Abstract
Background
Few studies have assessed the temporal association between homelessness and injection drug use, and injection-related risk behavior.
Methods
Among a cohort of 1,405 current and former injection drug users in follow-up from 2005–2009, we used random intercept models to assess the temporal association between homelessness and subsequent injection drug use, and to determine whether the association between homelessness and sustained injection drug use among active injectors differed from the association between homelessness and relapse among those who stopped injecting. We also assessed the association between homelessness and subsequent injection-related risk behavior among participants who injected drugs consecutively across two visits. Homelessness was categorized by duration: none, <1 month, and ≥1 month.
Results
Homelessness was reported on at least one occasion by 532 (38%) participants. The relationship between homelessness and subsequent injection drug use was different for active injectors and those who stopped injecting. Among those who stopped injecting, homelessness was associated with relapse [<1 month: AOR=1.67, 95% CI (1.01, 2.74); ≥1 month: AOR=1.34 95% CI (0.77, 2.33)]. Among active injectors, homelessness was not associated with sustained injection drug use [<1 month: AOR=1.03, 95% CI (0.71, 1.49); ≥1 month: AOR=0.81 95% CI (0.56, 1.17)]. Among those injecting drugs across two consecutive visits, homelessness ≥1 month was associated with subsequent injection-related risk behavior [AOR=1.61, 95% CI (1.06, 2.45)].
Conclusion
Homelessness appears to be associated with relapse and injection-related risk behavior. Strengthening policies and interventions that prevent homelessness may reduce injection drug use and injection-related risk behaviors.
Keywords: unstable housing, homelessness, relapse, injection drug use, injection-related risk behavior, random intercept models
1. INTRODUCTION
Injection drug use remains a significant public health issue, as a risk factor for premature mortality, HIV, and hepatitis C virus (HCV) infection (Armstrong et al., 2006; The Centers for Disease Control and Prevention, 2009; Mehta et al., 2011; Vlahov et al., 2008). Injection drug use also poses a considerable burden on society due to the costs of drug-related crime, loss of productivity (Alexandre and French, 2004), and other negative social implications (Wood et al., 2001). Approximately 1 million persons in the United States are estimated to have injected drugs, with the highest prevalence reported in Fresno, California, and Baltimore, Maryland (Brady et al., 2008). According to recent estimates, Baltimore ranked first in the country in per capita prevalence of injection drug use, with an estimated 336 injection drug users (IDUs) per 10,000 population aged 15–64 reported (Brady et al., 2008).
Homelessness has consistently been associated with injection drug use (Aidala et al., 2005; Bourgois, 1998; Briggs et al., 2009; Roy et al., 2010; Song et al., 2000) and a number of factors associated with homelessness, including poverty (Mizuno et al., 2009), inequitable housing policies (Dickson-Gomez et al., 2007), incarceration (Mizuno et al., 2009), social networks (Davey-Rothwell et al., 2011), and poor mental health (Aidala et al., 2005) have also been associated with injection drug use (Bohnert et al., 2009; Genberg et al., 2011a; Mackesy-Amiti et al., 2012; Mehta et al., 2012). However, while injection drug use and homelessness commonly co-occur, few studies have characterized the temporal relationship between homelessness and injection drug use (Aidala et al., 2005; Mehta et al., 2012; Shah et al., 2006). It is also unclear whether homelessness can trigger relapse into injection drug use among those who have stopped injecting, and increased risk behavior among those actively injecting.
There is some evidence to suggest a temporal link between homelessness and injection drug use. In prior studies, homelessness has been associated with initiation of injection drug use (Crofts et al., 1996; Roy et al., 2010) and has been negatively associated with utilization of mental health care and drug treatment (Appel et al., 2004; Muir-Cochrane et al., 2006), factors which tend to be associated with reduced drug use (The Substance Abuse and Mental Health Services Administration, 2005). Homelessness has also been found to mediate the relationship between adverse life events, such as childhood abuse and incarceration, and drug use (Chen et al., 2004; Krishnan et al., 2012). Additionally, drug use has been reported to be a coping strategy for untreated mental illness and uncomfortable living conditions experienced during homelessness (Williams and Stickley, 2011; Wright et al., 2005).
A temporal link between homelessness and injection-related risk behaviors has also been suggested (Aidala et al., 2005; Bourgois, 1998; Briggs et al., 2009; Small et al., 2006; Werb et al., 2008). Failure to cook or filter drugs, and unsafe disposal of drug paraphernalia has been reported to occur among homeless persons who rush injection to prevent confiscation and arrest by police (Small et al., 2006; Werb et al., 2008). Additionally, paraphernalia sharing, which has been associated with transmission of blood borne diseases (The Centers for Disease Control and Prevention, 2001; Sulkowski et al., 2002), has been reported as a consequence of confiscation of sterile syringes by police (Werb et al., 2008) and lack of income among homeless persons (Bourgois, 1998).
Despite the extensive literature supporting a link between homelessness, injection drug use, and injection-related risk behavior, gaps remain. The temporality of these relationships has not been assessed in a number of prior studies. Further, we and others have demonstrated that IDUs exhibit complex patterns of drug injection throughout their lifetime (Genberg et al., 2011b) and frequently transition in and out of injection drug use (Galai et al., 2003). Homelessness may be an important trigger for relapse among those who have stopped injecting, and for injection-related risk behavior among those who are persistent injectors. Prior studies have also not distinguished between those homeless for shorter vs. longer periods of time, which may differently impact risk.
The objectives of this study were: (1) to assess the temporal relationship between homelessness and injection drug use among current and former IDUs, (2) to assess whether homelessness differently impacts sustained injection drug use among active injectors vs. relapse among those who have stopped injecting; and (3) to assess the temporal relationship between homelessness and injection-related risk behavior among persistent injectors.
2. METHODS
2.1. Ethics Statement
All participants provided informed consent. The study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
2.2. Study Sample
The rationale and methods of the AIDS Linked to the Intravenous Experience (ALIVE) have been described (Vlahov et al., 1991). Briefly, a community-based sample of 2921 current and former IDUs in Baltimore was recruited between 1988 and 1989 through street outreach. Participants were eligible to participate in the initial recruitment period if they were 18 years of age or older and reported injection drug use within the past 11 years. Additionally, HIV positive participants had to be AIDS-free at enrollment to be eligible. To account for deaths and losses to follow-up, a total of 1510 participants were enrolled across four additional phases of recruitment (1994–1995, 1998, 2000, and 2005–2008); eligibility criteria were similar across waves. In the ALIVE cohort, mortality has ranged from 3–5% per year and loss to follow-up has ranged from 5–7% per year among surviving participants.
For this analysis, we included participants from all recruitment waves that attended at least two study visits after 2005 (n=1422), when the study questionnaire was modified to include additional questions on homelessness. These participants contributed a total of 7096 visits. We excluded visits with a gap greater than two years relative to the previous visit (n=48), and visits missing data on covariates of interest (n=388). The final study sample included 1405 participants who contributed 6660 visits. The median number of visits per person was 4 (IQR: 3–6 visits), and the median time between visits was 183 days (IQR: 181–192 days).
2.3. Data Collection
Follow-up visits for ALIVE occur semi-annually. At each visit, participants complete surveys and laboratory testing. Clinical information is ascertained by trained interviewers. Information on behavior, life events, and health-related outcomes is captured using audio-computer assisted self-interview (ACASI; Macalino et al., 2002).
The primary outcome for this analysis was injection drug use, defined as self-reported injection of heroin, cocaine, speedball, and/or any other drug not prescribed by a health care provider within the last six months. Injection drug use was treated as dichotomous, with no reported injection as the reference category. A secondary outcome was injection-related risk behavior, defined as report of at least one of the following in the past six months: needle sharing, cotton sharing, and shooting gallery attendance. The primary exposure was homelessness, defined as self-reported homelessness, or residence in a shelter, park, abandoned building, bus/train station, or on the street, for at least one night in the past six months. Duration of homelessness is captured as a categorical variable: <1 week, ≥1 week but <1 month, ≥1 month but <6 months, and ≥6 months. The association between homelessness and injection drug use was similar in the first two categories and in the latter two categories. Accordingly, homelessness was categorized into three categories for analysis: none, <1 month, and ≥ 1 month.
Covariates were selected a priori based upon prior studies that have identified correlates of homelessness, injection drug use, and injection-related risk behavior (Aidala et al., 2005; Celentano et al., 1991; Galai et al., 2003; Genberg et al., 2011a; Golub et al., 2007; Latkin et al., 1995; Mehta et al., 2012; Milloy et al., 2008; Shah et al., 2006; Tobin et al., 2010). Covariates were dichotomized as yes or no, unless otherwise stated. The following covariates were fixed at the first visit: gender, race (black vs. non-black), and age (categories: <35, 35–54, ≥55). Covariates treated as time-varying included: HIV status (positive vs. negative), current employment, depressive symptoms in the last week (CES-D (Radloff, 1977) cut-off score of 23), and self-reported diagnoses or treatment by a health care provider, for depression, manic depression, anxiety, or schizophrenia. Additional time-varying factors measured in the last six months included: suicidal ideation, legal income ($5000 USD vs. less), incarceration (≥1 week vs. less), frequency of injection (daily vs. less), crack use, needle and cotton sharing, shooting gallery attendance, methadone maintenance, detoxification, trading sex for money, drugs, shelter or food, and sex with an IDU partner. Last, prior history of homelessness, defined as having at least one prior episode of homelessness, was included in analysis.
2.4 Statistical Analysis
Characteristics of participants at the first visit were compared across strata of homelessness at the first visit using chi-square tests for categorical variables and Kruskal–Wallis tests for continuous variables. Logistic regression was used to assess temporal associations between homelessness and injection drug use, and injection-related risk behavior, at the next visit. Random intercepts (Diggle et al., 2002) were applied to the logistic regression model to adjust for repeated measures among individuals over time, and to condition on individual baseline propensity for subsequent injection drug use and subsequent injection-related risk behavior. Homelessness and other time-varying covariates were lagged one visit to ensure temporality between these factors and subsequent injection drug use, and subsequent injection-related risk behavior (e.g., homelessness and other covariates were measured at time t−1 and subsequent injection drug use and subsequent injection-related risk behavior were measured at time t).
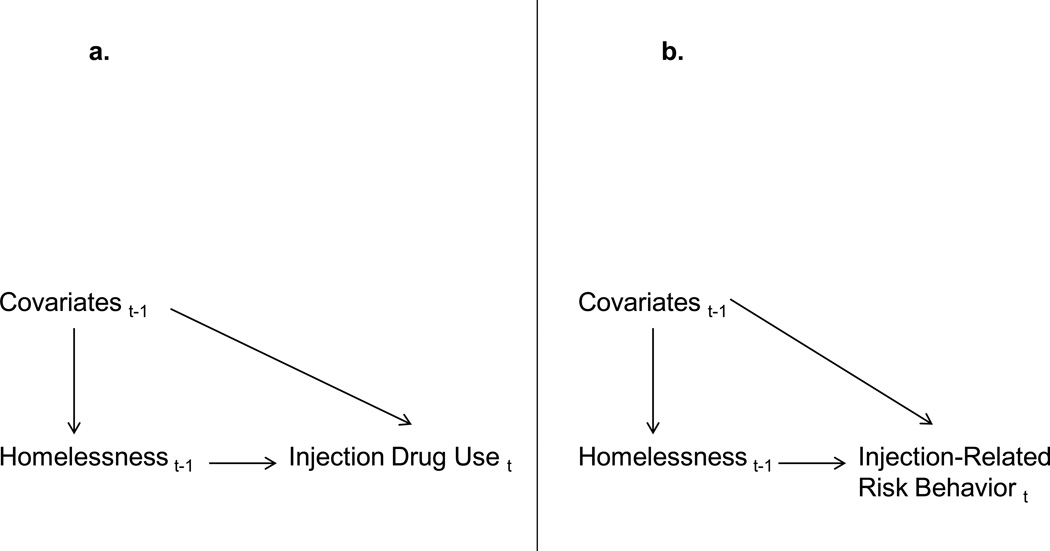
The unadjusted and adjusted associations between homelessness and subsequent injection drug use, and subsequent injection-related risk behavior, were assessed in four models. Model 1 assessed the association between homelessness and subsequent injection drug use among all observations (combined model). Because it has been suggested that correlates of relapse and sustained injection drug use may differ (Galai et al., 2003), we stratified the combined model according to whether injection drug use was reported or not reported at the lagged visit. Model 2 assessed the association between homelessness and relapse among visits when injection drug use was not reported at the lagged visit, and Model 3 assessed the association between homelessness and sustained injection drug use among visits when injection drug use was reported at the lagged visit. Model 4 assessed the association between homelessness and subsequent injection-related risk behavior when injection drug use was consecutively reported across two visits. Figure 1 illustrates the visits when homelessness, subsequent injection drug use, subsequent injection-related risk behavior, and covariates were measured in each model.
Figure 1.
a. Diagram illustrating when homelessness, injection drug use, and covariates are measured longitudinally at the lagged visit (t−1) and current visit (t) in models 1–3
Note: Model 1- All observations; Model 2- restricted to observations when injection drug use was not reported at visitt−1; Model 3- restricted to observations when injection drug use was reported at visitt−1
b. Diagram illustrating when homelessness, injection-related risk behavior, and covariates are measured longitudinally at the lagged visit (t−1) and current visit (t) in model 4
Note: Model 4- restricted to observations when injection drug use was reported at visitt−1 and visitt
Akaike’s Information Criteria (AIC) was used to evaluate model fit and establish a more parsimonious model that did not include all mental health variables. Model fit and parsimony improved with deletion of suicidal ideation and mental health conditions, excluding depressive symptoms as measured by CES-D. CES-D has been found to have good psychometric properties among persons with a history of drug use (Weissman et al., 1977). Additionally it may serve as a better marker of mental illness than diagnosed mental illness in this analysis, given the low levels of health care access in this population. Due to collinearity, frequency of injection, needle and cotton sharing, shooting gallery attendance, and non-fatal overdose were excluded from Model 1 and Model 2.
Interactions between homelessness and prior injection drug use, sex with an IDU partner and depressive symptoms were explored by including interaction terms in the combined adjusted model. Assessment of these interactions was based on literature supporting an association between injection drug use and having a drug using partner (Latkin et al., 1999), and poor mental health (Mackesy-Amiti et al., 2012). All analyses were performed using Stata (Version 12.1; StataCorp).
3. RESULTS
3.1. Study Participants
Of the 1405 participants, the majority were male (66%), black (87%), and between the ages of 35–54 (77%) at the first visit. The distribution of these characteristics was comparable to the distribution in the full ALIVE cohort. At the first visit, 347 (25%) participants reported homelessness. Among these participants, the duration of homelessness was reported to be < 1 week by 23% of participants, ≥ 1 week but < 1 month by 23% of participants, ≥ 1 month but < 6 months by 37% of participants and ≥ 6 months by 18% of participants. The primary location where participants slept differed by the duration of homelessness at the first visit. When homelessness was not reported, one’s own home was the most frequently reported location (61%), followed by the residence of a relative (22%) or significant other (7%). When homelessness <1 month was reported, a relative’s residence (27%), shelter (14%), or one’s own residence (11%) were most frequently reported. When homelessness ≥1 month was reported, a shelter (35%), the streets (18%), or friend’s residence (14%), were most frequently reported.
Characteristics by duration of homelessness at the first visit are shown in Table 1. Homelessness of any duration was common among those who were younger, non-black, unemployed, and who reported legal income less than $5000 USD, incarceration, daily injection, sex with an IDU partner, crack use, trading sex, not attending methadone maintenance, and attending a detoxification program (p<0.01 for all). Homelessness was also more common among those reporting depressive symptoms, suicidal ideation, and a clinical diagnosis or treatment for a mental health illness (p<0.0001 for all). In addition, residential instability, indicated by the number of moves reported in the last 6 months, injection-related risk behavior, and non-fatal overdose were higher among those reporting homelessness (p<0.0001 for all). Homelessness did not vary significantly by HIV status.
Table 1.
Characteristics of participants in the ALIVE study by homelessness strata at the first visit (n=1405)
| Total (N=1405) |
No Homelessness (N=1058) |
Homelessness <1month (N=158) |
Homelessness ≥1 month (N=189) |
P- value | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Demographic | |||||||||
| Age (years) | |||||||||
| 19–34 | 111 | 7.90 | 60 | 5.67 | 24 | 15.2 | 27 | 14.3 | <0.0001 |
| 35–54 | 1087 | 77.4 | 830 | 78.5 | 115 | 72.8 | 142 | 75.1 | |
| 55+ | 207 | 14.7 | 168 | 15.9 | 19 | 12.0 | 20 | 10.6 | |
| Female | 481 | 34.2 | 372 | 35.2 | 55 | 34.8 | 54 | 28.6 | 0.210 |
| Black | 1224 | 87.1 | 967 | 91.4 | 121 | 76.6 | 136 | 72.0 | <0.0001 |
| Legal income ≥$5000 USD | 311 | 22.2 | 267 | 25.2 | 24 | 15.2 | 20 | 10.6 | <0.0001 |
| Current employment | 310 | 22.1 | 274 | 25.9 | 14 | 8.86 | 22 | 11.6 | <0.0001 |
| Mean residential moves | 1401 | 2.32 | 1054 | 0.47 | 158 | 2.93 | 189 | 12.19 | <0.0001 |
| Mental health | |||||||||
| Depressive symptoms | 357 | 25.4 | 200 | 18.9 | 68 | 43.0 | 89 | 47.1 | <0.0001 |
| Depressiona | 341 | 24.3 | 221 | 21.0 | 55 | 35.0 | 65 | 34.4 | <0.0001 |
| Manic depressiona | 169 | 12.1 | 104 | 9.86 | 38 | 24.2 | 27 | 14.3 | <0.0001 |
| Anxietya | 172 | 12.3 | 103 | 9.75 | 36 | 22.9 | 33 | 17.5 | <0.0001 |
| Schizophreniaa | 175 | 12.5 | 109 | 10.3 | 37 | 23.4 | 29 | 15.3 | <0.0001 |
| Suicidal thoughts | 210 | 15.0 | 111 | 10.5 | 51 | 32.3 | 48 | 25.4 | <0.0001 |
| Suicide plans | 89 | 6.36 | 45 | 4.27 | 23 | 14.7 | 21 | 11.2 | <0.0001 |
| Suicide attempts | 38 | 2.71 | 19 | 1.80 | 9 | 5.73 | 10 | 5.32 | 0.001 |
| HIV | |||||||||
| HIV positive | 400 | 28.5 | 309 | 29.2 | 39 | 24.7 | 52 | 27.5 | 0.477 |
| Risk behavior and outcomes | |||||||||
| Frequency of injection | |||||||||
| None | 616 | 43.8 | 561 | 53.0 | 23 | 14.6 | 32 | 16.9 | <0.0001 |
| Less than daily | 333 | 12.7 | 232 | 21.9 | 43 | 27.2 | 58 | 30.7 | |
| Daily | 456 | 32.5 | 265 | 25.1 | 92 | 58.2 | 99 | 52.4 | |
| Incarcerated | 246 | 17.5 | 131 | 12.4 | 58 | 36.7 | 57 | 30.2 | <0.0001 |
| Sex with an IDU | 399 | 28.4 | 243 | 23.0 | 78 | 49.7 | 78 | 41.3 | <0.0001 |
| Trade sex for money /drugs | 151 | 10.8 | 64 | 6.05 | 48 | 30.4 | 39 | 20.6 | <0.0001 |
| Trade sex for food /shelter | 84 | 5.98 | 29 | 2.74 | 28 | 17.7 | 27 | 14.3 | <0.0001 |
| Crack use | 550 | 39.2 | 329 | 31.1 | 105 | 66.5 | 116 | 61.4 | <0.0001 |
| Methadone maintenance | 316 | 22.5 | 263 | 24.9 | 21 | 13.3 | 32 | 16.9 | 0.001 |
| Detoxification | 104 | 7.40 | 48 | 4.54 | 25 | 15.8 | 31 | 16.4 | <0.0001 |
| Needle sharingb | 335 | 42.5 | 152 | 30.6 | 81 | 60.0 | 102 | 65.0 | <0.0001 |
| Cotton sharingb | 314 | 39.8 | 150 | 30.2 | 76 | 56.3 | 88 | 56.1 | <0.0001 |
| Shooting gallery attendanceb | 136 | 17.2 | 48 | 9.66 | 35 | 25.9 | 53 | 33.8 | <0.0001 |
| Needle exchange program attendanceb | 223 | 28.3 | 136 | 27.5 | 37 | 27.4 | 50 | 31.9 | 0.551 |
| Non-fatal overdoseb | 162 | 20.5 | 70 | 14.1 | 40 | 29.6 | 52 | 33.1 | <0.0001 |
Note: All factors are measured in the past six months, excluding age, gender, race, and current employment measured at the time of the visit, and depressive symptoms measured in the past week. Depressive symptoms are measured using the Center for Epidemiologic Studies Depression Scale (CESD) with a cutoff score ≥ 23. Chi-squared test performed for all factors excluding residential moves (Kruskal-Wallis test)
Abbreviations: HIV, human immunodefiniciency virus; IDU, injection drug user
Self reported diagnosis or treatment for mental health illness by a health care provider
Among 789 participants reporting injection drug use
Across follow-up, homelessness was reported on at least one occasion by 532 (38%) participants, and 267 (50%) of these participants reported experiencing homelessness more than once.
3.2. Homelessness and Injection Drug Use
In unadjusted analysis, homelessness of any duration was significantly associated with subsequent injection drug use in the combined model (Table 2). After adjustment for other covariates in the combined model, homelessness <1 month and homelessness ≥ 1 month remained significantly associated with subsequent injection drug use [homelessness <1 month: AOR=1.74, 95% CI (1.27, 2.40); homelessness ≥1 month AOR=1.43, 95% CI (1.02, 2.01)]. Other covariates that were significantly associated with subsequent injection drug use in the adjusted combined model included younger age, non-black race, male gender, income less than $5000 USD, HIV negative serostatus, depressive symptoms, incarceration, sex with an IDU partner, and crack use. Past history of homelessness and trading sex were inversely associated with subsequent injection drug use.
Table 2.
Unadjusted and adjusted association between homelessness and subsequent injection drug use among 1405 active and former IDUs contributing 6660 visits from 2005–2009 (Model 1)
| Unadjusted OR | 95% CI | Adjusted ORa | 95% CI | |
|---|---|---|---|---|
| Homelessness | ||||
| No homelessness | Ref | Ref | ||
| < 1 Month | 2.46 | 1.79, 3.39 | 1.74 | 1.27, 2.40 |
| ≥ 1 Month | 2.27 | 1.62, 3.18 | 1.43 | 1.02, 2.01 |
| Past history of homelessness | 0.62 | 0.47, 0.81 | 0.76 | 0.58, 0.98 |
| Demographic | ||||
| Ages (years) | ||||
| 19–34 | Ref | Ref | ||
| 35–54 | 0.14 | 0.07, 0.27 | 0.38 | 0.19, 0.77 |
| 55+ | 0.05 | 0.02, 0.11 | 0.16 | 0.08, 0.35 |
| Female | 0.67 | 0.45, 1.00 | 0.50 | 0.35, 0.73 |
| Black | 0.12 | 0.06, 0.21 | 0.34 | 0.19, 0.62 |
| Legal income ≥$5000 USD | 0.62 | 0.49, 0.79 | 0.69 | 0.54, 0.87 |
| Current employment | 0.73 | 0.57, 0.93 | 0.87 | 0.67, 1.12 |
| Mental health | ||||
| Depressive symptoms | 2.40 | 1.90, 3.04 | 2.01 | 1.58, 2.54 |
| Depressionb | 1.12 | 0.87, 1.44 | ||
| Manic depressionb | 1.07 | 0.78, 1.46 | ||
| Anxietyb | 1.19 | 0.87, 1.63 | ||
| Schizophreniab | 1.01 | 0.74, 1.37 | ||
| Suicidal thoughts | 1.70 | 1.26, 2.30 | ||
| Suicide plans | 1.49 | 0.96, 2.33 | ||
| Suicide attempts | 2.17 | 1.04, 4.49 | ||
| HIV | ||||
| HIV positive | 0.54 | 0.35, 0.82 | 0.61 | 0.41, 0.88 |
| Risk Behavior | ||||
| Incarcerated | 1.83 | 1.39, 2.42 | 1.47 | 1.11, 1.94 |
| Sex with an IDU | 2.02 | 1.59, 2.57 | 1.84 | 1.42, 2.39 |
| Trade sex for drugs, money, food, or shelter | 1.00 | 0.90, 1.12 | 0.87 | 0.76, 0.99 |
| Crack use | 2.32 | 1.86, 2.90 | 1.83 | 1.46, 2.30 |
| Methadone maintenance | 0.82 | 0.62, 1.07 | 0.87 | 0.66, 1.14 |
| Detoxification | 1.25 | 0.88, 1.77 | 1.03 | 0.72, 1.46 |
Note: All factors are time-varying excluding age, gender, and race, which are measured at the first visit.
All time-varying factors are measured within the last six months, excluding current employment measured at the time of the visit, depressive symptoms measured in the past week. Time-varying factors are lagged one visit from when injection drug use is measured. Past homelessness is defined as any episode of homelessness prior to when homelessness is measured.
Abbreviations: CI, confidence interval; OR, odds ratio
Adjusted for baseline and time-varying covariates
Self reported diagnosis or treatment for mental health illness by a health care provider
Among visits when injection drug use was not reported in the prior six months (Table 3), homelessness <1 month was significantly associated with relapse into injection drug use in unadjusted analysis. The association between homelessness ≥1 month and relapse was of borderline statistical significance in unadjusted analysis. In adjusted analysis, homelessness <1 month remained significantly associated with relapse [AOR= 1.67, 95% CI (1.01, 2.74)]. Homelessness ≥1 month was also associated with relapse in adjusted analysis, but the association was not statistically significant [AOR=1.34; 95% CI (0.77, 2.33)]. Depressive symptoms, incarceration, sex with an IDU partner, and legal income less than $5000 USD were also significantly associated with relapse in the adjusted model.
Table 3.
Unadjusted and adjusted association between homelessness and relapse among 994 participants who reported no previous injection drug use across 3983 visits from 2005–2009 (Model 2)
| Unadjusted OR | 95% CI | Adjusted ORa | 95% CI | |
|---|---|---|---|---|
| Homelessness | ||||
| No homelessness | Ref | Ref | ||
| < 1 Month | 2.03 | 1.23, 3.35 | 1.67 | 1.01, 2.74 |
| ≥ 1 Month | 1.74 | 0.99, 3.05 | 1.34 | 0.77, 2.33 |
| Past history of homelessness | 1.23 | 0.86, 1.75 | 1.05 | 0.74, 1.49 |
| Demographic | ||||
| Ages (years) | ||||
| 19–34 | Ref | Ref | ||
| 35–54 | 0.65 | 0.26, 1.63 | 0.73 | 0.29, 1.86 |
| 55+ | 0.34 | 0.13, 0.90 | 0.42 | 0.16, 1.12 |
| Female | 1.02 | 0.72, 1.45 | 0.78 | 0.56, 1.10 |
| Black | 0.94 | 0.47, 1.87 | 1.38 | 0.70, 2.73 |
| Legal income ≥ $5000 USD | 0.55 | 0.40, 0.75 | 0.64 | 0.46, 0.88 |
| Current employment | 0.77 | 0.56, 1.05 | 0.98 | 0.71, 1.34 |
| Mental health | ||||
| Depressive symptoms | 1.99 | 1.43, 2.77 | 1.79 | 1.29, 2.49 |
| Depressionb | 1.54 | 1.12, 2.12 | ||
| Manic depressionb | 1.29 | 0.86, 1.94 | ||
| Anxietyb | 1.30 | 0.87, 1.95 | ||
| Schizophreniab | 1.13 | 0.76, 1.69 | ||
| Suicidal thoughts | 1.36 | 0.83, 2.24 | ||
| Suicide plans | 1.00 | 0.46, 2.17 | ||
| Suicide attempts | 2.16 | 0.59, 7.99 | ||
| HIV | ||||
| HIV positive | 1.18 | 0.82, 1.70 | 1.06 | 0.75, 1.50 |
| Risk Behavior | ||||
| Incarcerated | 2.13 | 1.38, 3.29 | 1.91 | 1.24, 2.94 |
| Sex with an IDU partner | 1.56 | 1.09, 2.23 | 1.57 | 1.09, 2.27 |
| Trade sex for drugs, money, food, or shelter | 0.96 | 0.83, 1.11 | 0.92 | 0.79, 1.08 |
| Crack use | 1.60 | 1.13, 2.25 | 1.32 | 0.94, 1.86 |
| Methadone maintenance | 1.27 | 0.91, 1.80 | 1.36 | 0.97, 1.90 |
| Detoxification | 1.41 | 0.70, 2.82 | 1.41 | 0.71, 2.78 |
Note: All factors are time-varying excluding age, gender, and race, which are measured at the first visit. All time-varying factors are measured within the last six months, excluding current employment measured at the time of the visit, and depressive symptoms measured in the past week. Time-varying factors are lagged one visit from when injection drug use is measured. Previous injection drug use refers to injection drug use measured at the lagged visit. Past homelessness is defined as any episode of homelessness prior to when homelessness is measured.
Abbreviations: CI, confidence interval; OR, odds ratio
Adjusted for baseline and time-varying covariates
Self reported diagnosis or treatment for mental health illness by a health care provider
Among visits when injection drug use was reported in the prior six months (Table 4), homelessness <1 month was significantly associated with sustained injection drug use in unadjusted analysis. Homelessness ≥1 month was not significantly associated with sustained injection drug use in unadjusted analysis. After adjustment for other covariates, there was no association between homelessness of any duration and sustained injection drug use [homelessness <1 month: AOR=1.03, 95% CI (0.71, 1.49); homelessness ≥1 month: AOR=0.81 95% CI (0.56, 1.17)]. Male gender, HIV negative serostatus, depressive symptoms, daily injection, and sharing cotton were significantly associated with sustained injection drug use in the adjusted model.
Table 4.
Unadjusted and adjusted association between homelessness and sustained injection drug use among 992 participants who reported previous injection drug use across 2677 visits from 2005–2009 (Model 3)
| Unadjusted OR | 95% CI | Adjusted ORa | 95% CI | |
|---|---|---|---|---|
| Homelessness | ||||
| No homelessness | Ref | Ref | ||
| < 1 Month | 1.43 | 1.01, 2.04 | 1.03 | 0.71, 1.49 |
| ≥ 1 Month | 1.25 | 0.89, 1.77 | 0.81 | 0.56, 1.17 |
| Past history of homelessness | 0.98 | 0.74, 1.31 | 1.02 | 0.76, 1.37 |
| Demographic | ||||
| Ages (years) | ||||
| 19–34 | Ref | Ref | ||
| 35–54 | 0.54 | 0.32, 0.91 | 0.81 | 0.46, 1.44 |
| 55+ | 0.46 | 0.25, 0.85 | 0.65 | 0.34, 1.27 |
| Female | 0.60 | 0.45, 0.81 | 0.52 | 0.38, 0.71 |
| Black | 0.46 | 0.31, 0.70 | 0.66 | 0.41, 1.06 |
| Legal income ≥$5000 USD | 0.82 | 0.61, 1.10 | 0.86 | 0.63, 1.17 |
| Current employment | 1.06 | 0.77, 1.46 | 1.10 | 0.79, 1.54 |
| Mental health | ||||
| Depressive symptoms | 1.69 | 1.29, 2.22 | 1.58 | 1.19, 2.10 |
| Depressionb | 0.80 | 0.61, 1.04 | ||
| Manic depressionb | 0.90 | 0.65, 1.28 | ||
| Anxietyb | 0.92 | 0.65, 1.31 | ||
| Schizophreniab | 0.94 | 0.67, 1.31 | ||
| Suicidal thoughts | 1.05 | 0.76, 1.44 | ||
| Suicide plans | 1.29 | 0.79, 2.09 | ||
| Suicide attempts | 1.28 | 0.59, 2.78 | ||
| HIV | ||||
| HIV positive | 0.52 | 0.38, 0.71 | 0.57 | 0.41, 0.78 |
| Risk Behavior | ||||
| Frequency of Injection | ||||
| Less than daily | Ref | Ref | ||
| Daily | 2.13 | 1.70, 2.67 | 1.83 | 1.44, 2.31 |
| Needle sharing | 1.77 | 1.35, 2.33 | 1.02 | 0.72, 1.43 |
| Cotton sharing | 2.36 | 1.78, 3.14 | 1.98 | 1.42, 2.76 |
| Shooting gallery attendance | 1.25 | 0.83, 1.88 | 0.72 | 0.46, 1.13 |
| Incarcerated | 1.31 | 0.97, 1.77 | 1.06 | 0.78, 1.45 |
| Sex with an IDU | 1.31 | 1.01, 1.70 | 1.18 | 0.87, 1.61 |
| Trade sex for drugs, money, food, or shelter | 1.03 | 0.91, 1.18 | 0.95 | 0.82, 1.11 |
| Crack use | 1.18 | 0.93, 1.50 | 1.06 | 0.82, 1.36 |
| Methadone maintenance | 0.70 | 0.52, 0.93 | 0.83 | 0.61, 1.11 |
| Detoxification | 0.92 | 0.64, 1.31 | 0.72 | 0.49, 1.04 |
| Overdose | ||||
| Non-fatal overdose | 1.68 | 1.19, 2.37 | 1.35 | 0.94, 1.93 |
Note: All factors are time-varying excluding age, gender, and race, which are measured at the first visit. All time-varying factors are measured within the last six months, excluding current employment measured at the time of the visit, and depressive symptoms measured in the past week. Time-varying factors are lagged one visit from when injection drug use is measured. Previous injection drug use refers to injection drug use measured at the lagged visit. Past homelessness is defined as any episode of homelessness prior to when homelessness is measured.
Abbreviations: CI, confidence interval; OR, odds ratio
Adjusted for baseline and time-varying covariates
Self reported diagnosis or treatment for mental health illness by a health care provider
Despite the observed heterogeneity of the impact of homelessness on relapse and sustained injection drug use, when an interaction between injection drug use and homelessness was included in the combined model it was not statistically significant [homelessness <1 month: (p=0.255); homelessness ≥1 month: (p=0.279)]. Further, no statistically significant interaction was observed between depressive symptoms and homelessness [homelessness <1 month: (p=0.405); homelessness ≥1 month: (p=0.466)] nor between sex with an IDU partner and homelessness [homelessness <1 month: (p=0.596); homelessness ≥1 month: (p=0.065)]. This data is not shown.
3.3. Homelessness and Injection-Related Risk Behavior
Among consecutive visits when participants reported injection drug use, homelessness of any duration was associated with subsequent injection-related risk behavior in unadjusted analysis (Table 5). In adjusted analysis, homelessness <1 month was no longer associated with subsequent injection-related risk behavior [AOR= 0.80, 95% CI (0.53, 1.21)] but homelessness ≥1 month remained significantly associated with subsequent injection-related risk behavior [AOR=1.61, 95% CI (1.06, 2.45)]. Past history of homelessness, non-black race, and previous needle and cotton sharing were significantly associated with subsequent injection-related risk behavior. The association between sex with an IDU partner and subsequent injection-related risk behavior was of borderline statistical significance.
Table 5.
Unadjusted and adjusted association between homelessness and subsequent injection-related risk behavior among 689 participants consecutively reporting injection drug use across 1900 visits from 2005– 2009 (Model 4)
| Unadjusted OR | 95% CI | Adjusteda OR | 95% CI | |
|---|---|---|---|---|
| Homelessness | ||||
| No Homelessness(reference) | Ref | Ref | ||
| < 1 Month | 1.70 | 1.04, 2.78 | 0.80 | 0.53, 1.21 |
| ≥ 1 Month | 4.22 | 2.54, 7.03 | 1.61 | 1.06, 2.45 |
| Past history of homelessness | 1.09 | 0.72, 1.65 | 1.57 | 1.14, 2.17 |
| Demographic | ||||
| Ages (years) | ||||
| 19–34 (reference) | Ref | Ref | ||
| 35–54 | 0.33 | 0.15, 0.71 | 0.99 | 0.54, 1.79 |
| 55+ | 0.22 | 0.08, 0.58 | 0.99 | 0.49, 2.04 |
| Female | 1.42 | 0.80, 2.51 | 1.04 | 0.74, 1.47 |
| Black | 0.15 | 0.08, 0.32 | 0.54 | 0.33, 0.88 |
| Legal income ≥$5000 USD | 0.92 | 0.58, 1.46 | 0.88 | 0.61, 1.28 |
| Current employment | 0.91 | 0.56, 1.46 | 1.06 | 0.72, 1.57 |
| Mental health | ||||
| Depressive symptoms | 2.12 | 1.45, 3.10 | 1.22 | 0.90, 1.66 |
| Depressionb | 1.74 | 1.14, 2.67 | ||
| Manic depressionb | 1.99 | 1.15, 3.47 | ||
| Anxietyb | 02.14 | 1.24, 3.69 | ||
| Schizophreniab | 01.69 | 0.98, 2.90 | ||
| Suicidal thoughts | 11.66 | 1.04, 2.67 | ||
| Suicide plans | 22.31 | 1.16, 4.63 | ||
| Suicide attempts | 22.59 | 0.85, 7.96 | ||
| HIV | ||||
| HIV positive | 0.99 | 0.53, 1.85 | 1.21 | 0.84, 1.74 |
| Risk behavior | ||||
| Frequency of injection | ||||
| Less than daily | Ref | Ref | ||
| Daily injection | 1.45 | 1.04, 2.03 | 1.18 | 0.90, 1.56 |
| Needle sharing | 7.58 | 5.51, 10.41 | 3.58 | 2.57, 4.99 |
| Cotton sharing | 5.66 | 4.11, 7.80 | 3.23 | 2.34, 4.44 |
| Shooting gallery attendance | 4.10 | 2.33, 7.23 | 1.55 | 0.95, 2.53 |
| Incarceration | 1.50 | 0.98, 2.29 | 1.11 | 0.79, 1.58 |
| Sex with an IDU | 2.79 | 1.90, 4.11 | 1.41 | 0.99, 1.99 |
| Trade sex for drugs, money, food, or shelter | 1.09 | 0.88, 1.34 | 0.92 | 0.77, 1.10 |
| Crack Use | 1.95 | 1.34, 2.84 | 1.22 | 0.91, 1.63 |
| Methadone maintenance | 1.10 | 0.69, 1.73 | 0.98 | 0.70, 1.39 |
| Detoxification | 0.97 | 0.59, 1.59 | 0.79 | 0.51, 1.20 |
| Overdose | ||||
| Non-fatal overdose | 2.14 | 1.37, 3.34 | 1.00 | 0.68, 1.46 |
Note: All factors are time-varying excluding age, gender, and race, which are measured at the first visit. All time-varying factors are measured within the last six months, excluding current employment measured at the time of the visit, and depressive symptoms measured in the past week. Time-varying factors are lagged one visit from when injection-related risk behavior is measured. Past homelessness is defined as any episode of homelessness prior to when homelessness is measured.
Abbreviations: CI, confidence interval; OR, odds ratio
Adjusted for baseline and time-varying covariates
Self reported diagnosis or treatment for mental health illness by a health care provider
4. DISCUSSION
We observed a high frequency of homelessness in this sample of current and former IDUs. Of particular concern was that half of the participants who reported any episode of homelessness experienced recurrent homelessness. The relationship between homelessness and subsequent injection drug use differed among those who were actively injecting as compared to those who were not. Homelessness was associated with relapse among those who had stopped injecting, but was not associated with sustained injection drug use among active injectors. While homelessness did not appear to influence sustained injection among active injectors, it was associated with increased likelihood of injection-related risk behavior among those who were homeless for at least one month.
These study findings are consistent with other studies that demonstrate frequent homelessness among IDUs, and studies that have shown a temporal relationship between homelessness and relapse (Mehta et al., 2012; Shah et al., 2006). Our findings are also comparable to studies that have demonstrated an association between incarceration and relapse (Mehta et al., 2012), and having a drug using partner and relapse (Termorshuizen et al., 2005). Further, the findings from this study demonstrate an inverse association between HIV positivity and sustained injection drug use as seen previously (Celentano et al., 1994).
Our study did not demonstrate that homelessness among active injectors increased or decreased the likelihood of sustained injection drug use after adjusting for other factors. This may reflect the baseline level of instability among active injectors such that homelessness has little additional influence on whether one continues or stops injecting. However, the relationship between homelessness and subsequent injection-related risk behavior among active injectors raises concerns. While HIV seroconversion in this cohort has declined over recent years (Mehta et al., 2006) HCV incidence remains high (Mehta et al., 2011), partly due to the large reservoir of HCV among IDUs and the greater likelihood of HCV transmission (as compared to HIV) through a single exposure (Sulkowski et al., 2002). Among persons recruited to ALIVE during the 2005–2008 wave, HCV incidence in the first year after recruitment was 7.8 per 100 per year compared with 0 for HIV (Mehta et al., 2011). A recent study demonstrated an association between HCV incidence and unstable housing among IDUs (Kim et al., 2009) and this association may partially be mediated by paraphernalia sharing.
This study has limitations that may impact the interpretation of results. Because we were unable to determine the exact time of exposure, we could not ascertain whether homelessness preceded or followed episodes of mental illness, or the occurrence of other events, which may be associated with subsequent injection drug use. Additionally, our definition of homelessness did not consider the different types of locations where participants slept, due to sample size. This may partially explain the observed differences in the magnitude and statistical significance of the associations between duration of homelessness and injection drug use, and injection-related risk behavior. Studies have demonstrated that patterns of drug use vary across settings. For example, temporary housing (e.g., hostels) has been described as being conducive to injection drug use and risky behavior (Briggs et al., 2009; Wright et al., 2005). Further, even though they may not prevent residents from using drugs or engaging in risky behaviors off premises (Gibson et al., 2011), shelters that require sobriety and administer drug testing may prevent residents from using drugs. It has also been reported that homeless drug users tend to reduce the amount of drugs that they use due to lack of income (Wright et al., 2005). But, at the same time, lack of income may actually encourage injection-related risk behavior among homeless IDUs who spend significant time on the street (Bourgois, 1998).
In this study, sleeping in a shelter or on the streets was reported more frequently when homelessness ≥1 month was reported as compared to when homelessness <1 month was reported. The lower likelihood of injection drug use among persons homelessness ≥1 month (as compared to <1 month) in this study may reflect factors present in shelters, and on the streets, which may discourage injection drug use. Further, lack of income among homeless persons on the streets may reduce the quantity of drugs used (Wright et al., 2005), but increase the likelihood of injection-related risk behavior (Bourgois, 1998). This may explain the association between homelessness ≥ 1 month and injection-related risk behavior observed in this study, as sleeping on the streets was frequently reported by participants homeless for ≥ 1 month. Additional research on the impact that different settings have on injection drug use is needed.
Other limitations include the exclusion of visits due to missing information and gaps between visits, which can induce selection bias. Previous homelessness, HIV positivity, depressive symptoms, incarceration, not having an IDU sex partner, legal income less than $5000 USD, and unemployment were observed more frequently (≥10%) among visits excluded due to missing information compared to visits that were included. Previous injection drug use, homelessness, HIV positivity, incarceration, sex with an IDU partner, legal income less than $5000 USD, unemployment, daily injection and cotton sharing were reported with greater frequency across visits excluded due to gaps as compared to visits included in analysis. Because only 6% of visits were excluded due to missing information or gaps between visits, it is expected that these exclusions did not overly impact our findings.
Finally, ALIVE represents a community-based cohort of predominantly middle-aged black men. Therefore these findings may not be generalizable to all IDUs. However these demographics are consistent with what has been reported in Baltimore by other sources.
With mounting evidence demonstrating a temporal relationship between homelessness, injection drug use, and injection-related risk behavior, greater support for housing-based interventions for persons with a history of drug use is warranted. Persons with a history of drug use face challenges in acquiring and maintaining proper housing, as they may be more likely to be low-income, unemployed, and have an incarceration record that can render them ineligible for subsidized housing. Housing First interventions, which provide housing to individuals without drug treatment or engagement in other services as a prerequisite, have been shown to increase housing stability and drug treatment retention among persons with substance abuse and psychiatric disorders (Appel et al., 2012; Tsemberis et al., 2004). Housing First models have also been reported to lessen healthcare and societal costs (Larimer et al., 2009).
This study suggests that homelessness is associated with relapse into injection drug use among those who have stopped injecting, and injection-related risk behavior among active injectors. Together such mechanisms may partially explain the link between homelessness and adverse outcomes including those related to HIV and HCV. This study strengthens support for policies that invest in affordable housing and Housing First models of care. Additionally, this study highlights the importance of strengthening risk reduction services for unstably housed persons that cannot abstain from injection. Greater understanding of the influence of homelessness on addiction over time, and how policies and public health interventions can be tailored to prevent homelessness, has the potential to improve drug recovery and other health outcomes.
Acknowledgements
The authors would like to thank the ALIVE study staff and participants, without whom this study would not be possible.
Role of Funding Source
This study was supported by the National Institute on Drug Abuse at the National Institutes of Health (grants R01DA012568, R01DA004334, and T32DA007292). The funder did not play any role in the design, conduct, or analysis of the data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
SL and SM conceived the aims of this study. SL performed the statistical analysis and wrote the initial draft of the manuscript. All authors have played a substantial role in revising and contributing to the paper. All authors have approved a final version of the manuscript.
Conflict of Interest
No conflict declared
REFERENCES
- Aidala A, Cross JE, Stall R, Harre D, Sumartojo E. Housing status and HIV risk behaviors: Implications for prevention and policy. AIDS Behav. 2005;9:251–265. doi: 10.1007/s10461-005-9000-7. [DOI] [PubMed] [Google Scholar]
- Alexandre PK, French MT. Further evidence on the labor market effects of addiction: chronic drug use and employment in metropolitan Miami. Contemp. Econ. Policy. 2004;22:382–393. [Google Scholar]
- Appel PW, Ellison AA, Jansky HK, Oldak R. Barriers to enrollment in drug abuse treatment and suggestions for reducing them: opinions of drug injecting street outreach clients and other system stakeholders. Am. J. Drug Alcohol Abuse. 2004;30:129–153. doi: 10.1081/ada-120029870. [DOI] [PubMed] [Google Scholar]
- Appel PW, Tsemberis S, Joseph H, Stefancic A, Lambert-Wacey D. Housing first for severely mentally ill homeless methadone patients. J. Addict. Dis. 2012;31:270–277. doi: 10.1080/10550887.2012.694602. [DOI] [PubMed] [Google Scholar]
- Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann. Int. Med. 2006;144:705–714. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- Bohnert ASB, Bradshaw CP, Latkin CA. A social network perspective on heroin and cocaine use among adults: evidence of bidirectional influences. Addiction. 2009;104:1210–1218. doi: 10.1111/j.1360-0443.2009.02615.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgois P. The moral economies of homeless heroin addicts: confronting ethnography, HIV risk, and everyday violence in San Francisco shooting encampments. Subst. Use Misuse. 1998;33:2323–2351. doi: 10.3109/10826089809056260. [DOI] [PubMed] [Google Scholar]
- Brady JE, Friedman SR, Cooper HLF, Flom PL, Tempalski B, Gostnell K. Estimating the prevalence of injection drug users in the US and in large US metropolitan areas from 1992 to 2002. J. Urban Health. 2008;85:323–351. doi: 10.1007/s11524-007-9248-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs D, Rhodes T, Marks D, Kimber J, Holloway G, Jones S. Injecting drug use and unstable housing: scope for structural interventions in harm reduction. Drugs. 2009;16:436–450. [Google Scholar]
- The Centers for Disease Control and Prevention. Public health and injection drug use. MMWR. 2001;50:377. [Google Scholar]
- The Centers for Disease Control and Prevention. HIV infection among injection-drug users: 34 states, 2004--2007. MMWR. 2009;58:1291–1295. [PubMed] [Google Scholar]
- Celentano DD, Munoz A, Cohn S, Nelson KE, Vlahov D. Drug-related behavior change for HIV transmission among American injection drug users. Addiction. 1994;89:1309–1317. doi: 10.1111/j.1360-0443.1994.tb03310.x. [DOI] [PubMed] [Google Scholar]
- Celentano DD, Vlahov D, Cohn S, Anthony JC, Solomon L, Nelson KE. Risk-factors for shooting gallery use and cessation among intravenous-drug users. Am. J. Public Health. 1991;81:1291–1295. doi: 10.2105/ajph.81.10.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen XJ, Tyler KA, Whitbeck LB, Hoyt DR. Early sexual abuse, street adversity, and drug use among female homeless and runaway adolescents in the midwest. J. Drug Issues. 2004;34:1–21. [Google Scholar]
- Crofts N, Louie R, Rosenthal D, Jolley D. The first hit: circumstances surrounding initiation into injecting. Addiction. 1996;91:1187–1196. doi: 10.1046/j.1360-0443.1996.918118710.x. [DOI] [PubMed] [Google Scholar]
- Davey-Rothwell MA, Latimore A, Hulbert A, Latkin CA. Sexual networks and housing stability. J. Urban Health. 2011;88:759–766. doi: 10.1007/s11524-011-9570-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson-Gomez J, Convey M, Hilario H, Corbett AM, Weeks M. Unofficial policy: access to housing, housing information and social services among homeless drug users in Hartford, Connecticut. Subst. Abuse Treat. Prev. Policy. 2007;2:8. doi: 10.1186/1747-597X-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diggle PJ, Heagerty PJ, Liang K-Y, Zeger SL. Anaylsis of Longitudinal Data. Oxford, England: Oxford University Press Inc.; 2002. [Google Scholar]
- Galai N, Safaeian M, Vlahov D, Bolotin A, Celentano D. Longitudinal patterns of drug injection behavior in the ALIVE Study cohort, 1988–2000; description and determinants. Am. J. Epidemiol. 2003;158:695–704. doi: 10.1093/aje/kwg209. [DOI] [PubMed] [Google Scholar]
- Genberg BL, Gange SJ, Go VF, Celentano DD, Kirk GD, Latkin CA, Mehta SH. The Effect of neighborhood deprivation and residential relocation on long-term injection cessation among injection drug Users (IDUs) in Baltimore, Maryland. Addiction. 2011a;106:1966–1974. doi: 10.1111/j.1360-0443.2011.03501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genberg BL, Gange SJ, Go VF, Celentano DD, Kirk GD, Mehta SH. Trajectories of injection drug use over 20 years (1988–2008) in Baltimore, Maryland. Am. J. Epidemiol. 2011b;173:829–836. doi: 10.1093/aje/kwq441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson EK, Exner H, Stone R, Lindquist J, Cowen L, Roth EA. A mixed methods approach to delineating and understanding injection practices among clientele of a Victoria, British Columbia needle exchange program. Drug Alcohol Rev. 2011;30:360–365. doi: 10.1111/j.1465-3362.2010.00219.x. [DOI] [PubMed] [Google Scholar]
- Golub ET, Strathdee SA, Bailey SL, Hagan H, Latka MH, Hudson SM, Garfein RS. Distributive syringe sharing among young adult injection drug users in five U.S. cities. Drug Alcohol Depend. 2007;91(Suppl. 1):S30–S38. doi: 10.1016/j.drugalcdep.2007.02.013. [DOI] [PubMed] [Google Scholar]
- Kim C, Kerr T, Li K, Zhang R, Tyndall MW, Montaner JSG, Wood E. Unstable housing and hepatitis C incidence among injection drug users in a Canadian setting. BMC Public Health. 2009;9:270. doi: 10.1186/1471-2458-9-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan A, Wickersham JA, Chitsaz E, Springer SA, Jordan AO, Zaller N, Altice FL. Post-release substance abuse outcomes among HIV-infected jail detainees: results from a multisite study. AIDS Behav. doi: 10.1007/s10461-012-0362-3. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Malone DK, Garner MD, Atkins DC, Burlingham B, Lonczak HS, Tanzer K, Ginzler J, Clifasefi SL, Hobson WG, Marlatt GA. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301:1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- Latkin C, Mandell W, Vlahov D, Knowlton A, Oziemkowska M, Celentano D. Personal network characteristics as antecedents to needle-sharing and shooting gallery attendance. Soc. Networks. 1995;17:219–228. [Google Scholar]
- Latkin CA, Knowlton AR, Hoover D, Mandell W. Drug network characteristics as a predictor of cessation of drug use among adult injection drug users: a prospective study. Am. J. Drug Alcohol Abuse. 1999;25:463–473. doi: 10.1081/ada-100101873. [DOI] [PubMed] [Google Scholar]
- Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. Aids Educ. Prev. 2002;14:367–378. doi: 10.1521/aeap.14.6.367.24075. [DOI] [PubMed] [Google Scholar]
- Mackesy-Amiti ME, Donenberg GR, Ouellet LJ. Prevalence of psychiatric disorders among young injection drug users. Drug Alcohol Depend. 2012;124:70–78. doi: 10.1016/j.drugalcdep.2011.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta SH, Astemborski J, Kirk GD, Strathdee SA, Nelson KE, Vlahov D, Thomas DL. Changes in blood-borne infection risk among injection drug users. J. Infect. Dis. 2011;203:587–594. doi: 10.1093/infdis/jiq112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta SH, Galai N, Astemborski J, Celentano DD, Strathdee SA, Vlahov D, Nelson KE. HIV incidence among injection drug users in Baltimore, Maryland (1988–2004) J. Acquir. Immune Defic. Syndr. 2006;43:368–372. doi: 10.1097/01.qai.0000243050.27580.1a. [DOI] [PubMed] [Google Scholar]
- Mehta SH, Sudarshi D, Srikrishnan AK, Celentano DD, Vasudevan CK, Anand S, Kumar MS, Latkin C, Solomon S, Solomon SS. Factors associated with injection cessation, relapse and initiation in a community-based cohort of injection drug users in Chennai, India. Addiction. 2012;107:349–358. doi: 10.1111/j.1360-0443.2011.03602.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Milloy MJ, Wood E, Small W, Tyndall M, Lai C, Montaner J, Kerr T. Incarceration experiences in a cohort of active injection drug users. Drug Alcohol Rev. 2008;27:693–699. doi: 10.1080/09595230801956157. [DOI] [PubMed] [Google Scholar]
- Mizuno Y, Purcell DW, Zhang J, Knowlton AR, De Varona M, Arnsten JH, Knight KR. Predictors of current housing status among HIV-seropositive injection drug users (IDUs): results from a 1-Year Study. AIDS Behav. 2009;13:165–172. doi: 10.1007/s10461-008-9364-6. [DOI] [PubMed] [Google Scholar]
- Muir-Cochrane E, Fereday J, Jureidini J, Drummond A, Darbyshire P. Self-management of medication for mental health problems by homeless young people. Int. J. Ment. Health Nurs. 2006;15:163–170. doi: 10.1111/j.1447-0349.2006.00420.x. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- Roy E, Boivin JF, Leclerc P. Initiation to drug injection among street youth: a gender-based analysis. Drug Alcohol Depend. 2010;114:49–54. doi: 10.1016/j.drugalcdep.2010.09.003. [DOI] [PubMed] [Google Scholar]
- The Substance Abuse and Mental Health Services Administration. U.S. Substance Abuse and Mental Health Services Administration: A report required by Congress on performance partnerships. Washington, DC: 2005. [Google Scholar]
- Shah NG, Galai N, Celentano DD, Vlahov D, Strathdee SA. Longitudinal predictors of injection cessation and subsequent relapse among a cohort of injection drug users in Baltimore, MD, 1988–2000. Drug Alcohol Depend. 2006;83:147–156. doi: 10.1016/j.drugalcdep.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Small W, Kerr T, Charette J, Schechter MT, Spittal PM. Impacts of intensified police activity on injection drug users: evidence from an ethnographic investigation. Intl. J. Drug Policy. 2006;17:85–95. [Google Scholar]
- Song JY, Safaeian M, Strathdee SA, Vlahov D, Celentano DD. The prevalence of homelessness among injection drug users with and without HIV infection. J. Urban Health. 2000;77:678–687. doi: 10.1007/BF02344031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulkowski MS, Ray SC, Thomas DL. Needlestick transmission of hepatitis C. JAMA. 2002;287:2406–2413. doi: 10.1001/jama.287.18.2406. [DOI] [PubMed] [Google Scholar]
- Termorshuizen F, Krol A, Prins M, Geskus R, van den Brink W, van Ameijden EJ. Prediction of relapse to frequent heroin use and the role of methadone prescription: an analysis of the Amsterdam Cohort Study among drug users. Drug Alcohol Depend. 2005;79:231–240. doi: 10.1016/j.drugalcdep.2005.01.013. [DOI] [PubMed] [Google Scholar]
- Tobin KE, Davey-Rothwell M, Latkin CA. Social-level correlates of shooting gallery attendance: a focus on networks and norms. AIDS Behav. 2010;14:1142–1148. doi: 10.1007/s10461-010-9670-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsemberis S, Gulcur L, Nakae M. Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am. J. Public Health. 2004;94:651–656. doi: 10.2105/ajph.94.4.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D, Anthony JC, Munoz A, Margolick J, Nelson KE, Celentano DD, Solomon L, Polk BF. The Alive Study - a longitudinal study of HIV-1 infection in intravenous drug users: description of methods. J. Drug Issues. 1991;21:759–776. [PubMed] [Google Scholar]
- Vlahov D, Wang C, Ompad D, Fuller CM, Caceres W, Ouellet L, Kerndt P, Des Jarlais DC, Garfein RS. Mortality risk among recent-onsetiInjection drug users in five U.S. cities. Subst. Use Misuse. 2008;43:413–428. doi: 10.1080/10826080701203013. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am. J. Epidemiol. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Werb D, Wood E, Small W, Strathdee S, Li K, Montaner J, Kerr T. Effects of police confiscation of illicit drugs and syringes among injection drug users in Vancouver. Intl. J. Drug Policy. 2008;19:332–338. doi: 10.1016/j.drugpo.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams S, Stickley T. Stories from the streets: people's experiences of homelessness. J. Psychiatr. Ment. Health Nurs. 2011;18:432–439. doi: 10.1111/j.1365-2850.2010.01676.x. [DOI] [PubMed] [Google Scholar]
- Wood E, Tyndall MW, Spittal PM, Li K, Kerr T, Hogg RS, Montaner JS, O'Shaughnessy MV, Schechter MT. Unsafe injection practices in a cohort of injection drug users in Vancouver: could safer injecting rooms help? CMAJ. 2001;165:405–410. [PMC free article] [PubMed] [Google Scholar]
- Wright N, Oldham N, Jones L. Exploring the relationship between homelessness and risk factors for heroin-related death--a qualitative study. Drug Alcohol Rev. 2005;24:245–251. doi: 10.1080/09595230500170308. [DOI] [PubMed] [Google Scholar]