Abstract
This paper describes process data from a randomized controlled trial among 781 adults recruited in the Emergency Department who reported recent drug use and were randomized to: intervener-delivered brief intervention (IBI) assisted by computer, computerized BI (CBI), or enhanced usual care (EUC). Analyses examined differences between baseline and post-intervention on psychological constructs theoretically related to changes in drug use and HIV risk: importance, readiness, intention, help-seeking, and confidence. Compared to EUC, participants receiving the IBI significantly increased in confidence and intentions; CBI patients increased importance, readiness, confidence, and help-seeking. Both groups increased relative to the EUC in likelihood of condom use with regular partners. Examining BI components suggested that benefits of change and tools for change were associated with changes in psychological constructs. Delivering BIs targeting drug use and HIV risk using computers appears promising for implementation in healthcare settings. This trial is ongoing and future work will report behavioral outcomes.
Keywords: computer-delivered therapy, emergency department, drug use, HIV, brief interventions
1. Introduction
1.1 Brief interventions for alcohol and/or other drug use
Screening, brief intervention, and referral to treatment (SBIRT) for substance use offer opportunities for early detection, motivational enhancement, and encouragement to seek treatment. The Emergency Department (ED) is a setting where BIs can be delivered in a “teachable moment” to reach non-treatment seeking patients who use substances. ED SBIRTs for alcohol have promising findings for alcohol-related consequences, but mixed findings on consumption (Academic ED SBIRT Collaborative, 2007; Bazargan-Hejazi et al., 2005; Field, Baird, Saitz, Caetano, & Monti, 2010; Forsythe & Lee, 2012; Havard, Shakeshaft, & Sanson-Fisher, 2008; Longabaugh et al., 2001; Monti et al., 2007; Nilsen et al., 2008). Evidence supports the cost-effectiveness of alcohol SBIRTs in the ED and primary care (Fleming et al., 2002; Gentilello, Ebel, Wickizer, Salkever, & Rivara, 2005; Neighbors et al., 2010). Billing codes have been created allowing for reimbursement for SBIRT (Fussell, Rieckmann, & Quick, 2011).
In contrast, few randomized controlled trials have tested SBIRTs for drugs in the ED (Cunningham et al., 2009), and most have been in adolescents (e.g., Bernstein et al., 2009) with a few studies of adults (Bernstein et al., 1997; 2005; Blow et al., 2010; Madras et al., 2009; Woolard et al., 2013). However, an ED alcohol SBIRT for young adults also reduced marijuana use (Magill, Barnett, Apodaca, Rohsenow, & Monti, 2009). The ED is an important setting for drug BIs given that people who use drugs are more likely to seek ED care than those who do not and data showing that 35-40% of ED patients have positive toxicology screens for illicit drugs (Cherpitel et al., 2003; Fuda & Immekus, 2006; Sohler et al., 2007; Vitale & Van de Mheen, 2006). The ED may be the only location to reach the large number of patients who visit the ED but do not have primary care and/or do not routinely receive any other medical care (Brown et al., 2012; Moineddin, Meaney, Agha, Zagorski, & Glazier, 2011). Urban EDs provide a setting for reaching a low socio-economic status, at-risk population (Geurts, Palatnick, Strome, & Weldon, 2012; Harris, Patel, & Bowen, 2011) that may not otherwise receive SBIRT.
1.2 Technology enhanced BIs for alcohol and/or other drug use
Despite the support for ED SBIRT, translation into practice has lagged due to limited staff time and personnel barriers required to deliver BIs with fidelity (Carroll & Rounsaville, 2011). One approach to overcome such barriers is to use technology to facilitate SBIRT delivery (Bickel, Christensen, & Marsch, 2011; Blow et al., 2006; Cunningham et al., 2009; Ondersma, Svikis, & Schuster, 2007). Computer technologies for substance use SBIRTs have been tested in practice settings; however, few occurred in the ED, most focused on alcohol rather than drug use, and evidence for these BIs with adults is mixed. For example, a computerized brief advice session decreased alcohol intake in injured ED patients (Neumann et al., 2006). A computerized alcohol screening and printed feedback reduced weekly consumption and heavy episodic drinking (for a long-feedback group, but not a short-feedback group), but did not change the overall proportion of “risky” drinkers (Trinks, Festin, Bendsten, & Nilsen, 2010; 2013). Another ED study found that computerized screening, tailored feedback, and tailored brief advice resulted in less alcohol consumption compared to conditions without brief advice (Blow et al., 2006).
Ondersma and colleagues (2007) developed a computerized single-session motivational interviewing-based BI for post-partum women with past drug use that reduced illicit drug use relative to a control group. Within-session data (captured via computer) on participants’ cognitions related to the intervention indicated that higher intervention satisfaction, lower perceived likelihood of future drug use, and within-session increases in treatment readiness were related to less drug use over a four-month follow-up (Ondersma, Grekin, & Svikis, 2011). Further, evidence supports that patients find computer-based BIs easy to use, enjoyable, and comfortable (Moore, Fazzino, Garnet, Cutter, & Barry, 2011; Murphy et al. 2013; Ondersma et al., 2005). Few studies, however, describe BIs for drug use among adults in detail and none have been applied in the ED. Computer-enhanced BIs allow for capturing data on potential active intervention components (i.e., “the black box of intervention) and process variables that may influence the efficacy of BIs (e.g., beliefs about drug use; Ondersma, Grekin, & Svikis, 2011).
1.3 Brief interventions for drug use and HIV risk behavior
BIs can concurrently target multiple risk behaviors, such as HIV risk behaviors (e.g., injecting drugs, risky sex) which often occur among adults who use drugs (e.g., El-Bassel, et al., 2001; Petry, 2001; Tross et al., 2009) yet are not addressed in most BIs. HIV risk behaviors may respond to BIs because decreased drug use may lead to involvement in fewer risky situations during which unprotected sex could occur and/or fewer episodes of intoxication which may lead to sexual risk behavior at the event level (Bryan, Schmiege, & Magnan, 2012; Stein, Anderson, Charuvastra, & Friedmann, 2001). Bernstein and colleagues (2012) provided initial support for a therapist-delivered BI for sexual risk reduction among adult ED patients who use drugs. Although patients receiving the BI, which included voluntary pre-test counseling and HIV testing, reduced sexual risk behaviors, and heroin and cocaine use, so did control patients who received pre-test counseling and HIV testing only. Marsch and Bickel (2004) found that a multi-session computerized educational HIV risk reduction BI was superior to a two-session therapist-delivered educational BI with regard to AIDS knowledge. Individuals in both conditions reduced their drug- and sex-related HIV risk behaviors, yet other drug use outcomes were not reported and this intervention was not designed to specifically reduce drug use. Further research is needed to develop and evaluate BIs for drug users that also integrate HIV risk reduction for ED patients.
1.4 The Present Study
Due to the high volume of patients with drug use in inner-city EDs, feasible, effective BIs for drug use and HIV risk behaviors that could reduce the associated public health burden are needed. Computers may bridge the gap between evidence-based BIs and implementing best practices while addressing research questions regarding process variables. Computerized ED-based BIs may address time and personnel barriers, as well as the facilitate fidelity and tailoring strategies to increase participants’ attention and receptivity, thereby increasing cognitions related to behavior change (Kreuter, Strecher, & Glassman, 1999; Lustria, Cortese, Noar, & Glueckauf, 2009). BIs must also be adaptable to the unique setting in order to provide flexible solutions to organizational and personnel challenges of implementation (Nilsen, 2010).
Therefore, in order to increase the availability and applicability of SBIRT for drug use in EDs, and to add to the literature on therapist and computer-delivered BIs, the present study developed and evaluated two tailored BIs among drug-using adults presenting to the ED: a fully computerized BI delivered on a tablet computer and a therapist-delivered BI that is guided by a tablet computer. During the BIs, data were captured on the computer in order to characterize within-session processes (e.g., concerns, benefits of change, etc.). The present paper describes the two BIs, reports the unique data captured throughout the intervention process, and evaluates whether the interventions, compared to enhanced usual care, result in pre- to post-intervention changes in psychological constructs conceptually related to drug use and HIV risk behavior change (e.g., importance, readiness, intention, help-seeking, and confidence). Hypotheses were that participants in both BI conditions would report significant increases in these psychological constructs relative to a control condition. Because the purpose of this study was to develop and assess the efficacy of the BIs in comparison to usual care, the study was not powered to detect differences between active interventions; however, we also conducted exploratory analyses evaluating the BIs relative to one another. Finally, exploratory analyses examining the association between various intervention components (e.g., concerns, tools for change) in relation to changes in psychological constructs from pre- to post-intervention were conducted.
2. Methods
2.1 Study Design
Study data come from a randomized controlled trial (HealthiER You). Procedures were approved by institutional review boards at the University of Michigan and Hurley Medical Center (HMC); a Certificate of Confidentiality was provided by the National Institutes of Health.
2.2 Study Setting and Population
Project HealithiER You took place in the HMC Emergency Department in Flint, Michigan. HMC is a 540-bed teaching hospital, Level 1 trauma center, and the only public hospital in Flint. HMC’s ED receives nearly 85,000 visits annually. Flint is a mid-sized city with poverty and crime rates similar to other urban centers (e.g., Camden, NJ; Philadelphia, PA; Oakland, CA; Federal Bureau of Investigation, 2007; Webster & Bishaw, 2007).
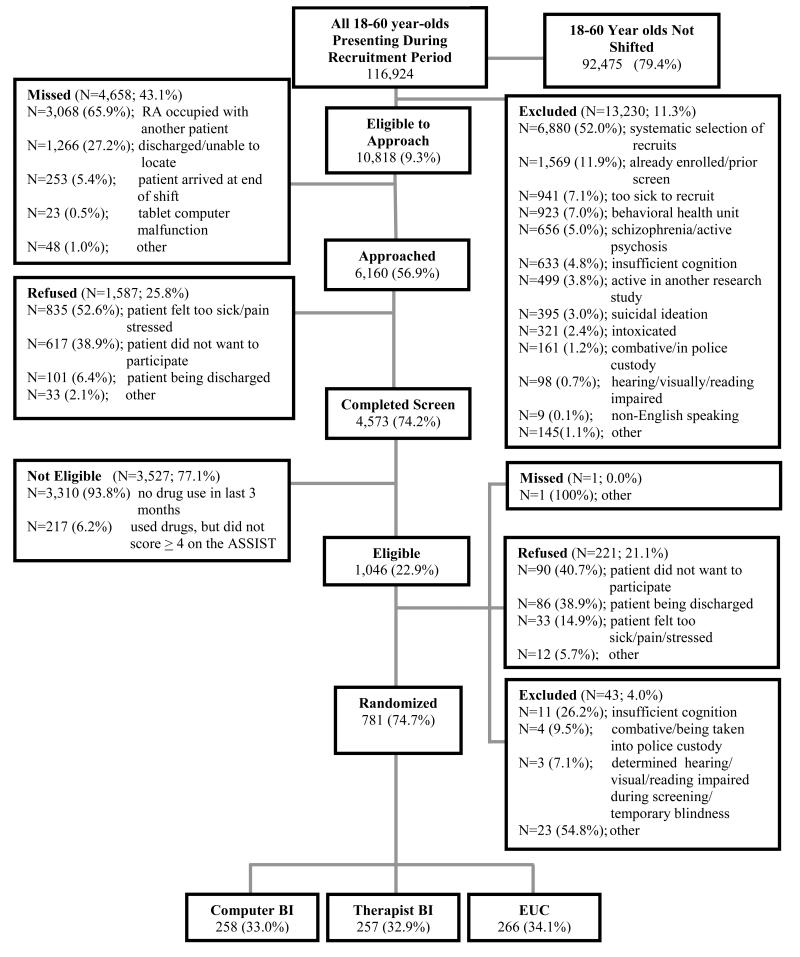
Patients aged 18-60 presenting to the ED were eligible for screening. Exclusion criteria included presenting with a condition precluding informed consent (acute psychosis, unconscious, insufficient cognitive orientation, medically unstable) and other criteria shown in Figure 1. Patients who were acutely intoxicated were approached after observation that they would be able to consent. Because more participants presented than research staff could screen at a given time, potential recruits were systematically selected. Those who refused participation were to provide information on gender and race (at baseline only) as well as reasons for refusal.
Figure 1.
HealthiER You recruitment flow and randomization.
2.3 Study Protocol
Recruitment occurred from February 2011 to March 2013, with patients recruited four days a week (except major holidays) on evening shifts for the entire course of the study (~3:00pm-midnight). Days of the week (Mondays, Tuesdays, Sundays, etc.) were covered equally throughout the study on a rotating schedule. During the first year, day shifts (triage from 8:00am-4:00pm) were randomly selected three days per month and midnight shifts (triage from 12:00am- 8:00am) were randomly selected once a month; these shifts were not covered after the first year given the lower yield of participants during these shifts compared to evening shifts.
All study-eligible ED patients (ages 18 to 60) were identified via electronic patient tracking logs. Far more patients presented during shifts than could be approached. To determine who to approach, we used a systematic selection procedure based on number of staff, rotating through ED section, and using pre-selected random digits corresponding to patients’ account numbers. Patients were approached by research staff in ED treatment and waiting areas, and were asked to complete screening surveys. Interested patients gave written informed consent, self-administered a 15-minute computerized survey (audio optional), and received a gift ($1.00 value; e.g., puzzle book, playing cards). Those reporting past 3-month use of illicit drugs or misuse of psychoactive prescription drugs and met an Alcohol, Smoking, and Substance Involvement Screening Test (see measures section) score of four or more on any of the illicit or prescription drug scales were eligible for the trial. Those interested in participating gave a second written informed consent before taking a 30-minute computerized baseline assessment (audio optional), followed by a semi-structured interview (assessments compensated with $20 cash) and urine drug screen (compensated with $5 cash). Using computer randomization (stratified by gender and meeting criteria for a drug use disorder), participants were assigned and immediately provided with one of three conditions: 1) a 30-minute therapist-delivered “intervener” BI with computer guidance (IBI), 2) a 30-minute computer-delivered BI (CBI), or, 3) enhanced usual care (EUC) which included a 3-minute review of written health resource brochures. The semi-structured interviews and BIs were audio-recorded. Upon completion of the assigned condition, participants self-administered a 5-minute computerized post-test questionnaire.
2.4 Measures
2.4.1. Substance use
During screening, patients completed the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST; Humeniuk et al., 2008; WHO ASSIST Working Group, 2002) for drug use (i.e., marijuana, cocaine, inhalants, hallucinogens, street opioids, methamphetamines, and prescription opioids, stimulants, and sedatives) during the past year and past three months. We used past three month ratings and calculated the total ASSIST score for marijuana separately because it was, the most commonly used drug by the sample. Other drugs were used infrequently, so we created two total ASSIST scores for all other illicit drugs and the three prescription drugs by summing the items for each drug’s subscale; a score of 4 or more reflects moderate risk (Humeniuk et al., 2008). Participants completed the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) for the past three months on which a score of 8 or higher reflects harmful alcohol use.
2.4.2 Psychological constructs associated with behavior change
Readiness Rulers were adapted to assess psychological constructs conceptually related to drug use behavior change, condom use, and HIV testing (Daeppen, Bertholet, Gmel, & Gaume, 2007; Hesse, 2006; LaBrie, Quinlan, Schiffman, & Earleywine, 2005). Patients rated the importance of and their readiness to cut down or quit using drugs “right now.” Plan (intention) to cut down or quit, how much help (help-seeking) is wanted for drug use, and confidence (self-efficacy) to reduce drug use were asked for the “next 3 months.” Current importance of using condoms “every time” was rated for regular and casual sex partners. Likelihood (intention) of using condoms every time with regular and casual partners and HIV testing in the next 3 months were queried. Rulers used a 10-point rating scale with anchors displayed for 1 (Not at all Important, Not Likely, etc.) and 10 (Very Important, Very Likely, etc.). The items were presented during the baseline assessment and were repeated during the post-test survey immediately following intervention administration.
2.4.3 Intervention Attitudes
After IBI and CBI sessions, participants rated the helpfulness of the intervention (“the computer program” or “talking with the health counselor”) “in making decisions about your drug use.” Participants completed an item asking how easy it was to “use the computer program with the health counselor” (CBI group) or to “use the computer while talking with your health counselor” (IBI group). Responses for each item ranged on a five-point Likert-type scale from “Not at All” to “Extremely.”
2.4.5 Data Capture of Intervention Components
Through the IBI and CBI, patients enter data into the computer tablets via a stylus. Participants are prompted to select goals (up to five from categories: internal/improve feelings, social/family/friends, health, activities/free time, work/school/finances), concerns (captured in CBI only; 27 options in five categories: health, activities/free time, work/school/finance, controlling drug use, with family/ friends), perceived benefits of changing drug use (35 options in CBI and 36 options in IBI in six categories: internal/improved feelings, social/ family/friends, health, activities/free time, reduced risk for sexually transmitted infection, work/school/finances), challenges (captured in CBI only), tools to reduce drug use (33 options in five categories: tools for managing people/places/situations, turning down using with others, managing thoughts and feelings, finding other things to do, spending time with healthy supports) and personal and social strengths (8 personal, 10 social).
2.4.6 Demographics
Items were adapted from prior research (Cacciola, Alterman, McLellan, Lin, & Lynch, 2007; McLellan, Cacciola, Carise, Coyne, & 1999; Office of Applied Studies, 2009; Smith et al., 1996; 2006) to capture participants’ demographics (e.g., age, gender, race, education) and other relevant characteristics (e.g., self-reported HIV status, HIV risk behaviors, and HIV testing history; Darke, Hall, Heather, Ward, & Wodak, 1991; Peralta, Deeds, Hipszer, & Ghalib, 2007; Wu, Ringwalt, Patkar, Hubbard, & Blazer, 2009).
2.5 Description of BI Conditions
Both BIs are based on motivational interviewing (MI; Miller & Rollnick, 2002) and the trans-theoretical model of change (Prochaska & DiClemente, 2002; Prochaska, Diclemente, & Norcross, 1992) and use FRAMES (Feedback, emphasis on Responsibility for change, Advice, Menu of options, Empathy, and Support for self-efficacy; Miller & Rollnick, 2002). The BIs were designed to address drug use, with HIV risk behaviors as a secondary outcome. The 30-minute BIs provided tailored feedback for drug use and consequences (generated from computerized assessment measures), reviewed participants’ goals, focused on developing discrepancy between drug use and ability to meet goals by eliciting consequences of use and benefits of changing use, identifying stage of change, and developing a change plan with the participant by identifying challenges and strategies to facilitate change (Table 1). BI participants received the review of community and treatment resources provided to the EUC group, however BI groups also received seven resource pamphlets (including food, employment, housing, legal, violence prevention, and overdose and substance use prevention). Briefly, BI participants uniquely explored with the therapist the resources of most interest to them. BIs were conducted during the ED visit; breaks were taken for medical studies or treatment as needed. For confidentiality, family/friends with the patient were asked not to remain close by during participation. The CBI and IBI were designed to present similar content using different modalities. At the end of each BI, participants received a 4-page “change plan” booklet containing: goals, plan related to their use, benefits, tools, and strengths.
Table 1.
Description of HealthiERYou BIs.
| Sections | Tasks for both BIs | Computer BI Tasks | Therapist BI Tasks |
|---|---|---|---|
|
What’s this
all about? ~2min |
|
|
|
|
| |||
|
What’s
important to me? ~4min |
|
|
|
|
| |||
|
What are
my health habits? ~2min |
|
|
|
|
| |||
|
How can
my health habits affect me? ~4min |
|
|
|
|
| |||
|
How can change improve
things? ~6min |
|
|
|
|
| |||
|
What’s
next for me? ~12min |
|
|
|
Note. DC indicates data capture by computer.
2.5.1 Computerized BI
The CBI was delivered via touchscreen tablet computers with audio headphones. The CBI included still images of actors streamed together and interactive questions and exercises. Participants first received a user tutorial and introduction by a virtual doctor comprised of still images and a recorded voice. Participants then selected one of 6 virtual health counselors (varied by race: African American, Hispanic, European American, and gender) by touching their picture, and the therapist’s voice was heard and varying streaming still images (silhouette overlaying an engaging screen of text) appeared throughout the CBI.
The virtual health counselor introduced choices and activities on the computer. Although the counselor delivered highly tailored reflections and summaries, based on participants’ activity responses, the responses were not read aloud by the counselor. Short video vignettes were developed; streaming together images of actors in a community scene. Vignettes included a recorded voice of the character telling a personal story of drug use (fictional scenario). Actors reflected the minority and gender characteristics relevant for inner city multi-ethnic participants. Interactive exercises during the CBI included: 1) choosing pictures of relevant life areas and selecting goals, concerns, benefits, change statement, challenges, tools/strategies and strengths; from which selections are saved and strategically displayed during later activities; 2) completing an importance ruler on a scale of 1 to 10; and, 3) viewing summarized content of previous selections in a visually dynamic design. This required active participation on exercise screens, combined with listening to strategic statements and summaries from the virtual health counselor in between exercises. The content included tailored feedback regarding drug use patterns, and completing exercises around identifying goals and values, concerns of drug use, benefits of changing use, personal strengths, and formulating a change plan specific to their identified stage of change (includes identifying challenges of avoiding use and tools/strategies towards change).
2.5.2 Intervener BI
The IBI was delivered by master’s level therapists (n = 8) trained in psychology and/or social work who received a two-day (16 hours) interactive workshop on motivational interviewing (by investigators), and small group trainings over the first month of employment, including IBI content review and role plays, led by clinicians practicing MI. Ongoing monthly individual supervision and twice monthly group supervision involved review of audiotaped sessions with one of several clinical psychologists or social workers (n=5).
Therapists used a touchscreen tablet computer to guide the session and to aid with protocol adherence and understanding of each participant’s baseline drug use. Screens for each element of the IBI (Table 1) included an optional therapist-specific screen including reminders of the purpose and goals of each element and key strategies. Throughout the IBI, the therapist handed the participant the computer so that he/she could view and collaboratively select goals, concerns, benefits, readiness to change statements for each drug, tools to manage challenging situations, and strengths. During the feedback portion of the IBI, participants viewed a graphic depicting the local prevalence of each substance the patient reported using during screening. The final screen IBI displayed a tailored summary which therapists used to provide a final verbal summary and which was printed and provided to the participant. Throughout the IBI, therapists could also review selections the participant made (goals, concerns about drug use, benefits of cutting down or quitting, readiness to change, tools, and personal and social strengths).
2.6 Data analysis
All data were analyzed using SAS 9.22 (SAS Institute; Cary, North Carolina). Means, frequencies, and other descriptive statistics were used to evaluate distributions and to summarize demographics and substance use. Chi-square and Wilcoxon signed rank non-parametric tests were used to evaluate differences across groups and between patients who were missed or refused participation and those who participated. Ratings of helpfulness and ease were estimated via proportions; counts, means, and proportions were used to summarize participants’ self-reported intervention components. Follow-ups for this trial are on-going, therefore results regarding BI effects on drug use and HIV risk behaviors are not yet available.
Repeated measures analyses compared the effects of the BI condition (IBI or CBI) on psychological constructs related to drug use (i.e., importance, readiness, intention, help-seeking, and confidence) and HIV risk behavior change (likelihood of HIV testing, importance and likelihood of condom use with regular and casual partners), compared to the EUC group based on data from pre- (baseline) to immediate post-test. Over 98% of those 781 randomized finished the BI (reasons for not completing were most often being discharged and computer error). A total of 717 (92%) completed the post-test (most commonly, post-tests were incomplete because they were discharged from the ED). For IBI vs. EUC and CBI vs. EUC, separate longitudinal linear mixed effects models were fit by residual maximum likelihood estimation, with time (pre-test [referent] and post-test), a two-level group, and time by group interactions as predictors. Based on suggestions by Peduzzi, Henderson, Hartigan, and Lavori (2002), time (coded 0 = baseline, 1 = post-test), CBI group (coded 0 = EUC, 1 = CBI), IBI group (coded 0 = EUC, 1 = IBI), and the group by time interaction were fixed effects, and the models were fit with random intercepts and a random slope for time. Effect sizes were estimated with the standardized mean difference for unequal sample sizes (Rosenthal & Rosnow, 2008). The study was powered to detect differences between the EUC group and each BI group, but not between the two BIs. However, we conducted exploratory analyses using the parameters above to compare the IBI vs. CBI.
For significant effects found for the IBI/CBI from pre- to post-test, we conducted partial correlations (using Fisher’s z-transformation; Fisher, 1970) between summary count variables of benefits, tools, strengths, and concerns and psychological constructs related to drug use changes measured at post-test, controlling for pre-test values on those same constructs. Because BI elements were moderately inter-correlated and variance inflation was a concern, we used partial correlations to estimate the degree of association between the psychological constructs at post-test and one of the BI element summary count variables, after taking into account the amount of variation in the post-test level of the psychological construct explained pre-test ratings.
3. Results
3.1 Study Sample
As shown in Figure 1, 24,048 patients presented to the ED during recruitment shifts; patients were excluded from recruitment most commonly due to systematic selection and being already enroled in the study or screened in the past 3 months. Potential recruits were most often missed due to staff being with another patient or discharge. Common reasons for refusal were for feeling too sick or not wanting to participate. A total of 4,573 completed screening, 22.9% were eligible for the baseline phase, and 74.7% were randomized to conditions (N = 781). Further details regarding refusals and exclusions are shown in Figure 1. At screening, men (48%) were more likely to be missed than women (40%) [χ2(1) = 63.4, p<.001]; age (categorized as 18-30 years and 31 years or older) distribution did not differ across those screened and missed. When comparing those who refused screening to those who consented, men (30%) refused more often than women (23%) [χ2(1) = 30.95, p<.001] and patients over age 30 (28%) refused more than those under 30 (23%) [χ2(1) = 21.83, p<.001]. At baseline, more men (26%) than women (19%) refused participation [χ2(1) = 8.84, p<.01] and fewer African Americans (19%) than individuals of other races/ethnicities (26%) refused [χ2(1) = 6.53, p<.05], but refusals at baseline did not differ across age group.
Table 2 displays demographics and substance use variables. Participants were mostly female (55%) and African American (56%), with a mean age of 31.2 years (SD = 10.9). No significant differences were observed by condition in demographics, substance use, or HIV risk behaviors. Past three-month marijuana use was reported by a large majority (90%). Alcohol and tobacco were also commonly reported (67% and 79%, respectively), but other illicit drugs (17%) and prescription drug misuse (17%) were less common. ASSIST scores suggest that marijuana was used to the greatest severity, although some problematic use of other drugs and prescription drugs was also evident. Most participants (80%) reported a prior HIV test; only 9 reported that a doctor told them they had HIV. The majority of sexually active participants reported not always using a condom during the past 3 months (78% with regular partners; 57% with casual partners).
Table 2.
Baseline sample demographics, substance use history, and HIV risk behaviors
|
Total (N = 781) % or M (SD) |
CBI (N = 258) % or M (SD) |
IBI (N = 257) % or M (SD) |
EUC (N =266) % or M (SD) |
|
|---|---|---|---|---|
| Female | 55% | 54% | 55% | 57% |
| African American (vs. other) | 56% | 58% | 54% | 56% |
| Married/Partnered (vs. other) | 29% | 27% | 26% | 34% |
| Age | 31.2 (10.9) | 30.7 (10.7) | 31.5 (11.0) | 31.3 (10.9) |
| High School Education or Less |
64% | 63% | 65% | 65% |
| Household income less than $19,999 |
77% | 75% | 80% | 77% |
| Extra income $100 or less | 70% | 72% | 70% | 69% |
| Employed | 26% | 24% | 24% | 30% |
| On probation/ parole | 7% | 10% | 4% | 7% |
| AUDIT score | 5.1 (7.2) | 5.6 (7.9) | 4.7 (6.6) | 4.9 (7.0) |
| Marijuana 3-month ASSIST score |
12.2 (8.3) | 12.7 (8.2) | 11.6 (8.6) | 12.4 (8.0) |
| Other Illicit Drugs 3-month ASSIST score |
4.2 (12.4) | 3.3 (10.2) | 4.50 (11.5) | 4.9 (14.9) |
| Prescription Drug 3-month ASSIST score |
4.0 (12.6) | 3.8 (12.7) | 3.8 (11.0) | 4.4 (13.9) |
| Sexually active in past 3 months |
85% | 84% | 83% | 87% |
| Inconsistent condom use with regular partnersa |
78% | 78% | 76% | 80% |
| Inconsistent condom use with casual partnersb |
57% | 62% | 51% | 58% |
| Ever had HIV test | 80% | 77% | 84% | 78% |
Calculated among those who were sexually active and had a regular partner in past 3 months (n = 608)
Calculated among those who were sexually active and had a casual partner in the past 3 months (n = 370).
3.2 Intervention Procedures and Attitudes
Regarding BI completion time, removing one outlier (>90 minutes), the IBI averaged 33.1 minutes (SD=11.4; range 9.9-72.1; n = 213 due to a computer error in tracking intervention times). The CBI averaged 25.4 minutes (SD=10.8; range 12.4-74.8; n = 249). Outliers reflect a limitation to this technology; if the participant or therapist did not pause the computer during a medical procedure, the computer recorded the entire time. The majority of participants in each BI condition reported finding the intervention “extremely” or “very much” helpful (CBI = 68%; IBI = 75%). In addition, among the two BI groups, the large majority of participants in both groups reported that using the computer was “very much” or “extremely” easy (CBI = 88%; IBI = 84%).
3.3. Intervention pre- and post-tests for psychological precursors of behavior change
Table 3 shows the results of longitudinal (pre- to post-test) analyses evaluating precursors of drug use behavior change for each BI group separately compared to EUC. There were no significant main effects for group in all analyses, indicating baseline equivalency on dependent measures. For importance, readiness, intention, and help-seeking (but not confidence) there were significant main effects for time in all analyses, indicating significant increases in these variables in the EUC group from baseline to post-test. Significant group by time interactions revealed that CBI patients reported greater increases in importance (d = .25), readiness (d = .24), help-seeking (d = .20) and confidence (d = .20) relative to the EUC group. IBI participants reported greater increases in confidence (d = .37) and in intention to reduce or quit drug use (d = .27) than EUC patients. In exploratory models comparing the IBI and CBI participants on pre- to post-test changes in these same constructs, the only significant group by time interaction occurred for confidence, indicating that CBI participants’ ratings of confidence increased less than IBI participants’ (β = −0.628, SE = 0.282, p <. 05, 95% CI = −1.18 - −0.07).
Table 3.
Repeated measures analyses (pre-test/post-test) examining changes in psychological constructs related to cutting down or quitting using drugs.
| Estimate (SE) | 95% CI | Effect Size (d) | |
|---|---|---|---|
| CBI vs. EUC group | |||
| Importance | |||
| Time | 0.825 (0.173) *** | 0.48 – 1.16 | |
| CBI group | 0.228 (0.330) | −0.42 – 0.88 | |
| Time × CBI group | 0.723 (0.256) ** | 0.21 – 1.23 | 0.25 |
| Readiness | |||
| Time | 0.491 (0.160) ** | 0.18 – 0.80 | |
| CBI group | 0.343 (0.323) | −0.29 – 0.98 | |
| Time × CBI group | 0.635 (0.237) ** | 0.17 – 1.10 | 0.24 |
| Intention | |||
| Time | 0.424 (0.158) ** | 0.11 – 0.73 | |
| CBI group | 0.543 (0.322) | −0.09 – 1.18 | |
| Time × CBI group | 0.234 (0.228) | −0.21 – 0.68 | |
| Help Seeking | |||
| Time | 0.768 (0.154) *** | 0.47 – 1.07 | |
| CBI group | 0.253 (0.319) | −0.37 – 0.88 | |
| Time × CBI group | 0.533 (0.248) * | 0.04 – 1.02 | 0.20 |
| Confidence | |||
| Time | −0.278 (0.174) | −0.62 – 0.06 | |
| CBI group | 0.181 (0.302) | −0.41 – 0.77 | |
| Time × CBI group | 0.563 (0.254) * | 0.06 – 1.06 | 0.20 |
| IBI vs. EUC group | |||
| Importance | |||
| Time | 0.828 (0.173) *** | 0.49 – 1.17 | |
| IBI group | 0.477 (0.328) | −0.17 – 1.12 | |
| Time × IBI group | 0.407 (0.278) | −0.14 – 0.95 | |
| Readiness | |||
| Time | 0.499 (0.160) ** | 0.18 – 0.81 | |
| IBI group | 0.369 (0.325) | −0.27 – 1.01 | |
| Time × IBI group | 0.437 (0.267) | −0.09 – 0.96 | |
| Intention | |||
| Time | 0.430 (0.158) ** | 0.12 – 0.74 | |
| IBI group | 0.346 (0.320) | −0.28 – 0.97 | |
| Time × IBI group | 0.542 (0.266) * | 0.02 – 1.06 | 0.27 |
| Help Seeking | |||
| Time | 0.770 (0.154) *** | 0.47 – 1.07 | |
| IBI group | 0.235 (0.317) | −0.39 – 0.86 | |
| Time × IBI group | 0.491 (0.257) | −0.01 – 1.00 | |
| Confidence | |||
| Time | −0.277 (0.174) | −0.62 – 0.07 | |
| IBI group | −0.059 (0.312) | −0.67 – 0.55 | |
| Time × IBI group | 1.191 (0.275) *** | 0.65 – 1.73 | 0.37 |
p < .05.
p<.01,
p<.001
Results of models evaluating changes in importance of and likelihood of condom use and likelihood of HIV testing are shown in Table 4. There were no main effects for group, indicating that the BI groups did not differ from EUC at baseline on these measures. For both groups compared to EUC, there were significant main effects for time on likelihood of HIV testing, importance of condom use with regular partners, and likelihood of condom use with regular partners. Significant group by time interactions were observed for likelihood of condom use with regular partners. Compared to the EUC, both the IBI group (d = .21) and the CBI group (d= .19) reported greater increases in likelihood from pre- to post-test. There were no significant group by time interactions in models comparing the IBI to CBI group participants on HIV variables. .
Table 4.
Repeated measures analyses (pre-test/post-test) examining changes in psychological constructs related to safer sex and future HIV testing.
| Estimate (SE) | 95% CI | Effect Size (d) |
|
|---|---|---|---|
| CBI vs. EUC group | |||
| Likelihood of testing (next 3 months) | |||
| Time | 0.772 (0.191) *** | 0.40 – 1.15 | |
| CBI group | 0.584 (0.337) | −0.08 – 1.25 | |
| Time × CBI group | 0.536 (0.302) | −0.06 – 1.13 | |
| Importance: condoms (regular partners) | |||
| Time | 0.818 (0.169) *** | 0.49 – 1.15 | |
| CBI group | 0.380 (0.352) | −0.31 – 1.07 | |
| Time × CBI group | 0.024 (0.263) | −0.49 – 0.54 | |
| Likelihood: condoms (regular partners) | |||
| Time | 0.580 (0.191) ** | 0.20 – 0.96 | |
| CBI group | 0.058 (0.353) | −0.63 – 0.75 | |
| Time × CBI group | 0.591 (0.276) * | 0.05 – 1.13 | .19 |
| Importance: condoms (casual partners) | |||
| Time | 0.125 (0.200) | −0.27 – 0.52 | |
| CBI group | 0.124 (0.319) | −0.50 – 0.75 | |
| Time × CBI group | 0.318 (0.262) | −0.20 – 0.83 | |
| Likelihood: condoms (casual partners) | |||
| Time | −0.006 (0.193) | −0.38 – 0.36 | |
| CBI group | −0.058 (0.325) | −0.70 – 0.58 | |
| Time × CBI group | 0.524 (0.270) | −0.01 – 1.05 | |
| IBI vs. EUC group | |||
| Likelihood of testing (next 3 months) | |||
| Time | 0.774 (0.191) *** | 0.40 – 1.15 | |
| IBI group | 0.502 (0.337) | −0.16 – 1.16 | |
| Time × IBI group | −0.046 (0.274) | −0.58 – 0.49 | |
| Importance: condoms (regular partners) | |||
| Time | 0.821 (0.169) *** | 0.49 – 1.15 | |
| IBI group | 0.518 (0.354) | −0.18 – 1.21 | |
| Time × IBI group | −0.035 (0.285) | −0.59 – 0.53 | |
| Likelihood: condoms (regular partners) | |||
| Time | 0.581 (0.192) ** | 0.20 – 0.96 | |
| IBI group | 0.160 (0.353) | −0.53 – 0.85 | |
| Time × IBI group | 0.730 (0.283) ** | 0.17 – 1.29 | 0.21 |
| Importance: condoms (casual partners) | |||
| Time | 0.094 (0.198) | −0.30 – 0.48 | |
| IBI group | 0.360 (0.310) | −0.25 – 0.97 | |
| Time × IBI group | 0.293 (0.272) | −0.24 – 0.83 | |
| Likelihood: condoms (casual partners) | |||
| Time | −0.011 (0.193) | −0.39 – 0.37 | |
| IBI group | 0.260 (0.314) | −0.36 – 0.88 | |
| Time × IBI group | 0.289 (0.278) | −0.26 – 0.83 |
p < .05.
p<.01,
p<.00l
3.4 Participants’ goals, concerns, challenges, benefits of change, tools and strengths
Participants in the IBI and CBI engaged in the BI by selecting a number of relevant components. The number of perceived benefits of reduced drug use selected was significantly higher in the CBI group (MCBI = 12.9, SD = 8.8, range = 1 to 35) than in the IBI group (MIBI = 9.0, SD = 5.5, range = 1 to 32; t(418.6) = 5.97; p < .0001), as was the number of tools (MCBI = 12.4, SD = 8.8, range = 1 to 33; MIBI=10.4, SD = 6.8, range = 1 to 33; t(469.9) = 2.85, p <.01). Participants in the CBI endorsed a higher number of strengths (MCBI = 10.5, SD = 5.6, range = 1 to 10) than those in the IBI (MIBI=8.7, SD = 2.0, range = 1 to 10; t(315.9) = 4.74; p <.0001).
When models revealed a significant group by time interaction (CBI: importance, help-seeking, readiness, confidence; IBI: confidence, intention), we used Pearson partial correlations to examine if counts of tools, benefits, strengths, and concerns were related to post-test levels of these psychological variables (controlling for pre-test values). For the CBI, the total number of benefits of change significantly correlated with post-test help-seeking intentions (r=.19, p<.01) and confidence (r=.13, p<.05). Number of tools selected was significantly associated with post-test importance of change (r=.16, p<.05) and help-seeking intentions (r= .15, p<.05). Counts of perceived benefits and tools were not related to readiness, tools were not related to confidence, and benefits were not related to importance. Concerns were not related to any post-test measure for the CBI. For the IBI, counts of both benefits and tools were significantly correlated with post-test confidence and intentions (rs range from .19 - .26, ps < .01). Counts of strengths were not significantly related to any post-test measures for either the CBI or the IBI group.
4. Discussion
These results provide insight into using technology for BIs in urban EDs, which allows for early identification of and intervention in a vulnerable population that may not receive help until significant drug use problems emerge. Regarding feasibility, most patients found the BIs helpful and the computers easy to use. Results show initial support for the efficacy of these BIs in changing psychological constructs that may be related to future behavior change. Compared to EUC participants, those in the IBI showed significant increases in self-efficacy and intentions to change drug use and condom use intentions with regular partners, but did not change in importance, readiness, or help-seeking for drug use or HIV-related variables. More consistent outcomes were found for the CBI relative to EUC, with post-test increases in importance, readiness, confidence, and help-seeking related to drug use, and condom use intentions with regular partners. These findings are promising, but more research is needed targeting behavioral outcomes for the BIs.
While the CBI appears to have affected more psychological pre-cursors of drug use behavior change compared to the IBI, direct comparisons of these two BIs revealed only one significant difference (the IBI group’s confidence increased more than the CBI group’s, although the CBI group did increase from pre- to post-test). In general, this early support for the CBI is consistent with other studies finding favorable effects of computer-based interventions for substance use (Blow et al., 2006; Neumann et al., 2006; Ondersma et al., 2007). Although a recent meta-analysis of college student studies found therapist-delivered alcohol BIs superior to computer BIs (Carey et al., 2012) and some computer alcohol BIs in primary care have not produced favorable effects (Butler, Chiauzzi, Bromberg, Budman & Buonio; 2003; Cucciare et al., 2013), pending behavioral outcome data, our results suggest that the CBI may be relevant and effective with the population of interest – drug using adults in an urban ED. Although the effect sizes reported in our results were small, this is relatively consistent with effect sizes reported for behavioral outcomes of alcohol BIs (Havard, Shakeshaft, & Sanson-Fisher, 2008).
Few effects were observed for the BIs on psychological pre-cursors of changing HIV risk behaviors with group by time interactions occurring only for condom use intentions with regular partners. Perhaps this is not surprising because the BIs primarily targeted substance use and only briefly addressed HIV risk. However, we only measured HIV testing intentions, condom use intentions, and importance of condom use, and did not assess confidence or readiness. It is possible that the BIs impacted these other constructs, but they may have also had little effect on these cognitions. Because HIV risk behaviors among drug users can occur as a result of acute intoxication, it may be that fewer HIV risk behaviors will result from any reduced drug use due to the BIs. Few ED-based BIs have targeted multiple risk behaviors; those that have report positive reductions in some, but not all outcomes (e.g., Walton et al., 2010). Thus, research is needed to determine if BIs for multiple risk behaviors are more or less effective than BIs for a single behavior, or if related risk behaviors change when not directly targeted in the BI (as in Magill et al., 2009). Along those lines, future research on BI outcomes should examine potential moderators of effectiveness, such as substance use severity, in order to refine screening protocols or allow for tailoring in order to target those mostly likely to benefit from the different BIs.
Further, these CBI and IBI methods differ in terms of efficiency, cost, training, and supervision needs and research is needed to determine if one delivery mode is superior. Although attempts were made to design the two BIs to have similar content, with different delivery mechanisms, in practice, unique aspects of the IBI and CBI were identified. First, it appears as if participants indicated more responses in the CBI for the number of benefits, tools related to changing drug use, and strengths than in the IBI. These data may reflect the fact that although the CBI had audio and the virtual health counselor “talked” to participants, this virtual counselor was not able to engage in a real conversation and the participant “talked” with the virtual counselor by clicking response options. Instead, in the IBI, the intervener engaged in discussion of benefits and tools, potentially resulting in fewer items selected. In this regard, it may be that the CBI lead to broader coverage of topics with the IBI resulting in fewer topics covered, but potentially at greater depth. Alternatively, the CBI was standardized whereas in the IBI, although prompted by the computer to cover certain topics, the therapist had greater leeway in deciding what was most important to cover within the framework of the motivational interviewing-based BI.
From a clinical perspective, this study’s findings provide insight into salient elements of BIs that may influence behavioral change. Specifically, participants who selected more benefits of change and tools during the BI were more likely to report increases in pre-cursors of behavior change, regardless of pre-test levels. Consistent with conceptualizations regarding the “causal chain” of MI-consistent therapist behaviors eliciting client speech that is associated with behavioral outcomes (Moyers & Martin, 2006; Moyers et al., 2007), benefits and tools may be important to elicit during BIs. Strengths were not associated with changes in these psychological outcomes and although only measured in the CBI, we did not find that “number of concerns” was related to any post-test measures. At first this appears counterintuitive with theory and research showing that BIs may be more effective among those with greater problem severity (e.g., Field & Caetano, 2010; Guth et al., 2008), potentially because this allows the therapist to elicit change talk to avoid these concerns in the future. It may be that more concerns do not directly influence changes in the constructs measured in this study (e.g., importance, readiness, self-efficacy); instead, such concerns may have indirect effects on other BI components, assisting in eliciting positive aspects of change (e.g., benefits). As previous research also supports the notion that within-session client processes are associated with increased abstinence (Armhein, Miller, Yahne, Palmer, & Fulcher, 2003; Martin, Christopher, Houck, & Moyers, 2011), future research should determine the predictive nature of these BI elements on behavioral outcomes for both therapist- and computer-delivered BIs.
Several limitations require acknowledgement. Data came from a single ED and findings require replication in other samples of varied backgrounds (e.g., race, socio-economic status). Although response rates were acceptable for this type of research, findings may not generalize to those who were missed or refused participation. Data presented are from an ongoing RCT; thus, behavioral outcomes and intervention fidelity data are not yet available. We conducted several statistical tests and corrections for multiple comparisons among a priori, inter-related outcomes may be overly conservative (Pocock, 1997) and are not typically applied in the literature on ED BI outcomes, yet it is possible that our results were influenced by Type I error. While prior work supports the relationship between psychological pre-cursors of behavior change and behavioral outcomes (Ondersma, Grekin, & Svikis, 2011), it is also noted that ratings on these items may be subject to floor or ceiling effects. Future work will examine the efficacy of the BIs on behavioral outcomes (drug use, HIV risk behaviors). Nonetheless, given the paucity of data on SBIRT for drug use, particularly BIs that use technology for screening, within-session data capture, and intervention delivery, these data are novel. Further, examining the BI process, in terms of the relationship between specific BI elements and post-test changes in psychological constructs theoretically related to behavior change, makes an important contribution to the literature.
These results highlight issues related to BI implementation in the ED that should be addressed. For example, refusals may pose challenges to integrating BIs into clinical care when patients are not compensated. At 21%, the refusal rate by eligible patients was similar to or less than other ED SBIRTs (e.g., Academic ED SBIRT Collaborative, 2007; Bernstein et al., 2012; Mello et al., 2008; Monti et al., 2007; Woolard et al., 2012); however that nearly 1 in 5 refused suggests the need to continue developing novel delivery systems or alternative means of reaching these patients, perhaps by further integrating technology to capture attention and ensure privacy. Second, although the CBI was mostly read to patients, screens with data captures were not read aloud and may have been less impactful to those with a lower reading level. Thus, in order to have to broadest possible impact, it will be important to consider relevant patient characteristics unique to the local setting when designing BIs as well as how to apply these approaches to reach those who could benefit from a BI, but may be excluded in traditional research. Finally, implementing therapist BIs can be affected by therapist drift, turnover, and/or experience. Drift may be reduced with computer-guided BIs in order to increase therapist fidelity, though this remains a question for future research. Further, research examining individual therapist effects on client outcomes may help identify key components of therapist training.
In conclusion, our findings suggest that computer-delivered or computer-guided BIs may be useful in translating SBIRT to medical settings for screening, standardization of therapy fidelity, and delivery of BIs with tailored content. Although the effect of these BIs on behavioral outcomes is a question for future study, the effects on precursors of behavior change compared to usual care is promising. Future research on the implementation of the BIs should evaluate which factors of the ED setting and patient population influence whether a fully computerized or a therapist-guided-by-computer BI is most effective. Further, for research purposes, computers can assist in efficient screening and capturing data during BIs to identify the key ingredients of such therapies to potentially maximize outcomes. Our data suggest that technology enhanced computerized BIs for the ED setting, in particular, are promising and well-received by patients.
Supplementary Material
Supplemental Figure 2. Significant interactions from pre- to post-test for psychological precursors of behavior change in computer brief intervention (CBI) and intervener brief intervention (IBI) groups.
Acknowledgments
The authors wish to acknowledge the support of our research by the patients and staff at Hurley Medical Center in Flint, Michigan. Financial support for this study was provided by the National Institute on Drug Abuse DA026029. Dr. Bonar’s work on this manuscript was supported by an NIAAA T32 training grant (#AA007477) awarded to the University of Michigan Addiction Research Center. NIDA, NIAAA, and the University of Michigan had no further role in the study design; in the collection, analysis, and interpretation of data; in the writing of this report; or in the decision to submit this manuscript for publication. A limited portion of this manuscript has been accepted for a poster presentation at the annual meeting of the Association of Behavioral and Cognitive Therapies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Academic ED SBIRT Collaborative The impact of screening, brief intervention, and referral to treatment on Emergency Department patients’ alcohol use. Annals of Emergency Medicine. 2007;50:699–710. doi: 10.1016/j.annemergmed.2007.06.486. [DOI] [PubMed] [Google Scholar]
- Armhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology. 2002;71:862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Bazargan-Hejazi S, Bing E, Bazargan M, Der-Martirosian C, Hardin E, Bernstein J, et al. Evaluation of a brief intervention in an inner-city emergency department. Annals of Emergency Medicine. 2005;46:67–76. doi: 10.1016/j.annemergmed.2004.10.014. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Levenson S. Project ASSERT: An ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Annals of Emergency Medicine. 1997;30:181–189. doi: 10.1016/s0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Ashong D, Heeren T, Winter M, Bliss C, Madico G, et al. The impact of a brief motivational intervention on unprotected sex and sex while high among drug-positive emergency department patients who receive STI/HIV VC/T and drug treatment referral as standard of care. AIDS and Behavior. 2012;16:1203–1216. doi: 10.1007/s10461-012-0134-0. [DOI] [PubMed] [Google Scholar]
- Bernstein J, Bernstein E, Tassiopoulos K, Heeren T, Levenson S, Hingson R. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug and Alcohol Dependence. 2005;77:49–59. doi: 10.1016/j.drugalcdep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Academic Emergency Medicine. 2009;16:1174–1185. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Christensen DR, Marsch LA. A review of computer-based interventiosn sued in the assessment, treatment, and research of drug addiction. Substance Use & Misuse. 2011;26:4–9. doi: 10.3109/10826084.2011.521066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blow FC, Barry KL, Walton MA, Maio RF, Chermack ST, Bingham CR, et al. The efficacy of two brief intervention strategies among injured, at-risk drinkers in the emergency department: impact of tailored messaging and brief advice. Journal of Studies on Alcohol. 2006;67:568–578. doi: 10.15288/jsa.2006.67.568. [DOI] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Murray R, Cunningham RM, Chermack ST, Barry KL, et al. Intervention attendance among ED patients with alcohol and drug use disorders. Journal of Studies on Alcohol and Drugs. 2010;71:713–719. doi: 10.15288/jsad.2010.71.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LE, Burton R, Hixon B, Kakade M, Bhagalia P, Vick C, et al. Factors influencing emergency department preference for access to healthcare. Western Journal of Emergency Medicine. 2012;8:410–415. doi: 10.5811/westjem.2011.11.6820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: Trajectories, risk factors, and event-level relationships. Developmental Psychology. 2012;48:1429–1442. doi: 10.1037/a0027547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler SF, Chiauzzi E, Bromberg JI, Budman SH, Buono DP. Computer-assisted screening and intervention for alcohol problems in primary care. Journal of Technology in Human Services. 2003;21:1–19. [Google Scholar]
- Cacciola JS, Alterman AI, McLellan AT, Lin YT, Lynch KG. Initial evidence for the reliability and validity of a “lite” version of the Addiction Severity Index. Drug and Alcohol Dependence. 2007;87:297–302. doi: 10.1016/j.drugalcdep.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ. A vision of the next generation of behavioral therapies research in the addictions. Addiction. 2011;102:850–862. doi: 10.1111/j.1360-0443.2007.01798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998-2010. Clinical Psychology Review. 2012;32:690–703. doi: 10.1016/j.cpr.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ. Changes in substance use associated with emergency room and primary care services utilization in the United States general population: 1995-2000. The American Journal of Drug and Alcohol Abuse. 2003;29:789–802. doi: 10.1081/ada-120026261. [DOI] [PubMed] [Google Scholar]
- Cucciare MA, Weingardt KR, Ghaus S, Boden MT, Frayne SM. A randomized controlled trial of a web-delivered brief alcohol intervention in veterans affairs primary care. Journal of Studies on Alcohol and Drugs. 2013;74:428–436. doi: 10.15288/jsad.2013.74.428. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Bernstein SL, Walton M, Broderick K, Vaca FE, Woolard R, et al. Alcohol, tobacco, and other drugs: Future directions for screening and intervention in the emergency department. Academic Emergency Medicine. 2009;16:1078–1088. doi: 10.1111/j.1553-2712.2009.00552.x. [DOI] [PubMed] [Google Scholar]
- Daeppen JB, Bertholet N, Gmel G, Gaume J. Communication during brief intervention, intention to change, and outcome. Substance Abuse. 2007;28:43–51. doi: 10.1300/J465v28n03_05. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behaviour among intravenous drug users. AIDS. 1991;5:181–185. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Fontdevila J, Gilbert L, Voisin D, Richman BL, Pitchell P. HIV risks of men in methadone maintenance treatment programs who abuse their intimate partners: A forgotten issue. Journal of Substance Abuse. 2001;13:29–43. doi: 10.1016/s0899-3289(01)00068-2. [DOI] [PubMed] [Google Scholar]
- Federal Bureau of Investigation Crime in the United States, 2006. 2007 Retrieved from: http://www2.fbi.gov/ucr/cius2006/index.html.
- Field CA, Baird J, Saitz R, Caetano R, Monti PM. The mixed evidence for brief intervention in emergency departments, trauma care centers, and inpatient hospital settings: What should we do? Alcoholism: Clinical and Experimental Research. 2010;34:2004–2010. doi: 10.1111/j.1530-0277.2010.01297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field CA, Caetano R. The effective of brief intervention among injured patients with alcohol dependence: Who benefits from brief interventions? Drug and Alcohol Dependence. 2010;111:13–20. doi: 10.1016/j.drugalcdep.2009.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher RA. Statistical Methods for Research Workers. Hafner Publishing Company; Davient, CT: 1970. [Google Scholar]
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: Long-term efficacy and benefit-cost analysis. Alcoholism: Clinical and Experimental Research. 2002;26:36–43. [PubMed] [Google Scholar]
- Forsythe M, Lee GA. The evidence for implementing alcohols screening and intervention in the emergency department – time to act. International Emergency Nursing. 2012;20:167–172. doi: 10.1016/j.ienj.2011.09.006. [DOI] [PubMed] [Google Scholar]
- Fuda KK, Immekus R. Frequent users of Massachusetts emergency departments: A statewide analysis. Annals of Emergency Medicine. 2006;48:9–16. doi: 10.1016/j.annemergmed.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Fussell HE, Rieckmann TR, Quick MB. Medicaid reimbursement for screening and brief intervention for substance misuse. Psychiatric Services. 2011;62:306–309. doi: 10.1176/ps.62.3.pss6203_0306. [DOI] [PubMed] [Google Scholar]
- Gentilello LM, Ebel BE, Wickizer TM, Salkever DS, Rivara FP. Alcohol interventions for trauma patients treated in emergency departments and hospitals. Annals of Surgery. 2005;241:541–550. doi: 10.1097/01.sla.0000157133.80396.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geurts J, Palatnick W, Strome T, Weldon E. Frequent users of an inner-city emergency department. Canadian Journal of Emergency Medicine. 2012;14:306–313. doi: 10.2310/8000.2012.120670. [DOI] [PubMed] [Google Scholar]
- Guth S, Lindberg SA, Badger GJ, Thomas CS, Rose GL, Helzer JE. Brief intervention in alcohol-dependent versus nondependent individuals. Journal of Studies on Alcohol and Drugs. 2008;69:243–250. doi: 10.15288/jsad.2008.69.243. [DOI] [PubMed] [Google Scholar]
- Harris MJ, Patel B, Bowen S. Primary care access and its relationship with emergency department utilization: An observational, cross-sectional, ecological study. British Journal of General Practice. 2011;61:e787–793. doi: 10.3399/bjgp11X613124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: Interventions reduce alcohol-related injuries. Addiction. 2008;103:368–376. doi: 10.1111/j.1360-0443.2007.02072.x. [DOI] [PubMed] [Google Scholar]
- Hesse M. The readiness ruler as a measure of readiness to change poly-drug use in drug abusers. Harm Reduction Journal. 2006;3:3. doi: 10.1186/1477-7517-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, et al. Validation of the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) Addiction. 2008;103:1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Strecher VJ, Glassman B. One size does not fit all: The case for tailoring print materials. Annals of Behavioral Medicine. 1999;21:276–283. doi: 10.1007/BF02895958. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Quinlan T, Schiffman JE, Earleywine ME. Performance of alcohol and safer sex change rulers compared with readiness to change questionnaires. Psychology of Addictive Behaviors. 2005;19:112–115. doi: 10.1037/0893-164X.19.1.112. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Woolard RF, Nirenberg TD, Minugh AP, Becker B, Clifford PR, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- Lustria MLA, Cortese J, Noar SM, Glueckauf RL. Computer-tailored health interventions delivered over the web: Review and analysis of key components. Patient Education and Counseling. 2009;74:156–173. doi: 10.1016/j.pec.2008.08.023. [DOI] [PubMed] [Google Scholar]
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug and Alcohol Dependence. 2009;99:280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Barnett NP, Apodaca TR, Rohsenow DJ, Monti PM. The role of marijuana use in a brief motivational intervention with young adult drinkers treated in an Emergency Department. Journal of Studies on Alcohol and Drugs. 2009;70:409–413. doi: 10.15288/jsad.2009.70.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch LA, Bickel WK. Efficacy of computer-based HIV/AIDS education for injection drug users. American Journal of Health Behavior. 2004;28:316–327. doi: 10.5993/ajhb.28.4.3. [DOI] [PubMed] [Google Scholar]
- Martin T, Christopher PJ, Houck JM, Moyers TB. The structure of client language and drinking outcomes in Project MATCH. Psychology of Addictive Behaviors. 2011;25:439–445. doi: 10.1037/a0023129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Cacciola JS, Carise D, Coyne TH. The Addiction Severity Index – Lite – Clinical Factors version (ASI-Lite-CF) The Treatment Research Institute; Philadelphia, PA: 1999. [Google Scholar]
- Mello MJ, Longabaugh R, Baird J, Nirenberg T, Woolard R. DIAL: A telephone brief intervention for high-risk alcohol use with injured emergency department patients. Annals of Emergency Medicine. 2008;51:755–764. doi: 10.1016/j.annemergmed.2007.11.034. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. Guilford Press; New York: 2002. [Google Scholar]
- Moineddin R, Meaney C, Agha M, Zagorski B, Glazier RH. Modeling factors influencing the demand for emergency department services in Ontario: A comparison of methods. BMC Emergency Medicine. 2011;11:13. doi: 10.1186/1471-227X-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti PM, Barnett NP, Colby SM, Gwaltney CJ, Spirito A, Rohsenow DJ, et al. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction. 2007;102:1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- Moore BA, Fazzino T, Garnet B, Cutter CJ, Barry DT. Computer-based interventions for drug use disorders: A systematic review. Journal of Substance Abuse Treatment. 2011;40:215–223. doi: 10.1016/j.jsat.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions. Journal of Substance Abuse Treatment. 2006;30:245–251. doi: 10.1016/j.jsat.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan JS, Armhein PC. Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcoholism: Clinical and Experimental Research. 2007;31(S3):41S–47S. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- Murphy MK, Bijur PE, Rosenbloom D, Bernstein SL, Gallagher EJ. Feasibility of a computer-assisted alcohol SBIRT program in an urban emergency department: Patient and research staff perspectives. Addiction Science & Clinical Practice. 2013;8:2. doi: 10.1186/1940-0640-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Barnett NP, Rohsenow DJ, Colby SM, Monti PM. Cost-effectiveness of a motivational intervention for alcohol-involved youth in a hospital emergency department. Journal of Studies on Alcohol and Drugs. 2010;71:384–394. doi: 10.15288/jsad.2010.71.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann T, Neuner B, Weiss-Gerlach E, Tonnesen H, Gentilello LM, Wernecke KD, et al. The effect of computerized tailored brief advice on at-risk drinking in subcritically injured trauma patients. The Journal of Trauma. 2006;61:805–814. doi: 10.1097/01.ta.0000196399.29893.52. [DOI] [PubMed] [Google Scholar]
- Nilsen P. Brief alcohol intervention – where to from here? Challenges remain for research and practice. Addiction. 2010;105:954–959. doi: 10.1111/j.1360-0443.2009.02779.x. [DOI] [PubMed] [Google Scholar]
- Nilsen P, Baird J, Mello MJ, Nirenberg T, Woolard R, Bendtsen P, et al. A systematic review of emergency care brief alcohol interventions of injury patients. Journal of Substance Abuse Treatment. 2008;35:184–201. doi: 10.1016/j.jsat.2007.09.008. [DOI] [PubMed] [Google Scholar]
- Office of Applied Studies . 2010 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2009. [Google Scholar]
- Ondersma SJ, Chase SK, Svikis DS, Schuster CR. Computer-based brief motivational intervention for perinatal drug use. Journal of Substance Abuse Treatment. 2005;28:305–312. doi: 10.1016/j.jsat.2005.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma SJ, Svikis DS, Schuster CR. Computer-based brief intervention: A randomized trial with postpartum women. American Journal of Preventive Medicine. 2007;32:231–238. doi: 10.1016/j.amepre.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma SJ, Grekin ER, Svikis D. The potential for technology in brief interventions for substance use, and during-session prediction of computer-delivered brief intervention response. Substance Use & Misuse. 2011;46:77–86. doi: 10.3109/10826084.2011.521372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peduzzi P, Henderson W, Hartigan P, Lavori P. Analysis of randomized controlled trials. Epidemiologic Review. 2002;24:26–38. doi: 10.1093/epirev/24.1.26. [DOI] [PubMed] [Google Scholar]
- Peralta L, Deeds BG, Hipszer S, Ghalib K. Barriers and facilitators to adolescent HIV testing. AIDS Patient Care and STDs. 2007;21:400–407. doi: 10.1089/apc.2006.0112. [DOI] [PubMed] [Google Scholar]
- Petry N. Reliability of drug users’ self-reported HIV risk behaviors using a brief, 11-item scale. Substance Use and Misuse. 2001;36:1731–1747. doi: 10.1081/ja-100107576. [DOI] [PubMed] [Google Scholar]
- Pocock SJ. Clinical trials with multiple outcomes: A statistical perspective on their design, analysis, and interpretation. Controlled Clinical Trials. 1997;18:530–545. doi: 10.1016/s0197-2456(97)00008-1. [DOI] [PubMed] [Google Scholar]
- Rosenthal R, Rosnow RL. Essentials of Behavioral Research: Methods and Data Analysis. 3rd Edition McGraw-Hill; New York: 2008. [Google Scholar]
- Prochaska JO, DiClemente CC. Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy: Theory, Research, and Practice. 1982;19:276–288. [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. American Psychologist. 1992;47:1102–1113. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Smith GR, Burnam MA, Mosley CL, Hollenberg JA, Mancino M, Grimes W. Reliability and validity of the substance abuse outcomes module. Psychiatric Services. 2006;57:1452–1460. doi: 10.1176/ps.2006.57.10.1452. [DOI] [PubMed] [Google Scholar]
- Smith GR, Kramer T, Babor T, Burnam MA, Mosley CL, Rost K, et al. Substance Abuse Outcomes Module – user’s manual. University of Arkansas for Medical Sciences; Little Rock, AR: 1996. [Google Scholar]
- Sohler NL, Wong MD, Cunningham WE, Cabral H, Drainoni M, Cunningham CO. Type and pattern of illicit drug use and access to health care services for HIV-infected people. AIDS Patient Care and STDs. 2007;21:S68–S-76. doi: 10.1089/apc.2007.9985. [DOI] [PubMed] [Google Scholar]
- Stein MD, Anderson B, Charuvusta A, Friedmann PD. Alcohol use and sexual risk taking among hazardously drinking drug injectors who attend needle exchange. Alcoholism: Clinical and Experimental Research. 2001;25:1487–1493. [PubMed] [Google Scholar]
- Trinks A, Festin K, Bendtsen P, Nilsen P. Reach and effectiveness of a computer-based alcohol intervention in a Swedish emergency room. International Emergency Nursing. 2010;18:138–146. doi: 10.1016/j.ienj.2009.08.004. [DOI] [PubMed] [Google Scholar]
- Trinks A, Festin K, Bendtsen P, Nilsen P. What makes emergency department patients reduce their alcohol consumption? – A computer-based intervention study in Sweden. International Emergency Nursing. 2013;21:3–9. doi: 10.1016/j.ienj.2011.11.004. [DOI] [PubMed] [Google Scholar]
- Tross S, Hanner J, Hu M, Pavlicova M, Campbell A, Nunes EV. Substance use and high risk sexual behaviors among women in psychosocial outpatient and methadone maintenance treatment programs. The American Journal of Drug and Alcohol Abuse. 2009;35:368–374. doi: 10.1080/00952990903108256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitale S, van de Mheen D. Illicit drug use and injuries: A review of emergency room studies. Drug and Alcohol Dependence. 2006;82:1–9. doi: 10.1016/j.drugalcdep.2005.08.017. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents. Journal of the American Medical Association. 2010;304:527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster BH, Bishaw A, U.S. Census Bureau . Income, earnings, and poverty: Data from the 2006 American Community Survey. Government Printing Office; Washington, DC: 2007. American Community Survey Reports, ACS-08. [Google Scholar]
- Woolard R, Baird J, Longabaugh R, Nirenberg T, Lee CS, Mello MJ, et al. Project reduce: Reducing alcohol and marijuana misuse: Effects of a brief intervention in the emergency department. Addictive Behaviors. 2013;38:1732–1739. doi: 10.1016/j.addbeh.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO ASSIST Working Group The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability, and feasibility. Addiction. 2002;97:1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Wu L, Ringwalt CL, Patkar AA, Hubbard RL, Blazer DG. Association of MDMA/ecstasy and other substance use with self-reported sexually transmitted diseases among college –aged adults: A national study. Public Health. 2009;123:557–564. doi: 10.1016/j.puhe.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 2. Significant interactions from pre- to post-test for psychological precursors of behavior change in computer brief intervention (CBI) and intervener brief intervention (IBI) groups.