Summary
Introduction
The aim of this study was to compare the results of classic laparoscopic, three-port and SILS cholecystectomy.
Materials and methods
We conducted a retrospective study of data collected between January 2010 and December 2012 pertaining to 159 selected patients with symptomatic gallstones. 57 underwent laparoscopic cholecystectomy, 51 three-port cholecystectomy and 48 SILS cholecystectomy. We then compared the groups with respect to mean operating time, intraoperative complications, postoperative pain, duration of hospitalization and final aesthetic result.
Results
The mean operating time was significantly higher in the SILS cholecystectomy group (93 minutes) than in the other two groups. There were no intraoperative complications. There were no significant differences in the duration of hospitalization among the three groups. Patients in the SILS cholecystectomy group reported significantly less pain 3, 6 and 12 hours after surgery. The aesthetic results at 1 and 6 months’ follow-up were also decidedly better.
Conclusions
On the basis of this study, SILS cholecystectomy is a feasible, safe procedure. In any case, it should be used in selected patients only and carried out by a dedicated team with strong experience in laparoscopy. The main advantages of this technique are a reduction in post-operative pain and improved aesthetic result, at the price, however, of its greater technical difficulty and longer operating times. Future studies are in any case necessary to evaluate any other benefits of this method.
Keywords: SILS cholecystectomy, Laparoscopic cholecystectomy, Laparoscopy
Introduction
The first laparoscopic cholecystectomy was carried out in 1987 in France by Philippe Mouret (1). The progressive evolution of the technique has led this procedure to become the gold standard in the treatment of symptomatic gallstones (2). As the technology improved, many surgeons began to reduce the number and size of the ports with the aim of achieving ever lower invasiveness, consequently reducing trauma and postoperative pain and improving the cosmetic results. There was thus a progression from conventional laparoscopic cholecystectomy (CLC) involving the use of 4 trocars to three-port cholecystectomy (3-port) and then minilaparoscopy, using 3–5 mm trocars (3–5). Since the 90s, the use of single incision laparoscopic surgery (SILS) cholecystectomy has further reduced the number of trocars (6).
Despite the continuous development of both the devices offered by the industry and the clinical applications, there still remain various concerns over the real benefits and safety of this new technique (7, 8). The various literature studies and meta-analyses have demonstrated that reducing the number of ports and the total length of the incisions significantly reduces post-operative pain, leading to shorter hospitalization times, reduced use of analgesics, earlier return to work, improved final aesthetic results and, thus, greater patient satisfaction (9).
With this background, we developed a retrospective study analyzing the data from our experience in the treatment of symptomatic gallstones. The data from each group were compared using χ2 test e Student’s t test with statistical significance (p) of < 0.05 and a 95% confidence interval.
Materials and methods
Study design
This retrospective study is based on the analysis of data collected between January 2010 and December 2012 at our teaching hospital. 156 non-consecutive patients with symptomatic gallstones diagnosed by abdominal ultrasound and/or CT scan were selected and scheduled for elective cholecystectomy. The exclusion criteria were acute cholecystitis (diagnosed clinically, by laboratory tests and/or by x-ray), pregnancy, Mirizzi’s syndrome, history of acute biliary pancreatitis, BMI > 35 Kg/m2, American Society of Anesthesiologists (ASA) classification > 3, previous upper laparotomy and previous upper GI surgery (10, 11). Umbilical hernia and choledocholithiasis were not exclusion criteria. In the latter case, we carry out sequential treatment with endoscopic retrograde cholangiopancreatogram (ERCP) and lavage of the main bile ducts, and these patients too can be treated using 3-port or SILS cholecystectomy. However, CLC and 3-port patients in whom abdominal drainage had been used were excluded from the study. This was because no abdominal drainage was used in patients treated by SILS cholecystectomy, so it would have represented a confounding factor in the evaluation of post-operative pain. All procedures were carried out by the same surgical team whose expertise in laparoscopy amounted to over 500 classic laparoscopic cholecystectomies.
Surgical technique
Patients were placed in a slight reverse Trendelenburg position (the classic French position). The first surgeon stands between the patient’s legs with the second surgeon to their right and the assistant to their left. We induced pneumoperitoneum to 12 mmHg in all cases, using Hasson’s technique via trans-umbilical open laparoscopy (12, 13). For CLC, we used two 10 mm trocars, one in the navel (optical trocar) and one in the left hypochondrium, along the mid-clavicular line (operator trocar). A 5 mm port was placed in the right hand side for traction of the infundibulum and another 5 mm subxiphoid incision was made for retraction of the gallbladder fundus and liver (14, 15).
In the 3-port group, we used a single 10 mm trocar in the navel and two other 5 mm trocars. No subxiphoid trocar was positioned and no sutures were used to suspend the gallbladder fundus (16).
In the SILS group, we always used the open technique with a 2–2.5 cm trans-umbilical incision. The procedures were carried out using two difference devices: TriPort-Laparoscopic Instrument Port® (Olympus™) and OCTO™Port (DalimSurgNET™)
The instruments used for the SILS are the same as for CLC. We used a 5- or 10-mm optical trocar as required, but always at 30°. A monopolar hook was always used for the dissection. The use of classic instruments resulted in a contained cost increase, affected only by the type of port used (17, 18).
At the end of the procedure the umbilical fascia was sutured with individual stitches. We use fast-resorbing intradermal sutures to achieve the best esthetic result (Fig. 1).
Fig. 1.
Umbilical scar with intradermal suture.
Soon after surgery we administered analgesic Acetaminophen 500 mg IV and Ketorolac 30 mg IM; latter was also used for any necessary postoperative analgesia.
Postoperative course
The patients began taking small quantities of fluid a few hours after surgery and could eat the following day. All patients were discharged with the prescription of low molecular weight heparin (LMWH) for prevention of thromboembolic disease.
Results
The 159 patients selected for this study between January 2010 and December 2012 were divided into three groups: 57 undergoing CLC, 51 three-port cholecystectomy (3-port) and 48 SILS cholecystectomy (SILS). The patient characteristics for the three groups were similar (Table 1).
Table 1.
PATIENT CHARACTERISTICS.
| Parameter | CLC (n = 57) | 3-port (n = 51) | SILS (n =48) |
|---|---|---|---|
| Sex (F:M) | 39:18 | 40:11 | 41:7 |
| Age (years)a | 48.5 (18–82) | 46 (18–62) | 31 (18–48) |
| BMI (Kg/m2)a | 24.5 (19.3–35) | 24 (18–34.8) | 22.2 (17–24) |
| ASA status (1:2:3) | 14:32:11 | 39:9:3 | 27:17:4 |
Values are reported as mean (range).
CLC conventional laparoscopic cholecystectomy, 3-port three-port cholecystectomy, SILS SILS cholecystectomy.
Surgical data (Table 2)
Table 2.
SURGICAL DATA.
| Parameter | CLC (n = 57) | 3-port (n = 51) | SILS (n =48) |
|---|---|---|---|
| Surgery time | 52.8 (range 15–140) | 57.5 (range 30–90) | 93 (range 75–110) |
| Blood loss | NS | NS | NS |
| Other procedures | |||
| ERCP | 5 (8.8%) | 2 (3.9%) | - |
| Umbilical hernia repair | 8 (14%) | 7 (13.7%) | 6 (12.5%) |
| Appendectomy | - | 4 (7.8%) | 2 (4.2%) |
| Pelvic endometriosis | - | - | 1 |
| Conversion | 0 | 0 | 0 |
| Adverse events | |||
| Bile leak | 0 | 0 | 0 |
| Wound infection | 2 (3.6%) | 1 (1.96%) | 0 |
| Seroma | 0 | 0 | 0 |
| Port hernia | 0 | 0 | 0 |
The mean operating time for the SILS group was 93 ± 13.5 min, significantly longer than for the other two groups. There was no statistically significant difference between the CLC group (52.8 ± 21.5 min) and the 3-port group (57.5 ± 14.4 min). In reality, the longer operating time for SILS cholecystectomy was at least partly due to the necessary learning curve, and later procedures with this technique took progressively less time, reaching a minimum of 75 minutes. Furthermore, an appendectomy was also performed in two patients in this group (Figure 2) while another underwent consensual treatment of an area of pelvic endometriosis (19). A unilateral inguinal hernia repair was carried out after SILS cholecystectomy in a male patient, although he was excluded from the study (20).
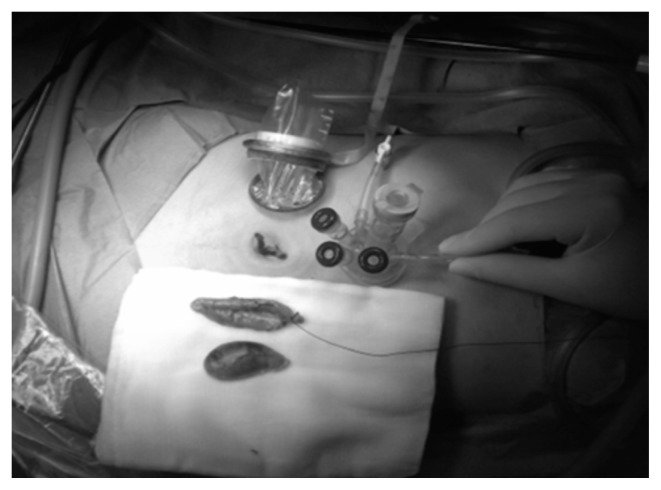
Fig. 2.
Single-access cholecystectomy and appendectomy.
There was no significant blood loss in any of the three groups and no abdominal drains were positioned. (In fact CLC patients for whom an abdominal drain was used were excluded from the study, in order to avoid interference with the evaluation of postoperative pain). An additional subxiphoid trocar was positioned in two patients (4.2%) in the SILS group, due to difficulty in exposing Calot’s triangle. Stitches for the suspension of the fundus or infundibulum of the gallbladder were not used in any case (21). None of the SILS procedures were converted to classic laparoscopy. No patients in any group were converted to open surgery. Calot’s triangle was dissected using the critical view of safety approach. Intraoperative cholangiography was not necessary in any patient (22), but ERCP and lavage of the main bile duct had been carried out 24–48 hours previously in 5 CLC patients and 2 3-port patients to treat choledocholithiasis. There were no intraoperative complications. 3 patients developed an infection of the umbilical wound (2 in the CLC group and 1 in the 3-port group; none in the SILS group). These complications were treated and resolved conservatively. No trocar hernias were found on follow-up.
Postoperative outcomes (Table 3)
Table 3.
POSTOPERATIVE OUTCOMES.
| Parameter | CLC (n = 57) | 3-port (n = 51) | SILS (n =48) |
|---|---|---|---|
| Pain location | |||
| Umbilical port | 35 (61%) | 33 (64.7%) | 41 (85.4%) |
| Right subcostal | 17 (29.8%) | 15 (29.4%) | 7 (14.6%) |
| Other site | 5 (8.7%) | 3 (5.9%) | 0 |
| Cosmetic results | |||
| After 1 month | 7.1 | 7.4 | 8.5 |
| After 6 months | 8.5 | 8.6 | 9.5 |
Postoperative pain was assessed with a visual analog scale (VAS) 3, 6, 12 and 24 hours after surgery. The SILS group patients reported significantly less pain at 3, 6 and 12 hours compared with the other two groups (P ≤ 0.05). The difference at 24 hours was not statistically significant. The most frequent site for pain was the navel. Some patients, distributed evenly across the three groups, reported right subcostal pain and pain in the corresponding scapula. This symptom can be reduced by use of local intraperitoneal anesthetic (23), but this procedure was not used in patients in this study. Less frequently, postoperative pain was reported in other trocar ports in the right side, left hypochondrium and subxiphoid area.
Postoperative analgesic use was generally less in the SILS and 3-port groups, although the differences were not statistically significant. Oral fluids were offered after a mean of 6.7 hours in the CLC group, 6.3 hours in the 3-port groups and 6.1 hours in the SILS group, thus the three groups were comparable. Duration of hospitalization was also comparable, with a mean duration of 1.8 days (range 1–2.5). The esthetic results and patient satisfaction were evaluated using the Patient and Observer Scar Assessment Scale (POSAS) (24). The esthetic results were significantly better in the SILS group than in the CLC group at 1 and 6 months (P ≤ 0.05).
Discussion
From its first use (25), single incision laparoscopic cholecystectomy has evolved progressively, encouraged by increasing patient – and thus industrial – interest. So, in the first cases of single-access cholecystectomy many authors used the “Swiss cheese technique” with the introduction of various trocars through the same umbilical incision. In parallel the industries developed several “multiport” specialized trocars. This new method simplified the surgical approach and probably also improved the final esthetic result.
The endpoint in this retrospective study was to demonstrate the feasibility and safety of SILS cholecystectomy as an alternative to multiport techniques in selected patients (26, 27). All procedures were carried out in selected patients by surgeons expert in laparoscopy. In contrast to the initial results of laparoscopic cholecystectomy (28), the SILS approach proved safe: there were no intraoperative complications in any patients. Moreover, its feasibility was demonstrated by the fact that there were no conversions to classic laparoscopy and additional subxiphoid trocars were needed in just two cases. The greatest surgical difficulty is undoubtedly the isolation of Calot’s triangle.
The benefits of SILS cholecystectomy are, above all, the improved postoperative outcome, with less postoperative pain and consequently reduced use of analgesics. The duration of hospitalization, in contrast, was comparable for all three groups. The other great benefit of SILS cholecystectomy is the final cosmetic result, the reason that this technique is preferred by the young and by women. The positioning of the trocar using Hasson’s technique via trans-umbilical open laparoscopy is essential to achieve this. After surgery, there is in fact a single, invisible scar, leading this technique to be called “no-scar” surgery.
The drawbacks include the longer operating time, although this is partly due to the individual surgeon’s learning curve (29, 30). Furthermore, while we did not experience any major intraoperative complications, there are numerous literature reports of iatrogenic injuries to the main bile duct, possibly requiring conversion to open surgery and significantly affecting the patient’s postoperative outcome. Other authors have pointed out the higher cost, deriving from the pre-curved or jointed instruments (often single-use) used for single-incision surgery. In our caseload, the increased cost was contained by the use of traditional laparoscopic instruments.
Given these considerations, we also analyzed the results of the 3-port technique, positioning a single 10-mm trans-umbilical trocar and two 5-mm trocars in the right side and left hypochondrium. This approach maintains the benefits of the classic laparoscopic triangulation but achieves excellent esthetic results while significantly reducing the operating time in comparison with SILS. It can also be used, with suitable adjustments, in more complex or emergency situations.
Conclusions
This retrospective analysis of cases at our hospital revealed that SILS cholecystectomy carried out by expert surgeons in selected patients is feasible and safe. The longer operating time is compensated by the improved outcome, with significantly reduced postoperative pain and consequently reduced use of analgesics. Costs can be contained by the use of traditional laparoscopic instruments. The improved results obtained with this technique are the main reason for its increasing use and popularity with patients. However, further studies are necessary to establish the method’s true safety and perhaps expand the number of conditions for which it is indicated.
References
- 1.Kaiser AM, Corman ML. History of laparoscopy. Surg Oncol Clin N Am. 2001;10(3):483–492. [PubMed] [Google Scholar]
- 2.Agresta F, Ansaloni L, Baiocchi GL, Bergamini C, Campanile FC, Carlucci M, Cocorullo G, et al. Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Società Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Società Italiana di Chirurgia (SIC), Società Italiana di Chirurgia d’Urgenza e del Trauma (SICUT), Società Italiana di Chirurgia nell’Ospedalità Privata (SICOP), and the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2012 Aug;26(8):2134–64. doi: 10.1007/s00464-012-2331-3. [DOI] [PubMed] [Google Scholar]
- 3.Sun S, Yang K, Gao M, He X, Tian J, Ma B. Three-port versus four-port laparoscopic cholecystectomy: meta-analysis of randomized clinical trials. World J Surg. 2009;33(9):1904–8. doi: 10.1007/s00268-009-0108-1. [DOI] [PubMed] [Google Scholar]
- 4.Cerci C, Tarhan OR, Barut I, Bülbül M. Three-port versus four-port laparoscopic cholecystectomy. Hepatogastroenterology. 2007;54(73):15–6. [PubMed] [Google Scholar]
- 5.de Carvalho LF, Fierens K, Kint M. Mini-laparoscopic versus conventional laparoscopic cholecystectomy: a randomized controlled trial. J Laparoendosc Adv Surg Tech A. 2013;23(2):109–16. doi: 10.1089/lap.2012.0349. [DOI] [PubMed] [Google Scholar]
- 6.Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. [PubMed] [Google Scholar]
- 7.Lirici MM, Califano AD, Angelini P, Corcione F. Laparo-endoscopic single site cholecystectomy versus standard laparoscopic cholecystectomy: results of a pilot randomized trial. Am J Surg. 2011;202(1):45–52. doi: 10.1016/j.amjsurg.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 8.Pucher PH, Sodergren MH, Singh P, Darzi A, Parakseva P. Have we learned from lessons of the past? A systematic review of training for single incision laparoscopic surgery. Surg Endosc. 2013;27(5):1478–84. doi: 10.1007/s00464-012-2632-6. [DOI] [PubMed] [Google Scholar]
- 9.Arezzo A, Scozzari G, Famiglietti F, Passera R, Morino M. Is single-incision laparoscopic cholecystectomy safe? Results of a systematic review and meta-analysis. Surg Endosc. 2013;27(7):2293–304. doi: 10.1007/s00464-012-2763-9. [DOI] [PubMed] [Google Scholar]
- 10.Abd Ellatif ME, Askar WA, Abbas AE, Noaman N, Negm A, El-Morsy G, El Nakeeb A, Magdy A, Amin M. Quality-of-life measures after single-access versus conventional laparoscopic cholecystectomy: a prospective randomized study. Surg Endosc. 2013;27(6):1896–906. doi: 10.1007/s00464-012-2625-5. [DOI] [PubMed] [Google Scholar]
- 11.Novo G, Corrado E, Tortorici E, Novo A, Agrusa A, Saladino V, Marturana I, Lentini R, Ferrandes M, Visconti C, Massenti F, D’Arienzo M, Vitale F, Gulotta G, Novo S. Cardiac risk stratification in elective non-cardiac surgery: role of NT-proBNP. Int Angiol. 2011;30(3):242–6. [PubMed] [Google Scholar]
- 12.Agrusa A, Romano G, Di Buono G, Dafnomili A, Gulotta G. Laparoscopic approach in abdominal emergencies: a 5-year experience at a single center. G Chir. 2012;33(11–12):400–3. [PubMed] [Google Scholar]
- 13.Cucinella G, Rotolo S, Calagna G, Granese R, Agrusa A, Perino A. Laparoscopic management of interstitial pregnancy: the “purse-string” technique. Acta Obstet Gynecol Scand. 2012;91(8):996–9. doi: 10.1111/j.1600-0412.2012.01437.x. [DOI] [PubMed] [Google Scholar]
- 14.Tuveri M, Borsezio V, Calò PG, Medas F, Tuveri A, Nicolosi A. Laparoscopic cholecystectomy in the obese: results with the traditional and fundus-first technique. J Laparoendosc Adv Surg Tech A. 2009;19(6):735–40. doi: 10.1089/lap.2008.0301. [DOI] [PubMed] [Google Scholar]
- 15.Romano G, Agrusa A, Frazzetta G, De Vita G, Chianetta D, Di Buono G, Amato G, Gulotta G. Laparoscopic drainage of liver abscess: case report and literature review. G Chir. 2013;34(5–6):180–2. doi: 10.11138/gchir/2013.34.5.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tebala GD. Three-port laparoscopic suture-suspension cholecystectomy. Chir Ital. 2008;60(2):285–9. [PubMed] [Google Scholar]
- 17.Ceci F, Di Grazia C, Cipriani B, Nicodemi S, Corelli S, Pecchia M, Martellucci A, Costantino A, Stefanelli F, Salvadori C, Napoleoni A, Parisella M, Spaziani E, Stagnitti F. Cholecystectomy by single incision laparoscopic surgery (SILS): early experience and technique standardization. G Chir. 2012;33(8–9):280–4. [PubMed] [Google Scholar]
- 18.Cantore F, Colombo EM, Giuseppe MD, Biondi A, Rausei S, Dionigi G, Rovera F, Boni L, Dionigi R. Single access cholecystectomy using standard laparoscopic instruments. Updates Surg. 2011;63(1):31–4. doi: 10.1007/s13304-011-0046-y. [DOI] [PubMed] [Google Scholar]
- 19.Granese R, Candiani M, Perino A, Venezia R, Cucinella G. Bladder endometriosis: laparoscopic treatment and follow-up. Eur J Obstet Gynecol Reprod Biol. 2008;140(1):114–7. doi: 10.1016/j.ejogrb.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 20.Amato G, Ober E, Romano G, Salamone G, Agrusa A, Gulotta G, Bussani R. Nerve degeneration in inguinal hernia specimens. Hernia. 2011;15(1):53–8. doi: 10.1007/s10029-010-0735-3. [DOI] [PubMed] [Google Scholar]
- 21.Pan MX, Jiang ZS, Cheng Y, Xu XP, Zhang Z, Qin JS, He GL, Xu TC, Zhou CJ, Liu HY, Gao Y. Single-incision vs three-port laparoscopic cholecystectomy: prospective randomized study. World J Gastroenterol. 2013;19(3):394–8. doi: 10.3748/wjg.v19.i3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bresadola V, Intini S, Terrosu G, Baccarani U, Marcellino MG, Sistu M, Scanavacca F, Bresadola F. Intraoperative cholangiography in laparoscopic cholecystectomy during residency in general surgery. Surg Endosc. 2001;15(8):812–5. doi: 10.1007/s004640090006. [DOI] [PubMed] [Google Scholar]
- 23.Roberts KJ, Gilmour J, Pande R, Nightingale P, Tan LC, Khan S. Efficacy of intraperitoneal local anaesthetic techniques during laparoscopic cholecystectomy. Surg Endosc. 2011;25(11):3698–705. doi: 10.1007/s00464-011-1757-3. [DOI] [PubMed] [Google Scholar]
- 24.Draaijers LJ, Tempelman FR, Botman YA, Tuinebreijer WE, Middelkoop E, Kreis RW, van Zuijlen PP. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113(7):1960–5. doi: 10.1097/01.prs.0000122207.28773.56. [DOI] [PubMed] [Google Scholar]
- 25.Pelosi MA, Pelosi MA. Laparoscopic appendectomy using a single umbilical puncture (minilaparoscopy) J Reprod Med. 1992;37:588–594. [PubMed] [Google Scholar]
- 26.Karim MA, Ahmed J, Mansour M, Ali A. Single incision vs. conventional multiport laparoscopic cholecystectomy: a comparison of two approaches. Int J Surg. 2012;10(7):368–72. doi: 10.1016/j.ijsu.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 27.Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P. Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc. 2012;26(5):1205–13. doi: 10.1007/s00464-011-2051-0. [DOI] [PubMed] [Google Scholar]
- 28.Parmeggiani D, Cimmino G, Cerbone D, Avenia N, Ruggero R, Gubitosi A, Docimo G, Mordente S, Misso C, Parmeggiani U. Biliary tract injuries during laparoscopic cholecystectomy: three case reports and literature review. G Chir. 2010;31(1–2):16–9. [PubMed] [Google Scholar]
- 29.Hong TH, You YK, Lee Kh. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009;23:1393–1397. doi: 10.1007/s00464-008-0252-y. [DOI] [PubMed] [Google Scholar]
- 30.Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011;98(12):1695–702. doi: 10.1002/bjs.7689. [DOI] [PubMed] [Google Scholar]