Abstract
[Purpose] This study investigated the effectiveness of a class- and home-based exercise with massage between Thai traditional and standardized physical therapy (TPT and SPT) in older people with knee osteoarthritis (KOA). [Subjects and Methods] Thirty-one subjects with KOA (aged 50–85 years) in two selected villages were randomly assigned into the TPT or SPT programs. Seventeen TPT subjects received Thai exercise with traditional massage, and 14 SPT individuals performed strengthening exercise with Swedish massage. Both programs consisted of a class with supervision plus home self-care for 8 weeks; the subjects then managed home self-care for 1 year. [Results] After 2 months, the six-minute walk test (6MWT), Western Ontario and McMaster Universities Arthritis Index (WOMAC), and SF-36 testing showed significant improvement in both groups, but the improvement of the TPT group was greater. After 1year, only the score for the 6MWT was greater in the TPT group than in the SPT group. [Conclusion] The TPT program yielded better results for the 6MWT, but, both programs had beneficial effects on the pain, function, and QOL of middle-aged and older patients with KOA in the community setting.
Key words: Knee osteoarthritis, Six-minute walk test, Bodyweight-based exercise training
INTRODUCTION
Knee osteoarthritis (KOA) is the most common joint disease in middle-aged and older people. Pain is the main symptom that leads to limitation in the patients’ abilities such as the ability to walk, stand up, and climb stairs, and dependency in daily living activities1). This disease leads to poor quality of life (QOL) and is a significant burden on health-care services2). The primary goal of treatment in KOA is reducing pain and improving functional capacity3). Non-pharmacological treatment, physical therapy (PT), and complementary and alternative medicine (CAM), which includes massage4), alternative exercise5), thermotherapy6), and acupuncture7), play an important role in health care for patients with KOA. The use of CAM in developed countries appears to be increasing as awareness increases. It may have been that use of CAM increased with socioeconomic status8). Currently, alternative exercises including yoga, Tai Chi, and aquatic programs are models of exercise therapy for patients with KOA5, 9, 10). Strengthening and aerobic exercise are beneficial for improving KOA-related symptoms in terms of pain11) and physical function12).
In Thailand, a form of Thai exercise that utilizes a wand is popular among elderly people and is a body weight-based form of resistance exercise; however, the intensity of this exercise can be increased by lifting the wand in upper limb exercise or can be decreased by using the wand to support the body. Our previous study shows that Thai exercise with a wand can improve QOL13). This exercise with a wand tends to increase muscle strength, which can be beneficial for pain improvement; however, the evidence regarding this is not clear. This exercise might be a better therapeutic form for reducing pain in KOA patients when combined with Thai massage because it has been shown to reduce the pain in patients with back pain14) and scapulocostal syndrome15).
Home- and class-based programs are some of the most suitable treatments for elderly people in the community16). Nonetheless, a previous study found that patients carried out a home-based program just for the initial phase and subsequently did not maintain a self-care program17). Thereby, a home-based program along with a class-based program supervised by physical therapists might provide confidence for patients to help in management of knee symptoms by themselves. However, there is no evidence concerning whether or not Thai exercise with traditional massage can effect the pain, walking ability, and QOL in patients with KOA. Thus, the aim of this study was to investigate the effectiveness of a class- and home-based program using Thai exercise with traditional massage and the long-term follow-up in the form of a home program on pain, walking ability, and QOL in middle-aged and older patients with KOA in a suburban community.
SUBJECTS AND METHODS
This study was a randomized controlled trial with a field-based assignment. The subjects were patients with KOA aged 50–85 years from two selected villages with similar socioeconomic statuses in a suburban community of Khon Kaen Province, Thailand. These two villages are small, and travel within them is difficult. Additionally, they were found to be in need of health promotion for people with KOA. A simple randomization was used to allocate each village into either the TPT or SPT program. The protocol and informed consent form were approved by the Khon Kaen University Ethics Committee for Human Research.
The diagnosis of KOA was confirmed for each patient based on their medical history report and a physical examination performed by physical therapists based on the clinical criteria of the American College of Rheumatology (1986)18). The inclusion criteria consisted of pain in the knee and three of the following conditions: 1) aged at least 50 years of age, 2) less than 30 min of morning stiffness, 3) crepitus on active motion, 4) bony tenderness, 5) bony enlargement, and 6) no palpable warmth of the synovium. The subjects who met the inclusion criteria were asked to join and had to sign an informed consent form before participation. All individuals were able to walk and were assessed for all measurements. Each of them received standard medical management of KOA from a local primary care unit.
The exclusion criteria consisted of diagnosis of KOA caused by other diseases, such as rheumatoid arthritis, or gouty arthritis or any accident/sports, contagious diseases, uncontrolled hypertension or diabetes mellitus, neurological deficits, or psychological symptoms. Subjects who were unable to perform standing and walking, or had received a knee replacement and those whose doctors advised against massage and exercise due to an underlying disease were also excluded. Twenty-four patients in the Thai physical therapy (TPT) group and 20 patients in standard physical therapy (SPT) group were assessed for their eligibility to participate in the study. Thirteen subjects were excluded for failing to meet the inclusion criteria. The remaining subjects, 17 in the TPT group and 14 in the SPT group, fulfilled the above criteria and agreed to participate in the study.
The TPT and SPT programs consisted of two phases. The first phase include class-based TPT and SPT group intervention programs at an appointed public indoor area in each village, and these programs were also associated with a home program. All subjects were asked to attend their group class, which was supervised by a researcher, three days/week. Additionally, they were recommended to follow their program at home at least two days/week for eight weeks. The second phase was performing the actual home self-care program with TPT or SPT alone, at least three times/week for twelve months. To extend the benefits of the home program, subjects received the booster session once a month during the first three months. Researchers incorporated content into each booster session to stimulate subject education and awareness regarding self-management, which included physical activity and exercise planning, and discussion of other related problems.
In the TPT group, exercise with a wand consisted of six exercises that were based on a past study13) that emphasized exercise in the muscle of the quadriceps and hamstrings. Concentric and eccentric isotonic contraction are applied with different positions (Fig. 1). These exercises are suitable for the knee joints and low impact. Each exercise was performed five times/session, two sets/day, and this was increased every two weeks until reaching 40 times/session. In the Thai massage session, the massage method used pressure on muscle lines of the quadriceps, hamstrings, tibialis anticus, and calves. To apply deep pressure, one or two thumb pads or the side of an elbow tip was used in some cases. Superficial heating with Thai herbs, containing 10 ingredients consisting of camphor, Kurkumin, lemon grass, and turmeric leaves, in a bag was applied to various areas of both upper and lower leg muscles and to cover the knees. In the SPT group, six progressive strengthening exercises for the quadriceps and hamstring muscles based on a past study were used19). Each exercise was performed 10 times/session, 2 sets/day, and the resistance was increased every two weeks (0.5 to 2 kg). The increase in load was flexible and depended on the subject’s requirements. Swedish massage consisted of superficial and deep stroking, and kneading or stroking various muscles of both the upper and lower leg. Additionally, a superficial heating bag filled with hot water was placed on the same areas. All subjects were suggested to perform the 30-minute exercise program, receive the 30-minute massage, and receive the 15-minute superficial heat/cold care whenever they might normally use an ice pack for acute or subacute knee pain. All outcomes were measured at baseline and at 2, 5, 8, and 14months. The primary outcome was the six-minute walk test (6MWT). The secondary outcomes included functional capacity evaluated by the Thai versions of the Western Ontario and McMaster Osteoarthritis Index (WOMAC) and quality of life (Thai Short Form-36, SF-36). The 6MWT was used for evaluating subjects’ walking capacity by measuring the distance walked during a defined period. The Thai 5-point Likert version of the WOMACTM 3.1 Index that was selected included 24 items grouped into 3 dimensions: pain (5 items), stiffness (2 items), and function (17 items). The SF-36 is a health-related quality of life (QOL) instruments that contains two dimensions, physical health (PH) and mental health (MH) (each range, 0–100). Adherence to the home program was assessed on a 5-point scale (1 time/wk = almost never, 2 times/wk = occasional adherence, 3 times/wk = regular adherence, 4 times/wk = often adherence, ≥ 5 times/wk = very often)20). All data are presented as means ± SD. Outcomes were analyzed using repeated measures analysis of variance (ANOVA) for evaluating differences within groups, and analysis of covariance (ANCOVA) was used for evaluating differences between groups. In the ANCOVA, the baseline values for all outcome variables in the posttest were adjusted for baseline differences. A p value < 0.05 was used as the criterion for statistical significance.
Fig. 1.
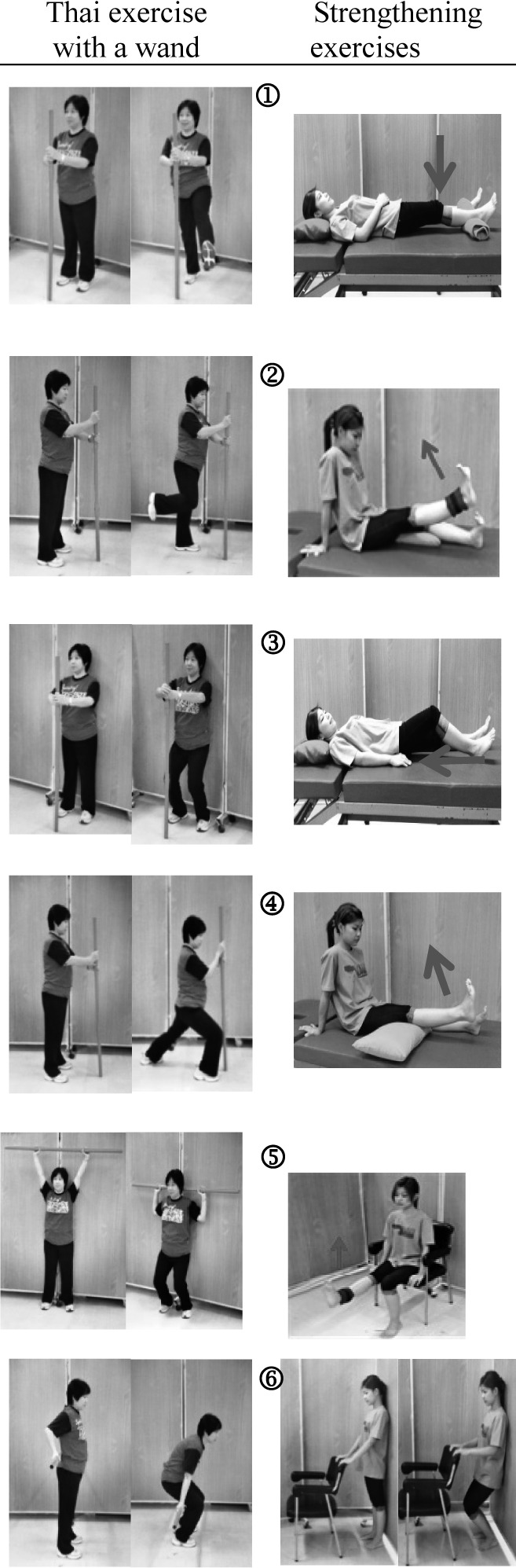
Thai exercise with a wand in the TPT group (left) and strengthening exercise in the SPT group (right)
RESULTS
The physical characteristics of all subjects are shown in Table 1. No statistical differences were found between the two groups.
Table 1. Subject characteristics.
| Characteristics | SPT group (n = 14) | TPT group (n = 17) |
| Sex; male/female (n) | 1/13 | 1/16 |
| Age (years)# | 69.8±8.4 | 67.8±6.4 |
| (Range) | (53 to 84) | (52 to 76) |
| Height (cm)# | 153.6±7.4 | 153.5±6.4 |
| Weight (kg)# | 61.7±6.5 | 62.3±11.2 |
| Body mass index-BMI (kg/m2)# | 26.3±3.6 | 26.4±3.8 |
| Visual Analogue # Scale-VAS (cm) | 6.35±2.01 | 6.25±1.32 |
| Domain of pain (n) | ||
| Left knee | 3 | 1 |
| Right knee | 1 | 3 |
| Both knees | 10 | 13 |
| Period of pain (n) | ||
| < 3 months | - | - |
| 1 year < 3 months | 1 | 2 |
| 1–3 years | 4 | 9 |
| > 3 years | 9 | 6 |
# Values are presented as the mean ± standard deviation (SD)
In the first phase, it was found that the 6MWT score was significantly increased in the TPT (p< 0.001) and SPT (p< 0.05) groups. In the second phase, the 6WMT distance was found to decreases over time compared with the baseline after treatment in each group, and the SPT group showed a significant decrease (p<0.05) (Table 2).
Table 2. All outcomes of each group over time.
| Items | Group | Baseline | 2nd month | 5th month | 8th month | 14th month |
| 6MWT | TPT | 301.46±69.03 | 331.38±81.66** | 258.92±66.41* | 256.62±82.46* | 216.62±67.41# |
| SPT | 312.94±74.45 | 376.18±91.94# | 335.94±63.19 | 300.12±61.19 | 300.12±71.11 | |
| WOMAC | ||||||
| Pain | TPT | 10.24±3.21 | 4.94±2.78# | 6.00±2.74# | 6.53±3.63# | 7.35±3.63* |
| SPT | 11.77±3.19 | 7.00±2.71# | 8.23±5.82* | 7.38±3.50# | 7.54±4.48# | |
| Stiffness | TPT | 2.65±1.97 | 0.47±0.72# | 0.41±0.62# | 0.71±1.3* | 0.59±0.80# |
| SPT | 2.46±1.27 | 1.00±1.16# | 0.77±1.64# | 0.54±0.88# | 0.38±0.77# | |
| Physical function | TPT | 27.82±8.62 | 15.41±8.68** | 19.35±8.18* | 19.35±10.15# | 23.29±5.06 |
| SPT | 33.92±8.27 | 21.69±8.26# | 27.92±7.25* | 25.92±8.58# | 24.69±7.642# | |
| SF-36 | ||||||
| Physical health | TPT | 49.10±13.15 | 78.58±10.48# | 79.91±9.77# | 73.32±12.64# | 68.49±10.65** |
| SPT | 50.67±14.46 | 73.28±11.39# | 72.01±9.13* | 68.54±12.24** | 69.47±14.81* | |
| Metal health | TPT | 58.71±12.61 | 89.98±7.94# | 91.46±5.62# | 89.94±8.14# | 87.60±7.19# |
| SPT | 73.87±14.71 | 79.82±9.87 | 86.20±7.33* | 89.76±7.31# | 93.34±2.40# | |
| Global | TPT | 53.90±10.03 | 84.28±7.90# | 85.68±6.31# | 81..63±8.90# | 78.04±7.78# |
| SPT | 62.27±11.79 | 76.55±10.16* | 79.11±7.62# | 79.15±8.93# | 81.40±8.18# | |
* p<0.05; ** p<0.01; # p<0.001; significant differences within a group when comparing baseline and post-training values by ANOVA
TPT, n=17; SPT, n=14
Changes in the WOMAC and SF-36 scores, as evaluated by comparison of baseline and after treatment scores (2nd, 5th, 8th, and 14th months), are shown in Table 2. There were significant improvements in the WOMAC and SF-36 scores for the physical health, mental health, and global dimensions when comparing the scores at baseline and 2 months in both groups (p< 0.05), but there was no change in the mental health dimension in the SPT group. In the second phase, all dimension scores of the WOMAC in both groups significantly improved when comparing the baseline scores with those after twelve months of treatment (p< 0.05), except for WOMAC physical function at the 14th month in the TPT group. Almost all of the SF-36 scores in both groups significantly improved; however, the TPT group showed a trend to decline over time.
Adjusted post-training scores for all outcomes in both groups are presented in Table 3. The 6MWT distances were significantly greater in the TPT group than in the SPT group at the 5th and 14th months (p= 0.01 and 0.03, respectively). The mean difference in 6MWT distances between the TPT and SPT groups was 60.94 meters (95% CI: 15.58 to 106.29 meters) at the 5th month and 47.23 meters at the 14th month (95% CI: 4.14 to 90.33 meters). At the 2nd and 5th months, the mental health and global dimension scores of the SF-36 were significantly increased in the TPT group compared with the SPT group (p<0.05). However, at the 14th month, the mental health dimension in the SPT group was significantly higher (p=0.01)
Table 3. Adjusted post-training means for all outcomes.
| Items | 2nd month | 5th month | 8th month | 14th month | ||||||||
| TPT | SPT | Mean Diff. (95%CI) | TPT | SPT | Mean Diff. (95%CI) | TPT | SPT | Mean Diff. (95%CI) | TPT | SPT | Mean Diff. (95%CI) | |
| 6MWT(m) | 371.4 | 337.5 | 33.90 (−8.68–76.48) | 329.0 | 268.1 | 60.94* (15.58 – 106.29) | 282 | 295.9 | −13.92 (−22.18 – 50.03) | 284.4 | 237.2 | 47.23* (4.14 – 90.33) |
| WOMAC | ||||||||||||
| Pain | 5.15 | 6.50 | −1.36 (−3.26 – 0.55) | 6.71 | 6.43 | 2.8 (−2.19 – 2.75) | 6.68 | 6.91 | −0.23 (−2.90 – 2.44) | 7.45 | 7.08 | 0.37 (−2.26 – 2.99) |
| Stiffness | 0.47 | 1.06 | −0.59 (−1.24 – 0.64) | 0.54 | 0.64 | −0.09 (−0.98 – 0.79) | 0.86 | 0.48 | 0.38 (−0.42 – 1.18) | 0.60 | 0.40 | 0.20 (−0.40 – 0.80) |
| Physical function | 17.05 | 19.51 | −2.47 (−8.10 – 3.17 ) | 20.97 | 25.32 | −4.35 (−8.98 – 0.28) | 21.42 | 21.56 | −0.14 (−7.28 – 7.01) | 23.49 | 21.68 | 1.81 (−1.84 – 5.46) |
| SF-36 | ||||||||||||
| Physical health | 78.85 | 73.15 | 5.70 (−2.22 – 13.62) | 78.47 | 72.41 | 6.06 (−0.46 – 12.57) | 74.00 | 69.62 | 4.38 (−6.23 – 14.98) | 68.47 | 68.60 | −0.13 (−10.03 – 9.77) |
| Mental health | 90.36 | 82.28 | 8.08* (0.54 – 15.63) | 91.48 | 84.67 | 6.81* (1.17 – 12.46) | 90.20 | 90.93 | –0.73 (−7.17 – 5.71) | 87.60 | 93.34 | −5.74* (−10.15 – −11.33) |
| Global | 85.60 | 77.13 | 8.47* (1.32 – 15.62) | 85.06 | 78.88 | 6.18* (0.33 – 12.03) | 83.27 | 80.47 | 2.80 (−4.46 – 10.07) | 77.97 | 81.23 | –3.26 (−9.54 – 3.03) |
Note: *p<0.05, significant difference in comparing the adjusted post-training means between groups by ANCOVA statistics
Regarding home program adherence, most of the SPT and TPT participants performed exercise “very often” in the period of 3 to 5 months, whereas the participants in the TPT group (76%) had better exercise adherence than the SPT group (62%). After five months, exercise adherence in both groups decreased. Massage adherence in the two groups was similar when compared at 5 and 8 months (23 to 30%). Most of the participants in both groups had low adherence to the superficial heat treatment (almost never used: 88% in the TPT group, 54% in the SPT group). There were no harmful effects of the interventions reported in either group.
DISCUSSION
The main findings of this study are that the TPT group showed improvement in the 6MWT, WOMAC, and SF-36 scores after 2 months of treatment and lower detraining effects on the 6MWT distance at 1 year after TPT as compared with the SPT group. Before the programs, the data for baseline characteristics, the main outcome, and other outcomes among the two groups were not significantly different. No significant difference was seen in most of the outcome measures when comparing the adjusted post-training means of the TPT and SPT groups after 2 months of treatment; however, the mental and global dimension SF-36 scores demonstrated significant improvement in the TPT group (p< 0.05). After 1 year, physical and mental health SF-36 scores gradually worsened in both groups. However, the 6MWT distance in the TPT group was significantly higher than in the SPT group at the 5th and 14th months (p<0.05).
This study showed improved distances of about 20% and 9% in the 6MWT in the TPT and SPT groups after2 months of treatment. The subjects in the TPT group seemed to have more improvement when compared with the SPT group. This might be explained by the following reasons. Firstly, Thai massage provides manual compression of deep tissues that may release muscle tension15) and increase blood flow, leading to relief of pain and increased ROM21). The results of the current study are in agreement with a previous study that demonstrated that modified Thai therapeutic massage could reduce pain and increase knee function in patients with primary KOA21). Also, superficial heat applied via a Thai herb bag may yield some effects that decrease pain and inflammation22). Another reason might be that Thai traditional therapy is familiar to subjects who live in Thailand. From the observation of the researchers, the TPT subjects were obviously interested in their class-based group. The training methods in the TPT program seemed to suit the local Thai culture more than the SPT program. Incidentally, there was an active leader in the TPT group who may have continually induced other subjects to stay with the program. This could have affected the adherence to the exercise class in the TPT group, causing it to be more than that in the SPT group, which had no group leader.
A strong point of this study was that all subjects in the two groups completed participation in their classed-based programs; that is, there were no dropouts. This may have been due to the flexibility the supervisor had with regard to arrangement of the program. However, the compliance in performing the home-based program as recorded in their exercise log books showed that the TPT subjects performed the program more regularly than the SPT subjects, which resulted in better improvements in the TPT group. During the home self-care program, the percentage of TPT subjects who performed their own program in keeping with the criteria of at least 2 days/week for 8 weeks was higher than that of the SPT group. For all of the above reasons, the TPT program tended to yield a better improvement within the group in terms of pain, walking ability, and QOL than the SPT program in patients with KOA who lived in these communities. Although the SPT program showed less improvement, we speculate that if subjects could have accepted the unfamiliar program and regularly practiced it for a long time, this program would certainly have had more impact. Most Thai people in rural communities believe that Thai traditional massage and hot herbal bags influence pain reduction and that body movement increases for a long time. This may well be a psychological effect. One’s belief in one’s own ability to perform tasks is also associated with higher adherence and better outcome23).
Home- and class-based exercise programs have shown benefits with regard to functional abilities in daily activities in elderly individuals24). It has been shown that weight-bearing exercise can increase muscle strength16), neuromuscular control25), and proprioception of the lower extremities26). Thai exercise with a wand is a low-impact resistance exercise in which the individual’s own body weight is used and is progressively performed with repetitive bouts. From the recorded diaries, TPT subjects had approximately 40% more exercise adherence than SPT subjects. In addition, the subjects in the SPT group utilized a lower target load with mostly open-kinetic exercise as compared with the TPT group for body weight-bearing strength training. These might be the reasons for less training effects in the SPT group. No supervision of the home-based programs resulted in reduced exercise adherence in both groups. However, greater exercise adherence was reported in the TPT group, probably due to more familiarity. It also resulted in a decline in the 6MWT distance in both groups. However, at the 5th and 14th months, the 6MWT distances in the TPT group were significantly better than in the SPT group due to more exercise adherence in the TPT group.
There were some limitations of the present study. Firstly, the sample size of the two groups was smaller than that the researchers desired, 23 subjects/group. In addition, the statistical power was 0.3. Thus, increasing the number of subjects may produce a stronger study. Secondly, there was relatively lower compliance with the home-based program in the SPT subjects than in the TPT subjects. There is a possibility that the subjects in the SPT group were not aware of the benefits of the program and that they felt uncomfortable performing self-care with Swedish massage or strength training with a load, although all subjects in the SPT and TPT groups commented that it was not fun to perform the program alone in their homes. Lastly, due to its nature as a community trial, it was impossible to blind the outcome assessors.
The current study was designed to be class based in order to promote self-efficacy expectations, and booster sessions were added to investigate maintenance in a prolonged program. Exercise self-efficacy was the only variable to significantly predict adherence to exercise during follow-up27). In the present study, the physical and mental health perception outcome variables tended to improve, but it was found that waking ability had decreased. Perceptions of personal efficacy have typically been identified as important predictors of exercise adherence and other health outcomes28). A future study should provide role play to enhance perceptions of personal efficacy in older patients with KOA and the utility of self-efficacy as a predictor of exercise maintenance over time. The results of this study demonstrated that the TPT program yielded better results in the 6MWT, although both programs had beneficial effects on the pain, physical function, and QOL in middle-aged and older patients with KOA in the two communities. Also, it seems that belief in traditional alternative treatments seems to influence self-efficacy in older people in rural communities.
Acknowledgments
The authors would like to thank the patients who participated in this study. The study was supported by the Incubation Research Group, and the Back, Neck and Other Joint Pain Research Group, Khon Kaen University.
REFERENCES
- 1.Lankhorst GJ, Van de Stadt RJ, Van der Korst JK: The relationships of functional capacity, pain, and isometric and isokinetic torque in osteoarthritis of the knee. Scand J Rehabil Med, 1985, 17: 167–172 [PubMed] [Google Scholar]
- 2.Roddy E, Zhang W, Doherty M, et al. : Evidence-based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee-the MOVE consensus. Rheumatology, 2005, 44: 67–73 [DOI] [PubMed] [Google Scholar]
- 3.Evcik D, Sonel B: Effectiveness of a home-based exercise therapy and walking program on osteoarthritis of the knee. Rheumatol Int, 2002, 22: 103–106 [DOI] [PubMed] [Google Scholar]
- 4.Perlman AI, Sabina A, Williams AL, et al. : Massage therapy for osteoarthritis of the knee: a randomized controlled trial. Arch Intern Med, 2006, 166: 2533–2538 [DOI] [PubMed] [Google Scholar]
- 5.Fransen M, Nairn L, Winstanley J, et al. : Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum, 2007, 57: 407–414 [DOI] [PubMed] [Google Scholar]
- 6.Brosseau L, Yonge KA, Robinson V, et al. : Thermotherapy for treatment of osteoarthritis. Cochrane Database Syst Rev, 2003, 4: CD004522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cao L, Zhang XL, Gao YS, et al. : Needle acupuncture for osteoarthritis of the knee. A systematic review and updated meta-analysis. Saudi Med J, 2012, 33: 526–532 [PubMed] [Google Scholar]
- 8.Eisenberg DM, Davis RB, Ettner SL, et al. : Trends in alternative medicine use in the United States, 1990–1997: Results of a Follow-up National Survey. JAMA, 1998, 280: 1569–1575 [DOI] [PubMed] [Google Scholar]
- 9.Ebnezar J, Nagarathna R, Bali Y, et al. : Effect of an integrated approach of yoga therapy on quality of life in osteoarthritis of the knee joint: a randomized control study. Int J Yoga, 2011, 4: 55–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolfson L, Whipple R, Derby C, et al. : Balance and strength training in older adults: intervention gains and Tai Chi maintenance. J Am Geriatr Soc, 1996, 44: 498–506 [DOI] [PubMed] [Google Scholar]
- 11.Lim CG, Lee SJ, Ko E, et al. : Effect of complex exercise program for the lower extremities on quadriceps activity and pain of elderly patients with knee osteoarthritis: a pilot study. J Phys Ther Sci, 2013, 25: 249–251 [Google Scholar]
- 12.Ettinger WH, Burns R, Messier SP, et al. : A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. JAMA, 1997, 277: 25–31 [PubMed] [Google Scholar]
- 13.Puengsuwan P, Promdee K, Sruttabul W, et al. : Effectiveness of Thai Wand Exercise training on health-related quality of life in sedentary older adults. Chula Med J, 2008, 52: 107–121 [Google Scholar]
- 14.Chatchawan U, Thinkhamro B, Kharmwan S, et al. : Effectiveness of traditional Thai massage versus Swedish massage among patients with back pain associated with myofascial trigger points. J Bodyw Mov Ther, 2005, 9: 298–309 [DOI] [PubMed] [Google Scholar]
- 15.Buttagat V, Eungpinichpong W, Chatchawan U, et al. : Therapeutic effects of traditional Thai massage on pain, muscle tension and anxiety in patients with scapulocostal syndrome: a randomized single-blinded pilot study. J Bodyw Mov Ther, 2012, 16: 57–63 [DOI] [PubMed] [Google Scholar]
- 16.Yamauchi J, Nakayama S, Ishii N: Effects of bodyweight-based exercise training on muscle functions of leg multi-joint movement in elderly individuals. Geriatr Gerontol Int, 2009, 9: 262–269 [DOI] [PubMed] [Google Scholar]
- 17.Thomas KS, Muir KR, Doherty M, et al. : Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ, 2002, 325: 752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altman R, Asch E, Bloch D, et al. : Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum, 1986, 29: 1039–1049 [DOI] [PubMed] [Google Scholar]
- 19.McCarthy CJ, Mills PM, Pullen R, et al. : Supplementing a home exercise programme with a class-based exercise programme is more effective than home exercise alone in the treatment of knee osteoarthritis. Rheumatology, 2004, 43: 880–886 [DOI] [PubMed] [Google Scholar]
- 20.Sluijs EM, Kok GJ, Van der Zee J: Correlates of exercise compliance in physical therapy. Phys Ther, 1993, 73: 771–782 [DOI] [PubMed] [Google Scholar]
- 21.Klinsrisuk S, Eungpinichpong W, Sumanont S, et al. : The effect of modified Thai therapeutic massage on pain reduction and knee function in individuals with primary knee osteoarthritis: a randomized control trial. J Med Tech Phy Ther, 2007, 9: 248–260 [Google Scholar]
- 22.Lekutai S, Tansuwannon W, Sereechotchahiran S, et al. : Pain-relieving effects of hot herbal compress in patients with knee osteoarthritis. J Thai Tradit Altern Med, 2008, 6: 219–228 [Google Scholar]
- 23.Marks R, Allegrante J: Chronic osteoarthritis and adherence to exercise: a review of the literature. J Aging Phys Act, 2005, 13: 434–460 [DOI] [PubMed] [Google Scholar]
- 24.King AC, Haskell WL, Taylor CB, et al. : Group- vs. home-based exercise training in healthy older men and women. A community-based clinical trial. JAMA, 1991, 266: 1535–1542 [PubMed] [Google Scholar]
- 25.Jan MH, Lin CH, Lin YF, et al. : Effects of weight-bearing versus non weight bearing exercise on function, walking speed, and position sense in subjects with knee osteoarthritis: a randomized controlled trial. Arch Phys Med Rehabil, 2009, 90: 897–904 [DOI] [PubMed] [Google Scholar]
- 26.Lephart SM, Pincivero DM, Rozzi SL: Proprioception of the ankle and knee. Sports Med, 1998, 25: 149–155 [DOI] [PubMed] [Google Scholar]
- 27.McAuley E, Lox C, Duncan TE: Long-term maintenance of exercise, self-efficacy, and physiological change in older adults. J Gerontol Psy Sci, 1993, 48: 218–224 [DOI] [PubMed] [Google Scholar]
- 28.McAuley E: The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J Behav Med, 1992, 15: 65–88 [DOI] [PubMed] [Google Scholar]


