Community health workers (CHWs) used smart phones with and without patient navigation to promote breast health in rural Bangladesh and were compared with CHWs using paper-and-pencil methods only. Findings showed that CHWs who did not use the smart phone applications completed fewer interviews, had inferior data quality, and identified significantly fewer women with abnormal breast exams, indicating that smart phones can be used to promote breast health in rural areas. CHWs with smart phones and 1-day training in patient navigation were more effective in encouraging women with abnormal breast exams to attend for proper care.
Keywords: Breast cancer, Community health workers, Health promotion, Patient navigation
Abstract
Objective.
To demonstrate proof of concept for a smart phone-empowered community health worker (CHW) model of care for breast health promotion, clinical breast examination (CBE), and patient navigation in rural Bangladesh.
Methods.
This study was a randomized controlled trial; July 1 to October 31, 2012, 30 CHWs conducted door-to-door interviews of women aged 25 and older in Khulna Division. Only women who disclosed a breast symptom were offered CBE. Arm A: smart phone with applications to guide interview, report data, show motivational video, and offer appointment for women with an abnormal CBE. Arm B: smart phone/applications identical to Arm A plus CHW had training in “patient navigation” to address potential barriers to seeking care. Arm C: control arm (no smart phone; same interview recorded on paper). Outcomes are presented as the “adherence” (to advice regarding a clinic appointment) for women with an abnormal CBE. This study was approved by Women’s College Hospital Research Ethics Board (Toronto, Ontario, Canada) and district government officials (Khulna, Bangladesh). Funded by Grand Challenges Canada.
Results.
In 4 months, 22,337 women were interviewed; <1% declined participation, and 556 women had an abnormal CBE. Control group CHWs completed fewer interviews, had inferior data quality, and identified significantly fewer women with abnormal breast exams compared with CHWs in arms A and B. Arm B had the highest adherence.
Conclusion.
CHWs guided by our smart phone applications were more efficient and effective in breast health promotion compared with the control group. CHW “navigators” were most effective in encouraging women with an abnormal breast examination to adhere to advice regarding clinic attendance.
Implications for Practice:
In low-income countries such as Bangladesh, there are few opportunities for affordable, quality care for breast cancer. Gender inequity and cancer myths limit a woman’s choice to seek care if she finds a breast lump. This is the first study to suggest that we can make an impact on breast cancer with basic training of community health workers guided by smart phone applications. With just 1 day of extra training in “patient navigation,” we also show that social and cultural issues can be addressed, which improve the likelihood that women with a serious breast problem will attend for proper care.
Introduction
Breast cancer is the most common cancer in women worldwide [1]. In high-income counties, most women diagnosed with breast cancer will survive their disease, whereas those in a low- or middle-income country (LMIC) may face odds of survival as low as 10%–25% [2–4]. Despite lower age-standardized incidence rates, the majority of breast cancer deaths occur in developing countries, and affect mostly poor, premenopausal women [1, 4, 5]. In Bangladesh, there are few opportunities for affordable, comprehensive care, and myths about cancer, taboos regarding the female body, and gender inequity limit the extent to which women believe they have a “choice” to attend for proper medical care if they have a breast symptom [6].
We previously published a report on breast cancer control in Bangladesh [6] that included qualitative research on barriers to seeking care and an overview of the systemic problems of governance, transparency, and corruption [7]. The latter are pervasive issues that confound efforts to improve the dismal survival rates for breast and other cancers, particularly in rural areas. The majority of women whose stories are highlighted in the report had locally advanced or metastatic breast cancer at diagnosis, and many presented with a fungating mass, severe brachial plexopathy, or uncontrolled pain. When we asked why they delayed seeking care, they told us that they were aware for months or even years that they had a serious, even life-threatening health problem. Most had first seen a homeopath, and at least one third had the original breast lump “removed,” which often meant incomplete surgical excision with no pathological diagnosis or follow-up. We heard about fears of family abandonment and a sense of fatalism that breast cancer is a death sentence.
Breast screening with clinical breast examination (CBE) or breast self-examination in LMICs remains unproven [8–10] but is included as an option in the resource-tiered guidelines of the Breast Health Global Initiative [11]. However, given the low incidence of breast cancer in rural Bangladesh (estimated age-standardized rate = 21.7/100,000 women per year) [12], the young age of onset (mean age = 41 years) [13], and the difficulty in “closing the loop” from presentation through diagnosis, treatment, and appropriate follow-up, a population-based screening program can be considered premature at this time.
In 2009, the International Breast Cancer Research Foundation (IBCRF; Madison, WI) [14] partnered with Amader Gram (“Our Village” in Bengali), a Bangladeshi nongovernmental organization specializing in “Information and Communications Technology for Development,” to form Amader Gram Breast Care [15]. This unique partnership led to the first resource-appropriate, locally informed, evidence-based clinical practice guidelines for breast cancer in Bangladesh [16] and the creation of a breast center for assessment, diagnosis, treatment planning, and follow-up. AGBC offers diagnostic ultrasound-guided core biopsy, a mechanism for timely access to complete histopathology (including estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2), and referral to the local government hospital for staging investigations, surgical intervention, and if necessary, chemotherapy. Radiation is not yet available in Khulna Division, Bangladesh. There is a nominal, one-time registration fee, and all services are either free of charge or based on a modest sliding scale, following means testing. AGBC also opened three “walk-in” clinics at the sites of the rural IT training centers, attended weekly by a female physician. Women found to have a significant breast abnormality are offered referral to AGBC Centre in Khulna City for further assessment, as appropriate. Once the program was established, it became clear that more community-based health promotion efforts would be needed, and that individualized, confidential peer-to-peer discussions might encourage women to disclose a breast symptom and to attend for medical care. In an effort to achieve these aims, AGBC and the IBCRF partnered with mPower Health, a division of mPower Social Enterprises Ltd. [17], a Bangladeshi-owned social business with expertise in mobile phone applications for population health interventions.
“Digital Bangladesh” [18], a government mandate aimed at closing the so-called “digital divide,” is a development success story in a country where 52% of the population is under age 25 [19]. Over the past decade, there have been major infrastructural improvements with near-complete Internet coverage through telecommunication networks and extensive use of low-cost mobile phones throughout the country. Government, nongovernmental organizations, and private businesses are taking advantage of this enormous potential, incorporating SMS texting and other functions to boost the effectiveness of development efforts, real-time information updates for commerce, and, more recently, health interventions [20–23]. In Bangladesh, the deployment of female community health workers (CHWs) is a well-established model for family planning and maternal/child health interventions, particularly in rural areas and urban slums [24]. To enhance the impact of CHW programs, several groups are tapping into the potential of Digital Bangladesh to create “mHealth” projects [17, 22]. For the current report, mHealth is defined broadly as “the use of mobile and wireless technologies to support the achievement of health objectives” [25].
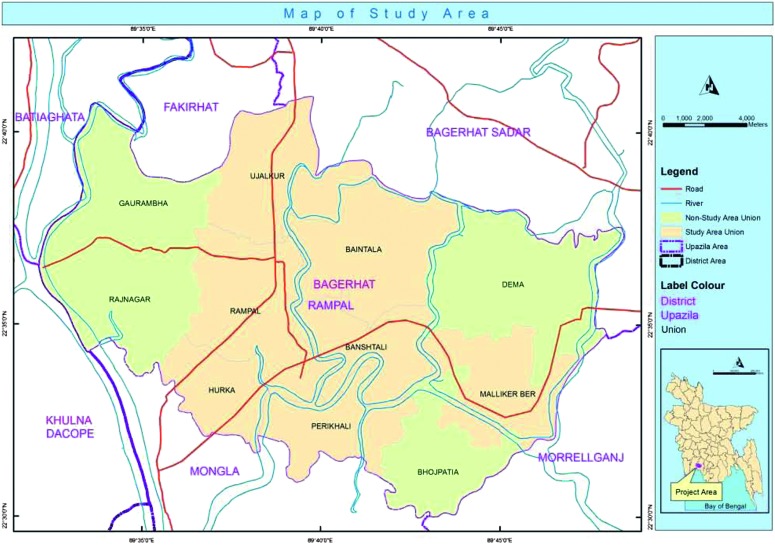
Khulna Division, population 15,563,000, is densely populated, with 76.5% living on less than $2/day [26]. Despite recent advances in early childhood education particularly for girls, ∼48% of adult women in Bangladesh are illiterate [27]. Flooding is frequent and roads are routinely impassable during the monsoon season. The only public (government) hospital in Khulna Division is Khulna Medical College Hospital, which has two oncologists. The hospital suffers from extreme overcrowding, limited human resources, and inadequate infrastructure [6]. Although oncologists have dual training in medical and radiation oncology, the nearest public hospital with a functioning cobalt machine is in Barisal, which is approximately 3 hours by road, rendering this option effectively inaccessible for most rural patients. Although there are a few private clinics that offer diagnostic mammography and fine needle aspiration, to our knowledge, none outside of AGBC Centre perform diagnostic core biopsy, and none have access to high-quality hormone receptor testing. Rural Khulna Division would therefore fall into the Breast Health Global Initiative’s “Basic” resource tier [11]. The largest of the AGBC walk-in clinics is in Bagerhat District, with a population of ∼1.5 million in an area close to 4,000 km2. Bagerhat was chosen as the study intervention area (Figs. 1 and 2).
Figure 1.
Map of Bangladesh and its six administrative divisions.
Figure 2.
Study area map with insert.
Pilot Work
Pilot work (unpublished) was first undertaken to demonstrate the feasibility of the model, including training CHWs to take informed consent, use mobile phone applications for a guided interview and data reporting, perform a clinical breast examination (CBE), and refer women with abnormal breast exams to our clinic. We developed novel mobile phone applications to guide eight CHWs (who we recruited specifically for this project) to conduct a structured interview and report data to our central secure server. We also created a short “motivational” video, including testimonials from local women who have been patients at AGBC. The CHWs were instructed to offer a CBE only to women who answered “yes” to specific questions about their breast health (i.e., a lump in the breast or axillae, nipple retraction, skin erythema, or dimpling). This was therefore not a screening intervention but one of “case finding.” The pilot was funded by the IBCRF. Administrative approval was granted by the Bagerhat District Government Authority, as is the usual practice for public health programs with CHWs.
Eight CHWs were divided into four groups to test the feasibility of different models, which would presumably take different amounts of time, depending on model complexity: two carried phones with the basic mobile phone applications, two carried the same phones plus video, two carried phones and were instructed to do an extended interview for women with an abnormal breast examination to address potential barriers to seeking care, and two used paper and pen only (no phone, no video, no additional navigation). The latter was the control group, although the study was not powered for statistical comparison. In 128 workdays, the eight CHWs who completed our training program interviewed 3,150 women (aged 15 and older) from 2,356 households in eight villages. Only 3 women declined an interview. Manual data collection (“control”) was missing data in 80% of interviews, and took on average 5 minutes longer, compared with the three teams carrying mobile phones.
Materials and Methods
Based on our experience with the pilot, we designed a three-arm randomized controlled field intervention trial to determine whether our CHW-led mHealth platform (including motivational video and patient navigation) would improve the efficiency and efficacy of CHWs to interview women about breast health, identify those with an abnormal CBE, and encourage clinic attendance (“adherence”). We enhanced the CHW training curriculum, developed a more formalized “patient navigation” training program, and improved the mobile phone platform using smart phone technology for a field intervention trial. To our knowledge, this is the first CHW-led breast “mHealth” promotion intervention and the first to evaluate a CHW-led patient navigation model in a low-income country.
Study Arms
CHWs were randomized to one of three study arms:
Arm A: smart phone with applications to guide interview, report data, show motivational video, and offer an appointment for women with an abnormal CBE.
Arm B: smart phone platform as in arm A plus additional “patient navigation training.”
Arm C: control group (no smart phone). CHWs conducted the same interview and recorded data on paper.
Study Participants
Inclusion criteria were adult women aged 25 and older and living in the catchment area of Khulna Division, Bangladesh. Exclusion criteria were women younger than age 25 and women unable to give verbal consent.
Community Health Worker Recruitment and Training
We recruited and trained 30 CHWs from rural villages in Khulna Division, who were otherwise unemployed young women with a high school education. Three female CHW supervisors, also local women but with postsecondary education and prior experience in the health or social services sector, were hired to oversee daily work flow and to liaise with our field operations team. CHWs and supervisors attended an intensive 3-day training program, which was revised and expanded from that used in our pilot feasibility study.
Selected members of Amader Gram, AGBC, and mPower Health conducted the training. Each took part in sections appropriate to their skills set. The only non-Bangladeshi trainer was the principal investigator (O.M.G.). Two of AGBC’s female physicians carried out the sessions on breast anatomy, physiology, and pathology, as well as the 2-hour training session on CBEs. (It should be noted that no male team member was present during these sessions, at the request of the class.) The mobile phone training sessions were led by a senior member of mPower Health who has expertise in education and also community mobilization for social change (BCP).
CHWs were taught in a gentle, culturally sensitive manner how to obtain informed verbal consent, to ask the structured interview questions, and to perform a CBE. As with the interview, CBEs would be performed in private, in the household (see Ethical Considerations). A 2-hour session for CBE training was led by the female doctors and included hands-on training using the MammaCare training models, designed with varying degrees of difficulty in detecting benign and cancerous masses. Interview questions included basic individual and household demographics, followed by specific questions about breast health, such as “Do you have any problem with your breast?” and “Do you have any problem with one breast that is different from the other, such as a lump, nipple discharge or skin changes?” CHWs were instructed to offer a CBE only for women who disclosed a current breast symptom; separate consent was taken for the CBE. Participants with an abnormal CBE were offered an appointment at AGBC Centre (Khulna City) or our walk-in clinic in Bagerhat; they were encouraged to attend for care at either our clinics or a “local or government” doctor as appropriate. Training also included role-playing exercises, whereby each CHW (and supervisor) had the opportunity to explore how a study participant might respond to the information and consent discussions, interview questions, and breast examination.
Only the 10 CHWs randomized to arm B were given an extra day of training in patient navigation, which included additional questions for women with an abnormal CBE, such as “Is there any reason that you can think of which will prevent you from coming to your clinic appointment?” and “Do you need permission from your husband? in-laws?” The importance of nonverbal communication was emphasized. They were also instructed to offer specific enabling tasks, for example, to suggest accompanying the woman to her appointment or to return at a more suitable time to facilitate discussion with family members. Lastly, navigation training included role-playing exercises to ensure that CHWs would become familiar with the types of situations likely to be encountered.
Village Selection
The population structure and demographics were evaluated by the Amader Gram staff and were based on their analysis of previous work in Bagerhat District. The villages were selected and allocated to each study arm on their “best fit” of characteristics including geographical distance to the AGBC Centre, Bagerhat walk-in clinic, and Khulna City. Efforts were taken to ensure equitable allocation of villages to each CHW study arm.
Randomization Procedures
The 30 CHWs were randomized by manual lottery (by O.M.G., eyes closed, hand in jar with identical folded papers with CHW names) to one of the three study arms.
Smart Phone Platform
Given the limited availability of smart phones in the country at the time of the project launch, two very similar models were used: Samsung Galaxy Pop GT-S5570 (18 handsets, 9 for arm A and 9 for arm B) and Samsung Galaxy Young GT-S5360 (1 for arm A and 1 for arm B). The new mPower applications, based on Java-J2ME or Android software, were uploaded. Data were digitized in real time and sent to a secure server through GPRS connectivity to create a comprehensive and secure electronic dashboard.
Video
A 3.5-minute motivational video was developed by mPower and Amader Gram using testimonials by real patients previously seen at AGBC Centre. The video was uploaded to all smart phones for easy access and viewing by study subjects in arms A and B (available on YouTube, with English subtitles; http://www.youtube.com/watch?v=hwmyclLK_eQ).
Sample Size Calculation
From our early pilot data, the prevalence of an abnormal CBE was estimated at 1/400. We planned to interview a convenience sample of 20,000 women aged 25 and older to detect 50 women with a serious breast abnormality. We estimated an effect size of 45% between the smart phone study arms (A + B) versus control arm (C) in terms of adherence to CHW advice (i.e., a study participant with an abnormal exam who attends her scheduled appointment at AGBC Centre, Bagerhat walk-in clinic, or a local/government doctor, or within 1 month if patient rescheduled). The study was powered (80%) to detect a significant difference (p = .05) in our primary endpoint, with a 1:2 randomization (arm C/arms A + B).
Analysis
Descriptive statistics were used to report the number of women with abnormal CBEs and the adherence (clinic attendance) in each arm. We used the chi-square test to evaluate the primary endpoint: adherence rate for the mobile arms (arms A and B combined) versus control arm (arm C); the secondary endpoint was adherence in arm A (mobile) versus arm B (mobile + navigation). “Efficiency” described the number of women interviewed in each arm, by the end of accrual, as well as the degree of data completeness. “Efficacy” describes the adherence rates between arms.
Ethical Considerations
This study was approved by the Research Ethics Board at Women’s College Hospital, a teaching hospital of the University of Toronto. In Bangladesh, the study was approved by the local (Bagerhat) district government official. All CHW interactions with study participants, including obtaining informed verbal consent, were in Bengali. CHWs provided participants with contact information of the principal investigator, coinvestigators, and the CHW as well as AGBC.
Results
Following research ethics and district government approvals, we conducted the 3-day training course in Bagerhat, June 5–7, 2012. At the completion of the course, CHWs were randomized as described. An additional day of training in patient navigation was held June 18, 2012, only for the CHW supervisors and the 10 CHWs randomized to arm B. On July 1, CHWs were deployed in Bagerhat District.
In a 4-month period, the 30 CHWs interviewed 22,337 eligible women. Fewer than 1% of women declined the interview, and none withdrew consent at any point. No woman who disclosed that she had a breast symptom declined a CBE. Table 1 shows the sociodemographic characteristics of 22,337 participants. The mean age was 38 years (range: 25–88 years). Close to one third were over age 45; 97.13% were married. Age, monthly household expenditures (the income measure used widely in Bangladesh), highest education level attained for “household head,” and marital status (not shown) were balanced between study arms. However, compared with arms A and B, fewer women in arm C reported the highest quartile of household expenditures, and fewer arm C participants were illiterate. Sociodemographic data were incomplete for 19% of study participants interviewed in arm C (control CHWs), compared with only 1% from the CHWs in arms A and B.
Table 1.
Sociodemographic information of all study participants
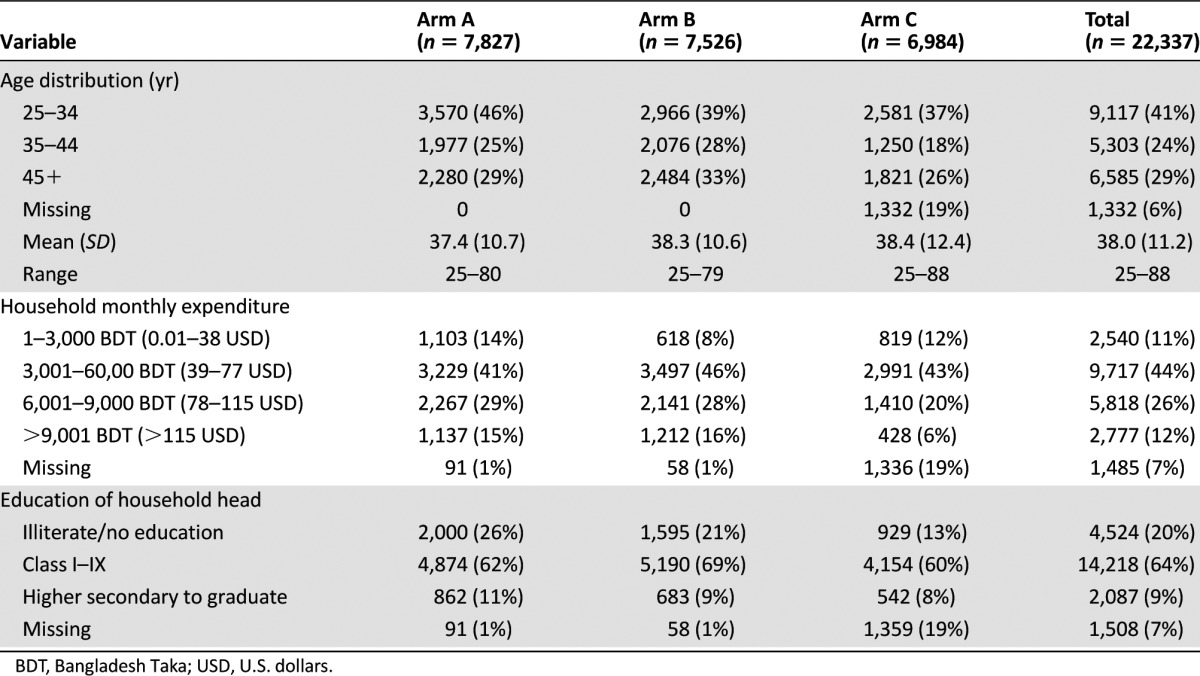
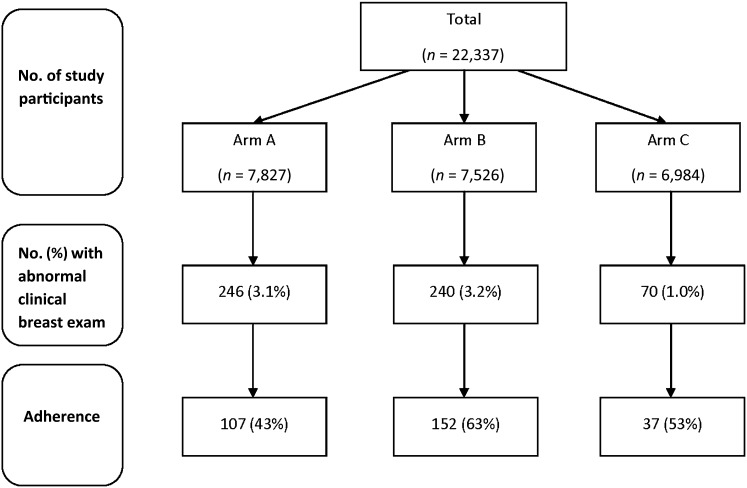
Figure 3 shows the number and proportion of study participants in each arm who had an abnormal CBE and those who adhered to CHW advice to attend their appointment (at AGBC Centre or with a local/government doctor). Over the 4-month accrual period, control arm CHWs interviewed fewer women than CHWs in either arm A or arm B. A total of 556 of 22,337 women had an abnormal CBE, of which only 70 were from the control arm. The proportion of study participants found to have an abnormal CBE was more than 3 times greater in arm A (3.1%) and arm B (3.2%) versus arm C (1.0%), p < .0001. Adherence was higher than expected in all three study arms and our primary endpoint; adherence in both arms A + B versus C was the same (53%). However, women in arm B (smart phones plus patient navigation) were significantly more likely to attend for care versus women in arm A (smart phones without navigation; 63% vs. 43%, p < .0001).
Figure 3.
Number of study participants who had an abnormal clinical breast examination and their adherence rate. Adherence is the percentage of participants with abnormal breast examination who attended clinic for assessment (includes Amader Gram Breast Care Centre/Bagerhat walk-in clinics and local clinic/government hospital).
We were able to determine final diagnoses for 67 of the 85 women who attended AGBC Centre or Bagerhat walk-in clinics. Forty-two women had no significant findings; other diagnoses included fibrocystic breasts (3), fibroadenoma (3), mastalgia (9), mastitis (7), breast abscess (1), fungal infection (1), enlarged breast (not diagnosed; 1). No clinical data are available for the 211 women who attended government or local doctors.
Discussion
We conducted a randomized controlled trial to test whether CHWs guided by smart phone applications would be more efficient and effective than CHWs without phones at encouraging women with an abnormal breast exam to adhere to advice regarding a clinic appointment. We also tested a patient navigation model by comparing clinic attendance for women interviewed by CHWs with and without an extra day of navigation training. CHWs in the control group interviewed fewer women, had inferior data completeness, and identified fewer women with possible breast abnormalities. Adherence was highest for women interviewed by CHWs with smart phones and who acted as patient navigators. The high level of community acceptance, initially demonstrated in the pilot feasibility study, was confirmed.
Significantly fewer study participants interviewed by control group CHWs had an abnormal breast examination (threefold less than their smart phone-guided counterparts). Based on extensive interviews with CHWs and supervisors, we believe there was likely a significant difference in disclosure of breast problems, most notably with arm C versus arms A and B. As noted below as a study limitation, we cannot provide direct evidence for this because of data incompleteness, particularly for arm C.
If disclosure was significantly different between the control arm and the mobile phone arms, a likely explanation is the motivational video, shown only in arms A and B. The video provided “peer-to-peer” communication and detail about what is involved in attending the center for care. It also included “testimonials” by patients seen at AGBC Centre and emphasized the importance of taking care of one’s health.
Arm B showed significantly improved adherence compared with arm A. This suggests that the patient navigation component of the model was more efficacious, particularly as the extra discussion offered only to those women found to have abnormal CBE did not negatively impact the overall number of interviews by the arm B CHWs; in other words, it did not seem to be counterbalanced by inefficiency.
Delayed presentation of breast cancer is common in LMICs [28–31]. Reasons for this are multifactorial and may include health systems issues; low priority of women’s health and cancer on the national health agenda; lack of awareness that breast cancer can be effectively treated if detected early; and societal, cultural, and religious factors [30–32]. Literature on effective breast health awareness interventions in rural LMICs is sparse, and breast screening in these settings remains unproven [9–11]. A number of promising approaches are currently being evaluated for breast cancer control in LMICs, including telemedicine, task-shifting, and institutional twinning. Breast health promotion and early detection interventions can also be “plugged into” an established program of care for other important health conditions [29, 31, 33, 34]. A recent study used volunteer health workers (without an mHealth component) to screen for breast cancer in rural Sudan [34]: 14,788 women were screened with CBE, of which 138 were referred to the district hospital; 118 attended for care; and of these, 9 were found to have breast cancer. In the observation group, only 3 women (who self-referred) during the same period were found to have breast cancer. This study highlights the challenges and opportunities for breast cancer control in rural low-income populations.
Despite the promise of mHealth to make a significant impact on individualized health assessment, reporting, and monitoring, there is a dearth of rigorous evaluation of such programs, not only in LMICs but also in high-income countries [35–37]. According to the World Health Organization 2009 Global Survey [25], “mHealth has the potential to transform the face of health service delivery across the globe”; however, only 12% of World Health Organization member states that participated in the survey (including Bangladesh) reported evaluation of projects. A policy white paper on mHealth in LMICs from the Earth Institute, Columbia University, also highlights growing criticism regarding the significant “research gap” in this and other analyses of mHealth programs [36]. Patient navigation programs for cancer are similarly in need of more rigorous evaluation [38].
Strengths of our study include the randomized controlled design, powered to demonstrate a difference between interventions, including a control group of CHWs without phones. CHWs in this study were paid employees, with wages commensurate with those of other projects in Bangladesh. Their daily workflow was closely monitored by the CHW supervisors and, for the two mobile phone arms, could be tracked in real time. Accounting for inclement weather, religious and public holidays, and frequent national strikes, we anticipated that our recruitment target would be reached by 6–8 months. However, in 4 months we surpassed our accrual goals. We had the benefit of longstanding community trust, as Amader Gram is well known for providing training in basic computer skills, which has led to better employment for male and female graduates in rural Khulna. In the first 2 weeks after the CHW recruitment announcement was posted, we had more than 100 applicants for the 30 positions. Those who were selected for interviews but who were not ultimately hired were offered free computer training with Amader Gram. Since completion of their 6-month employment contract, 10 of the CHWs and two of the supervisors have been hired back for other Amader Gram positions.
This study had important limitations. We were unable to track the final diagnoses of women with abnormal breast exams who attended for care at a local or government doctor and for some women who attended AGBC Centre. Given data incompleteness particularly for the control arm, we were also unable to adequately document the proportion of women in each arm who disclosed having a current breast problem.
Regarding scale-up and potential for sustainability, it will be important to include another geographical region in a “transition-to-scale” project. This study was based in Khulna Division, where we anticipated a great degree of community trust because of Amader Gram’s well-established and highly regarded program in Information and Communication for Development. It will be also be critical to demonstrate that a surrogate marker for breast cancer-specific survival, such as clinical down-staging, can be achieved prior to scaling the model more widely. Challenges will thus include ensuring that the “loop” is closed adequately, from suspected breast abnormality to referral, accurate and timely diagnosis, staging, treatment planning, and completion of evidence-based, resource-appropriate treatment and follow-up. Plans are in development for such a project to demonstrate adaptability with the potential for nationwide deployment.
Conclusion
The current report suggests that even with minimal cancer control infrastructure a locally based, multidisciplinary project team can begin to address barriers to seeking care for breast symptoms. Although capacity for cancer care and control is developing in many major urban centers in LMICs, there remains a pressing need to address the increasing gap in cancer services in rural areas. This can begin with cancer awareness, addressing sociocultural barriers and overcoming cancer myths. To our knowledge, this is the first such program for breast cancer awareness in a low-income country that used a “CHW-mHealth” model of care. We believe that this is also the first study to report a patient navigation model for breast health in a low-income country. In order to make rapid and lasting impact on breast cancer control in low-income countries such as Bangladesh, concerted interdisciplinary efforts are needed, including rigorous evaluation prior to scale-up.
Acknowledgments
We thank Dr. Richard R. Love, Dr. Syed Mozammel Hossain, Dr. Naznin Nahar, and Chameli Akhter. Pilot work was funded by the International Breast Cancer Research Foundation. Dr. Ginsburg’s work is supported by a Rising Stars in Global Health award from Grand Challenges Canada.
Author Contributions
Conception/Design: Ophira M. Ginsburg, Mridul Chowdhury, Md Touhidul Imran Chowdhury, Bidhan Chandra Pal, James H. Woods, Reza Salim
Provision of study material or patients: Mridul Chowdhury, Bidhan Chandra Pal, Raiyan Al-Mansur, Sahin Mahmud, Reza Salim
Collection and/or assembly of data: Mridul Chowdhury, Bidhan Chandra Pal, Zahid H. Khan, Dali Dutta, Raiyan Al-Mansur, Sahin Mahmud,
Data analysis and interpretation: Ophira M. Ginsburg, Mridul Chowdhury, Wei Wu, Bidhan Chandra Pal, Rifat Hasan, Dali Dutta, Arif Abu Saeem, Heather H. Story, James H. Woods, Reza Salim
Manuscript writing: Ophira M. Ginsburg, Mridul Chowdhury, Wei Wu, Md Touhidul Imran Chowdhury, Heather H. Story, James H. Woods
Final approval of manuscript: Ophira M. Ginsburg, Mridul Chowdhury, Wei Wu, Md Touhidul Imran Chowdhury, Bidhan Chandra Pal, Zahid H. Khan, Dali Dutta, Arif Abu Saeem, Heather H. Story, James H. Woods, Reza Salim
Disclosures
The authors indicated no financial relationships.
References
- 1.Globocan 2012. Available at http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx Accessed August 6, 2013.
- 2.SEER Stat Fact Sheets: Breast Cancer. Available at http://seer.cancer.gov/statfacts/html/breast.html#survival Accessed August 6, 2013.
- 3.SEER Stat Fact Sheets: Cervix Uteri Cancer. Available at http://seer.cancer.gov/statfacts/html/cervix.html#survival Accessed August 6, 2013.
- 4.Sankaranarayanan R, Swaminathan R, Brenner H, et al. Cancer survival in Africa, Asia, and Central America: A population-based study. Lancet Oncol. 2010;11:165–173. doi: 10.1016/S1470-2045(09)70335-3. [DOI] [PubMed] [Google Scholar]
- 5.Ginsburg OM, Love RR. Breast cancer: A neglected disease for the majority of affected women worldwide. Breast J. 2011;17:289–295. doi: 10.1111/j.1524-4741.2011.01067.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Story HL, Love RR, Salim RR, et al. Improving outcomes from breast cancer in a low-income country: lessons from Bangladesh. Int J Breast Cancer. 2012;2012:423562. doi: 10.1155/2012/423562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Transparence International. Corruption by Country/Territory. Available at http://www.transparency.org/country#BGD Accessed August 5, 2013.
- 8.Thomas DB, Gao DL, Ray RM, et al. Randomized trial of breast self-examination in Shanghai: Final results. J Natl Cancer Inst. 2002;94:1445–1457. doi: 10.1093/jnci/94.19.1445. [DOI] [PubMed] [Google Scholar]
- 9.Pisani P, Parkin DM, Ngelangel C, et al. Outcome of screening by clinical examination of the breast in a trial in the Philippines. Int J Cancer. 2006;118:149–154. doi: 10.1002/ijc.21343. [DOI] [PubMed] [Google Scholar]
- 10.Al-Foheidi M, Al-Mansour MM, Ibrahim EM. Breast cancer screening: Review of benefits and harms, and recommendations for developing and low-income countries. Med Oncol. 2013;30:471. doi: 10.1007/s12032-013-0471-5. [DOI] [PubMed] [Google Scholar]
- 11.Yip C-H, Smith RA, Anderson BO, et al. Breast Health Global Initiative Early Detection Panel Guideline implementation for breast healthcare in low- and middle-income countries: Early detection resource allocation. Cancer. 2008;113(suppl):2244–2256. doi: 10.1002/cncr.23842. [DOI] [PubMed] [Google Scholar]
- 12.Globocan 2012. Available at http://globocan.iarc.fr/Pages/fact_sheets_population.aspx Accessed August 6, 2013.
- 13.Cancer Registry Report—National Institute for Cancer Research and Hospital 2005–2007. National Institute of Cancer Research and Hospital, Dhaka, Bangladesh, 2009. Available at http://www.ban.searo.who.int/LinkFiles/Publication_Cancer_Registry_Report.pdf Accessed August 9, 2013.
- 14.IBCRF. Available at http://ibcrf.org/ Accessed August 13, 2013.
- 15.AGBC Centre. Available at http://www.agbreastcare.org Accessed August 6, 2013.
- 16.AGBC Centre. Available at http://www.agbreastcare.org/wp-content/uploads/2013/06/Amader_Gram_CPG_Practise_Guidlines.pdf Accessed August 6, 2013.
- 17.mPower. Available at http://www.mpower-social.com Accessed August 6, 2013.
- 18.Digital Bangladesh. Available at http://en.wikipedia.org/wiki/Vision_2021#Digital_Bangladesh Accessed August 11, 2013.
- 19.World Fact Book. Available at https://www.cia.gov/library/publications/the-world-factbook/geos/bg.html Accessed August 11, 2013.
- 20.Grameen Foundation. Available at http://www.grameenfoundation.org/ Accessed August 11, 2013.
- 21.MAMA Bangladesh—Connecting Health Information and Services to Mothers Through Mobiles. Available at http://blog.usaid.gov/2012/04/mama-bangladesh-connecting-health-information-and-health-services-to-mothers/ Accessed August 11, 2013.
- 22.mHealth Alliance. Available at http://www.mhealthalliance.org/media-a-resources/press-releases/56-bangladesh-launches-national-mobile-health-service-aponjon-to-reach-2-million-moms-by-2015 Accessed August 7, 2013.
- 23.Next Billion. Bangladesh’s Mobile Tech Surge, What It means for Development. Available at http://www.nextbillion.net/blogpost.aspx?blogid=2446 Accessed August 7, 2013.
- 24.UNICEF. In Remote Regions of Bangladesh, Community Health Workers Break Barriers to Healthcare. Available at http://www.unicef.org/infobycountry/bangladesh_66012.html Accessed August 6, 2013.
- 25.mHealth: New Horizons for Health Through Mobile Technologies: Based on the Findings of the Second Global Survey on eHealth (Global Observatory for eHealth Series, Volume 3). 2011. World Health Organization. ISBN: 978-92-4-156425-0. Available at http://whqlibdoc.who.int/publications/2011/9789241564250_eng.pdf Accessed August 7, 2013.
- 26.World Bank. Available at http://data.worldbank.org/indicator/SI.POV.2DAYAccessed August 6, 2013.
- 27.World Bank. Available at http://data.worldbank.org/country/bangladesh Accessed August 6, 2013.
- 28.Vorobiof DA, Sitas F, Vorobiof G. Breast cancer incidence in South Africa. J Clin Oncol. 2001;19(suppl):125S–127S. [PubMed] [Google Scholar]
- 29.Errico KM, Rowden D. Experiences of breast cancer survivor-advocates and advocates in countries with limited resources: A shared journey in breast cancer advocacy. Breast J. 2006;12(suppl 1):S111–S116. doi: 10.1111/j.1075-122X.2006.00208.x. [DOI] [PubMed] [Google Scholar]
- 30.Price AJ, Ndom P, Atenguena E, et al. Cancer care challenges in developing countries. Cancer. 2012 doi: 10.1002/cncr.26681. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 31.Knaul FM, Atun R, Bhadelia A. Closing the Cancer Divide: An Equity Imperative. Cambridge, MA: Harvard Global Equity Initiative; 2012. [Google Scholar]
- 32.Ginsburg OM. Breast and cervical cancer control in low and middle-income countries: Human rights meet sound health policy. J Cancer Policy. in press. [Google Scholar]
- 33.UNAIDS. Available at http://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2011/september/20110913pinkribbonredribbon/. Accessed August 9, 2013
- 34.Abuidris DO, Elsheikh A, Ali M, et al. Breast-cancer screening with trained volunteers in a rural area of Sudan: A pilot study. Lancet Oncol. 2013;14:363–370. doi: 10.1016/S1470-2045(12)70583-1. [DOI] [PubMed] [Google Scholar]
- 35.Free C, Phillips G, Watson L, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: A systematic review and meta-analysis. PLoS Med. 2013;10:e1001363. doi: 10.1371/journal.pmed.1001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mechael PN, Batavia H, Kaonga N et al. Barriers and gaps affecting mHealth in low- and middle-income countries. Policy white paper. New York, NY: Columbia University, 2010. Available at http://cghed.ei.columbia.edu/sitefiles/file/mHealthBarriersWhitePaperFINAL.pdf Accessed August 7, 2013.
- 37.SciDev.Net. Evidence Lacking on mHealth Effectiveness in Poor Countries. Available at http://www.scidev.net/global/health/news/evidence-lacking-on-mhealth-effectiveness-in-poor-countries.html Accessed August 7, 2013.
- 38.Paskett ED, Harrop JP, Wells KJ. Patient navigation: An update on the state of the science. CA Cancer J Clin. 2011;61:237–249. doi: 10.3322/caac.20111. [DOI] [PMC free article] [PubMed] [Google Scholar]