS]). Additional adjustment covariates for Model 2 included hospital region, teaching status, bed size, and percentage of black patients treated. Variables added into the 3rd model included cardiac catheterization, PCI, CABG, discharge medications (aspirin, beta blocker, statin, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, and clopidogrel), smoking-cessation counseling, cardiac rehabilitation referral, and diet modification counseling.
We performed sensitivity analyses examining 30-day cardiovascular readmissions, defined by Diagnosis Related Group codes (see Supplement Table 1). Additionally, we examined all-cause and cardiovascular 30-day readmissions among high-risk AMI patients, defined as patients with ≥10% predicted mortality calculated using the Global Registry of Acute Coronary Events (GRACE) 6-month post-discharge risk score.8 Predicted 6-month mortality was calculated using age, history of MI, history of CHF, pulse, systolic blood pressure, creatinine, cardiac enzymes, ST-segment depression, and in-hospital PCI. Patients missing any of these variables were excluded from these analyses (n=1256). Evaluations of early cardiology follow-up used physician specialty codes from outpatient Medicare Part B provider claims to classify cardiologists. Unplanned all-cause readmissions were identified by excluding probable staged revascularization procedures using previously described methodology whereby PCI or CABG procedures associated with primary diagnosis codes unlikely to represent elective admissions were considered unplanned readmissions.9
Results
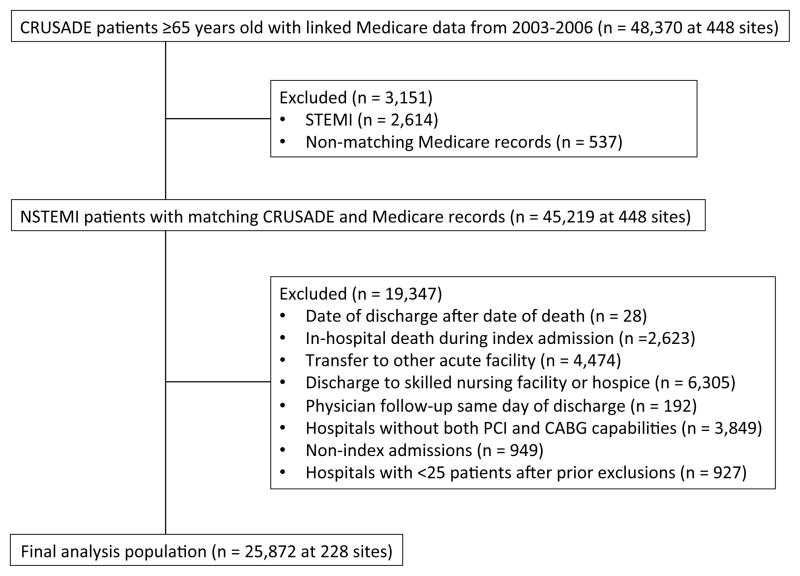
Overall, a total of 48,370 CRUSADE patients ≥65 years old from 448 hospitals had linked longitudinal CMS data from 2003–2006. We excluded STEMI patients (n=2,614) and patients who died in-hospital (n=2,623), were transferred to acute care facilities (n=4,474), or were discharged to a skilled nursing facility or hospice (n=6,305). After exclusions (Figure 1), the final analysis population included 25,872 patients from 228 sites.
Figure 1.
Flow Diagram of Patient Selection. This figure displays inclusions and exclusions and the final study cohort. CABG indicates coronary artery bypass graft; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-segment-elevation myocardial infarction.
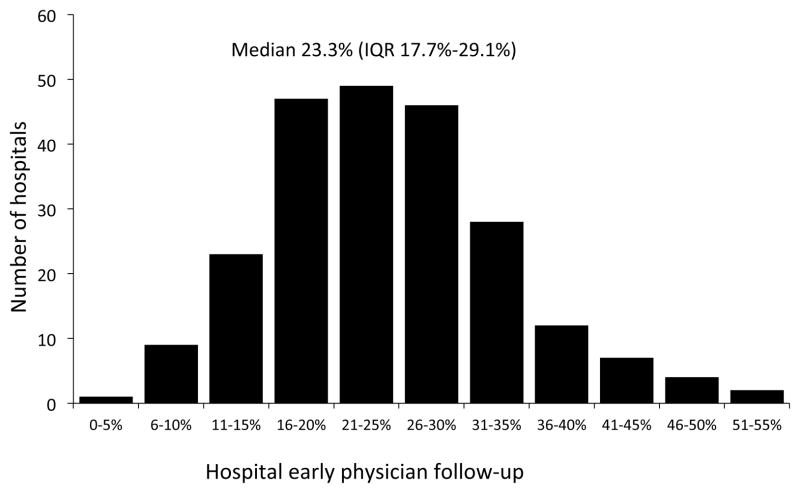
Among 228 centers, the median hospital-level percentage of patients receiving early physician follow-up was 23.3%; however, there was wide hospital variation in early follow-up ranging from 2.6% to 51.6% (interquartile range [IQR] 17.7%–29.1%; Figure 2). In the overall study population, the median age was 76 years, 44.2% (n=11,438) were female, and 7.6% (n=1953) were black. We examined patient and hospital characteristics according to quartile of hospital-level early follow-up (Table 1). Compared with hospitals in the lowest two quartiles of early follow-up (<17.8% and 17.8%–23.2%), those with most frequent follow-up (23.3%–28.9% and >28.9%) treated a higher proportion of black patients and patients with more comorbidities. Hospitals with higher follow-up rates were also less likely to use PCI and CABG than sites in the lower three quartiles and had slightly longer median LOS (Table 2).
Figure 2.
Variation in Hospital-level Early Physician Follow-up. Shown here is the distribution of hospital-level early physician follow-up. IQR indicates interquartile range.
Table 1.
Patient and Treatment Characteristics According to Quartile of Hospital-level Early Follow-up
| Hospital Quartile 1 (n=6129) | Hospital Quartile 2 (n=6759) | Hospital Quartile 3 (n=7626) | Hospital Quartile 4 (n=5358) | p-value | |
|---|---|---|---|---|---|
| Hospital early follow-up (%) | <17.8 | 17.8–23.2 | 23.3–28.9 | >28.9 | |
| Demographics | |||||
| Age, median (IQR), y | 76.0 (70.0, 81.0) | 76.0 (70.0, 82.0) | 76.0 (70.0, 82.0) | 77.0 (71.0, 82.0) | <0.0001 |
| Weight, median (IQR), kg | 78.2 (66.7, 90.3) | 77.6 (66.2, 90.0) | 77.1 (66.2, 90.0) | 77.1 (65.8, 89.0) | 0.01 |
| Female sex (%) | 43.7 | 44.3 | 44.8 | 43.9 | 0.62 |
| Race (%) | <0.0001 | ||||
| White | 89.2 | 87.8 | 82.5 | 83.6 | |
| Black | 6.1 | 7.3 | 8.5 | 8.3 | |
| Asian | 0.4 | 0.2 | 1.3 | 0.8 | |
| Hispanic | 2.4 | 1.5 | 4.1 | 2.9 | |
| Other | 1.0 | 0.9 | 2.3 | 2.7 | |
| Medical history (%) | |||||
| Hypertension | 75.7 | 76.3 | 77.9 | 76.6 | 0.01 |
| Diabetes mellitus | 33.4 | 33.2 | 34.5 | 35.5 | 0.01 |
| Peripheral arterial disease | 13.9 | 14.2 | 14.8 | 12.7 | 0.01 |
| Current/recent smoking | 14.0 | 13.8 | 13.2 | 13.1 | 0.32 |
| Family history of CAD | 34.6 | 28.3 | 21.7 | 29.6 | <0.0001 |
| Prior MI | 28.4 | 30.0 | 31.8 | 31.6 | <0.0001 |
| Prior PCI | 23.9 | 23.5 | 22.9 | 22.6 | 0.36 |
| Prior CABG | 25.2 | 26.3 | 24.5 | 24.6 | 0.07 |
| Prior heart failure | 17.8 | 18.0 | 19.9 | 20.3 | <0.0001 |
| Chronic renal insufficiency | 14.0 | 14.9 | 15.6 | 16.2 | 0.004 |
| Presentation features | |||||
| Signs of heart failure (%) | 25.8 | 24.3 | 25.3 | 28.0 | <0.0001 |
| ECG findings (%) | <0.001 | ||||
| ST-segment depression | 25.6 | 28.7 | 28.1 | 27.6 | |
| Transient ST-segment elevation | 3.0 | 3.1 | 3.3 | 3.9 | |
| Neither | 70.5 | 67.5 | 67.6 | 67.5 | |
| Both | 0.9 | 0.7 | 1.0 | 0.9 | |
| Hematocrit, median (IQR), % | 39.6 (35.8, 43.2) | 39.8 (36.0, 43.2) | 39.5 (35.6, 43.0) | 39.3 (35.5, 42.8) | <0.001 |
| Transfer-in status (%) | 31.0 | 31.1 | 24.1 | 15.3 | <0.0001 |
| In-hospital treatment (%) | |||||
| Cardiac catheterization | 78.0 | 77.6 | 75.0 | 73.8 | <0.0001 |
| PCI | 46.1 | 45.2 | 44 | 43.6 | 0.03 |
| CABG | 12.1 | 10.8 | 10 | 9.8 | 0.0001 |
| LVEF assessment | 86.4 | 86.8 | 85.8 | 83.4 | <0.0001 |
| Discharge treatment (%) | |||||
| Medications prescribed | |||||
| Aspirin | 94.8 | 95.5 | 95.5 | 94.3 | 0.001 |
| Clopidogrel | 72.4 | 74.5 | 71.3 | 73.8 | <0.0001 |
| Beta-blocker | 91.7 | 93.6 | 92.7 | 91.9 | 0.0001 |
| Statin | 78.6 | 79.4 | 81.5 | 78.4 | <0.0001 |
| ACEI/ARB | 67.5 | 66.3 | 66.2 | 64.9 | 0.08 |
| Cardiac rehabilitation referral | 67.7 | 66.0 | 62.7 | 61.4 | <0.0001 |
| Smoking cessation counseling | 79.4 | 79.9 | 80.0 | 80.7 | 0.92 |
| Diet modification counseling | 86.9 | 81.5 | 80.6 | 85.9 | <0.0001 |
ACEI indicates angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CABG, coronary artery bypass graft surgery; CAD, coronary artery disease; ECG, electrocardiogram; IQR, interquartile range; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention
Table 2.
Hospital Characteristics According to Hospital-level Early Follow-up
| Hospital Quartile 1 (n=57) | Hospital Quartile 2 (n=57) | Hospital Quartile 3 (n=57) | Hospital Quartile 4 (n=57) | p-value | |
|---|---|---|---|---|---|
| Hospital characteristics | |||||
| Region | 0.10 | ||||
| West | 1.8 | 7.0 | 19.3 | 15.8 | |
| Northeast | 22.8 | 28.1 | 17.5 | 17.5 | |
| Midwest | 36.8 | 33.3 | 28.1 | 38.6 | |
| South | 36.8 | 31.6 | 35.1 | 24.6 | |
| Teaching hospital (%) | 22.8 | 38.6 | 26.3 | 31.6 | 0.28 |
| Total hospital beds, median (IQR) | 374 (274, 500) | 431 (299, 539) | 352 (284, 485) | 391 (250, 610) | 0.87 |
| Length of stay, median (IQR), days | 5.3 (4.8, 6.2) | 5.3 (4.8, 5.9) | 5.4 (4.9, 6.1) | 5.5 (5.0, 6.4) | 0.69 |
All abbreviations can be found in Table 1.
Early Physician Follow-up and 30-day Outcomes
Overall, 18.51% (n=4474) of 24,165 patients with Medicare fee-for-service insurance for 30 days post-discharge were readmitted. Table 3 shows unadjusted rates of 30-day outcomes according to quartiles of hospital-level early follow-up. There was no significant difference in the unadjusted rates of readmission, mortality, or the composite endpoint of mortality or readmission across quartiles.
Table 3.
Rates of 30-day Readmission, Mortality, and Readmission or Mortality According to Hospital-level Early Physician Follow-up
| Hospital Quartile 1 <17.8% (n=6129) |
Hospital Quartile 2 17.8%–23.2% (n=6759) |
Hospital Quartile 3 23.3%–28.9% (n=7626) |
Hospital Quartile 4 >28.9% (n=5358) |
p-value | |
|---|---|---|---|---|---|
| Readmission, % | 18.7 | 17.9 | 18.1 | 19.5 | 0.13 |
| Mortality, % | 2.9 | 2.4 | 2.4 | 2.5 | 0.19 |
| Readmission or mortality, % | 19.2 | 18.3 | 18.6 | 20.0 | 0.12 |
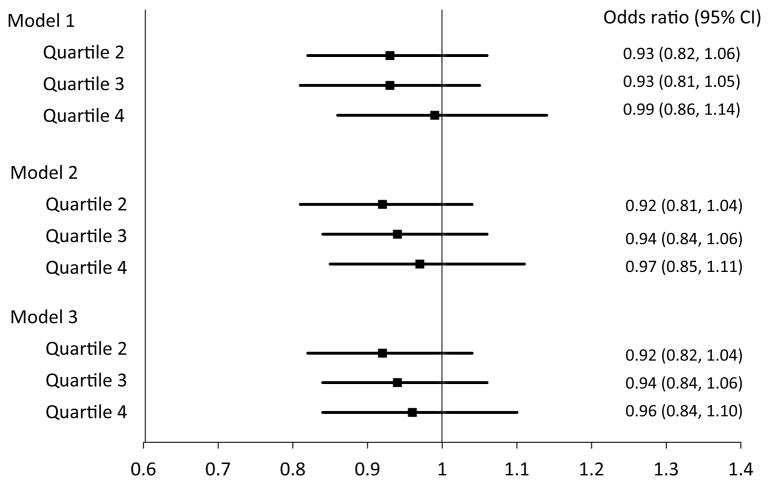
After adjustment for patient demographic and clinical characteristics, no association between hospital-level early follow-up and 30-day readmission was found among pairwise comparisons of the 2nd, 3rd, and 4th quartiles versus the 1st quartile of hospital-level early follow-up (Figure 3) or through continuous measurement (adjusted OR per 5% follow-up increase 0.99; 95% confidence interval [CI] 0.97, 1.02; p=0.60). Neither the addition of hospital features (adjusted OR per 5% increase early follow-up 0.99; 95% CI 0.97, 1.02; p=0.63) nor further adjustment for treatment features (adjusted OR per 5% increase early follow-up 0.99; 95% CI 0.97, 1.02; p=0.57) impacted these results.
Figure 3.
Adjusted 30-day All-cause Readmission by Hospital-level Early Physician Follow-up. Adjusted odds ratios and 95% confidence intervals are shown for the 2nd through 4th quartiles of hospital-level early physician follow-up using the 1st quartile as the reference group. Model 1 = adjustment for patient demographic and clinical characteristics; Model 2 = covariates in model 1 + hospital features; Model 3 = covariates in model 2 + treatment features. P-values for all odds ratios were >0.05. CI indicates confidence intervals
Sensitivity Analyses
We performed several sensitivity analyses to evaluate the robustness of our primary results (Supplement Figure 1). First, we assessed whether early physician follow-up may have affected the composite endpoint of 30-day all-cause readmission or mortality, but found, similar to our overall results, no association between the two (OR per 5% increase early follow-up 0.99; 95% CI 0.97, 1.02; p=0.51 using the 3rd adjustment model). Second, we examined whether early follow-up was associated with cardiovascular-specific causes of readmission. Overall, 13.2% (n=3,024) of patients were readmitted for a cardiovascular cause within 30 days of discharge. Again, there was no association between hospital rates of early physician follow-up and 30-day cardiovascular readmissions (OR per 5% increase 0.99; 95% CI 0.96, 1.02; p=0.48 using the 3rd adjustment model).
Third, we assessed whether early follow-up was more impactful among higher risk patients. High-risk was defined as a GRACE 6-month post-discharge mortality of ≥10% (present in 33.52% [n=7679] of eligible patients). Among high-risk patients, 26.0% were seen by a physician within 7 days of discharge. While those with high-risk features were more likely to be readmitted within 30 days than low-risk patients (23.4% vs. 16.0%; p<0.0001), adjusted analyses showed no association between early physician follow-up and 30-day all-cause readmission in the high-risk patient subgroup (OR per 5% increase early follow-up 0.99; 95% CI 0.96, 1.03; p=0.60 using the 3rd model) or 30-day cardiovascular readmission (OR per 5% increase early follow-up 0.99; 95% CI 0.95, 1.03; p=0.58 using the 3rd model).
Fourth, we evaluated whether physician specialty might influence the association between cardiology specialty follow-up and readmission. Overall, the median hospital-level early cardiology follow-up rate was low at 5.6% (IQR 2.7%, 9.2%). We demonstrated no association between hospital-level early cardiology follow-up and 30-day all-cause readmission (OR per 5% increase early follow-up 0.99; 95% CI 0.95, 1.03; p=0.68 using the 3rd adjustment model) or 30-day cardiovascular readmission (OR per 5% increase early follow-up 0.98; 95% CI 0.94, 1.03; p=0.43 using the 3rd adjustment model).
We also performed additional analyses to assess for potential relationships between early follow-up and readmission in our cohort (Supplement Figure 2). To ensure stable estimates of hospital-level early follow-up used in our analyses, we increased the threshold for excluding low-volume hospitals from ≥25 to ≥50 cases. Among the 22,314 patients treated at 175 sites in this analysis, there was no association of early follow-up with readmission (OR per 5% increase early follow-up 1.01; 95% CI 0.98, 1.03; p=0.67 using the 3rd adjustment model).
Next, we included patients discharged to skilled nursing facilities (n=3,931) into our analysis, as this population is generally at higher readmission risk due to disease severity and comorbid conditions, but failed to demonstrate any relationship between early follow-up and readmission (OR per 5% increase early follow-up 0.99; 95% CI 0.96, 1.02; p=0.49 using the 3rd adjustment model). Although CMS policies currently target all-cause readmission, we were interested to see if there was any potential impact of early follow-up on unplanned readmissions. Among the 24,165 patients included in our main study population, 15.7% (n=3,800) had unplanned 30-day readmissions, yet no relationship between early follow-up and unplanned readmissions was found (OR per 5% increase in early follow-up 1.00; 95% CI 0.97, 1.02; p=0.84 using the 3rd adjustment model). Our data also do not support an association between early follow-up and readmission among non-revascularized patients (n=10,061; OR per 5% increase early follow-up 0.99; 95% CI 0.96, 1.02; p=0.71 using the 3rd adjustment model). This hypothesis was tested due to the fact that this group may be more reliant on anti-anginal medications for symptom relief and might benefit from earlier physician evaluation of the adequacy of their medication regimens.
Next, we included an additional measure of socioeconomic status, median household income, to our adjustment model, as patients with lower socioeconomic status may be at higher risk of readmission; despite this addition, we saw no change in our primary results (OR per 5% increase early follow-up 0.99; 95% CI 0.97, 1.02; p=0.59 using the 3rd adjustment model). Finally, recognizing that both NSTEMI and STEMI patients are included in CMS readmission payment policies, we included an additional 1,512 STEMI patients meeting other inclusion and exclusion criteria into our analysis. In this expanded population, we did not find any relationship between early follow-up and readmission (OR per 5% increase early follow-up 1.00; 95% CI 0.97, 1.02; p=0.85 using the 3rd adjustment model).
Discussion
In the U.S., 30-day readmissions following AMI are common and increase resource use. Among over 25,000 older NSTEMI patients in the CRUSADE Registry, we found wide variation among hospitals in early physician follow-up use after discharge. Nevertheless, we did not find that those hospitals more commonly using early physician follow-up had lower rates of 30-day all-cause readmission. In addition, sensitivity analyses extended these null findings to 30-day cardiovascular readmissions, high-risk subgroups, and early cardiology follow-up. Therefore, these data do not support the hypothesis that more frequent early physician follow-up within a week of discharge can reduce 30-day readmissions in the AMI population. Early follow-up may still be important in managing the transition from hospital to outpatient care after an acute event.
While it seems intuitive that strategies focusing on the “transitional” period after hospitalization would be effective in reducing 30-day readmissions, data on these interventions are inconsistent. Randomized trials have shown that comprehensive discharge planning and implementation of care transition teams can reduce readmissions in older and heart failure populations.10–12 Observational data also suggest an association between physician follow-up and reduced readmission for Medicare beneficiaries and for patients hospitalized with chronic obstructive pulmonary disease (COPD).13,14 However, physician follow-up has not been found to reduce readmissions for general medicine patients,15 and a systematic review of interventions to reduce 30-day readmission found no consistent association of any single intervention or group of interventions with reduced readmission.16
Although a study found an association between physician follow-up within 7 days of discharge and reduced 30-day readmission in the heart failure population,4 we failed to demonstrate a similar relationship among patients hospitalized for NSTEMI. Heart failure and COPD—two diseases for which physician follow-up has been linked with reduced readmissions—are more chronic conditions, whereby careful titration of medications and short-term physiology for recurrence may affect patient symptoms and disease exacerbations. The need for active patient education in heart failure and COPD may also make it more plausible that early contact following discharge can reinforce behavioral and medication instructions and, subsequently, reduce readmission risk. In contrast, post-discharge readmission rates are lower in the AMI population, and these patients may be less likely to have disease-specific decompensation early after the index event—particularly after coronary revascularization and with active secondary prevention medications prescribed at discharge. As a result, the putative benefits of early physician follow-up may be diminished for AMI patients relative to these other conditions.
Other factors specific to AMI may also affect readmission risk. Patients presenting with AMI who experience complications after angiography or revascularization, such as contrast-induced nephropathy, are at higher risk for 30-day readmission and may require inpatient management for these complications.17 Furthermore, data suggest that approximately one-third to one-half of readmissions after incident MI are for unrelated reasons.17,18 Likewise, we found that 28.56% (n=3024) of 30-day readmissions after AMI in our study were non-cardiovascular. Thus, the unavoidable nature of procedural complications requiring inpatient treatment and frequency of readmissions unrelated to index admission among AMI patients may partly explain our findings. Although early physician follow-up may play an important role in limiting preventable readmissions in this population, deciphering these events post-hoc may be confounded.
Another important outcome we examined was mortality after admission for AMI. In our study, the 30-day mortality rate was only 2.5%. Prior data indicate that interventions focused on transitions of care may improve 1-year and even longer-term survival,19,20 yet when assessed, we did not find an association between early physician follow-up and 30-day readmission or mortality. Our findings may be due to the low rate of short-term mortality after hospital discharge in our population. Further exploration of the effect of early physician follow-up on longer-term outcomes is warranted.
While our analysis did not demonstrate an impact of physician follow-up within 7 days of discharge on readmissions, physician visits remain an important component of post-hospitalization transitional care. These visits provide the opportunity to ensure patient understanding of changes to medication regimens and activity limitations, confirm patient compliance with and tolerance of medications, and follow-up on any outstanding test results. However, there is little current evidence to support scheduling follow-up specifically within the first week after discharge to improve patient outcomes.4 Indiscriminate application of such a policy could have significant financial implications, and our data do not suggest that this strategy will be effective in the general population to reduce readmissions after AMI. Taken together, our findings that 30-day readmissions are common and are not associated with early follow-up highlight the need to both improve risk stratification to accurately identify AMI patients at highest risk for readmission and to investigate other potential strategies to reduce 30-day readmission after AMI hospitalizations.
Limitations
Our study had several limitations. First, our analysis was observational. Patients treated at hospitals with greater early follow-up were sicker, and use of statistical adjustment and hospital-level analyses may not have fully accounted for confounding by severity of illness. Second, our study was restricted to Medicare beneficiaries, potentially limiting generalizability to younger patients. Nevertheless, Medicare patients make up a large proportion of MI admissions and are at higher risk of readmission. Third, we defined early follow-up as a physician visit within 7 days post-discharge and examined 30-day outcomes. The 7-day window has been previously studied and was chosen for historical precedent as well as for clinical plausibility: a large proportion of post-AMI readmissions occur within 15 days of hospitalization and could potentially be prevented by an early physician visit.18 However, prior studies showing the benefit of physician follow-up on readmission have examined a larger range of timeframes for both variables and could be explored in AMI patients.13,14 We also chose to evaluate follow-up with any physician because of expected greater primary care physician availability for early follow-up, as well as the important role that primary care physicians play in patient care. A sensitivity analysis examining early cardiology follow-up did not significantly change our primary results.
Fourth, previous analyses have demonstrated improved outcomes with better integration of care from the hospital to outpatient setting,21 yet we lacked data on other factors that may affect readmission risk, including home health visits, non-physician medical contacts, degree of coordination of hand-offs from inpatient to outpatient providers, and patient education. In our study, early follow-up did not appear to be associated with reduced readmissions in patients at highest risk for mortality; whether these patients also represent the highest risk group for readmission is unclear, as prediction models for readmission after AMI have generally not performed well.22 Fifth, we examined the impact of early physician follow-up as an isolated intervention, whereas early follow-up might prove more effective as part of a bundled strategy.21 Finally, the hospital-level variable may be too insensitive to detect a relationship between follow-up and readmission using our statistical methodology and among our study population. CRUSADE was a voluntary initiative; hence, participating hospitals were likely more interested in ACS quality improvement. The lack of benefit seen with early follow-up in this hospital-level analysis might be related to high levels of discharge processes and standards for ACS care already in place at sites.
Conclusions
Readmissions after AMI are common, and approximately 1 in 5 older NSTEMI patients in our study was readmitted within 30 days after discharge. Most NSTEMI patients were not seen in follow-up by a physician within a week of discharge, though rates of early follow-up varied across sites. Despite this variation, we did not find an association between early physician follow-up and lower rates of 30-day readmission. Therefore, our data suggest that indiscriminate application of an early follow-up policy may not reduce 30-day readmission after AMI. Other approaches to improve readmission rates in this population should be investigated.
Supplementary Material
Acknowledgments
We thank Erin LoFrese for her editorial contributions to this manuscript. Ms. LoFrese did not receive compensation for her contributions, apart from her employment at the institution where this study was conducted.
Funding Sources: CRUSADE was funded by Millennium Pharmaceuticals, Schering-Plough Corporation, and the Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership. Connie N. Hess received support from the National Institutes of Health (5T32HL069749-09). Funding sources had no role in the design, conduct, or reporting of the study.
Footnotes
Conflict of Interest Disclosures: Dr. Shah reports consulting for Castlight. Health, LLC and Cardinal Health. Dr. Roe reports research funding from Eli Lilly & Company, KAI Pharmaceuticals, and Sanofi-Aventis (all significant); educational activities or lectures for AstraZeneca and Janssen Pharmaceuticals (both modest); consulting for Bristol Myers Squibb, Eli Lilly & Company, Glaxo Smith Kline, and Regeneron (all modest), Merck & Co., Janssen Pharmaceuticals, and Daiichi-Sankyo (all significant). Dr. Peterson reports research funding from Eli Lilly & Company, Ortho-McNeil-Janssen Pharmaceuticals, Inc., Society of Thoracic Surgeons, American Heart Association, American College of Cardiology (all significant); consulting for AstraZeneca, Boehringer Ingelheim, Genentech, Johnson & Johnson, Ortho-McNeil-Janssen Pharmaceuticals, Inc., Pfizer, Sanofi-Aventis, and WebMD (all modest). The remaining authors have no disclosures.
References
- 1.Wier LM, Andrews RM. Statistical Brief #107. The national hospital bill: the most expensive conditions by payer, 2008. [Accessed January 18, 2013];Healthcare cost and utilization project. web site. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb107.pdf. Updated March, 2011.
- 2.Bernheim SM, Grady JN, Lin Z, Wang Y, Savage SV, Bhat KR, Ross JS, Desai MM, Merrill AR, Han LF, Rapp MT, Drye EE, Normand SL, Krumholz HM. National patterns of risk-standardized mortality and readmission for acute myocardial infarction and heart failure. Update on publicly reported outcomes measures based on the 2010 release. Circ Cardiovasc Qual Outcomes. 2010;3:459–467. doi: 10.1161/CIRCOUTCOMES.110.957613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patient protection and affordable care act of 2010, Public law 111–148, 11th Congress. U.S. government printing office web site. http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf. Updated March 23, 2010. Accessed January 18, 2013.
- 4.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Peterson ED, Curtis LH. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 5.Roe MT, Chen AY, Thomas L, Wang TY, Alexander KP, Hammill BG, Gibler WB, Ohman EM, Peterson ED. Predicting long-term mortality in older patients after non-ST-segment elevation myocardial infarction: the CRUSADE long-term mortality model and risk score. Am Heart J. 2011;162:875–883. e1. doi: 10.1016/j.ahj.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Hoekstra JW, Pollack CV, Jr, Roe MT, Peterson ED, Brindis R, Harrington RA, Christenson RH, Smith SC, Ohman EM, Gibler WB. Improving the care of patients with non-ST-elevation acute coronary syndromes in the emergency department: the CRUSADE initiative. Acad Emerg Med. 2002;9:1146–1155. doi: 10.1111/j.1553-2712.2002.tb01569.x. [DOI] [PubMed] [Google Scholar]
- 7.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009;157:995–1000. doi: 10.1016/j.ahj.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, Van De Werf F, Avezum A, Goodman SG, Flather MD, Fox KA. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 9.Krumholz HM, Lin Z, Drye EE, Desai MM, Han LF, Rapp T, Mattera JA, Normand ST. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Int Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 11.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 12.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291:1358–1367. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 13.Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Int Med. 2010;170:1664–1670. doi: 10.1001/archinternmed.2010.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin CY, Barnato AE, Degenholtz HB. Physician follow-up visits after acute care hospitalization for elderly Medicare beneficiaries discharged to noninstitutional settings. J Am Geriatr Soc. 2011;59:1947–1954. doi: 10.1111/j.1532-5415.2011.03572.x. [DOI] [PubMed] [Google Scholar]
- 15.Grafft CA, McDonald FS, Ruud KL, Liesinger JT, Johnson MG, Naessens JM. Effect of hospital follow-up appointment on clinical event outcomes and mortality. Arch Int Med. 2010;170:955–960. doi: 10.1001/archinternmed.2010.105. [DOI] [PubMed] [Google Scholar]
- 16.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Int Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 17.Dunlay SM, Weston SA, Killian JM, Bell MR, Jaffe AS, Roger VL. Thirty-day rehospitalizations after acute myocardial infarction: a cohort study. Ann Int Med. 2012;157:11–18. doi: 10.7326/0003-4819-157-1-201207030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Bernheim SM, Suter LG, Drye EE, Krumholz HM. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ho PM, Luther SA, Masoudi FA, Gupta I, Lowy E, Maynard C, Sales AE, Peterson ED, Fihn SD, Rumsfeld JS. Inpatient and follow-up cardiology care and mortality for acute coronary syndrome patients in the Veterans Health Administration. Am Heart J. 2007;154:489–494. doi: 10.1016/j.ahj.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 20.Rogers AM, Ramanath VS, Grzybowski M, Riba AL, Jani SM, Mehta R, De Franco AC, Parrish R, Skorcz S, Baker PL, Faul J, Chen B, Roychoudhury C, Elma MA, Mitchell KR, Froehlich JB, Montoye C, Eagle KA. The association between guideline-based treatment instructions at the point of discharge and lower 1-year mortality in Medicare patients after acute myocardial infarction: the American College of Cardiology’s Guidelines Applied in Practice (GAP) initiative in Michigan. Am Heart J. 2007;154:461–469. doi: 10.1016/j.ahj.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Oddone EZ, Weinberger M. Hospital readmission rates: are we measuring the right thing? Ann Intern Med. 2012;157:910–911. doi: 10.7326/0003-4819-157-12-201212180-00013. [DOI] [PubMed] [Google Scholar]
- 22.Desai MM, Stauffer BD, Feringa HH, Schreiner GC. Statistical models and patient predictors of readmission for acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2009;2:500–507. doi: 10.1161/CIRCOUTCOMES.108.832949. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.