Abstract
Objective:
To determine the rate of long-term cochlear implant (CI) use in children
Study Design:
Consecutive case series
Setting:
Tertiary referral center
Patients:
474 patients <18 years who received a first CI from 1999-2011
Interventions:
Cochlear implantation
Main Outcome Measure(s):
Regular CI use, defined as using the CI for ≥ 8 hours per day
Results:
We successfully contacted and obtained follow-up data on 402 patients (85%) via email, telephone, and postal survey. The rate of regular CI use was 93.2% (95% CI, 90.0-95.4) at 5 years post-implantation and 87.7% (95% CI, 82.9-91.3) at 10 years post-implantation. The mean number of hours of use per day was 12.0 hours (SD, 4.1 hrs). Cox proportional hazard regression analysis demonstrated a linear association between the age at implantation and the risk of discontinuing regular CI use. Rates of CI discontinuation increased by 18.2% per year of age at implantation (95% CI, 7.2-30.4%). Reported reasons for CI use < 8 hours of per day include poor hearing benefit (53.2%), social pressure (21.3%), and recurrent displacement of the transmitter coil (17.0%).
Conclusions:
High rates of regular CI use are sustained after childhood implantation, and younger age at implantation is associated with a higher rate of continued device usage.
BACKGROUND
Over the past 30 years, more than 200,000 individuals worldwide have received a cochlear implant (CI).1 While CIs can routinely enable deaf children to develop verbal language 2-5, accurate rates of long-term use of the cochlear implant after childhood implantation have received little longitudinal assessment. CI nonuse can be difficult to determine because it can happen many years after the initial surgical implantation. Several small studies have estimated that between 63% to 96% of pediatric CI recipients continue to regularly use their implants over periods of 5 to 14 years.6-9
The benefits of cochlear implants are observed in three time periods: short-term benefits (0-3 years) of sound awareness and early language development, medium-term benefits (3-8 years) of proficiency in verbal language and acquisition of reading and writing skills, and long-term benefits (>8 years) consisting of later educational, social and vocational opportunities that depend on verbal language proficiency.10 This conceptual framework of the effects of CI across developmental stages underscores how an accurate characterization of nonuse requires long-term data collection from patients across these three time periods, particularly with respect to guiding familial expectations of long-term outcomes.
The purpose of our study was to investigate long-term rates of sustained cochlear implant use in a large pediatric population, employing a rigorous, consecutive case series design.
MATERIALS AND METHODS
STUDY COHORT
We queried a clinical database of CI recipients maintained at the Johns Hopkins Listening Center to identify all pediatric patients (<18 years) who received their first cochlear implant at Johns Hopkins Hospital from 1999-2011 (n = 474). Exclusion criteria were: age ≥18 years at time of CI surgery, patients whose mailing address and phone number were outside of the US, and/or patients who had a CI placed before 1999. One additional patient was excluded from the study because he died before his implant was activated due to unrelated progressive cardiomyopathy.
We were able to successfully contact 402 (85%) patients to gather follow-up data (Table 1), and these individuals form the analytic cohort for this study. Individuals who we were able to contact were not significantly different than those who we were not able to contact by sex, age at implantation, or need for revision (data not shown). However, patients who could not be reached for contact were more likely to have been implanted earlier in the course of the study. This study was approved by the Johns Hopkins Medicine Institutional Review Board.
Data collection oN CI use
All study patients and/or the patients’ parents were contacted from June to July 2012 as part of an ongoing quality assurance initiative at the Johns Hopkins Listening Center. Study patients with an email address were sent standardized emails requesting the hours of CI use per day over the past 4 weeks. Our a priori definition of regular CI use was ≥8 hours a day. Patients who reported using the CI for <8 hours/day were asked for the month and year they stopped using their device on average for ≥8 hours a day and the primary reason for discontinuation. Unless otherwise noted, bilateral CI patients with discordant use between their left and right implant were analyzed using data from their first implant. If a patient gave a range of hours of daily use (e.g., 12-14 hours), we took the average of the values as the reported number of hours of daily use (i.e., 13 hours).
Patients who could not be contacted via email were sent postal surveys asking the same set of structured questions with a prepaid return envelope. Individuals who did not respond or responded unclearly to the email or postal survey received phone calls. Telephone interviews were conducted via a standardized semi-structured interview template with the patient or a proxy respondent (generally the patient’s parent).
STATISTICAL METHODOLOGY
Associations between CI cessation and categorical covariates were explored using chisquare and Fisher’s exact tests where applicable. The relationship between age at implantation and risk of discontinuing regular CI was analyzed using Kaplan-Meier methods and Cox proportional hazards regression. The assumption of proportional hazards was evaluated using the correlation coefficient between transformed survival time and the scaled Schoenfeld residuals. The assumption of linearity was checked using penalized splines. A threshold of p < .05 (two-sided) was used to evaluate statistical significance. All analyses were conducted in Stata 12 (Stata Corp) and R version 2.1511, using the Survival package. 12
RESULTS
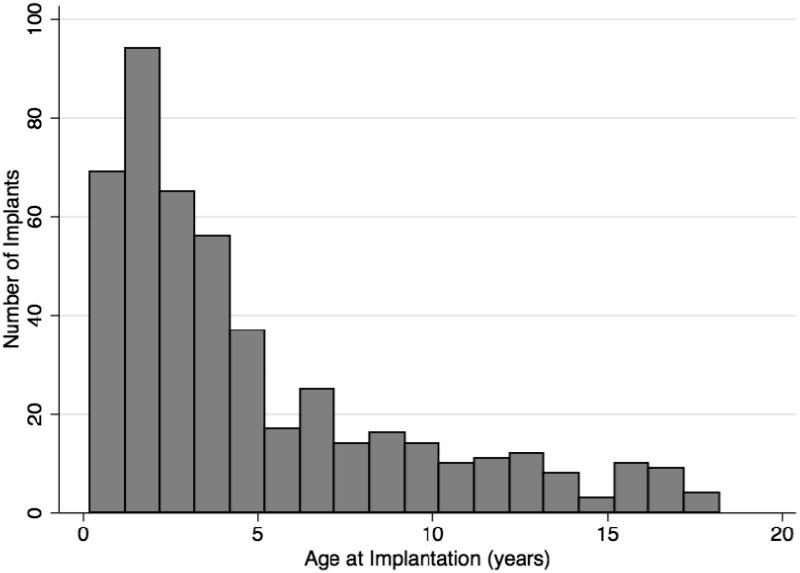
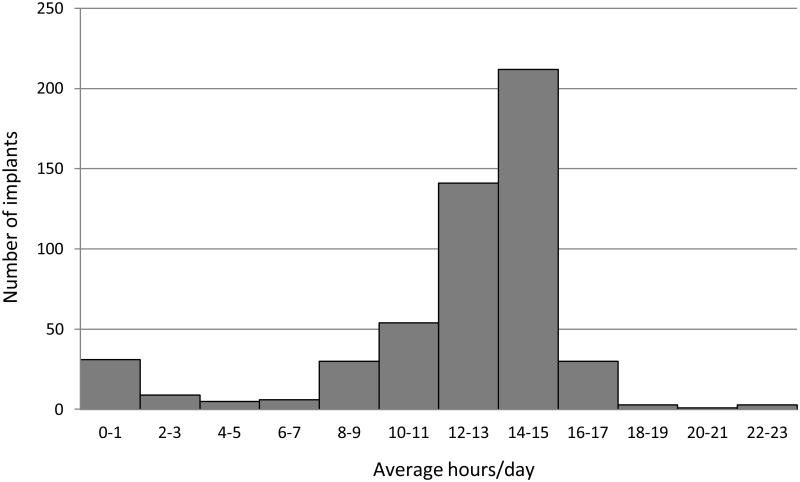
Clinical data for sex, year of implantation, age at initial CI, and side of implantation for all pediatric CI patients receiving their first implant at Johns Hopkins Hospital are presented in Table 1. The mean age at implantation was 4.9 years (SD, 4.3) (Fig. 1). The mean duration of use per day was 12.0 hours (SD, 4.1) (Fig. 2).
FIG 1.
Age at first cochlear implantation, Johns Hopkins 1999-2011 (n = 474).
FIG 2.
Average hours of cochlear implant use per day. For bilateral users, results are reported for each implant (n = 525).
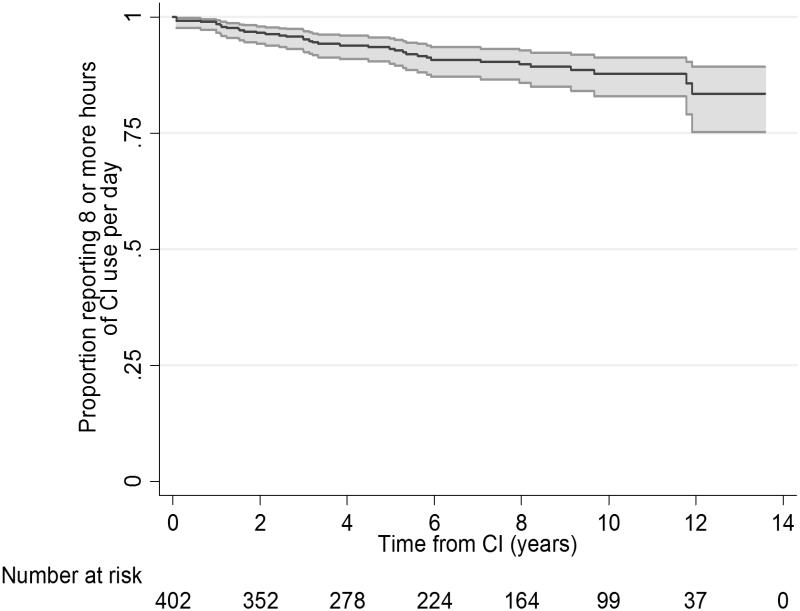
The cumulative rates of regular CI use were 93.2% (95% CI , 90.0-95.4) at 5 years post-implantation, 87.7% (95% CI, 82.9-91.3) at 10 years post-implantation, and 83.5% (95% CI, 89.3-75.2) at 13 years post-implantation (Fig. 3).
FIG 3.
Time from cochlear implant (CI) placement until incident nonuse (<8 hours of CI use/day) (n = 402). Gray area indicates 95% confidence interval.
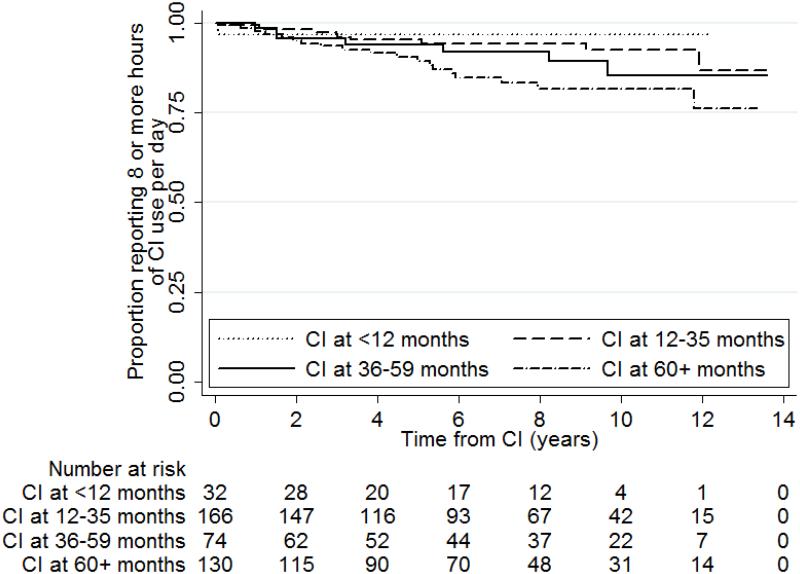
We further investigated how age at implantation was associated with regular CI use (Fig. 4). Rates of regular CI use differed by age at implantation with children implanted at younger ages having higher rates of regular CI use. For patients implanted at less than 12 months of age, the cumulative rate of regular CI use was 96.8% (95% CI, 79.8-99.6) at 13 years post-implantation. For patients implanted at 12 to 35 months of age, the cumulative rates of regular CI use were 95.3% (95% CI, 90.3-97.7) at 5 years post-implantation, 92.6% (95% CI, 85.6-96.3) at 10 years post-implantation, and 86.7% (95% CI, 68.8-94.8) at 13 years post-implantation. For patients implanted at 35-59 months of age, the cumulative rates of regular CI use were 93.8% (95% CI, 84.4-97.6) at 5 years post-implantation, 85.4% (95% CI, 70.1-93.2) at 10 years post-implantation, and 85.4% (95% CI, 70.1-93.2) at 13 years post-implantation. For patients implanted after 59 months of age, the cumulative rates of regular CI use were 89.4% (95% CI, 82.0-93.9) at 5 years post-implantation, 81.6% (95% CI, 71.9-88.2) at 10 years post-implantation, and 76.2% (95% CI, 60.5-86.3) at 13 years post-implantation.
FIG 4.
Long-term rate of regular CI (cochlear implant) use by age at implantation (n=402).
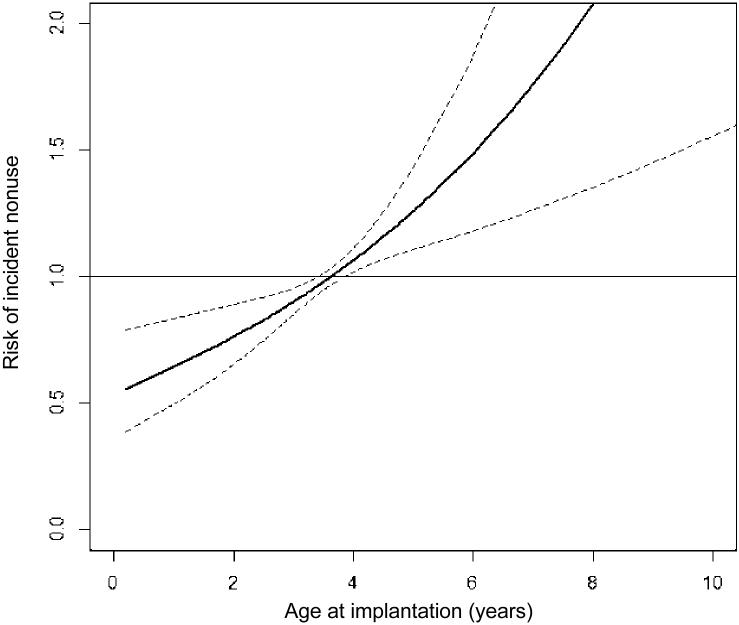
We investigated the observed trend toward higher rates of discontinuation of regular CI use with older age at CI with Cox proportional hazard models. Age of implantation was positively associated with increased risk of discontinuing regular CI use (p < 0.001). Rates of CI discontinuation increased by 18.2% per year of age at implantation [95% CI, 7.2-30.4%] (Fig. 5).
FIG 5.
Hazard ratio of incident cochlear implant nonuse (<8 hours of use/day) by age at implantation (n=402). Dotted line indicates 95% confidence interval.
Finally, we explored patients’ reasons for nonuse. For individuals using their implant <8 hours/day, the most commonly reported reasons for nonuse were poor hearing benefit (53.2%), social pressure (21.3%), described as a voluntary decision to discontinue CI use due to negative input from the user's peers, and recurrent displacement of the transmitter coil (17.0%) (Table 2).
DISCUSSION
Our results are based on the largest consecutive case series of children with cochlear implants to date and demonstrate that the rates of regular CI use remain high at 87.7% after 10 years. Participants on average wore their implant at least half the day, with a mean CI use of 12 hours a day. Younger age at implantation was associated with lower rates of discontinuing regular CI use. The most common reasons for nonuse were poor hearing benefit, social pressure, and recurrent displacement of the transmitter coil.
In comparing our findings to prior studies which estimated rates of regular CI use between 63% and 96%, our results are consistent with the larger studies with longer periods of follow-up.6-9 Our average duration of 12 hours of CI use a day was slightly higher than other studies, which reported CI use of 10.56 hours/day 8 and 11 hours/day.13 Prior research has also found a similar association between older age of implantation and increasing rates of nonuse. 8,9,14 Previously suggested reasons for nonuse have been anecdotal but include pain on stimulation, complex psychosocial issues at home14, and minimal audiological benefit.8,9 The strengths of the present study include a relatively large sample size, analytic methods allowing for differential periods of follow-up, a consecutive case series at a single institution, and a high response rate.
Few studies to date have attempted to quantify regular CI use. A study consisting of 27 participants catagorized "consistent" CI users as those who wore their CI at least 6 hours a day.8 Our a priori definition of regular use being ≥8 hours a day proved to be an effective metric as there appeared to be a natural cutpoint in CI usage at this value (Fig. 2).
A key limitation of our study is possible recall bias. Patient or parent-proxy reports of CI use may overestimate the hours of CI use/day or underreport the actual time to discontinuation of regular CI use.15,16 Previous studies of medical device use in children, such as asthma inhalers, have suggested that surveyed data tend to slightly overestimate actual device use.17,18 Presumptively, such overestimations are due to a conscious or subconscious desire to respond in accordance with prior guidance emphasizing the importance of regular CI use. Every attempt was made to limit recall bias by using a standardized questionnaire that was distributed via email or postal mail instead of telephone whenever possible. Future efforts to reduce such bias will be possible with data logging capabilities incorporated into the CI processor, a technology which has long been available in hearing aids and is just now being incorporated into CI processors. There is also the possibility that individuals who could not be reached for this study (15% of all CI recipients from 1999-2011) may have had poorer outcomes that would not be accounted for in our results. However, we note that the age at implantation, sex, and need for revision did not differ between the individuals who we were or were not able to contact. Because patients who were unable to be contacted were implanted earlier in the course of the study, these patients were also more likely to have moved since the time of their initial implantation and hence more difficult to contact.
Our results demonstrate high long-term rates of continued regular CI use in children and a strong association between later age at implantation and lower rates of regular CI use. These results contribute to a growing body of literature which strongly supports early identification and implantation of children meeting criteria for cochlear implantation.
Our observations can further inform studies of cost-utility associated with childhood cochlear implantation wherein data on long-term use were not included.19-21 Our results appear to bolster and can further refine models of cost-utility indicating that earlier cochlear implantation of childhood candidates provides significantly greater utility.22 Indeed, device non-use observed in the present study would substantially reduce predicted cost-utility in children who received their implants at older ages.
Future research incorporating data from CI processors with data logging capabilities will allow for more detailed investigations into precise rates and patterns of CI use. Importantly, such data will enable a greater understanding of the factors affecting daily usage and correlates of performance.
Supplementary Material
Acknowledgments
Funding: This manuscript was supported in part by NIH K23DC011279, the Eleanor Schwartz Charitable Foundation, and a Triological Society/American College of Surgeons Clinician Scientist Award.
Footnotes
Disclosures: Dr. Frank Lin reports being a consultant to Cochlear, on the scientific advisory board for Autifony and Pfizer, and a speaker for Med El and Amplifon
REFERENCES
- 1.Disorders NIoDaOC Cochlear Implants. NIH Publication No. 11-4798. 2011. Accessed March 26, 2012.
- 2.Geers AE, Sedey AL. Language and verbal reasoning skills in adolescents with 10 or more years of cochlear implant experience. Ear and hearing. 2011 Feb;32(1 Suppl):39S–48S. doi: 10.1097/AUD.0b013e3181fa41dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niparko JK, Tobey EA, Thal DJ, et al. JAMA : the journal of the American Medical Association. 2010 Apr 21;303(15):1498–1506. [Google Scholar]
- 4.Spencer LJ, Barker BA, Tomblin JB. Exploring the language and literacy outcomes of pediatric cochlear implant users. Ear and hearing. 2003 Jun;24(3):236–247. doi: 10.1097/01.AUD.0000069231.72244.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Svirsky MA, Robbins AM, Kirk KI, Pisoni DB, Miyamoto RT. Language development in profoundly deaf children with cochlear implants. Psychological science. 2000 Mar;11(2):153–158. doi: 10.1111/1467-9280.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beadle EA, McKinley DJ, Nikolopoulos TP, Brough J, O'Donoghue GM, Archbold SM. Long-term functional outcomes and academic-occupational status in implanted children after 10 to 14 years of cochlear implant use. Otol Neurotol. 2005 Nov;26(6):1152–1160. doi: 10.1097/01.mao.0000180483.16619.8f. [DOI] [PubMed] [Google Scholar]
- 7.Uziel AS, Sillon M, Vieu A, et al. Ten-year follow-up of a consecutive series of children with multichannel cochlear implants. Otol Neurotol. 2007 Aug;28(5):615–628. doi: 10.1097/01.mao.0000281802.59444.02. [DOI] [PubMed] [Google Scholar]
- 8.Spencer LJ, Gantz BJ, Knutson JF. Outcomes and achievement of students who grew up with access to cochlear implants. The Laryngoscope. 2004 Sep;114(9):1576–1581. doi: 10.1097/00005537-200409000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waltzman SB, Cohen NL, Green J, Roland JT., Jr. Long-term effects of cochlear implants in children. Otolaryngol Head Neck Surg. 2002 May;126(5):505–511. doi: 10.1067/mhn.2002.124472. [DOI] [PubMed] [Google Scholar]
- 10.Summerfield AQ, Marshall DH. Paediatric cochlear implantation and health-technology assessment. Int J Pediatr Otorhinolaryngol. 1999 Feb 15;47(2):141–151. doi: 10.1016/s0165-5876(98)00133-5. [DOI] [PubMed] [Google Scholar]
- 11.R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2012. computer program. [Google Scholar]
- 12.A Package for Survival Analysis in S. [computer program]. Version R package version 2.36-142012.
- 13.Haensel J, Engelke JC, Ottenjann W, Westhofen M. Long-term results of cochlear implantation in children. Otolaryngol Head Neck Surg. 2005 Mar;132(3):456–458. doi: 10.1016/j.otohns.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 14.Archbold SM, Nikolopoulos TP, Lloyd-Richmond H. Long-term use of cochlear implant systems in paediatric recipients and factors contributing to non-use. Cochlear implants international. 2009 Mar;10(1):25–40. doi: 10.1179/cim.2009.10.1.25. [DOI] [PubMed] [Google Scholar]
- 15.Pastides H, Goldberg RJ. Case-control studies in pediatric epidemiology: parent surrogates and potential pitfalls of inaccurate and selective recall. Sozial- und Praventivmedizin. 1992;37(1):22–26. doi: 10.1007/BF01369098. [DOI] [PubMed] [Google Scholar]
- 16.Coughlin SS. Recall bias in epidemiologic studies. Journal of clinical epidemiology. 1990;43(1):87–91. doi: 10.1016/0895-4356(90)90060-3. [DOI] [PubMed] [Google Scholar]
- 17.Butz AM, Donithan M, Bollinger ME, Rand C, Thompson RE. Monitoring nebulizer use in children: comparison of electronic and asthma diary data. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology. 2005 Mar;94(3):360–365. doi: 10.1016/S1081-1206(10)60988-X. [DOI] [PubMed] [Google Scholar]
- 18.Berg J, Dunbar-Jacob J, Rohay JM. Compliance with inhaled medications: the relationship between diary and electronic monitor. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 1998;20(1):36–38. doi: 10.1007/BF02893807. Winter. [DOI] [PubMed] [Google Scholar]
- 19.Cheng AK, Rubin HR, Powe NR, Mellon NK, Francis HW, Niparko JK. Cost-utility analysis of the cochlear implant in children. JAMA : the journal of the American Medical Association. 2000 Aug 16;284(7):850–856. doi: 10.1001/jama.284.7.850. [DOI] [PubMed] [Google Scholar]
- 20.Barton GR, Stacey PC, Fortnum HM, Summerfield AQ. Hearing-impaired children in the United Kingdom, IV: cost-effectiveness of pediatric cochlear implantation. Ear and hearing. 2006 Oct;27(5):575–588. doi: 10.1097/01.aud.0000233967.11072.24. [DOI] [PubMed] [Google Scholar]
- 21.The Laryngoscope. 2000 Jan;110(1):156–160. doi: 10.1097/00005537-200001000-00028. [DOI] [PubMed] [Google Scholar]
- 22.Semenov YR, Yeh ST, Seshamani M, et al. Age-Dependent Cost-Utility of Pediatric Cochlear Implantation. Ear and hearing. 2013 Feb 7; doi: 10.1097/AUD.0b013e3182772c66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.