Summary
Myositis Ossificans (MO) is an unusual pathological entity still largely unknown, characterized by dystrophic calcification leading to heterotopic ossification of intramuscular connective tissue. The masticatory muscles are exceptionally involved.
Four distinct types of myositis ossificans have been described: MO Progressiva, which is a genetic disorder involving several muscular groups; MO Circumscripta, limited to a single muscle and generally due to calcification of an intramuscular haematoma following severe trauma and progressive ossification; MO Pseudo-malignant limited to soft tissue and not associated to any trauma; MO associated to paraplegia.
A case of circumscribed myositis ossificans of the masseter muscle in a 62 years-old woma is reportedn.
Keywords: Myositis ossificans, Circumscribed Myositis Ossificans, Masseter muscle
Introduction
Myositis ossificans (MO) is a non neoplastic lesion, localised, self limiting, characterised by a more or less wide bone production from interstitial connective tissue. It involves muscles and only rarely tendons, layers, periostum and subcutaneous fat tissue (1).
MO includes four distinct clinical pathologies:
Circumscribed or traumatic MO indicates bone metaplasia in a muscle, when in the clinical history there is a report of a trauma, in which the intramuscular haemorrhage causes a bone metaplasia. It can be due also to repeated microtraumas and/or inflammatory disease. It generally involves the lateral pterygoid muscle (2) and medial pterygoid muscle (3) and only rarely the masseter muscle.
MO Progressiva also called fibrodysplasia ossificans progressiva, is an autosomal dominant disease of the pediatric age, more frequent in females; characterized by symmetric skeletal malformations of the hands and feet such as microdattilia, syndattilia, polidattilia, agenesia of one or more feet phalanx; moreover it presents a progressive heterotopic ossification of soft tissues (4).
Pseudomalignant MO is a myositis without history of trauma (5). These patients present a soft tissue mass with intermittent pain and localized erythema. More frequent localization is around the pelvis, greater trochanter, femur, and knee.
MO associated with paraplegia; the prognosis is poor. Costello e Brown (6) indicate as primitive event the atrophy and tissue degeneration.
MO is considered as predisposing factor for Temporo-Mandibular Joint ankilosys.
Case report
A 62-years-old, Caucasian female was observed at our Department of Maxillofacial surgery because of an opening mouth reduction. The patient was affected by ipertension since 12 years and underwent colon resection two years before for colorectal carcinoma. Two months before our observation an incidental orthopantomography was performed that showed an iperdense area of the right upper jaw (Fig. 1). Clinically there was a flattening of the upper right vestibular fornix, with a modest reduction of the mouth opening for the presence in 18–16 area of a hard, smooth mass. The Computed Tomography (CT) scan showed a grossly round mass, 3 cm in the larger diameter, fixed to the posterior-lower part of right malar bone, with inhomogeneous bone density (Figs. 2a,b). This lesion was in close proximity to Bichat fat and masseter muscle, and presented inside calcific microformations compatible with tooth bud.
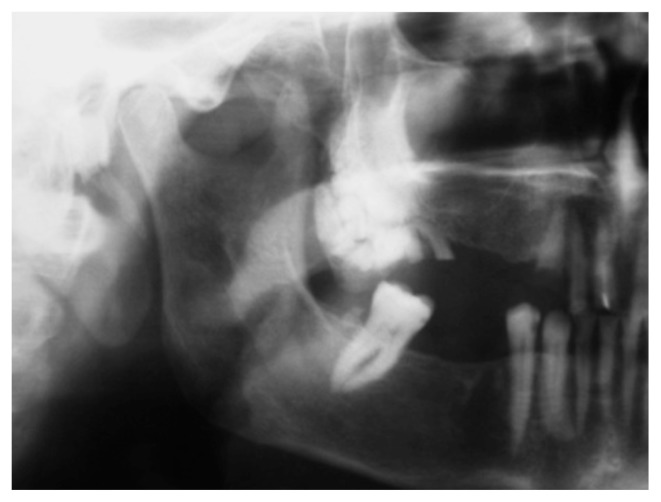
Fig. 1.
Preoperative orthopantomography showing an iperdense area of the right upper jaw.
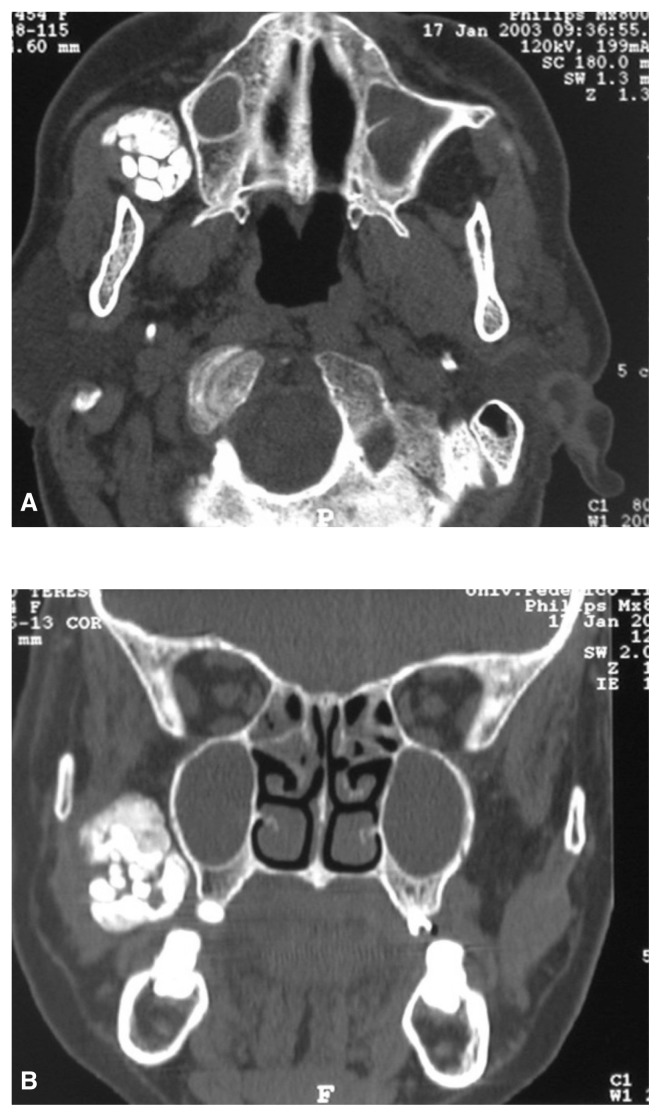
Fig. 2.
Preoperative CT scans in axial (A) and coronal (B) view showing an inhomogeneous bone density mass fixed to the posterior-lower part of right malar bone.
Under general anaesthesia the mass was removed by a trans-oral approach (Fig. 3).
Fig. 3.
Intraoperative picture showing the trans-oral approach for mass removal.
The lesion measured 3 cm in greatest diameter, and was well circumscribed. The cut surface was white and soft in the centre, and yellow-grey with a rough granular surface at the periphery (Fig. 4). The tumour was routinely fixed in 10% buffered formaldehyde and embedded in paraffin; 5μ thick sections were cut and stained with haematoxylin-eosin.
Fig. 4.
The cut surface was white and soft in the centre, yellow-grey with a rough granular surface at the periphery.
Microscopically, the lesion showed lamellar bone together with intersperses fat cells, fibrous tissue, and thin-walled vascular spaces. The results suggested the diagnosis of MO.
The patient was followed-up every three months for two years with orthopantomography and CT scan twice a year (Fig. 5). After surgery there was an improvement in opening of the jaw that was observed constant also during following controls.
Fig. 5.
Two year postoperative TC scan on coronal view showing the complete mass removal.
Discussion
Myositis ossificans, contrary to the name, is not an inflammatory condition and in some case there is no evidence of bone or muscle in the lesion. Gilmer e Anderson (7) consider myositis ossificans a benign condition with eterotopic formation of bone in the muscular tissue.
The anamnesis and the clinical examination in patients with reduced mouth opening and/or recently operated in the oral cavity is fundamental for the diagnosis. Radiologic findings (Computed Tomography and Magnetic Resonance) allow to define the extension and, in many cases, the nature of the lesion with characteristic pattern according the degree of development (8, 9).
Histology is very important in diagnosis identifying the characteristic zonal arrangement of the lesion and in order to avoid incorrect diagnosis it is indicated to remove the entire lesion.
Firstly Gotte (10) and then Wakely (11) described the characteristic zonal arrangement:
a central zone characterised by the presence of an inflammatory infiltrate with macrophages, lymphocytes, polymorphic fibroblasts and angiogenesis phenomena, muscular fibres with atrophic or degenerative appearance;
an intermediate zone with a more regular appearance with collagen trabeculae and immature, osteoid cells;
a peripheral zone made by calcified osteoid with areas of cartilagineous metaplasia and lamellar mature bone separated from the surrounding muscle by connective tissue without inflammatory infiltrate.
Therapy is based on surgical complete removal of the lesion followed by a prudent rehabilitation with minimal trauma starting as soon as possible. Nowadays endoscopy is widely used in maxillofacial surgery, and it can be used for removal of such lesions (12–15).
Sometimes a medical treatment is still indicated with prolonged assumption of Etidronic Acid (16) and myorelaxing drugs. After surgery we recommend cold therapy in order to minimize swallow and post oper
References
- 1.Ackerman LV. Extra-osseous localized non-neoplastic bone and cartilage formation (so-called myositis ossificants) J Bone Joint Surg Am. 1958;49:279–98. [PubMed] [Google Scholar]
- 2.Abidin HA, Prabhu SR. Traumatic miositis ossificants of lateral pterygoid muscle. J Oral Med. 1984;39:54–6. [PubMed] [Google Scholar]
- 3.Narang R, Dixon RA., Jr Miositis ossificans: medial pterygoid muscle a case report. Br J Oral. 1974;12:229–39. doi: 10.1016/0007-117x(74)90130-9. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan FS, Tabas JA, Zasloff MA. Fibrodysplasia ossificans progressiva: a clue from the fly. Calcif Tissue Int. 1990;47:117–25. doi: 10.1007/BF02555995. [DOI] [PubMed] [Google Scholar]
- 5.Heinrich SD, Zembo MM, MacEwen GD. Pseudomalignant myositis ossificans. Orthopedics. 1989;12:599–602. doi: 10.3928/0147-7447-19890401-15. [DOI] [PubMed] [Google Scholar]
- 6.Costello FV, Brown A. Myositis ossificans complicatine anterior poliomyelitis. J Bone Joint Surg Br. 1951;33:594–7. doi: 10.1302/0301-620X.33B4.594. [DOI] [PubMed] [Google Scholar]
- 7.Gilmer WS, Anderson LD. Reactions of soft somatic tissue which may progress to bone formation: circumscribed (traumatic) myositis ossificans. South Med J. 1959;52:1432–48. [Google Scholar]
- 8.Shorkhoda A, Armin AR, Bis KG, Makris J, Irwin RB, Shetty AN. MR imaging of myositis ossificans: variable patterns at different stages. J Magn Reson Imaging. 1995;5(3):287–92. doi: 10.1002/jmri.1880050312. [DOI] [PubMed] [Google Scholar]
- 9.Cvitanic O, Sedlak J. Acute myositis ossificans. Skeletal Radiol. 1995;24(2):139–41. doi: 10.1007/BF00198078. [DOI] [PubMed] [Google Scholar]
- 10.Gotte P, Cortelazzi R, Politi M, Sonetti F, Pelosi G. Miosite ossificante traumatica del muscolo pterigoideo mediale. Minerva Stomatol. 1988;37(10):757–62. [PubMed] [Google Scholar]
- 11.Wakely PE, jr , Almeida M, Frable WJ. Fine-needle aspiration biopsy cytology of myositis ossificans. Mod Pathol. 1994;7(1):23–5. [PubMed] [Google Scholar]
- 12.Belli E, Rendine G, Mazzone N. Concha bullosa: endoscopic treatment. J Craniofac Surg. 2009;20(4):1165–8. doi: 10.1097/SCS.0b013e3181acdbb1. [DOI] [PubMed] [Google Scholar]
- 13.Belli E, Longo B, Balestra FB, Matteini C. Could transcranial endoscopy represent an alternative to craniotomy in skull base surgery. J Craniofacial Surg. 2005;16(1):155–8. doi: 10.1097/00001665-200501000-00031. [DOI] [PubMed] [Google Scholar]
- 14.Castelnuovo PG, Belli E, Bignami M, Battaglia P, Sberze F, Tomei G. Endoscopic nasal and anterior craniotomy resection for malignant nasoethmoid tumors involving the anterior skull base. Skull Base. 2006;16(1):15–8. doi: 10.1055/s-2005-922095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Belli E, Matteini C, D’Andrea GC, Mazzone N. Navigator system guided endoscopic intraoral approach for remodelling of mandibular condyle in Garré syndrome. J Craniofac Surg. 2007;18(6):1410–5. doi: 10.1097/scs.0b013e3181534b26. Erratum in: J Craniofac Surg 2008;19(1):293. [DOI] [PubMed] [Google Scholar]
- 16.Oz BB, Boneh A. Myositis Ossificans Progressiva: a 10-year follow-up on a patient treated with etigronate disodium. Acta Paediatr. 1994;83(12):1332–4. doi: 10.1111/j.1651-2227.1994.tb13032.x. [DOI] [PubMed] [Google Scholar]
- 17.Belli E, Rendine G, Mazzone N. Cold therapy in maxillofacial surgery. J Craniofac Surg. 2009;20(3):878–80. doi: 10.1097/SCS.0b013e3181a14d3d. [DOI] [PubMed] [Google Scholar]