Sir,
Post-dural-puncture-headache is a common complication seen after an intentional or an accidental breach of the dura mater at the spinal level. Epidural blood patch (EBP) is a commonly utilized interventional modality for treating difficult-to-intractable headache after a dural puncture. However, in comparison with the reports about the success rates of EBP, the complications and concerns related to EBP as an intervention itself have been rarely reported.[1] We hereby present a case wherein, our patient was re-admitted to the emergency room due to radicular pains after a successful EBP.
A 20-year-old female patient presented to the emergency room with the chief complaint of intermittent and shooting low back pain, radiating bilaterally to buttocks and knees. Four days prior, she had undergone a continuous labor epidural placement, complicated by post-dural-puncture-headache that was most likely secondary to unrecognized dural puncture during epidural placement. Subsequently, she had received an EBP with 20 mL autologous blood. She had not reported pain or neurological symptoms during EBP placement. Her back pain had started 48 h after EBP placement. Emergent magnetic resonance imaging (MRI) of the lumbosacral spine revealed small amounts of clear fluid with hemorrhagic components in posterior lumbar epidural space, associated with thecal sac compression [Figure 1]. Neurosurgery team recommended conservative management. Patient was discharged home with analgesics and advised regular follow-up.
Figure 1.
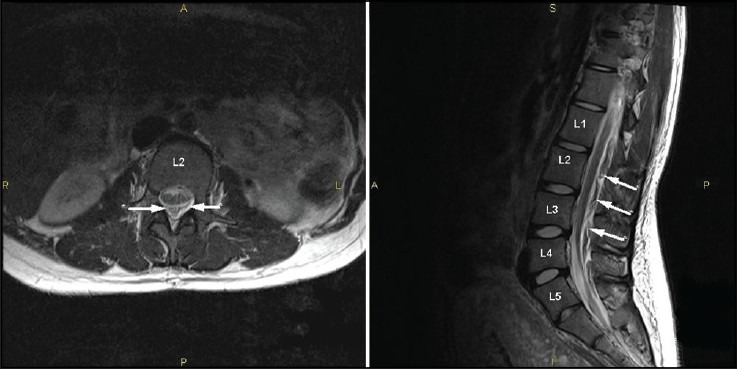
T2-weighted magnetic resonance imaging: Axial image (image on the left side) at second lumbar vertebral body (L2) and sagittal image (image on the right side) of the lumbosacral spine demonstrating diffuse, but mild thecal compression secondary to the collection in the posterior epidural space; limits of this epidural space collection (inhomogeneous foci representing blood-mixed cerebrospinal fluid) is marked by (←) in axial image for its side-to-side extent and by (←) in sagittal image for its posterior extent. Incidental finding of transitional fifth lumbar vertebra marked as L5
Back pain following neuraxial procedures (including EBP) is secondary to procedural technique, irritant medications as well as due to compression secondary to fluid collection.[2,3] In patients with non-resolving or worsening back pain or neurological symptoms, lumbosacral MRI may be essential to rule out significant post-EBP complications such as intrathecal hematoma,[4] cauda equina syndrome,[4] spinal subdural hematoma[3] and epidural abscess.[2,4] In contrast to our patient's presentation, these catastrophic complications usually have rapidly-progressive course with worsening sensorimotor deficits and bladder-bowel dysfunction unless an early diagnosis with MRI and timely neurosurgical intervention ensue.[2] In our patient, fluid with blood components was confined to posterior epidural space without any apparent subdural or intrathecal extensions of injected blood ruling out the above mentioned catastrophic complications of EBP. In addition based on her symptoms, non-infectious (inflammatory) arachnoiditis was considered as differential diagnosis, but the definitive radiological signs for arachnoiditis[5] (loculated subarachnoid space, clumped nerve roots with “empty-sac” sign) were not present. Hence, we concluded that our patient developed compressive lumbar radiculopathy secondary to standard volume (20 mL) EBP unlike as reported with large volume (40 mL) EBP by Desai et al.[3] Although Beards et al. had demonstrated that only small clots were visible 18 h following EBP injection,[6] our patient demonstrated blood (injected component) with cerebrospinal fluid (leakage component) within the epidural space, even 48 h following EBP. However, it cannot be ruled out that the fluid component visible on MRI was secondary to the onset of clot organization with liquefaction in the epidural space because EBP induces accelerated coagulation mechanisms in the region of cerebrospinal fluid leak.[6]
In summary, although immediate but transient radicular symptoms during EBP placement have been used as cut-off for injected blood volume's therapeutic adequacy and safety,[7,8] persistent radicular symptoms in post-EBP patients act as warning signals for compressive lumbar radiculopathy that requires active interventions including analgesics and steroidal medications[3] as well as neurosurgical consultation.
References
- 1.Weakland HJ. The epidural blood patch — Current practices and concerns. CRNA. 1994;5:156–63. [PubMed] [Google Scholar]
- 2.New York: The New York School of Regional Anesthesia (NYSORA, Inc.); 1996; 2012. [Updated on 2009 Jan 3; Cited on 2013 Jun 10]. Nysora.com [homepage on the Interne]. Epidural blockade [about 1 screen] Available from: http://www.nysora.com/regional_anesthesia/neuraxial_techniques/3026-epiduralblockade.html . [Google Scholar]
- 3.Desai MJ, Dave AP, Martin MB. Delayed radicular pain following two large volume epidural blood patches for post-lumbar puncture headache: A case report. Pain Physician. 2010;13:257–62. [PubMed] [Google Scholar]
- 4.Kalina P, Craigo P, Weingarten T. Intrathecal injection of epidural blood patch: A case report and review of the literature. Emerg Radiol. 2004;11:56–9. doi: 10.1007/s10140-004-0365-0. [DOI] [PubMed] [Google Scholar]
- 5.Holz A, Levy LM, Coombs BD, DeLaPaz RL, Krasny RM, Smirniotopoulos JG. New York: WebMD LLC; 1994-2013. [Updated on 2011 May 25; Cited on 2013 Jun 10]. Arachnoiditis imaging [about 1 screen]. Emedicine.Medscape.com [homepage on the Internet] Available from: http://emedicine.medscape.com/article/336605-overview#a21 . [Google Scholar]
- 6.Beards SC, Jackson A, Griffiths AG, Horsman EL. Magnetic resonance imaging of extradural blood patches: Appearances from 30 min to 18 h. Br J Anaesth. 1993;71:182–8. doi: 10.1093/bja/71.2.182. [DOI] [PubMed] [Google Scholar]
- 7.Szeinfeld M, Ihmeidan IH, Moser MM, Machado R, Klose KJ, Serafini AN. Epidural blood patch: Evaluation of the volume and spread of blood injected into the epidural space. Anesthesiology. 1986;64:820–2. doi: 10.1097/00000542-198606000-00028. [DOI] [PubMed] [Google Scholar]
- 8.Mehta B, Tarshis J. Repeated large-volume epidural blood patches for the treatment of spontaneous intracranial hypotension. Can J Anaesth. 2009;56:609–13. doi: 10.1007/s12630-009-9121-y. [DOI] [PubMed] [Google Scholar]


