Abstract
Purpose:
To evaluate serially long-term macular morphologic changes after successful macula-involving rhegmatogenous retinal detachment repair and correlate changes with macular function.
Methods:
Repeat Fourier domain optical coherence tomography (FD OCT) imaging and microperimetry (MP-1) testing of 8 of the initial cohort of 17 eyes studied 5 years earlier.
Results:
The mean follow-up after rhegmatogenous retinal detachment repair was 3.4 months (range, 1–8.5 months) for the first FD OCT and 5 years (range, 3.75–5.75 years) for the follow-up FD OCT. The final postoperative best-corrected visual acuity mean was 20/201 (range, 20/20 to counting fingers). Six eyes with final best-corrected visual acuity >20/40 had an intact external limiting membrane and progressive resolution of photoreceptor inner segment–outer segment junction disruption and/or subretinal fluid on serial FD OCT, which correlated with improvement in macular function on MP-1. Two eyes with poor or worsening best-corrected visual acuity on follow-up had persistent or worsening inner segment–outer segment disruption on serial FD OCT. External limiting membrane was intact in one eye and persistently disrupted in the other.
Conclusion:
Macular function may progressively improve or worsen long-term after successful rhegmatogenous retinal detachment repair. Progressive resolution of subretinal fluid and/or inner segment–outer segment disruption on FD OCT correlated with improvement in macular function, whereas worsening or persistent inner segment–outer segment disruption correlates with worsening or persistently poor visual outcome.
Keywords: external limiting membrane, Fourier domain optical coherence tomography, microperimetry, photoreceptor, rhegmatogenous retinal detachment, spectral domain optical coherence tomography
Rhegmatogenous retinal detachment (RRD) is a fairly common sight-threatening disease with an estimated incidence rate of 17.9 per 100,000 persons in the United States.1 Despite successful anatomical repair, visual acuity usually does not return to baseline when the RRD involves the macula preoperatively. This has been attributed to various factors such as epiretinal membrane (ERM), presence of residual postoperative subretinal fluid (SRF), cystoid macular edema, macular hole, retinal folds, pigment migration, and duration of retinal detachment before surgical repair.2-6
Time domain optical coherence tomography (TD OCT; Stratus, Carl Zeiss Meditec, Inc., Dublin, CA) has been used in the past to study changes in macular morphology 1 month to 24 months after successful repair of RRD involving the macula.6,7 Persistent subfoveal fluid after repair and increased preoperative foveal thickness were found to be OCT features associated with worse visual outcome after surgery.6 However, another study by Seo et al7 contradicted this finding by reporting that the presence and extent of submacular fluid after successful scleral buckle surgery for macula-involving RRD did not influence final visual acuity.
With the introduction of Fourier domain OCT (FD OCT), that is, spectral domain OCT, with image acquisition speeds of ~100 times or faster than TD OCT and axial resolution of 3 μm to 5 μm (compared with 10 μm axial resolution of TD OCT), photoreceptor layer inner segment/outer segment (IS/OS) disruptions were reported by several groups after successful repair of RRD.8-16 These changes could not be realized well using TD OCT.13 Serial FD OCT macular imaging at 1 month to 6 months after successful repair of RRD showed that resolution of macular IS/OS disruption correlated with subsequent visual acuity improvement.13 Serial FD OCT imaging 1 month to 25 months after RRD repair showed the importance of external limiting membrane (ELM) integrity in predicting subsequent IS/OS restoration and visual acuity recovery after RRD repair.12
In this study, a research-grade FD OCT constructed at our institution was used to study serially the morphologic changes in the macula 5 years after successful repair of macula-involving RRD. This FD OCT instrument produces axial image resolution of 4.5 μm, a somewhat higher image resolution than current commercially available FD OCT systems.8,9 The same FD OCT system was used 5 years earlier to study macular morphologic changes noted within 1 year after successful RRD repair.13 This earlier study was the first study to use FD OCT to study this condition and concluded that there is a strong correlation between decreased macular function on microperimetry (MP-1) and the presence of photoreceptor disruption or SRF on FD OCT.13 The current study using the same original cohort is the longest follow-up study to date using this imaging system to evaluate serially the long-term macular morphologic changes after successful anatomical repair of macula-off RRD.
Methods
This study is a prospective observational follow-up study of 17 patients who were enrolled 5 years earlier and imaged with the same research-grade FD OCT instrument used in the current study.13 The original 17 patients were selected after a chart review of patients seen at the University of California Davis Eye Center between January 2005 and December 2006 for primary macula-off RRD.13 These patients had successful repair of RRD with two or fewer procedures or surgeries.13 Exclusion criteria included dense ocular media, preexisting macular conditions (e.g., age-related macular degeneration), and clinically evident postoperative changes (e.g., cystoid macular edema and significant ERM) that were likely to adversely affect visual outcome. Written informed consent was obtained before imaging. The study was conducted according to a protocol approved by the Office of Human Research Protection at the University of California Davis School of Medicine.
Of the original cohort of 17 patients, 8 patients were eligible and willing to participate in this long-term follow-up study using FD OCT imaging and microperimetry (MP). The patients for the current study were enrolled from October 15, 2010 to May 20, 2011 after obtaining a second informed consent.
Demographic data collected included age, sex, ocular history, duration of preoperative symptoms, extent of RRD, and surgical details. Best-corrected visual acuity (BCVA) by Snellen chart, anterior segment examination, and dilated fundus examination with indirect and slit-lamp biomicroscopy were performed on all patients.
The study eyes were imaged with the same research-grade FD OCT system used in our earlier study.13 Briefly, these images were acquired using a broad bandwidth superluminescent diode light source (model D855; Superlum, Diode Ltd., Moscow, Russia). Measured axial resolution was 4.5 μm, and estimated transverse resolution was 10 μm to 15 μm. A set of 100 B-scans (1,000 A-scans/B-scan, 24 frames per second), covering a 6 × 6 × 2-mm volume of macula (lateral × lateral × depth), was acquired for each patient in ~4 seconds.
Four patients also underwent functional vision testing with the MP-1 Microperimeter (Nidek Technologies Nidek Technologies, Padova, Italy) as was done in our previous study.13 Four patients were unable to perform the test because of poor fixation. The central 20° was tested in patients with undilated pupils using a Goldmann size-III stimulus and 4-2-1 staircase as described previously.13 Fixation was tracked by the infrared camera, and the visual field was projected onto the corresponding fundus photograph. The test was considered reliable if >80% and >90% of fixation points were within 2° and 4° of center, respectively.
Results
Among the original 17 subjects who were imaged with FD OCT, 8 eyes from 8 subjects were imaged for the second time with the same FD OCT to study the long-term morphologic changes in the macula after successful RRD repair. Tables 1 and 2 summarize the demographic and clinical data for these 8 subjects. The mean postoperative follow-up duration at the time of the initial FD OCT scan for these 8 subjects was 3.4 months (range, 1–8.5 months). The mean postoperative follow-up for the final FD OCT scan was 5.0 years (range, 3.75–5.75 years).
Table 1.
Demographic Data for Patients With Rhegmatogenous Retinal Detachment
| Patients Number |
Age at Time of RRD/ Gender |
Duration of RRD Before Repair |
Location of RRD | Number of Clock Hours of RRD Involved |
Procedure | Additional Procedure |
|---|---|---|---|---|---|---|
| 1 | 56/M | Unknown | Superotemporal HST and 1 quadrants of RRD |
4 | Pneumatic retinopexy with cryotherapy |
Recurrent macula-on RRD at POW#4, s/p repeat cryotherapy and pneumatic |
| 2 | 64/M | 7 days | Superotemporal HST and 1 quadrants of RRD |
2 | Pneumatic retinopexy with cryotherapy |
None |
| 3 | 58/F | 2 days | Multiple superior and inferior breaks with inferior 2 quadrants of RRD |
12 | Scleral buckle and cryotherapy |
None |
| 4 | 57/M | 7 days | Superotemporal HST and 1 quadrant of RRD |
5 | Pneumatic retinopexy with laser |
None |
| 5 | 50/F | 2 days | Superotemporal hole; superior 1 quadrants of RRD |
4 | Pneumatic retinopexy with cryotherapy |
None |
| 6 | 51/M | 10 days | Superotemporal HST and 1 quadrants of RRD |
4 | Pneumatic retinopexy with cryotherapy |
Recurrent RRD at 1 week, s/p repeat pneumatic and cryotherapy |
| 7 | 38/F | 2 months | Inferior 2 quadrants of RRD |
4 | Scleral buckle, cryotherapy, and external drainage |
None |
| 8 | 68/F | 1 day | Multiple inferior breaks with inferior 2 quadrants of RRD |
4 | Pars plana vitrectomy, scleral buckle |
History of 2 superior RRD, 5 months and 1 year prior, s/p pneumatic and cryotherapy X2 |
HST, horseshoe tear; POW, postoperative week; s/p, status post.
Table 2.
Clinical and FD OCT Findings on Initial (Short-term) Scan and Final (Long-term) Scan After Rhegmatogenous RRD Repair
| Patient Demographics |
Follow-up Duration Post-RRD Repair |
VA |
||||
|---|---|---|---|---|---|---|
| Patient Number |
Age/ Gender |
Initial Scan (Months) |
Final Scan (Years) |
Preoperative VA |
Postoperative VA (Initial Scan) |
Postoperative VA (Final Scan) |
| 1 | 60/M | 2.5 | 3.75 | 20/150 | 20/25 | 20/20 |
| 2 | 70/M | 2 | 5.4 | CF | 20/50 | 20/30 |
| 3 | 62/F | 1 | 5.75 | CF | 20/60 | 20/25 |
| 4 | 63/M | 2 | 5.3 | CF | 20/40 | 20/25 |
| 5 | 50/F | 6 | 5.75 | 20/150 | 20/20 | 20/20 |
| 6 | 51/M | 8.5 | 4.8 | HM | 20/20 | 20/20 |
| 7 | 38/F | 2.5 | 4.9 | CF | CF | CF |
| 8 | 68/M | 3 | 4.18 | 20/80 | 20/25 | 20/40 |
HM, hand motions; VA, visual acuity.
The duration of vision loss secondary to RRD before surgical repair ranged from 1 day to 2 months (Table 1). In one patient, the duration of vision loss from retinal detachment was unknown. The short- and long-term visual outcomes after RRD repair are summarized in Table 2. The mean preoperative Snellen BCVA among these 8 eyes was 20/941 (range, 20/80 to hand motions). The mean BCVA at the initial postoperative FD OCT imaging was 20/209 (range, 20/20 to counting fingers [CF]). The mean BCVA at the final postoperative FD OCT imaging was 20/201 (range, 20/20 to CF). Three patients had an inferior retinal detachment successfully repaired after one surgery. The other five patients had superior retinal detachments repaired with pneumatic retinopexy combined with retinal cryopexy or laser retinopexy. Among these 5 patients, 2 patients required repeat pneumatic retinopexy for recurrent retinal detachment not involving the macula at 1 and 2 weeks after the initial pneumatic retinopexy. Both eyes were successfully treated with repeat pneumatic retinopexy and retinal cryopexy.
Table 3 summarizes the preoperative and postoperative clinical and morphologic FD OCT findings of the patients at the time of the initial and final scan. These patients can be subdivided into two groups: Group 1 consisting of patients with excellent visual outcome with persistent or progressively improved visual outcome (i.e., 6 patients) and Group 2 consisting of patients with poor visual outcome with persistent or progressive vision loss (i.e., 2 patients).
Table 3.
Macular Morphology Results Visualized Using FD OCT at Initial (Short-term) and Final (Long-term) Follow-up Examination
| Patient Number |
Macular Morphology on Initial FD OCT Scan |
Macular Morphology on Final FD OCT Scan |
||||||
|---|---|---|---|---|---|---|---|---|
| SRF | IS/OS | ERM | ELM | SRF | IS/OS | ERM | ELM | |
| 1 | None | Minimal disruption |
Absent | Normal | None | Complete restoration | Absent | Normal |
| 2 | Present | Disruption | ERM with mild retinal thickening |
Normal | Resolved | Complete restoration | Persistent ERM with mild retinal thickening |
Normal |
| 3 | Present | Disruption | Present; no CME | Normal | Resolved | Complete restoration, subfoveal, partial restoration extrafoveal |
Persistent ERM; no CME | Normal |
| 4 | None | Disruption | Absent | Normal | None | Partial restoration | Absent | Normal |
| 5 | Present | Normal | Absent | Normal | Resolved | Normal | Absent | Normal |
| 6 | None | Normal | Absent | Normal | None | Normal | Absent | Normal |
| 7 | None | Disruption | Absent | Normal | None | Multiple persistent disruptions |
New ERM; no CME | Normal |
| 8 | None | Disruption | Absent | Subfoveal disruption |
None | Worsening disruption | New ERM; no CME | Persistent disruption |
CME, cystoid macular edema.
Group 1: Patients with Good and/or Improving Visual Outcome
Among the 6 patients (Patients 1 through 6) with excellent visual outcome with persistent or progressively improving BCVA after successful RRD repair, preoperative BCVA ranged from 20/150 to hand motions and the duration of vision loss before repair ranged from 2 days to 10 days (unknown in 1 patient). Five patients in this group had retinal detachment repaired by pneumatic retinopexy, combined with retinal cryopexy or laser retinopexy. One patient had scleral buckle surgery with retinal cryopexy. The duration of retinal detachment was 10 days or less in all eyes (Table 1). Two of these patients had a history of a retinal detachment (macular sparing) that had been repaired with pneumatic retinopexy.
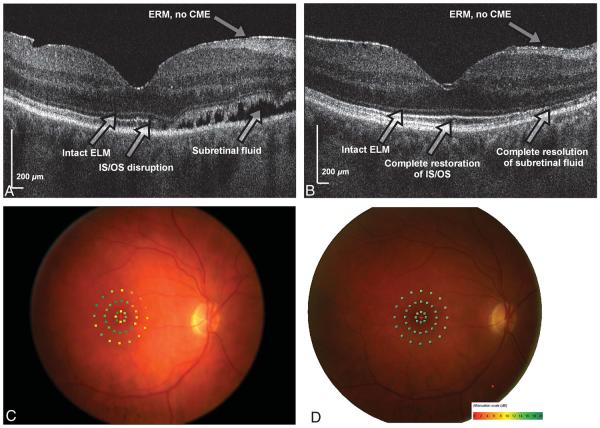
Postoperative BCVA at the time of the initial FD OCT ranged from 20/20 to 20/60 among these 6 eyes, with 4 eyes having BCVA worse than 20/20 (Patients 1, 2, 3, and 4) at the time of the initial FD OCT scan. All these 4 patients had foveal photoreceptor IS/OS disruptions noted on the initial postoperative FD OCT images (Figure 1A). These photoreceptor changes resolved partially (Patient 4) or completely (Patients 1, 2, and 3) on the follow-up postoperative FD OCT scan, concurrent with progressive improvement in BCVA in all 4 eyes (Figure 1B). Patient 3 was noted with mild residual IS/OS disruption in the peripheral macula, not affecting the fovea. Of note, all six patients had an intact ELM on the initial postoperative FD OCT scan. Subretinal fluid was present in 2 patients that completely resolved on the final follow-up FD OCT image (Figure 1, A and B). The final postoperative BCVA was 20/30 or better in all 6 eyes in this group, despite the presence of an ERM noted in 2 eyes (Patients 2 and 3) and mild associated macular thickening in 1 eye (Patient 2).
Fig. 1.
Fourier domain OCT and microperimetric findings of Patient 3 with progressive improvement in BCVA at 5.75 years after RRD repair. The BCVA at the time of the initial FD OCT scan 1 month after surgical repair was 20/60. Fourier domain OCT shows diffuse disruption of the photoreceptor IS/OS junction line with an intact ELM and SRF (A). The BCVA improved to 20/25 when the second FD OCT image was obtained at 5.75 years (B). Note that the IS/OS line is intact expect for some mild disruption in the peripheral macula. External limiting membrane is also intact. Microperimetry (MP-1) done at the time of the first FD OCT scan shows areas of decreased sensitivity (yellow dots) in the macula (C) that correlated with the region of the macula with SRF and/or IS/OS disruption noted on FD OCT. Follow-up MP-1 (D) obtained 5.75 years after surgical repair shows almost complete normalization of macular sensitivity.
Follow-up MP-1 testing was performed on Patients 3 and 4. Areas of the macula with restoration of IS/OS and resolution of SRF correlated with areas of improved sensitivity on MP in both patients (Figure 1, C and D). Patients 1 and 2 were not available for MP testing.
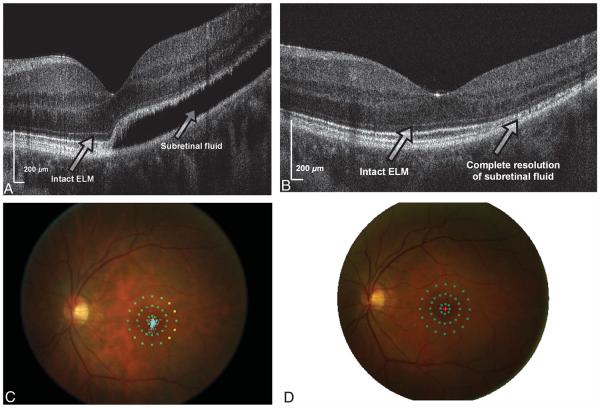
The remaining 2 patients in this group (Patients 5 and 6), who had BCVA 20/20 at the time of both the initial and the final FD OCT imaging, had intact IS/OS junctions and ELM on both the initial and final FD OCT scans (Figure 2, A and B). Patient 5 had SRF noted on the initial FD OCT scan that corresponded to areas of decreased sensitivity on MP-1 (Figure 2C), as reported in our previous study.13 At follow-up of 5.75 years, there was complete resolution of the SRF on FD OCT (Figure 2B) with normalization of macular sensitivity on follow-up MP-1 (Figure 2D).
Fig. 2.
Fourier domain OCT imaging and microperimetry of Patient 5. The initial postoperative FD OCT scan shows SRF and an intact photoreceptor IS/OS junction and ELM. The BCVA was 20/20 (A). The final follow-up FD OCT scan at 5.75 years after surgical repair showed complete resolution of SRF, and BCVA remained at 20/20 (B). MP-1 performed at the time of the initial FD OCT scan showed areas of decreased sensitivity in the temporal macula (yellow dots) (C) where SRF was noted on FD OCT. The final follow-up MP-1 scan showed normalization of macular sensitivity (green dots) concurrent with resolution of SRF on FD OCT (D).
Of interest, Patient 6 had intact IS/OS and ELM on the initial and final scans and visual acuity remained at 20/20. However, the patient had some decreased sensitivity on MP-1 scanning initially at 8.5 months, which did not correspond to any anatomical abnormality via FD OCT. These abnormalities on MP-1 completely resolved at 4.8-year follow-up MP-1 testing.
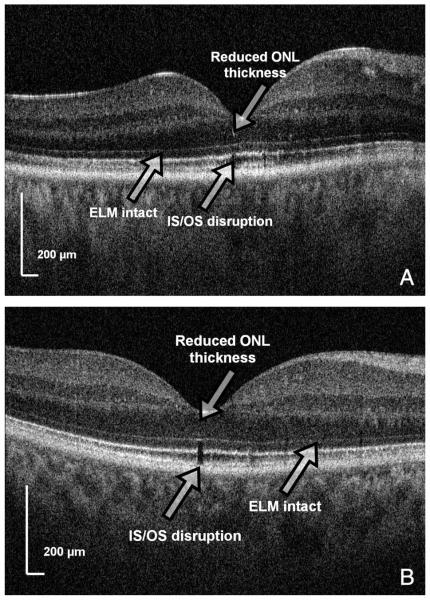
Group 2: Patients with Persistently Poor and/or Worsening Visual Outcome
Among the 2 patients in this group, Patient 7 had severely decreased BCVA at CF preoperatively, which failed to improve postoperatively 4.9 years after successful repair of RRD. This patient had the longest duration of retinal detachment (i.e., 2 months) before repair of RRD among our study subjects and had scleral buckle surgery requiring retinal cryopexy. The initial FD OCT scans acquired 2.5 months after repair of RRD showed multiple areas of photoreceptor IS/OS junction disruption extending into the fovea with an intact ELM (Figure 3A). The follow-up postoperative FD OCT image obtained 4.9 years after successful surgical repair showed that the subfoveal IS/OS junction disruption was persistent and more evident with an intact ELM (Figure 3B). Additionally, a new ERM was seen at the final follow-up FD OCT image, without associated macular traction or edema. Of interest, the outer nuclear layer thickness was decreased on both the initial and final FD OCT scans (Figure 3, A and B). The final BCVA remained CF. MP-1 could not be performed because of poor fixation.
Fig. 3.
Fourier domain OCT findings of Patient 7 with persistently decreased visual acuity to CF at 5 years after RRD repair. An intact ELM with a focal foveal disruption of the photoreceptor IS/OS junction is noted 2.5 months after surgical repair (A). The BCVA remained CF at 4.9 years after RRD repair when the follow-up FD OCT was obtained showing a more prominent foveal IS/OS junction with an intact ELM (B). The outer nuclear layer (ONL) appears attenuated in both FD OCT images. This patient had RRD present for 2 months before repair.
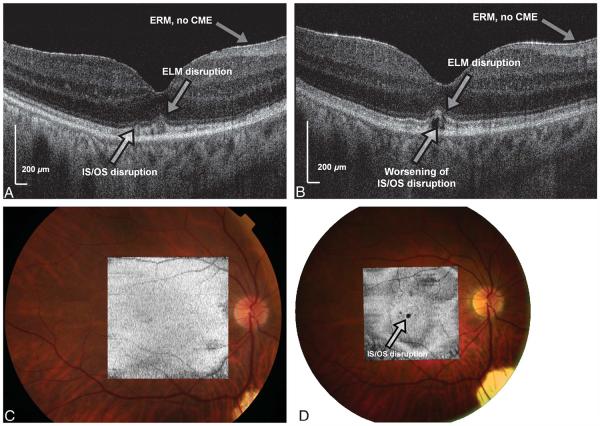
Patient 8 had 2 previous episodes of superior macular-sparing retinal detachment that had been successfully repaired with pneumatic retinopexy. The preoperative BCVA was 20/80. One day after vision loss secondary to RRD involving the macula, successful repair was achieved with a combination of vitrectomy and scleral buckle surgery. The BCVA improved to 20/25 postoperatively 3 months after successful repair. The initial FD OCT scan showed subtle areas of foveal IS/OS junction and ELM disruption (Figure 4, A and C).
Fig. 4.
Fourier domain OCT findings of Patient 8 with initial transient improvement in BCVA after surgical repair of RRD. The initial postoperative FD OCT image obtained 3 months after surgical repair showed subtle foveal IS/OS and ELM disruption and irregularity (A). The BCVA was 20/25. The final follow-up FD OCT scan obtained 4.2 years after surgery showed worsening foveal IS/OS and ELM disruption (B). The BCVA declined to 20/40. The C-scan superimposed on fundus photograph at 3 months postoperative scan and at the final follow-up showing the evolution of focal foveal IS/OS disruption in the macula (C and D).
The BCVA subsequently declined to 20/40 at 4.2-year follow-up. The final follow-up FD OCT image revealed an increase in foveal IS/OS junction disruptions when compared with the initial scan image (Figure 4, B–D), with worsening disruption of foveal ELM. In addition, a new ERM was noted on FD OCT without macular traction or edema. MP-1 could not be performed reliably on this patient because of poor fixation. The worsening of the visual acuity could not be accounted for by any other eye findings.
Discussion
This is the longest prospective follow-up study to date of patients with successful anatomical repair of RRD involving the macula imaged serially with FD OCT. Our study is also the only study thus far where visual function was assessed by both microperimetry and BCVA and correlated with FD OCT findings serially. A research-grade FD OCT and microperimetry (MP-1) used in the original cohort was again used for direct comparison in this follow-up study.13 The research-grade FD OCT instrument used in this study provides a somewhat higher axial image resolution than the currently commercially available FD OCT (spectral domain OCT) instruments. Our previous study published in 2008 was the first report using FD OCT to correlate areas of photoreceptor disruption and persistent SRF with decreased macular function on microperimetry.13 The current study was undertaken to further understand the long-term morphologic and functional changes in the macula in eyes after successful macular-involving RRD repair.
In our study, we found that BCVA may improve or worsen long-term after RRD repair. The disruption of photoreceptor IS/OS is found to be the most important correlate of visual acuity and function in the early postoperative period and long-term follow-up. A previous study using serial FD OCT scan from 1 month to 25 months after surgical repair also found that the photoreceptor IS/OS junction integrity was an important factor correlation in visual restoration in eyes after repair of macula-involving RRD.12 The mean postoperative follow-up period for our current study was much longer at 5 years (range, 3.75–5.75 years). With this longer follow-up, our study shows that IS/OS disruption and macular function can gradually improve, but some eyes can have persistent or worsening IS/OS disruption with extended follow-up in the absence of other visually significant macular pathology. This latter finding is new.
The back reflection arising from the IS/OS junction represents the abrupt boundary between the IS structures and highly organized OS of the photoreceptor layer. One hypothesis suggests that the hyperreflective IS/OS line is because of back reflection of the perpendicular photoreceptor stack, and hence, the disruption of IS/OS junction may represent photoreceptor misalignment or swelling of the photoreceptors. Recently, Spaide and Curcio17 suggested that the band often attributed to the boundary between the IS and OS of the photoreceptors may actually align with ellipsoid portion of the inner segments. In our study, the initial scan at the mean follow-up of 3.4 months after RRD repair showed IS/OS disruption in 6 of 8 patients (i.e., 75% of the patients; 4 patients from Group 1 and 2 patients from Group 2), with BCVA ranging from 20/25 to CF among these patients. The 2 patients with 20/20 BCVA on initial scan had intact IS/OS junctions. Subsequent follow-up FD OCT at mean 5 years after surgery showed that of these 6 patients with IS/OS disruption on initial scan, 4 had complete (n = 3) or near complete (n = 1) restoration of IS/OS junction that correlated with visual improvement in BCVA (range, 20/25–20/30). The remaining 2 patients had persistent (Patient 7) or worsening (Patient 8) IS/OS disruptions resulting in persistently poor (i.e., CF) or worsening BCVA (i.e., 20/25 worsening to 20/40) at 5-year follow-up. Therefore, long-term visual outcome after RRD repair seems to be dependent on foveal IS/OS integrity and restoration. Previous studies with shorter follow-up (up to 25 months), using commercial FD OCT and TD OCT have similarly shown photoreceptor IS/OS restoration as a prognostic marker for visual improvement after RRD repair and ERM peel after RRD repair.12,14 However, none of the previous studies showed progressive worsening of vision and photoreceptor disruption after successful repair of retinal detachment noted with Patient 8 in our study with longer follow-up in the absence of other concurrent visually significant maculopathy. Although Patient 8 was noted with a new ERM on the final FD OCT, this did not appear to be visually significant since there was no foveal traction noted on FD OCT. Our previous study has shown that increase in foveal thickness from traction of the ERM correlated best with visual acuity in eyes with idiopathic ERM.15
It is of interest that among the four of six patients who had IS/OS disruption on initial scan, with complete restoration of IS/OS junction at the final follow-up, all had an intact ELM seen on the initial FD OCT scan. However, Patient 8 who had worsening IS/OS disruption between the initial and final follow-up FD OCT scans had ELM disruption seen on the initial FD OCT scan which appeared even more evident on the follow-up FD OCT. Hence, ELM integrity in early postoperative phase may be an important predictor of restoration of photoreceptor IS/OS disruptions, as well as visual acuity and function long-term. This possibility was also suggested in previous reports of eyes after RRD with shorter follow-up.12,16 In the absence of an intact ELM, photoreceptor disruption may persist or even worsen as noted in our study.
External limiting membrane is formed by the junction of photoreceptor nuclei and Muller cells.18 Loss of ELM on FD OCT may be indicative of damage or loss of the photoreceptor nuclear body and Muller cells, which may lead to irreversible photoreceptor and vision loss at long-term follow-up.16 Because histopathological studies of fovea centralis have shown that the inner half of the foveola is composed of inverted cone-shaped zone of Muller cells in human retina, damage to foveal Muller cells may also play a role in long-term gradual degeneration of the foveal photoreceptor. Human Muller cells can differentiate into rod photoreceptors when transplanted into mouse retina, suggesting that Muller cells may have some plasticity to act as photoreceptor progenitor cells under certain conditions.19,20
Patient 7 is the only exception to the above observation. This patient had an intact ELM at the initial FD OCT scan. However, BCVA postoperatively was CF and failed to improve at long-term follow-up. One explanation could be the long duration of RRD (i.e., 2 months) before repair. Based on the previous studies, repair of macula-off RRD may be delayed up to 1 week after development of macula-off RRD without significant adverse effect on visual outcome.3 However, visual recovery with further delay in repair is generally poorer.4 In our study, only Patient 7 had retinal detachment duration of more than 10 days before repair of retinal detachment. This patient failed to have restoration of the IS/OS junction even after several years after successful RRD repair, likely because of irreversible loss of photoreceptors via apoptosis which may have occurred before RRD repair.21,22 Consistent with this theory is the attenuated outer nuclear layer in the fovea noted both in the early and final FD OCT images (Figure 3). A wave of photoreceptor degeneration via apoptosis is seen as early as 1 and 3 days after experimental RRD. It is possible that this mechanism of photoreceptor loss may not be associated with disruption of ELM seen on FD OCT but can result in profound early and persistent vision loss.22
Subfoveal fluid was present in 3 of 8 eyes at the initial FD OCT imaging. Two of these patients had RRD repaired via pneumatic retinopexy combined with retinal cryopexy, and one patient had scleral buckle repair with retinal cryopexy. Of interest, the visual acuity at the initial FD OCT imaging was 20/20 and not affected by the presence of subfoveal SRF, perhaps because of an intact foveal IS-OS junctions (Patient 5). This patient did have some areas of decreased sensitivity on MP-1 extrafoveally that corresponded to areas of more prominent SRF on FD OCT. In the other two patients with subfoveal fluid, BCVA was decreased and both foveal SRF and IS/OS defect were present on the initial postoperative FD OCT scan. All three patients had complete resolution of the SRF on follow-up FD OCT 5 years later. Concurrent with resolution of SRF was improvement in foveal IS/OS disruption, visual acuity, and normalization of MP-1 sensitivity observed in all three eyes. Historically, persistent SRF has been thought to be responsible for persistently decreased BCVA shortly after RRD repair.5,23 However, studies with longer follow-up have shown complete resolution of SRF at 6 months to 24 months after scleral buckle surgery with no influence on the final visual acuity.6,12
Our present study has some obvious limitations. The sample size is very small because only 8 of the original 17 patients could be contacted and agreed to participate in this follow-up study. Thus, our impressions are based on the limited observations, and future larger studies are needed to validate our impressions. Second, these results are based on a cohort of patients with favorable preoperative factors such as shorter duration of retinal detachment before repair and younger age. Many patients who underwent RRD repair at the University of California Davis Eye Center had complex RRDs requiring multiple repairs or had significant postoperative changes in the macula that did not qualify them for the study. Nevertheless, this study is the longest follow-up report using serial FD OCT to study the long-term macular morphologic and functional changes after successful macula-off RRD repair and provides new insights regarding possible mechanisms for visual recovery and visual loss after RRD repair.
In conclusion, our study results suggest that the macular function and BCVA may progressively improve or worsen long-term after successful repair of macula-involving RRD. The presence of foveal IS-OS photoreceptor disruptions seems to correlate with visual acuity outcome after RRD repair both short-term and long-term. The presence of an intact ELM in the early postoperative course may be a good prognostic indicator in that it may correlated with eventual restoration of photoreceptor IS/OS disruption and visual recovery. In contrast, a loss of ELM in the early postoperative FD OCT image may be a poorer prognostic sign, potentially leading to permanent or progressive photoreceptors damage and vision loss. The presence of SRF on the early postoperative FD OCT images may lead to transient decrease in visual function, but SRF usually seems to resolve spontaneously with long-term follow-up. Thus, draining trace amounts of residual SRF seen postoperatively on FD OCT may not be necessary unless it increases or is associated with worsening vision. Future studies using newer imaging techniques, such as adaptive optics OCT that allow even higher image resolution, may provide more information regarding cellular changes associated with retinal detachment and repair. A better understanding of pathogenesis of the vision loss associated with retinal detachment will allow us to develop a more effective therapy to minimize long-term vision loss associated with this condition.
Acknowledgments
Supported by the National Eye Institute, Bethesda, MD (grant no. 014743 to J.S.W.) and by the Research to Prevent Blindness unrestricted departmental grant, New York, NY.
Footnotes
None of the authors have any conflicting interests to disclose.
References
- 1.Rowe JA, Erie JC, Baratz KH, et al. Retinal detachment in Olmsted County, Minnesota, 1976 through 1995. Ophthalmology. 1999;106:154–159. doi: 10.1016/S0161-6420(99)90018-0. [DOI] [PubMed] [Google Scholar]
- 2.Shimoda Y, Sano M, Hashimoto H, et al. Restoration of photoreceptor outer segment after vitrectomy for retinal detachment. Am J Ophthalmol. 2010;149:284–290. doi: 10.1016/j.ajo.2009.08.025. [DOI] [PubMed] [Google Scholar]
- 3.Ross WH, Kozy DW. Visual recovery in macula-off rhegmatogenous retinal detachments. Ophthalmology. 1998;105:2149–2153. doi: 10.1016/S0161-6420(98)91142-3. [DOI] [PubMed] [Google Scholar]
- 4.Burton TC. Recovery of visual acuity after retinal detachment involving the macula. Trans Am Ophthalmol Soc. 1982;80:475. [PMC free article] [PubMed] [Google Scholar]
- 5.Wolfensberger TJ, Gonvers M. Optical coherence tomography in the evaluation of incomplete visual acuity recovery after maculaoff retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2002;240:85–89. doi: 10.1007/s00417-001-0410-6. [DOI] [PubMed] [Google Scholar]
- 6.Ricker LJ, Noordzij LJ, Goezinne F, et al. Persistent subfoveal fluid and increased preoperative foveal thickness impair visual outcome after macula-off retinal detachment repair. Retina. 2011;31:1505–1512. doi: 10.1097/IAE.0b013e31820a6910. [DOI] [PubMed] [Google Scholar]
- 7.Seo JH, Woo SJ, Park KH, et al. Influence of persistent submacular fluid on visual outcome after successful scleral buckle surgery for macula-off retinal detachment. Am J Ophthalmol. 2008;145:915–922. doi: 10.1016/j.ajo.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Alam S, Zawadzki RJ, Choi S, et al. Clinical application of rapid serial Fourier-domain optical coherence tomography for macular imaging. Ophthalmology. 2006;113:1425–1431. doi: 10.1016/j.ophtha.2006.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Truong SN, Alam S, Zawadzki RJ, et al. High resolution Fourier-domain optical coherence tomography of retinal angiomatous proliferation. Retina. 2007;27:915–925. doi: 10.1097/IAE.0b013e31805468fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chin EK, Sedeek RW, Li Y, et al. Reproducibility of macular thickness measurement among five OCT instruments: effects of image resolution, image registration, and eye tracking. Ophthalmic Surg Lasers Imaging. 2012;3:1–12. doi: 10.3928/15428877-20111222-02. [DOI] [PubMed] [Google Scholar]
- 11.Kiernan DF, Hariprasad SM, Chin EK, et al. Prospective comparison of cirrus and stratus optical coherence tomography for quantifying retinal thickness. Am J Ophthalmol. 2009;147:267–275. doi: 10.1016/j.ajo.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 12.Wakabayashi T, Oshima Y, Fujimoto H, et al. Foveal microstructure and visual acuity after retinal detachment repair: imaging analysis by Fourier-domain optical coherence tomography. Ophthalmology. 2009;116:519–528. doi: 10.1016/j.ophtha.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Smith AJ, Telander DG, Zawadzki RJ, et al. High-resolution Fourier-domain optical coherence tomography and microperimetric findings after macula-off retinal detachment repair. Ophthalmology. 2008;115:1923–1929. doi: 10.1016/j.ophtha.2008.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rossetti A, Doro D, Manfrè A, Midena E. Long-term follow-up with optical coherence tomography and microperimetry in eyes with metamorphopsia after macula-off retinal detachment repair. Eye (Lond) 2010;24:1808–1813. doi: 10.1038/eye.2010.138. [DOI] [PubMed] [Google Scholar]
- 15.Pilli S, Lim P, Zawadzki RJ, et al. Fourier-domain optical coherence tomography of eyes with epiretinal membrane: correlation between morphologic changes and visual function. Eye (Lond) 2011;25:775–783. doi: 10.1038/eye.2011.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Romano MR, Vinciguerra P, Radice P, et al. Outer retinal layers. Ophthalmology. 2011;118:1006.e2. doi: 10.1016/j.ophtha.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 17.Spaide RF, Curcio CA. Anatomical correlates to the bands seen in the outer retina by optical coherence tomography. Retina. 2011;31:1609–1619. doi: 10.1097/IAE.0b013e3182247535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spitznas M. The fine structure of the so-called outer limiting membrane in the human retina. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1970;180:44–56. doi: 10.1007/BF02384821. [DOI] [PubMed] [Google Scholar]
- 19.Xia X, Li Y, Huang D, et al. Oncostatin M protects rod and cone photoreceptors and promotes regeneration of cone outer segment in a rat model of retinal degeneration. PLoS One. 2011;6:e18282. doi: 10.1371/journal.pone.0018282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giannelli SG, Demontis GC, Pertile G, et al. Adult human Müller glia cells are a highly efficient source of rod photoreceptors. Stem Cells. 2011;29:344–356. doi: 10.1002/stem.579. [DOI] [PubMed] [Google Scholar]
- 21.Lewis GP, Charteris DG, Sethi CS, et al. The ability of rapid retinal reattachment to stop or reverse the cellular and molecular events initiated by detachment. Invest Ophthalmol Vis Sci. 2002;43:2412–2420. [PubMed] [Google Scholar]
- 22.Cook B, Lewis GP, Fisher SK, Adler R. Apoptotic photoreceptor degeneration in experimental retinal detachment. Invest Ophthalmol Vis Sci. 1995;36:990–996. [PubMed] [Google Scholar]
- 23.Benson SE, Schlottmann PG, Bunce C, et al. Optical coherence tomography analysis of the macula after scleral buckle surgery for retinal detachment. Ophthalmology. 2007;114:108–112. doi: 10.1016/j.ophtha.2006.07.022. [DOI] [PubMed] [Google Scholar]