Abstract
While increased serum phosphate concentration is a significant risk factor for vascular calcification, it is unclear whether serum phosphate is also a risk factor for increased arterial wall thickness in chronic kidney disease (CKD) patients. Using B-mode ultrasonography, we examined carotid intimal-medial thickness (CIMT) of CKD patients and analyzed risk factors for increased IMT with regard to the effect of serum phosphate. One hundred patients were enrolled (73 patients without diabetes, 27 patients with diabetes; 57 men, 43 women; age, 46.2 ± 15.3 years). CIMT of patients with diabetes was significantly greater than that of patients without diabetes (0.78 ± 0.250 versus 0.66 ± 0.178 mm; P < 0.0001). For the group of all patients, CIMT correlated strongly and significantly with serum phosphate (r = 0.911; P < 0.001). In multiple regression analysis serum phosphate level (β = 0.356; <0.0001) was found to be a significant independent risk factor for increased CIMT, in addition to other independent risk factors, including advanced age, higher systolic blood pressure, urinary albumin and the presence of diabetes (R2 = 0.956; P < 0.00001). In conclusion, high serum phosphate level is a significant and independent factor associated with advanced arteriosclerosis in CKD patients with and without diabetes in addition to advanced age.
Keywords: Carotid intimal-medial thickness, chronic kidney disease, diabetes, phosphate
Introduction
Chronic kidney disease (CKD) is a significant predictor of cardiovascular disease.[1,2,3] Cardiovascular disease and stroke are the leading causes of death in patients with end-stage renal disease, who have a risk for death 10 to 20 times that of age- and sex-matched general population.[4,5,6] It has been recently reported that arteriosclerosis, assessed by means of the arterial wall thickness and stiffness, is advanced in patients with the chronic renal failure.[7,8] In the general population, advanced age, hypertension, cigarette smoking and hyperlipidemia are the most significant risk factors for advanced arteriosclerosis,[9] In uremic patients, it is unclear whether risk factors for arteriosclerosis are similar to those in the non-uremic population; it is also unclear whether there is a difference in risk factors for advance arteriosclerosis between uremic patients without and with diabetes. Although increased serum phosphate concentration is a significant risk factor for vascular calcification,[10] which is an advanced form of atherosclerosis, it is unclear whether serum phosphate concentration is associated with arterial wall thickness in CKD. In the present study, using a non-invasive method of B-mode ultrasonography, we examined carotid arterial thickness of a 100 CKD patients and explored risk factors for an increase in the arterial wall thickness. We focus on risk factors for arteriosclerosis of CKD patients without and with diabetes, separately, and examined whether serum phosphate level is associated with carotid arterial thickness.
Materials and Methods
Patients
A total of 124 patients with diagnosis of CKD meeting the inclusion and exclusion criteria were enrolled for study in medicine/nephrology Department of Hamidia Hospital Bhopal from 1 December 2011 to 30 October 2012. This study was approved by the Gandhi Medical College and Hamidia Hospital Bhopal. Patient having diagnosed as acute kidney injury, history of carotid surgery, patient having previous history of ischemic heart disease, myocardial infarction and stroke were excluded.
Of these, 116 patients CKD patients gave informed consent to participate in the study, and 100 patients could complete the requisite battery of investigation and their clinical data were analyzed. Of these patients, 27 patients had type 2 diabetes, 13 men and 14 women aged 30 to 75 years (mean, 53.93 ± 12.40 years), 12 receiving dialysis and 15 not receiving dialysis and 73 patients did not have diabetes consisting of 44 men and 29 women with an age range of 14 to 80 years (mean, 44.04 ± 16.80 years), 40 were on dialysis and 33 were not on dialysis. Glomerular filtration rate (GFR) was calculated using Cockcroft-Gault formula. Maximum 77 patients were in CKD stage 5, 18 were in stage 4 and 5 were in CKD stage 3. The percentage of patients with diabetes (27%) is similar to that for the population of patients with CKD in India at the end of 2011 (28.1%).
Blood pressure was recorded with standard mercury sphygmomanometer with cuff adapted to arm circumference without arteriovenous fistula, after the subject had rested in the supine position for 15 minutes. The systolic and diastolic blood pressure levels were taken as the points of appearance and disappearance of Korotkoff sounds respectively. Three measurements were taken with 10 min break and average of measurements was taken as the final value of blood pressure. Body mass index (BMI) was calculated using the formula: BMI = Weight (Kg)/Height2 (m2).
The presence of cardiovascular complication was evaluated by means of clinical information on patient charts regarding past and present history of coronary (myocardial infarction, angina pectoris), cerebral (stroke), and peripheral (amputation, angiographically shown arteriosclerosis obliterans) artery diseases. Information for cardiovascular medications, including antihypertensives and nitrites were collected from patient charts.
Measurements of carotid artery intimal-medial thickness
Carotid intima media thickness was measured by B mode ultrasound using a 3.5MHz transducer. Intima Media Thickness is defined as distance between the leading edge of first echogenic line (Lumen–Intima interface) and second echogenic line (Media– Adventitia interface) of far wall. Three measurements were taken 0.5, 1 and 2 cm below carotid bifurcation of common carotid artery on each side. The arithmetical averages of these were taken. The IMT of both sides (right and left) was calculated and averages of these two values were used for statistical analysis. Carotid intimal-medial thickness (CIMT) measurement was always performed by single radiologist in plaque free arterial segments. Plaques are defined as focal widening relative to the adjacent segment, with protrusion into the lumen. For different parameters, mean and standard deviation was calculated. The values of P which are (P < 0.05) were treated as significant.
Biochemical assays
Blood was drawn after 8 hour of overnight fasting to measure serum parameters such as albumin, creatinine, hemoglobin, C-reactive protein (CRP), calcium, phosphate, total cholesterol, high-density lipoprotein (HDL) cholesterol and triglyceride. Morning urine sample was taken for estimation of urinary albumin. Measurements were performed using routine laboratory methods. Corrected calcium was calculated by using formula: Corrected calcium = 0.8 (4-serum albumin) + serum calcium (mg/dL).
Statistical analysis
All values were expressed as mean ± SD. Unpaired Student's t-test and Chi-square test were performed for comparison of CKD patients without and with diabetes. Correlation and multiple linear regression analysis were performed to examine relationships between IMT and clinical variables. Multiple regression analysis was performed to assess the combined effects of clinical variables on CIMT. Dummy variables were used for sex (1 for male, 2 for female), diabetes (1 for no diabetes, 2 for diabetes) modality of treatment (1 for Dialysis, 2 for not on dialysis). P < 0.05 was considered statistically significant. All statistical analyses were performed by using the SPSS Version 17.0.
Results
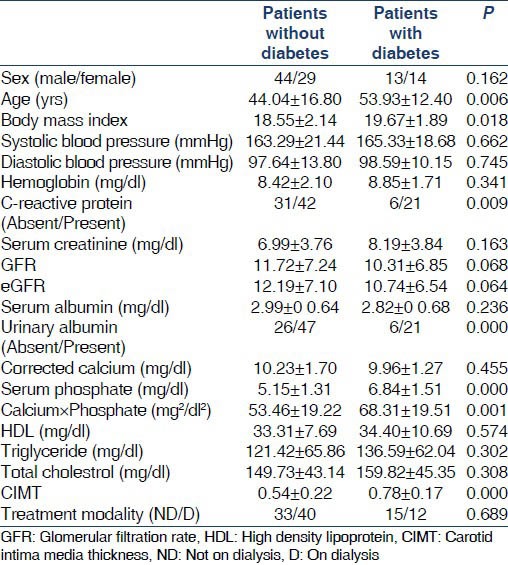
Table 1 lists clinical characteristics of CKD patients without and with diabetes. Age, BMI, Systolic blood pressure, CRP, urinary albumin, serum phosphate and calcium phosphate product of CKD patient were significantly higher with diabetes than those of non-diabetes. Other clinical parameter did not different significantly between the two groups. The patient in CKD group without diabetes had higher values of serum albumin, GFR, corrected serum calcium whereas values were more for BMI, systemic blood pressure, diastolic blood pressure, hemoglobin, serum creatinine, high-density lipoprotein, low-density lipoprotein and total cholesterol in the diabetic group.
Table 1.
Patient clinical characteristics according to presence of diabetes
Relationship between carotid intimal-medial thickness and clinical parameters
Relationship between CIMT and clinical parameters were examined for the groups for all patients, patients without diabetes and CKD patients with diabetes separately by mean of correlation analysis [Table 2]. In the group of all CKD patients, significant high positive correlation were found between mean carotid intimal-medial thickness (mCIMT) and age, BMI, systolic blood pressure, Corrected serum calcium, serum phosphorous and calcium phosphate product. The correlation was strong with Age, BMI, systemic blood pressure, urinary albumin and serum phosphate but is only mildly correlated with corrected calcium. There was mild negative correlation mCIMT with GFR, which is also significant statistically. There was a negative correlation with serum albumin in group of all patients, but it is not significant statistically.
Table 2.
Clinical characteristics of all patients without and with diabetes
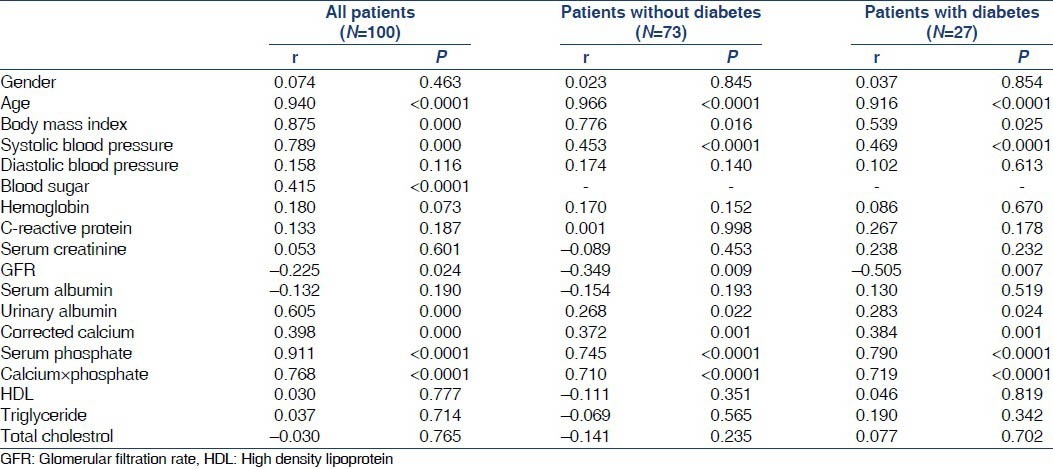
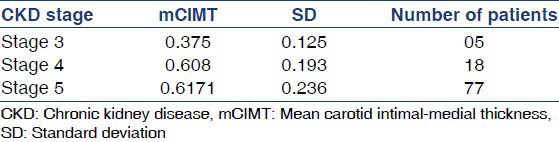
Similar results were found in the CKD patients without and with diabetes but the correlation were moderate for systolic blood pressure, BMI, calcium phosphate product in both groups with significant difference. The correlation was weak for urinary albumin, corrected calcium, but with statistically significant difference. There was weak negative correction with GFR in both non-diabetic and diabetic group with significant statistical difference. However, no significant correlation could be established with diastolic blood pressure, CRP, HDL, Triglyceride, Total cholesterol in any of the group under study. There was direct correlation of mCIMT and CKD stage (P ≤ 0.0001). As the stage of CKD increases the mCIMT increases but in our study more increase is noted between stage 3 and stage 4 and little increment between stage 4 and stage 5 as depicted in Table 3.
Table 3.
Distribution of mCIMT and number of patients as per CKD staging by Cockcroft-Gault formula
Risk factors for increased CIMT
To examine the combined effect of factors affecting CIMT, multiple regression analysis was performed separately for the group of all patients, patients without and with diabetes [Table 4]. Independent variables were selected based on results of correlation analysis performed on the group in the study separately. Results were similar in the study groups and it was found that serum phosphate was significant and independent risk factor for increased CIMT in addition to the conventional risk factor such as blood sugar, age, BMI, Systolic blood pressure and urinary albumin. The relationship between CIMT and serum phosphate level in the group of all CKD patients is shown in Figure 1.
Table 4.
Multiple linear regression analysis of factors associated with CIMT
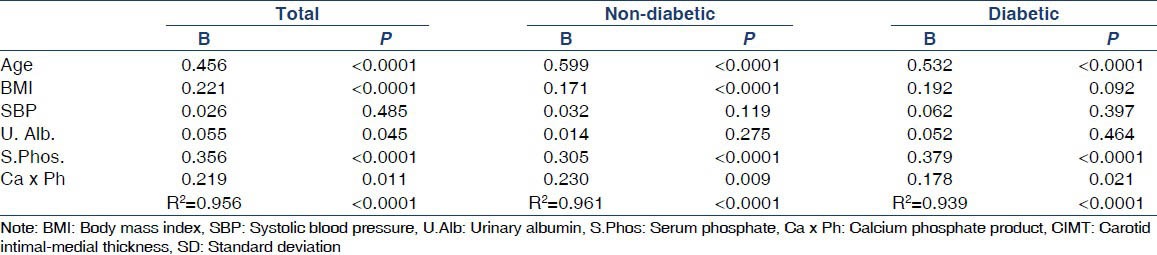
Figure 1.
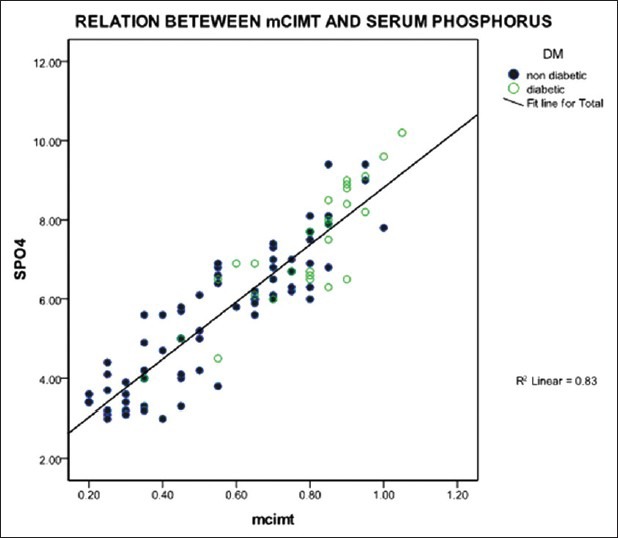
Scatter diagram showing relationship between mCIMT and serum Phosphorus using multiple linear regression analysis
Discussion
CIMT, which can be measured noninvasively using B-mode ultrasonography, has been reported be an early marker of atherosclerosis and predictor of vascular events. By examining 100 CKD patients in the present study, we showed that arteriosclerosis, assessed by means of CIMT of CKD patients with diabetes, was significantly advanced compared with that of CKD patients without diabetes. Furthermore, analyses of factors associated with advanced arteriosclerosis showed that increased serum phosphate level was one of the significant and independent factors associated with increased IMT of the carotid artery, not only for the group of all patients, but also for CKD patients with and without diabetes, in addition to advanced age and other conventional risk factors.
Recently, arteriosclerosis was reported to be advanced in patients with chronic renal failure,[7] and CKD has been emphasized as a significant predictor of cardiovascular disease.[1,2,3] In previous studies, IMT in patients with uremia, not only those on hemodialysis therapy, but also predialysis uremic patients, was advanced compared with that in control subjects. Ishimura et al., found risk factors for increased CIMT for the group of all hemodialysis patients, patients without diabetes and with diabetes.[11,12] They found that older age, higher systolic blood pressure and diabetes were significant and independent risk factors. In addition to these factors, serum phosphate level was also found to be a significant independent risk factor for increased CIMT in hemodialysis patients (P ≤ 0.001). Oh et al.,[13] in an examination of 39 patients with young onset chronic renal failure, also found a significant correlation between serum phosphate level, CRP and CIMT in their study (P ≤ 0.001). Goodman et al.,[14] demonstrated in children and young adults that increase due to calcium containing phosphate binder and increased calcium phosphate product causes advanced calcification and increase in carotid and coronary artery thickness. Similar results with increased calcium phosphate product with increased CIMT were noted in our study. Desbien et al.,[15] found decreased kidney function is associated strongly with faster change in CIMT. Similar changes were noted in our study as mCIMT in CKD stage 3, 4, 5 were 0.375 ± 0.125 mm, 0.608 ± 0.193 mm, 0.6171 ± 0.236 mm respectively. Faster change is noted between stage 3 and stage 4 CKD as compared to stage 4 and stage 5. In the analysis of the group of all CKD patients, serum phosphate level was a significant risk factor for increased CIMT independent of other confounding factors. There was very strong correlation between mCIMT and serum phosphate in our study group (P < 0.0001).
In CKD patients, hyperphosphatemia has been emphasized as a significant risk factor for the development of secondary hyperparathyroidism and uremic bone disease.[16,17] Hyperphosphatemia has been reported to be a significant risk factor for vascular calcification and phosphate level reduction by means of phosphate binders has been reported to attenuate vascular calcification.[18,19] These studies examined vascular calcification, not the degree of arterial thickness itself. Recently, inorganic phosphate was reported to induce phenotypic change of vascular smooth muscle cells in vitro into osteoblast-like cells, such as inducing alkaline phosphatase and calcium-binding protein (osteocalcin and osteopontin).[20,21,22] Inorganic phosphate also induced by core-binding factor a 1, a key transcription factor in osteoblastic differentiation, in vascular smooth muscle cells in vitro.[21,22] These in vitro findings, suggest that hyperphosphatemia may induce osteoblastic phenotypic changes in vascular smooth muscle cells and vascular cell proliferation, possibly leading to increased arterial wall thickness in CKD patients.
In conclusion, in an examination of the CIMT of CKD patients, we found that greater serum phosphate level was one of the significant and independent factors associated with increased IMT, in addition to advance age, serum albumin, urinary albumin and calcium phosphate product. Correction of hyperphosphatemia may be emphasized for the prevention of progression of arteriosclerosis, in addition to prevention of vascular calcification, in CKD patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Weiner DE, Tighiouart H, Amin MG, Stark PC, MacLeod B, Griffith JL, et al. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: A pooled analysis of community-based studies. J Am Soc Nephrol. 2004;15:1307–15. doi: 10.1097/01.asn.0000123691.46138.e2. [DOI] [PubMed] [Google Scholar]
- 2.Coresh J, Astor B, Sarnak MJ. Evidence for increased cardiovascular disease risk in patients with chronic kidney disease. Curr Opin Nephrol Hypertens. 2004;13:73–81. doi: 10.1097/00041552-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem DN, Griffith JL, et al. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol. 2003;41:47–55. doi: 10.1016/s0735-1097(02)02663-3. [DOI] [PubMed] [Google Scholar]
- 4.Foley RN, Parfrey PS, Sarnak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis. 1998;32(Suppl 3):S112–9. doi: 10.1053/ajkd.1998.v32.pm9820470. [DOI] [PubMed] [Google Scholar]
- 5.Bethesda, MD: The National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 1999. US Renal Data System: USRDS 1998 Annual Data Report. [Google Scholar]
- 6.Ma KW, Greene EL, Raij L. Cardiovascular risk factors in chronic renal failure and hemodialysis populations. Am J Kidney Dis. 1992;19:505–13. doi: 10.1016/s0272-6386(12)80827-4. [DOI] [PubMed] [Google Scholar]
- 7.Shoji T, Emoto M, Tabata T, Kimoto E, Shinohara K, Maekawa K, et al. Advanced atherosclerosis in predialysis patients with chronic renal failure. Kidney Int. 2002;61:2187–92. doi: 10.1046/j.1523-1755.2002.00372.x. [DOI] [PubMed] [Google Scholar]
- 8.Shinohara K, Shoji T, Tsujimoto Y, Kimoto E, Tahara H, Koyama H, et al. Arterial stiffness in predialysis patients with uremia. Kidney Int. 2004;65:936–43. doi: 10.1111/j.1523-1755.2004.00468.x. [DOI] [PubMed] [Google Scholar]
- 9.Hiatt WR. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001;344:1608–21. doi: 10.1056/NEJM200105243442108. [DOI] [PubMed] [Google Scholar]
- 10.Davies MR, Hruska KA. Pathophysiological mechanisms of vascular calcification in end-stage renal disease. Kidney Int. 2001;60:472–9. doi: 10.1046/j.1523-1755.2001.060002472.x. [DOI] [PubMed] [Google Scholar]
- 11.Ishimura E, Taniwaki H, Tabata T, Tsujimoto Y, Jono S, Emoto M, et al. Cross-sectional association of serum phosphate with carotid intima-medial thickness in hemodialysis patients. Am J Kidney Dis. 2005;45:859–65. doi: 10.1053/j.ajkd.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Ishimura E, Shoji T, Emoto M, Motoyama K, Shinohara K, Matsumoto N, et al. Renal insufficiency accelerates atherosclerosis in patients with type 2 diabetes mellitus. Am J Kidney Dis. 2001;38(Suppl 1):S186–90. doi: 10.1053/ajkd.2001.27440. [DOI] [PubMed] [Google Scholar]
- 13.Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, et al. Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation. 2002;106:100–5. doi: 10.1161/01.cir.0000020222.63035.c0. [DOI] [PubMed] [Google Scholar]
- 14.Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000;342:1478–83. doi: 10.1056/NEJM200005183422003. [DOI] [PubMed] [Google Scholar]
- 15.Desbien AM, Chonchol M, Gnahn H, Sander D. Kidney function and progression of carotid intima-media thickness in a community study. Am J Kidney Dis. 2008;51:584–93. doi: 10.1053/j.ajkd.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 16.Nolan CR, Qunibi WY. Calcium salts in the treatment of hyperphosphatemia in hemodialysis patients. Curr Opin Nephrol Hypertens. 2003;12:373–9. doi: 10.1097/00041552-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Behets GJ, Verberckmoes SC, D’Haese PC, De Broe ME. Lanthanum carbonate: A new phosphate binder. Curr Opin Nephrol Hypertens. 2004;13:403–9. doi: 10.1097/01.mnh.0000133973.86816.e9. [DOI] [PubMed] [Google Scholar]
- 18.Cozzolino M, Dusso AS, Slatopolsky E. Role of calcium-phosphate product and bone-associated proteins on vascular calcification in renal failure. J Am Soc Nephrol. 2001;12:2511–6. doi: 10.1681/ASN.V12112511. [DOI] [PubMed] [Google Scholar]
- 19.Chertow GM, Burke SK, Raggi P Treat to Goal Working Group. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245–52. doi: 10.1046/j.1523-1755.2002.00434.x. [DOI] [PubMed] [Google Scholar]
- 20.Jono S, McKee MD, Murry CE, Shioi A, Nishizawa Y, Mori K, et al. Phosphate regulation of vascular smooth muscle cell calcification. Circ Res. 2000;87:E10–7. doi: 10.1161/01.res.87.7.e10. [DOI] [PubMed] [Google Scholar]
- 21.Giachelli CM, Jono S, Shioi A, Nishizawa Y, Mori K, Morii H. Vascular calcification and inorganic phosphate. Am J Kidney Dis. 2001;38(Suppl 1):S34–7. doi: 10.1053/ajkd.2001.27394. [DOI] [PubMed] [Google Scholar]
- 22.Shioi A, Mori K, Jono S, Wakikawa T, Hiura Y, Koyama H, et al. Mechanism of atherosclerotic calcification. Z Kardiol. 2000;89(Suppl 2):75–9. doi: 10.1007/s003920070103. [DOI] [PubMed] [Google Scholar]


