Abstract
Nicotine in tobacco smoke causes not only pathophysiological changes in the smoker's body, but also develops tolerance to its own action with repeated use. Repeated exposure to nicotine develops neuroadaptation of the receptors, resulting in tolerance to many of the effects of nicotine. Pharmacotherapies for smoking cessation should reduce withdrawal symptoms and block the reinforcing effects of nicotine without causing excessive adverse effects. All forms of nicotine replacement therapy (NRT) – gum, patches and inhaler – and bupropion are safe and effective for increasing smoking cessation rates in the short and long-term use. Combination NRT (more than one therapy) may be indicated in patients who have failed monotherapy.
Keywords: Nicotine replacement therapy, smoking cessation, varenicline
INTRODUCTION
The ubiquity of tobacco smoking and its persistence in the face of vigorous proscriptions, despite the generally agreed health risks, is a remarkable phenomenon. Tobacco smoking is highly contextual and associated with certain rituals, which start with the opening of a packet of cigarettes or a bundle of beedi, followed by the lighting process and then the sight and smell of smoke. Tobacco smoking is one of the strangest of human behaviors.[1] Why should world's one-third adult population perform an act which is necessary neither for the maintenance of life nor for the satisfaction of social, cultural or spiritual needs, an act which is acknowledged by the smokers to be harmful to health and even distasteful?
BASIC NEUROBIOLOGY OF SMOKING
From the incandescent tip of a lighted cigarette, burning at a temperature of 800°C, the smoker with each puff draws into his mouth a hot potpourri of gases and many sized particles. Of the 4000 chemicals identified in tobacco smoke, nicotine is the pharmacological agent of prime importance, which is highly toxic and potentially lethal alkaloid (1-methyl-2-[3-pyrodyl] pyrrolidine), responsible for a number of pathophysiological changes in the body. Nicotine remains dissolved in the moisture of the tobacco leaf as a water soluble salt, but in a burning cigarette it volatilizes and remains suspended on minute droplets of tar as free nicotine. These droplets, less than 1000 of a millimeter across, can reach the smallest alveoli in the lungs. About 90% of nicotine present in inhaled smoke is absorbed.[2] Absorption leads to a marked increase in arterial nicotine level within 15 seconds.[3] Blood nicotine levels rise very rapidly and peak at the time cigarette is extinguished and steep decline occurs until the next cigarette is smoked.[4] This bolus of nicotine activates the brain-reward system by increasing dopamine release as it is a potent psycho-active drug.[5] This brain reward system is a common pathway for pleasurable activities in most drugs of addiction.[6] The euphoria induced serves as a re-inforcer for its use. This peak in plasma nicotine level and the transient activation of the reward system is followed by a gradual fall in nicotine levels into a state of withdrawal that is, in turn, relieved by the next cigarette. Nicotine meets the criteria for a highly addictive drug and a great majority of regular smokers are dependent on tobacco smoking and not simply addicted to nicotine.[7] Dependence arises from the temporal association of the rituals and sensory inputs with the repeated stimulation and relief of withdrawal symptoms.[2] This required association explains why nicotine replacement therapy (NRT) products, that deliver nicotine slowly and do not produce high plasma nicotine levels, have minimal addictive potential.[8]
CUES TO SMOKING
Some people smoke when they work alone and others when they are in company. Cues, such as an ashtray, the sight of seeing the other person smoking etc., can elicit strong craving not only in newly abstained and current smokers, but also in individuals who have achieved long term abstinence.[9] Some people smoke excessively when they are angry, frustrated, or unhappy. They may be vulnerable to a crisis even when the crisis occurs after an extended period of abstinence.[10] Some smokers rely heavily upon nicotine in regulating their mood, especially negative affect, whereas some use smoking as a means of sustaining attention. There are some others who use smoking as an aid to relaxation.[11] Nicotine in tobacco smoke affects mood and performance that can become the source of addiction to tobacco.[12]
Tobacco smoking like any other form of drug dependence, involves both pharmacological and behavioral factors and therefore treatment approaches involve pharmacological agents, behavioral strategies, or a combination of both.
BARRIERS TO SMOKING CESSATION
Addiction
Addiction to nicotine is the main barrier for smoking cessation.[13] Individual smokers are often not aware that they are at as much risk of becoming addicted as other smokers. It may be the intake of just four cigarettes that a person is exposed to the risk of becoming an addict.[14] The first symptoms of nicotine addiction can appear within days to weeks of the onset of occasional use, often before the onset of daily smoking. Addiction then becomes the main barrier for smoking cessation.[15] Withdrawal symptoms in adults and children include increased irritability, restlessness and depression, difficulty with concentration, hunger and craving. Physiological changes occur in the brain, along with a drop in the heart rate and adrenal output and a rise in skin temperature.[16]
Fear of weight gain
Fear of weight gain is quite common in women[17] and some women smoke cigarettes to control their weight.[18] Smoking increases metabolic rate, which may fall with smoking cessation.[19] Nicotine increases the energy expenditure associated with light activity.[20] Tobacco smoking may independently reduce serum leptin concentrations, rather than smokers having lower leptin levels just because they are leaner. Nicotine, through its various effects on the central nervous system, may modify leptin sensitivity, resulting indirectly into reduced leptin levels and maintenance of a lower body weight.[21] Many women start and continue to smoke to control appetite and reduce bodyweight[22] that may be an attempt to restrain post-puberty fatness.[23] Women gain more weight than men, in the proportion of 3.8-2.8 kg, when they quit smoking.[24] Heavy smokers tend to gain more weight during attempts to quit.[25] During the 1st month of smoking cessation, the average caloric intake increases by 300-400 calories/day.[26] Fear of weight gain leads to relapse after cessation and young women are 3-4 times as likely as men to report weight gain as a cause of smoking relapse.[27]
Depression
Depression is twice as common among women as men and can present another barrier for smoking cessation in women.[28] Childbirth and menstrual cycle[29] are associated with depression and may even serve as a trigger for an episode of major depression.[30] Depression is also found to be 4 times more common among smokers than non-smokers.[31] Hormones related to the reproductive cycle influence depression and smoking behavior. Women use smoking for mood management and for coping with stress.[32] Some smokers may self-medicate depressed moods with nicotine.[33] Smoking also helps in the treatment for depression with nicotine and monoamine-oxidase (MAO) inhibitors present in tobacco smoke. Neurotransmitters such as glutamate and serotonin are also implicated.[34]
Smoking cessation itself may provoke depression among smokers who may or may not have histories of major depression. When depressive symptoms emerge during withdrawal from nicotine, the likelihood is higher for both cessation failure and relapse. Furthermore, resumption of smoking can reverse depression symptoms.[31]
TREATMENT
Nicotine dependence warrants medical treatment as does any drug-dependence disorder or chronic disease.[35] A detailed history, severity of addiction and motivation to leave smoking, physical and mental health status and co-morbidity need to be assessed before staring treatment. Environmental factors, possibly working as re-inforcers need to be evaluated. Benefits of tobacco-cessation and the cessation process along with the possible withdrawal symptoms should be explained to the patient. In consultation with the patient, treatment strategy that suits the patient should be selected. Severity of nicotine dependence should be assessed with the help of available questionnaires such as CAGE questionnaire, a simple, accurate tool for screening patients with addictive disorders.[36,37] This questionnaire has been revised to evaluate smoking behavior[38] and can be included in clinical interview. Fagerstrom test for nicotine dependence has six questions, based on the DSM IV criteria and quantifies high, moderate and minimal dependence.[2]
PHARMACOLOGICAL APPROCHES
A pharmacological treatment for smoking cessation should both block the positive reinforcing effect of nicotine and prevent or reduce the development of withdrawal symptoms. Pharmacotherapy should also target the receptor subtypes involved in nicotine addiction without affecting the receptors that if activated, would produce unwanted adverse effects.[39]
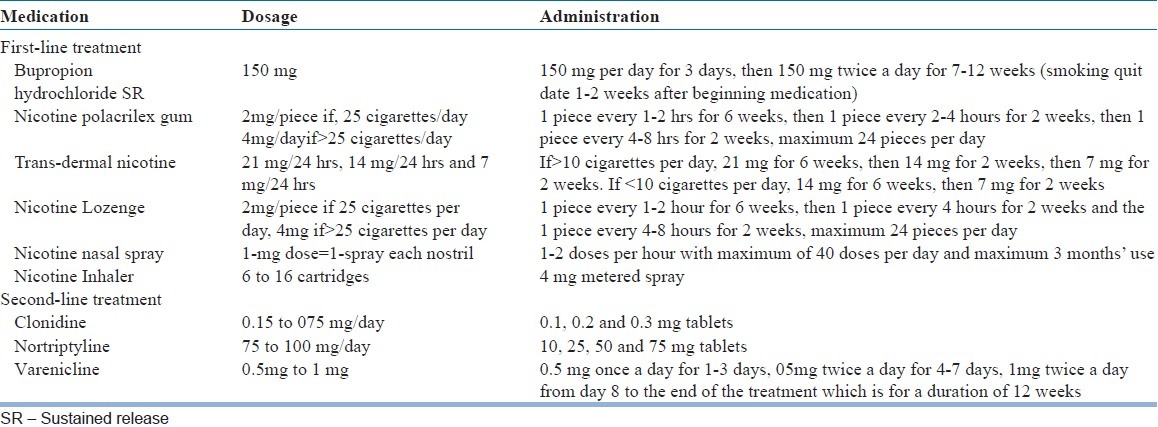
Food and Drug Administration (FDA) of USA approved medications used for smoking-cessation include NRT trans-dermal patch, gum, nasal spray, inhaler and lozenges;[40,41] Bupropion and varenicline. Nortriptyline and clonidine, though not approved by the FDA, are clinically effective in smoking-cessation.[42] The first line medications for smoking cessation are NRT and sustained release (SR) Bupropion. Other medications used as second line treatment are clonidine, nortriptyline and varenicline.
NRT
The general principle of replacement therapies is to present the patient with a safer and more therapeutically manageable form of the drug that directly alleviates the signs and symptoms of withdrawal and craving. NRT is modeled after those originally developed to treat dependence on heroin and other opiates.[43] A variety of non-tobacco-based delivery systems provide potentially effective means for nicotine replacement.
Nicotine injection
The first attempt to use nicotine injection was made by a Wallace general practitioner, Lennox Johnston in 1942 to help people quit smoking. 1/7500 and 1/500 of a grain of intravenous nicotine, which produced sensations equivalent to those following one deep inhalation from a cigarette, was used. Non-smokers found the sensations queer, but the smokers found them pleasant and after repeated injections, did not feel inclined to smoke for a while afterwards. This showed that the injected nicotine could substitute for sensations that were normally derived from smoking. However, this trial was not free from the possible influence of conscious and unconscious expectations.[2] In another experiment smokers receiving a slow intravenous infusion of either nicotine solution or saline water solution, were subjected to perform a variety of psychological tests and their blood pressure and the electrocardiogram were measured. The injection of 22 mg of nicotine (equivalent to the nicotine delivery of 22 medium-strength cigarettes) was accompanied by a 30% drop in the number of cigarettes smoked.[44] However, this approach is not clinically viable since the nicotine half-life is short and repeated administration of nicotine can lead to toxicity.
Nicotine polacrilex Gums
The next systematic approach was the development of nicotine polacrilex gum.[45] The weaning from nicotine actually begins with the switch from cigarette to gum in that nicotine polacrilex (1) produces slower-rising plasma nicotine levels than cigarette and (2) reduces the inhaled nicotine bolus effect believed to contribute to nicotine's addictive potential in smoke. The same mechanism applies to other replacement approaches including nicotine trans-dermal delivery, nasal nicotine solution (NNS) and smoke-free nicotine cigarettes. The different forms allow variation in delivery (dose and speed), which may influence effectiveness, relief of withdrawal, patient acceptance and outcome.[2]
Although guidelines for selecting different NRT have not been established, clinicians should individualize the treatment based on the patient characteristics and adverse effect profile of each product. NRT attenuates the tobacco withdrawal symptoms and approximately doubles the success rate of quitting smoking relative to smoking.[46]
“Nicotine resin complex” commonly known as nicotine gum, is a nicotine delivery system in which the nicotine is incorporated into an ion exchange resin base, which permits release of nicotine in the proper environment (i.e., saliva in the mouth) when appropriate physical pressure (i.e., chewing) is applied. At 20-30 min of proper chewing results in the release of approximately 90% of nicotine, although there are multiple determinants of how much nicotine actually is absorbed. 10-15 min of chewing results in the release of approximately 50-60% of nicotine in a piece of gum. Variability exists both within and across subjects. Swallowed nicotine is approximately 70% detoxified because of its first pass through the liver. 2 mg and 4 mg nicotine polacrilex gum has been used. 2 mg piece nicotine polacrilex chewing gum is the only one form of nicotine replacement strategy approved by the FDA of United States.
Nicotine-specific withdrawal symptoms, which interfere with successful cessation, can be prevented or attenuated by nicotine replacement. This therapy promotes cessation as well as prevents relapse. Nicotine gum does not fully replace the nicotine provided by cigarette smoking. 4-mg nicotine gum produces plasma nicotine level approximating that of a 1.2 mg-nicotine-yield cigarette. When nicotine polacrilex gum is chewed, drug levels of plasma rise slowly and peak in around 20-30 min, whereas 4-mg gum replaces nicotine more completely. However, effective nicotine replacement strategies may not require the same range of nicotine blood levels as those produced by cigarette smoking. Perhaps because of this, only the 2-mg dose has been approved. The 2-mg nicotine polacrilex gum increases nicotine cessation rates significantly in several placebo-controlled studies.[2] Nicotine gum is quickly absorbed and closely approximates the course of plasma nicotine levels observed after cigarette smoking.
Studies show that nicotine polacrilex gum reduces symptoms of withdrawal in comparison to placebo controls.[47] The degree of relief is directly related to the dose of nicotine that is actually obtained when the polacrilex gum is used.[48] The urge to smoke (craving) is not reliably decreased by nicotine replacement.[49]
Weight gain, is a significant problem in smoking-cessation. It can be reduced by NRT.[50] A 2-mg nicotine gum dose has been found to produce significantly less weight gain.[51]
Craving, often described as an increased urge or desire to use a drug often forces an individual to use a drug. Craving generally is not relieved by NRT. However, to some extent, relief of craving has been reported with 2-mg nicotine polacrilex gum compared with placebo controls in some outcome trials.[52]
4-mg nicotine polacrilex gum improved success rate for more highly dependent tobacco smokers, whereas 2-mg nicotine polacrilex gum is found better in less dependent smokers. In general, 2 mg gum pieces are used for consumers who use <25 cigarettes/day and 4 mg gum pieces for those who smoke >25 cigarettes/day. One gum piece every 1-2 h is used for the first 6 weeks and then one piece every 2-4 h for 2 weeks (7th-9th week) and then one piece every 4-8 h for another 2 weeks. Nicotine from the gum is absorbed through the buccal mucosa, with peak nicotine plasma concentration reached within 15-30 min, when compared with 1-2 min after smoking a cigarette.[53] Acidic beverages like coffee and juices should be avoided before and after the use of nicotine gum, because they decrease the absorption of nicotine. Nicotine gum also provides substitute oral activity during tobacco abstinence.
Nicotine lozenge
Similar to nicotine gum, the nicotine polacrilex lozenge is available over-the-counter as an aid for smoking cessation in 2 mg and 4 mg doses of nicotine. The 4 mg dose is preferred for highly dependent smokers - those who smoke within 30 min of awakening.[54] The nicotine lozenge delivers 25% more nicotine than nicotine gum, because some nicotine is retained in the gum and nicotine is dissolved completely.[55] The lozenge may have better patient acceptability, especially in those who cannot use the gum because of dentures temporomandibular joint pain or for those who do not prefer chewing gum.
Nicotine trans-dermal patch
A trans-dermal delivery system can eliminate some of compliance and chewing problems associated with nicotine polacrilex gum. Steady-state administration expected from such a system may be more effective in preventing withdrawal symptoms. Since the patch does not allow for self-administration in response to the smoking urge, it could potentially be used in combination with the other rapidly absorbed forms of nicotine replacement. Nicotine trans-dermal system acts better when used in conjunction with a support programme such as counseling, group therapy or behavior therapy.
The nicotine patch is available for 16- or 24-h delivery systems. For the 24-h delivery system the recommended dose of trans-dermal patch for those who smoke >10 cigarettes/day, 21 mg patch is used every day for the first 6 weeks, then 14 mg every day for the next 2 weeks and then 7 mg patch every day for another 2 weeks. If the cigarette consumption is lesser than 10 cigarettes a day, 14 mg patch/day for first 6 weeks and then 7 mg patch/day for another 2 weeks is used [Table 1]. For the 16-h delivery system, where the patch is taken off before going to sleep, the recommended dose is 15 mg/day for 6 weeks. A meta-analysis shows no benefit of using the nicotine patch longer than 8 weeks.[56] With the nicotine patch, nicotine is absorbed slowly, with peak levels reaching 4-8 h after application and nicotine levels are about half those obtained through smoking. The nicotine patch is easy to administer, requires less frequent dosing, with fewer adverse effects and better compliance. The disadvantage of the patch is the lack of acute (rescue) dosing for craving episodes, which can be provided with other NRTs.[57] In fact, the nicotine patch may be combined with other NRTs to increase its efficacy in treatment resistant cases.[58]
Table 1.
Medications for smoking cessation
The use of nicotine chewing gum or trans-dermal nicotine patches during smoking cessation delays weight gain until NRT is stopped. However, neither nicotine gum nor the patch combined with smoking cessation provides any long-term benefit of attenuating weight gain.[26]
NNS
A gel-like droplet of nicotine is squeezed into the nose from a small vial. Rapid and efficient absorption of nicotine from the gel is possible. It achieves peak venous nicotine levels within 4-15 min, faster than any other NRT. Due to the fast nicotine delivery, nicotine spray may have some abuse liability (patients continue to use spray even after quitting smoking).[9]
One dose of nicotine nasal spray is equal to two sprays (0.5 mg/spray). The usual recommended dose is 1-2 doses/h for 8 weeks, with a minimum of 8 doses/day and maximum of 40 doses/day and maximum 3 months use [Table 1]. Between weeks 9 and 14, a gradual taper is recommended. The main disadvantage of a nasal spray is the initial local irritation and for some patients stigma of its use.
Nicotine aerosols (inhaler)
With nicotine inhaler, the nicotine is absorbed through the buccal mucosa in contrast to the absorption through the lungs with cigarette smoking. On inhalation with inhaler, peak plasma, nicotine concentrations are generally achieved within 15 min.[59] The recommended dose of nicotine inhaler is 6-16 cartridges/day for 12 weeks, with a gradual weaning over 6-12 weeks. Each cartridge contains 10 mg of nicotine and delivers a maximum of 4 mg of nicotine. One cartridge provides 20 min of active puffing. Nicotine sublingual tablets are also available as NRT.
Comparison of preparations
All nicotine replacement products produce side-effects. Nicotine polacrilex gum may produce mouth sores, gastric upset and hiccups. NNS produces runny nose and irritation, whereas trans-dermal devices can result in skin irritation. Trans-dermal devices have the advantage of better patient compliance with treatment and steady-state drug levels, whereas NSS and nicotine polcrilex gum have the advantage of ad libitum access to replacement. A combination of preparations may be most useful to control symptoms as well as to allow instance responses to smoking urges.
Dependence on nicotine replacement
Withdrawal symptoms upon abrupt cessation of nicotine polacrilex gum have been reported which indicate that nicotine polacrilex gum produces physical dependence. How much should be the length of treatment with nicotine replacement devices, is still not clear. Many abstinent smokers are unable to discontinue nicotine polacrilex gum use.
Since nicotine can increase a baby's heart rate, a pregnant woman or a nursing mother should be cautious to use a NRT. Moreover, these products should not be used by any one below 18 years of age or who continues to use any other product that contains nicotine. Side-effects and complications associated with these products are similar to those found when smoking cigarettes and include irregular or rapid heartbeat, palpitation, nausea, vomiting, dizziness and weakness. Persons with heart disease, recent myocardial infarction, hypertension, gastric ulcer, insulin treatment for diabetes mellitus and anti-depressant drugs or drugs for asthma should consult a physician prior to use.[60]
Other pharmacological therapies
Nicotine administration and its withdrawal produce a number of neurohormonal and other physiological effects and these effects mediate various actions of tobacco. Because several such effects are functional in maintenance of cigarette smoking and in relapse, it is generally assumed that addressing such factors would enhance treatment programmes. Such strategies are also an integral part of many interventions for drug addiction in general.
There is a long history of unsuccessful pharmacologic treatment of smoking cessation. Experimentation with lobeline sulfate as a smoking substitute dates back to early 1900s. Lobeline is a partial nicotine agonist (that is, it blocks the effects of nicotine), which has been used in a variety of commercially available preparations to help stop smoking. The rationale for its use in smoking cessation is that it may block the rewarding effect of nicotine and thus reducing the urge for smoke. However, lobeline appears to be no more effective than a placebo in facilitating abstinence.
Anti-depressants – fluoxetine has a small effect on cessation and that other antidepressants might also be effective. Bupropion and nortriptyline are other anti-depressants of particular interest in the treatment of smoking cessation.
Bupropion
It is an anti-depressant in a SR form with its action as a neuronal reuptake inhibitor of dopamine and noradrenalin. It was observed that the depressives treated with bupropion spontaneously stopped smoking. The dopaminergic and noradrenergic properties of bupropion hydrochloride provide a theoretical benefit in smoking cessation, in treating the neurochemical changes resulting from nicotine addiction and withdrawal. Bupropion hydrochloride has the benefit of being an oral non-nicotine therapy. Studies demonstrated the efficacy of Bupropion SR for the treatment of tobacco dependence.[61] FDA approved its therapeutic use in 1997 as a first-line treatment for tobacco cessation. Bupropion is equally effective in smokers with or without a history of depression however, this drug could be a better choice in the smokers with the history of depression. The depressives already being treated with some anti-depressants and wish to quit smoking can be given bupropion additionally.
Bupropion is chemically unrelated to nicotine or other agents currently used in the treatment of tobacco dependence. It is a week but selective inhibitor of the neuronal reuptake of dopamine and noradrenalin, with a very minimal effect on serotonin and does not inhibit MAO. Abstaining effect of bupropion is presumably related to its dopaminergic and/or adrenergic properties and to involve the two pathways in the brain that are important in the addiction process. It is hypothesized that dopaminergic activity of bupropion affects the area implicated in the reinforcing properties of the addictive drug and the development of dependence - the reward pathway, or mesolimbic system - while its noradrenergic activity in the locus ceruleus plays a role in withdrawal from nicotine.
Bupropion increases the levels of extracellular dopamine in the nucleus accumbens and enhances dopaminergic activity in the ventral tegmental area of the midbrain via inhibition of reuptake. These effects of dopamine are responsible for overcoming the dependence on nicotine and helping to reduce the craving associated with nicotine dependence. Bupropion decreases the firing rate of noradrenergic neurons in the locus ceruleus; enhances noradrenergic activity, which account for the reduction in nicotine withdrawal symptoms. Bupropion also produces an acute functional blockade of human nicotine receptors.
Bupropion treatment is started while the patient is still smoking and a target date to stop smoking is fixed within 2 weeks of onset of therapy. This is done to allow the time for plasma levels of bupropion to reach steady state and, hence, for the drug to start working effectively. The initial dose should be 150 mg daily for 3 days, increasing to 150 mg twice a day to a remainder of 2 months course (maximum length of treatment 9-12 weeks). However, some clinicians recommend treatment up to 6 months.[62] The length of treatment for tobacco use cessation depends upon many factors, including severity of addiction and the presence or absence of co-morbidities. It is important that the patients complete the full treatment course prescribed in order to maximize the likelihood of long-term abstinence from smoking and so that any patient who fails to quit smoking on the “stop date” can set a new one with the possibility of quitting later in the treatment course.[63] There should be an interval of at least 8 h between successive doses. Maximum single dose should not exceed 150 mg and the total daily dose should not exceed 300 mg.
Similar to other anti-depressants, bupropion also lowers the seizure threshold and should not be used in those with history of seizure disorder, serious head trauma, eating disorders (bulimia or anorexia nervosa) and in those who receive other medications that may lower seizure threshold.
Nortriptyline
Nortriptyline is a tricyclic anti-depressant medication found effective in smoking cessation in various clinical trials.[64,65] It is recommended as a second-line medication for tobacco cessation[35] in the dosage of 75-100 mg/day and length of treatment is 8-12 weeks.
Clonidine
Clonidine was originally approved to lower blood pressure. It is an alfa-2-adrenergic receptor agonist anti-hypertensive agent that decreases central sympathetic activity. It acts on the central nervous system and may reduce withdrawal symptoms associated with smoking cessation. Potentially hazardous side effects of clonidine should be considered before starting it as an adjunct therapy for smoking cessation. Abrupt cessation of clonidine in some cases has led to severe hypertension and in rare cases to hypertensive encephalopathy and even death. More common is sedation and one should not use it while driving or under similar situations.
Although clonidine is effective for smoking cessation, its clinical use is limited by significant adverse effects, such as sedation, dizziness and dry mouth. Clonidine appears to be more effective in female smokers[28] and it is a second-line option for smoking cessation pharmacotherapy.
Anxiolytics
The signs and symptoms of tobacco withdrawal vary in nature and severity among individuals. Symptoms can be treated independently of their origin; symptomatic therapeutic approach might be useful in the alleviation of tobacco abstinence-associated discomfort. Alprazolam (1 mg orally) may be effective in reducing the craving for a cigarette. However, there is little evidence of effectiveness of anxiolytics, benzodiazepines, in improving smoking cessation.[61]
Nicotine may serve as a regulator of mood, selective use of minor tranquilizers, or even psychomotor stimulants may be beneficial in preventing relapse. Stressful situations lead to increased smoking and that smoking may reduce smoker distress responses to stressful stimuli and enhance reported mood. Relapse to cigarette smoking generally occur in response to stressful situations.
Varenicline
It is an analogue of cyticine, reported to have the benefit in smoking cessation. Varenicline has high and selective activity at alfa4-beta2 receptor. It is a partial agonist at this receptor in vivo producing lesser response than that of nicotine (30-60%) but also blocks the effect of any nicotine added to the system. It stimulates the central nervous mesolimbic system, the neuronal mechanism underlying reinforcement and reward experienced upon smoking. Thus, varenicline maintains a moderate level of dopamine release, which reduces craving and withdrawal symptoms during abstinence. It also blocks the reinforcing effects of nicotine obtained from cigarette smoke in the case of relapse.[66,67,68] Varenicline is the non-nicotine containing medication developed with the purpose of treating nicotine addiction. The recommended treatment begins 1-2 weeks before the quit date. For the first 3 days 0.5 mg daily dose is given and on the 4th day the dose is increased to 0.5 mg twice daily up to 7th day. The dose is further increased on 8th day to 1 mg twice a day up to the end of 12 weeks. A further treatment for another 12 weeks with 1 mg twice a day is recommended[69] to prevent relapse. The efficacy of varenicline has been demonstrated in various clinical trials. The main adverse effects such as nausea, headache, vomiting, flatulence, insomnia and abnormal dreams, generally mild in nature are observed which diminish over time. Varenicline is found to have significant effectiveness in long-term relapse prevention. Increased cessation rates have been demonstrated both in long-term and short-term therapy.[70] In India where use of smoke-less tobacco is quite common,[2] varenicline was found to be effective in a double-blind placebo controlled randomized trial for the treatment of smokeless tobacco dependence. Varenicline was also found to be safe for treating smoke-less tobacco dependence.[71]
Nicotine blockade therapy
The goal of blockade therapy is to reduce or eliminate any rewarding pharmacological effects, should the person attempt to resume the drug use. Pharmacological antagonists of nicotine, which diminish a variety of responses to nicotine, have been known for several decades. Those antagonists, which act both centrally and peripherally (mecamylamine), but not those that only act peripherally (pentolinium and hexamethonium); appear to have functional effects on pattern of cigarette smoking in humans. Certain antagonists also alter the behavioral effects of nicotine (including self-administration) in animals.[72]
Mecamylamine
It can be used as an antagonist to block the nicotine-mediated reinforcing consequences of cigarette smoking. The following findings are of particular relevance:
Mecamylamine pre-treatment produces a dose-related blockade of the ability of animals and humans to discriminate nicotine from a placebo.
Mecamylamine pre-treatment diminishes the reinforcing efficacy of intravenous nicotine administration in animals[73] and possibly in human beings.[74]
Mecamylamine pre-treatment increases the preference for high-nicotine-delivering cigarette smoke (apparently by reducing its nicotine effects) when subjects are tested with a device which blends smoke from high and low nicotine-delivering cigarettes.
Mecamylamine pre-treatment increases various measures of cigarette smoking behavior and tobacco smoke intake when subjects are allowed to freely smoke.
In heavy cigarette smokers, mecamylamine combined with counseling, reduces craving for smoking and helps 50% of the subjects quit smoking within 2 weeks of initiation of treatment. In a study, the mean dose of mecamylamine at the time of quitting was 26.7 mg/day. Because mecamylamine blocks the effects of nicotine, it precipitates withdrawal and hence is not of help in acute cessation. The difficulties to this treatment approach are the ganglionic blocking and anti-hypertensive effects of mecamylamine the strong likelihood of considerable difficulty of obtaining adequate therapeutic compliance and conditioned and non-nicotine mediated reinforce of tobacco use, which may be powerful enough to sustain urges to smoke even when they are no longer associated with the pharmacological effects of nicotine.[75]
Naltrexone
It is a long acting firm of opioid antagonist. The rationale for using naltrexone for smoking cessation is that the performance enhancing and other positive effects of nicotine may be opioid mediated. Some studies point out the beneficial effects of Naltrexone.[76]
Newer drugs
NicVAX
It works by stimulating the immune system to make antibodies that bind to nicotine molecules, making them too big to cross the blood-brain barrier and preventing them from reaching nicotine receptors and triggering the pleasure sensation that smokers experience and become addicted to. Data from pre-clinical trials suggest that the injectable vaccine would be effective not only in helping people quit smoking but also from relapsing back into the habit because the nicotine antibodies last a long time.[77]
Tobacco addiction, like other addictions, is a complex process involving the interplay of pharmacology, conditioned factors, personality and social setting. Therefore, the ideal treatment for tobacco-cessation involves a comprehensive approach that addresses all major issues of tobacco addiction both pharmacological and non-pharmacological.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ashton H, Stepney R. Smoking: Psychological and Pharmacology. London: Tavistock Publications; 1982. [Google Scholar]
- 2.Jiloha RC. Tobacco Use: Health and Behaviour. Delhi: New Age International; 2008. [Google Scholar]
- 3.Jiloha RC. Biological basis of tobacco addiction: Implications for smoking-cessation treatment. Indian J Psychiatry. 2010;52:301–7. doi: 10.4103/0019-5545.74303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balfour DJ, Wright AE, Benwell ME, Birrell CE. The putative role of extra-synaptic mesolimbic dopamine in the neurobiology of nicotine dependence. Behav Brain Res. 2000;113:73–83. doi: 10.1016/s0166-4328(00)00202-3. [DOI] [PubMed] [Google Scholar]
- 5.Stauffer HP, Riedwyl H. Interaction and pH dependence of effects of nicotine and carbon monoxide in cigarette smoke inhalation experiments with rats. Agents Actions. 1977;7:579–88. doi: 10.1007/BF02111133. [DOI] [PubMed] [Google Scholar]
- 6.Zhou FM, Liang Y, Dani JA. Endogenous nicotinic cholinergic activity regulates dopamine release in the striatum. Nat Neurosci. 2001;4:1224–9. doi: 10.1038/nn769. [DOI] [PubMed] [Google Scholar]
- 7.Tomkins DM, Sellers EM. Addiction and the brain: The role of neurotransmitters in the cause and treatment of drug dependence. CMAJ. 2001;164:817–21. [PMC free article] [PubMed] [Google Scholar]
- 8.Pontieri FE, Tanda G, Orzi F, Di Chiara G. Effects of nicotine on the nucleus accumbens and similarity to those of addictive drugs. Nature. 1996;382:255–7. doi: 10.1038/382255a0. [DOI] [PubMed] [Google Scholar]
- 9.West R, Hajek P, Foulds J, Nilsson F, May S, Meadows A. A comparison of the abuse liability and dependence potential of nicotine patch, gum, spray and inhaler. Psychopharmacology (Berl) 2000;149:198–202. doi: 10.1007/s002130000382. [DOI] [PubMed] [Google Scholar]
- 10.Pomerleau O, Adkins D, Pertschuk M. Predictors of outcome and recidivism in smoking cessation treatment. Addict Behav. 1978;3:65–70. doi: 10.1016/0306-4603(78)90028-x. [DOI] [PubMed] [Google Scholar]
- 11.Ikard FF, Tomkins S. The experience of affect as a determinant of smoking behavior: A series of validity studies. J Abnorm Psychol. 1973;81:172–81. doi: 10.1037/h0034555. [DOI] [PubMed] [Google Scholar]
- 12.Hughes JR, Goldstein MG, Hurt RD, Shiffman S. Recent advances in the pharmacotherapy of smoking. JAMA. 1999;281:72–6. doi: 10.1001/jama.281.1.72. [DOI] [PubMed] [Google Scholar]
- 13.Kenkel D, Chen L. Consumer information and tobacco use. In: Jha P, Chaloupka FJ, editors. Tobacco Control in Developing Countries. Oxford: Oxford University Press; 2000. pp. 77–214. [Google Scholar]
- 14.Russell MA. The nicotine addiction trap: A 40-year sentence for four cigarettes. Br J Addict. 1990;85:293–300. doi: 10.1111/j.1360-0443.1990.tb03085.x. [DOI] [PubMed] [Google Scholar]
- 15.DiFranza JR, Rigotti NA, McNeill AD, Ockene JK, Savageau JA, St Cyr D, et al. Initial symptoms of nicotine dependence in adolescents. Tob Control. 2000;9:313–9. doi: 10.1136/tc.9.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mansvelder HD, McGehee DS. Long-term potentiation of excitatory inputs to brain reward areas by nicotine. Neuron. 2000;27:349–57. doi: 10.1016/s0896-6273(00)00042-8. [DOI] [PubMed] [Google Scholar]
- 17.Brownell KD. Dieting and the search for the perfect body: Where physiology and culture collide. Behav Ther. 1991;22:1–12. [Google Scholar]
- 18.Hajek P, Jackson P, Belcher M. Long-term use of nicotine chewing gum. Occurrence, determinants and effect on weight gain. JAMA. 1988;260:1593–6. [PubMed] [Google Scholar]
- 19.Moffatt RJ, Owens SG. Cessation from cigarette smoking: Changes in body weight, body composition, resting metabolism and energy consumption. Metabolism. 1991;40:465–70. doi: 10.1016/0026-0495(91)90225-l. [DOI] [PubMed] [Google Scholar]
- 20.Perkins KA, Epstein LH, Marks BL, Stiller RL, Jacob RG. The effect of nicotine on energy expenditure during light physical activity. N Engl J Med. 1989;320:898–903. doi: 10.1056/NEJM198904063201404. [DOI] [PubMed] [Google Scholar]
- 21.Williams M, Sullivan JP, Arneric SP. Neuronal nicotine acetylcholine receptors. Drug News Perspect. 1994;7:205–23. [Google Scholar]
- 22.Pirie PL, McBride CM, Hellerstedt W, Jeffery RW, Hatsukami D, Allen S, et al. Smoking cessation in women concerned about weight. Am J Public Health. 1992;82:1238–43. doi: 10.2105/ajph.82.9.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crisp AH. Regulation of the self in adolescence with particular reference to anorexia nervosa. Trans Med Soc Lond. 1982;99-100:67–74. [PubMed] [Google Scholar]
- 24.Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. N Engl J Med. 1991;324:739–45. doi: 10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- 25.Killen JD, Fortmann SP, Newman B. Weight change among participants in a large sample minimal contact smoking relapse prevention trial. Addict Behav. 1990;15:323–32. doi: 10.1016/0306-4603(90)90042-v. [DOI] [PubMed] [Google Scholar]
- 26.Perkins KA, Levine MD, Marcus MD, Shiffman S. Addressing women's concerns about weight gain due to smoking cessation. J Subst Abuse Treat. 1997;14:173–82. doi: 10.1016/s0740-5472(96)00158-4. [DOI] [PubMed] [Google Scholar]
- 27.Gilbert RM, Pope MA. Early effects of quitting smoking. Psychopharmacology (Berl) 1982;78:121–7. doi: 10.1007/BF00432247. [DOI] [PubMed] [Google Scholar]
- 28.Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. Am J Psychiatry. 1994;151:979–86. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 29.Craig D, Parrott A, Coomber JA. Smoking cessation in women: Effects of the menstrual cycle. Int J Addict. 1992;27:697–706. doi: 10.3109/10826089209068761. [DOI] [PubMed] [Google Scholar]
- 30.Borrelli B, Bock B, King T, Pinto B, Marcus BH. The impact of depression on smoking cessation in women. Am J Prev Med. 1996;12:378–87. [PubMed] [Google Scholar]
- 31.Glassman AH. Cigarette smoking: Implications for psychiatric illness. Am J Psychiatry. 1993;150:546–53. doi: 10.1176/ajp.150.4.546. [DOI] [PubMed] [Google Scholar]
- 32.Ward KD, Klesges RC, Zbikowski SM, Bliss RE, Garvey AJ. Gender differences in the outcome of an unaided smoking cessation attempt. Addict Behav. 1997;22:521–33. doi: 10.1016/s0306-4603(96)00063-9. [DOI] [PubMed] [Google Scholar]
- 33.Campbell IA, Lyons E, Prescott RJ. Stopping smoking. Do nicotine chewing-gum and postal encouragement add to doctors’ advice. Practitioner. 1987;231:114–7. [PubMed] [Google Scholar]
- 34.Gamberino WC, Gold MS. Neurobiology of tobacco smoking and other addictive disorders. Psychiatr Clin North Am. 1999;22:301–12. doi: 10.1016/s0193-953x(05)70078-2. [DOI] [PubMed] [Google Scholar]
- 35.Fiore MC, Bailey WC, Cohen SJ. A Clinical Practice Guideline. Rockville, MD: US Department of Health and Human Services; 2000. Treating Tobacco Use and Dependence. [Google Scholar]
- 36.Crowe RR, Kramer JR, Hesselbrock V, Manos G, Bucholz KK. The utility of the Brief MAST’ and the CAGE’ in identifying alcohol problems: Results from national high-risk and community samples. Arch Fam Med. 1997;6:477–83. doi: 10.1001/archfami.6.5.477. [DOI] [PubMed] [Google Scholar]
- 37.Morton JL, Jones TV, Manganaro MA. Performance of alcoholism screening questionnaires in elderly veterans. Am J Med. 1996;101:153–9. doi: 10.1016/s0002-9343(96)80069-6. [DOI] [PubMed] [Google Scholar]
- 38.Lairson DR, Harrist R, Martin DW, Ramby R, Rustin TA, Swint JM, et al. Screening for patients with alcohol problems: Severity of patients identified by the CAGE. J Drug Educ. 1992;22:337–52. doi: 10.2190/H8QV-KAYU-QBYH-1LN3. [DOI] [PubMed] [Google Scholar]
- 39.Fiore MC, Jaen CR, Baker TB. Treating tobacco use and dependence: 2008 update. US Department of Health and Human Services. 2008. [Last accessed on 2011 Oct 17]. Available from: http://www.surgeongeneral.gov/tobacco/treating_tobacco_use08.pdf .
- 40.Quick Reference Guide for Clinicians: Treating Tobacco Use and Dependence. Washington (DC): The Department; 2000. [Last accessed on 2008 May 12]. US Department of Health and Human Services. Available from: http://www.ahrq.gov/clinic/tobacco/tobaqrg.pdf . [Google Scholar]
- 41.Tønnesen P, Tonstad S, Hjalmarson A, Lebargy F, Van Spiegel PI, Hider A, et al. A multicentre, randomized, double-blind, placebo-controlled, 1-year study of bupropion SR for smoking cessation. J Intern Med. 2003;254:184–92. doi: 10.1046/j.1365-2796.2003.01185.x. [DOI] [PubMed] [Google Scholar]
- 42.Ahluwalia JS, Harris KJ, Catley D, Okuyemi KS, Mayo MS. Sustained-release bupropion for smoking cessation in African Americans: A randomized controlled trial. JAMA. 2002;288:468–74. doi: 10.1001/jama.288.4.468. [DOI] [PubMed] [Google Scholar]
- 43.Henningfield JE, Jasinki DR. Pharmacological basis for nicotine replacement. In: Pomerleau OF, Pomerleau CS, Fagerstrom KO, Henningfield JE, Hughjes JR, editors. Nicotine Replacement: A Critical Evaluation. New York: Alan R Liss; 1988. [Google Scholar]
- 44.Leventhal H, Cleary PD. The smoking problem: A review of the research and theory in behavioral risk modification. Psychol Bull. 1980;88:370–405. doi: 10.1037/0033-2909.88.2.370. [DOI] [PubMed] [Google Scholar]
- 45.Ferno O, Lichtneckert S, Lundgreen CA. A substitute for tobacco smoking. Psychopharmacologia. 1973;31:301–4. doi: 10.1007/BF00422510. [DOI] [PubMed] [Google Scholar]
- 46.Malcolm R, Currey HS, Mitchell MA, Keil JE. Silver acetate gum as a deterrent to smoking. Chest. 1986;90:107–11. doi: 10.1378/chest.90.1.107. [DOI] [PubMed] [Google Scholar]
- 47.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43:289–94. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 48.Henningfield JE, Sampson A, Nemeth-Coslett R. Effect of nicotine replacement in tobacco withdrawal. Presented at the American Psychological Convention; Washington DC. 1986. [Google Scholar]
- 49.West R, Schneider N. Craving for cigarettes. Br J Addict. 1987;82:407–15. doi: 10.1111/j.1360-0443.1987.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 50.Fagerstrom KO. Reducing the weight gain after stopping smoking. Addict Behav. 1987;12:91–3. doi: 10.1016/0306-4603(87)90015-3. [DOI] [PubMed] [Google Scholar]
- 51.Stitzer ML, Gross J. Smoking relapses: The role of pharmacological and behavioural factors. In: Pomerleau OF, Pomerleau CS, Fagerstrom KO, Henningfield JE, Hughes JR, editors. Nicotine Replacement: A Critical Evaluation. New York: Alan R Liss Inc.; 1988. [Google Scholar]
- 52.Hjalmarson AI. Effect of nicotine chewing gum in smoking cessation. A randomized, double blind placebo-controlled study studies. J Am Med Assoc. 1984;252:2835–8. [PubMed] [Google Scholar]
- 53.Benowitz NL. Pharmacology of nicotine: Addiction and therapeutics. Annu Rev Pharmacol Toxicol. 1996;36:597–613. doi: 10.1146/annurev.pa.36.040196.003121. [DOI] [PubMed] [Google Scholar]
- 54.Shiffman S, Dresler CM, Hajek P, Gilburt SJ, Targett DA, Strahs KR. Efficacy of a nicotine lozenge for smoking cessation. Arch Intern Med. 2002;162:1267–76. doi: 10.1001/archinte.162.11.1267. [DOI] [PubMed] [Google Scholar]
- 55.Choi JH, Dresler CM, Norton MR, Strahs KR. Pharmacokinetics of a nicotine polacrilex lozenge. Nicotine Tob Res. 2003;5:635–44. doi: 10.1080/1462220031000158690. [DOI] [PubMed] [Google Scholar]
- 56.Fiore MC, Smith SS, Jorenby DE, Baker TB. The effectiveness of the nicotine patch for smoking cessation. A meta-analysis. JAMA. 1994;271:1940–7. [PubMed] [Google Scholar]
- 57.Hurt RD, Offord KP, Croghan IT, Croghan GA, Gomez-Dahl LC, Wolter TD, et al. Temporal effects of nicotine nasal spray and gum on nicotine withdrawal symptoms. Psychopharmacology (Berl) 1998;140:98–104. doi: 10.1007/s002130050744. [DOI] [PubMed] [Google Scholar]
- 58.Sweeney CT, Fant RV, Fagerstrom KO, McGovern JF, Henningfield JE. Combination nicotine replacement therapy for smoking cessation: Rationale, efficacy and tolerability. CNS Drugs. 2001;15:453–67. doi: 10.2165/00023210-200115060-00004. [DOI] [PubMed] [Google Scholar]
- 59.Schneider NG, Olmstead RE, Franzon MA, Lunell E. The nicotine inhaler: Clinical pharmacokinetics and comparison with other nicotine treatments. Clin Pharmacokinet. 2001;40:661–84. doi: 10.2165/00003088-200140090-00003. [DOI] [PubMed] [Google Scholar]
- 60.Schuh KJ, Schuh LM, Henningfield JE, Stitzer ML. Nicotine nasal spray and vapor inhaler: Abuse liability assessment. Psychopharmacology (Berl) 1997;130:352–61. doi: 10.1007/s002130050250. [DOI] [PubMed] [Google Scholar]
- 61.Hurt RD, Sachs DP, Glover ED, Offord KP, Johnston JA, Dale LC, et al. A comparison of sustained-release bupropion and placebo for smoking cessation. N Engl J Med. 1997;337:1195–202. doi: 10.1056/NEJM199710233371703. [DOI] [PubMed] [Google Scholar]
- 62.Miller NS, Brady KT. Addictive disorders. Psychiatr Clin North Am. 2004;27:xi–xviii. doi: 10.1016/j.psc.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 63.Johnston JA, Hughes AR, Ascher JA. Evaluation of safety and tolerability of bupropion SR as an ad to smoking cessation. Poster presentation at the 5th Annual Meeting of The Society for Research on Nicotine and Tobacco; San Diego CA. 1999. [Google Scholar]
- 64.Prochazka AV, Weaver MJ, Keller RT, Fryer GE, Licari PA, Lofaso D. A randomized trial of nortriptyline for smoking cessation. Arch Intern Med. 1998;158:2035–9. doi: 10.1001/archinte.158.18.2035. [DOI] [PubMed] [Google Scholar]
- 65.Hall SM, Humfleet GL, Reus VI, Muñoz RF, Hartz DT, Maude-Griffin R. Psychological intervention and antidepressant treatment in smoking cessation. Arch Gen Psychiatry. 2002;59:930–6. doi: 10.1001/archpsyc.59.10.930. [DOI] [PubMed] [Google Scholar]
- 66.Jorenby DE, Hays JT, Rigotti NA, Azoulay S, Watsky EJ, Williams KE, et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: A randomized controlled trial. JAMA. 2006;296:56–63. doi: 10.1001/jama.296.1.56. [DOI] [PubMed] [Google Scholar]
- 67.Coe JW, Brooks PR, Vetelino MG, Wirtz MC, Arnold EP, Huang J, et al. Varenicline: An alpha4beta2 nicotinic receptor partial agonist for smoking cessation. J Med Chem. 2005;48:3474–7. doi: 10.1021/jm050069n. [DOI] [PubMed] [Google Scholar]
- 68.Gonzales D, Rennard SI, Nides M, Oncken C, Azoulay S, Billing CB, et al. Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: A randomized controlled trial. JAMA. 2006;296:47–55. doi: 10.1001/jama.296.1.47. [DOI] [PubMed] [Google Scholar]
- 69.Rao J, Shankar PK. Varenicline: For smoking cessation. Kathmandu Univ Med J (KUMJ) 2009;7:162–4. doi: 10.3126/kumj.v7i2.2714. [DOI] [PubMed] [Google Scholar]
- 70.Kaur K, Kaushal S, Chopra SC. Varenicline for smoking cessation: A review of the literature. Curr Ther Res. 2009;70:35–54. doi: 10.1016/j.curtheres.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jain R, Jhanjee S, Veena J, Gupta T. Nicotine and tobacco research. Oxford J: 2013. [Google Scholar]
- 72.Stolerman IP. Discriminative stimulus properties in nicotine: Correlations with nicotine binding. Proceedings of the International Symposium on Tobacco Smoking and Health: A Neuro-biologic Approach.1986. [Google Scholar]
- 73.Goldberg SR, Spealman RD, Risner ME, Henningfield JE. Control of behavior by intravenous nicotine injections in laboratory animals. Pharmacol Biochem Behav. 1983;19:1011–20. doi: 10.1016/0091-3057(83)90408-2. [DOI] [PubMed] [Google Scholar]
- 74.Henningfield JE, Goldberg SR. Control of behavior by intravenous nicotine injections in human subjects. Pharmacol Biochem Behav. 1983;19:1021–6. doi: 10.1016/0091-3057(83)90409-4. [DOI] [PubMed] [Google Scholar]
- 75.Tennant FS, Traver AL, Rawson RA. Clinical evaluation of mecamylamine for withdrawal from nicotine dependence. In: Harrison LS, editor. Problems of Drug-Dependence 1983 NIDA. Research Monograph 49. Department of Health and Human Services; 1984. [PubMed] [Google Scholar]
- 76.Kumar R, Vijayan VK. Smoking cessation programs and other preventive strategies for chronic obstructive pulmonary disease. J Assoc Physicians India. 2012;60(Suppl):53–6. [PubMed] [Google Scholar]
- 77.Paddock C. Vaccine to treat nicotine addiction steps closer to market as companies agree option deal. Medical News Today. 2009 Nov 18; [Google Scholar]


